1236
Biliary pancreatitis occurs when the bile ducts become inflamed and is most often accompanied by severe abdominal pain. The diagnosis is made by doctors based on test results and diagnostics.
This form of inflammation of the pancreas most often occurs in a chronic condition, which is determined by the characteristics of the course of concomitant diseases. A patient with chronic pathology must follow the doctor’s recommendations throughout his life and undergo timely treatment.
What is biliary pancreatitis
The digestive system includes two important glands – the liver and pancreas (in Latin “pancreas”). The secretions they produce - bile and pancreatic juice - flow through the common duct of Vater into the duodenum.
This relationship becomes the cause of biliary pancreatitis - inflammation of the pancreas, provoked by diseases of the liver, gallbladder and bile ducts, which together form the hepatobiliary system.
The disease occurs in two forms: acute and chronic.
Treatment
The manifesting symptoms and treatment of the biliary form of pancreatitis should primarily consist of eliminating the primary pathology and normalizing the functionality of the affected liver, gallbladder or bile ducts.
To relieve pain, it is necessary to take into account the form of intestinal dysfunction: if spasm of the gallbladder and bile ducts develops, it is necessary to take antispasmodic medications, in the form of Duspatalin or Debridate; with the development of atonic processes, prokinetic drugs are prescribed, such as Domperidone, Eglonil, Metoclopromide.
To restore the composition and properties of bile, combination drugs with a hepostabilizing effect complemented by an antispasmodic effect, such as Hepatofalk or Odeston, are prescribed.
Treatment of chronic biliary pancreatitis can be carried out through conservative therapy and direct surgical intervention. The most important role in the treatment of the disease is given to a special dietary diet.
Causes of the disease
There are several causes of biliary-dependent pancreatitis:
- Congenital pathologies of the biliary system (narrowing of the ducts, bending of the gallbladder) cause bile to enter the pancreas and become inflamed.
- As a result of inflammatory lesions, the infection penetrates through the lymphatic tract into the pancreas, and pancreatitis develops.
- If there are stones in the bladder (gallstones), bile can enter the pancreas, causing irritation.
- Thickening of bile leads to the formation of sediment on the walls of the bile ducts, narrowing of their lumen, reflux of bile into the pancreatic ducts, and the development of pancreatitis.
- Pathologies of the duct of Vater (tumor, narrowing) prevent the passage of bile into the intestines and contribute to its entry into the pancreas.
Stone formation is considered the main cause of the disease: chronic biliary pancreatitis is found in more than 50% of people suffering from gallstone disease.
A long period of primary pathologies helps to maximize the likelihood of developing a disease such as chronic biliary-dependent pancreatitis, and in most cases, the development of this disease is facilitated by cholelithiasis with the presence of small stones in the gallbladder ducts.
The movement of stones along the bile ducts causes pancreatitis in the acute stage. It can be triggered by overeating, fatty and fried foods, and carbonated drinks.
Causes
Stones in the ducts are frequent provocateurs of the development of biliary pancreatitis.
More than 60% of cases of this pathology are indirectly associated with the development of gallstone disease. Also, provoking factors include the following:
- disruption of the structure of the choleretic tract;
- inflammatory lesions of the gallbladder;
- problems with gallbladder contraction;
- cirrhosis and other liver damage;
- helminthic infestations;
- inflammatory and pathological phenomena in the area of the duodenal papilla.
That is, such a disease belongs to the class of secondary diseases. This is explained by the fact that it is a consequence of malfunctions not of the pancreas itself, but of functional failures occurring in nearby organs.
Symptoms of biliary pancreatitis
The chronic process is often characterized by the absence of clinical manifestations, but the following signs may be observed:
- dull pain in the epigastrium and/or right hypochondrium that occurs a couple of hours after eating;
- night pain that radiates to the back;
- nausea, sometimes vomiting;
- bitterness in the mouth is possible in the morning;
- bowel disorders, especially after overeating;
- loss of appetite;
- weight loss
In the acute stage, biliary-dependent pancreatitis is characterized by paroxysmal severe pain caused by the movement of stones.
Biliary-dependent pancreatitis: symptoms, prognosis
The symptoms of the disease are in many ways similar to other disorders of the digestive system, which makes diagnosis difficult. In the absence of severe pain, patients are in no hurry to consult a specialist, attributing their malaise to fatigue, poor quality of products, etc.
Meanwhile, the symptoms of biliary pancreatitis are as follows:
- Vomit;
- Nausea;
- Pain in the hypochondrium and back;
- Bitter taste in the mouth;
- Constipation;
- Diarrhea;
- Diarrhea.
Patients note that, as a rule, anxiety begins some time after eating fried, spicy and/or fatty foods. The nature of the pain varies depending on whether it is an acute attack or a chronic stage of the disease.
Chronic biliary pancreatitis is characterized by aching and prolonged pain. Together with a slight increase in temperature and acute spasm, the acute phase of the disease makes itself felt.
Pancreatitis is an insidious disease that has a bad reputation and a generally unfavorable prognosis. However, in fairness, we note that the success of treatment largely depends on discipline and responsibility. This means that you need to not only listen to the doctor’s recommendations, but also follow them unquestioningly.
Diagnostic methods
To make an accurate diagnosis, a complex of laboratory and instrumental techniques is used. Laboratory research methods include general clinical and biochemical tests of blood, urine and feces. In biliary acute pancreatitis, leukocytosis is detected in the blood and the ESR increases. In the case of a protracted chronic process, their decrease relative to the norm is noted.
Biochemical blood parameters allow you to assess the condition of the biliary system, liver and pancreas:
- During an exacerbation, the content of total protein and globulins in the blood increases, and the level of albumin decreases.
- The amount of amylase enzyme in the blood and urine, which is responsible for the breakdown of carbohydrates in the intestines, increases.
- The activity of lipase in the blood, which is involved in the breakdown of lipids, increases.
- Bilirubin levels increase. This indicates swelling of the gland, which prevents the release of bile into the intestines.
- Stagnation of bile in the biliary system is indicated by a significant increase in the activity of the enzyme glutamyl transpeptidase.
- An increase in alkaline phosphatase activity indicates pathologies of the biliary organs.
- The function of the pancreas can be assessed by glucose levels in the blood and urine.
- Evidence of the biliary type of pancreatitis is an increase in the blood levels of cholesterol and transaminases (ALT and AST).
At the same time, a stool analysis is carried out: with this disease, it is very light with an oily sheen.
The initial diagnosis is made at the stage of visual examination of the patient, collection of anamnesis and palpation examination of the peritoneal cavity.
The test results are confirmed by instrumental diagnostic methods:
- Ultrasound reveals swelling of the pancreas, the presence of stones and concretions in the organs of the biliary system, focal or diffuse changes in the liver and pancreas.
- Computed tomography with the introduction of a contrast agent shows the slightest changes in the pancreas, liver, pancreatic and biliary ducts.
- MRI of the abdominal organs reveals inflammatory processes, the presence of stones, and changes in the biliary system.
- Endoscopic retrograde cholangiopancreatography is used to diagnose pathologies of the biliary and pancreatic ducts and stone formation.
Symptoms of the disease, results of laboratory and instrumental studies allow us to establish an accurate diagnosis and begin therapy.
Treatment of pathology
A disease such as biliary pancreatitis requires complex treatment. First of all, the provoking factor of pathological reflux of bile is eliminated. In the acute stage, surgery may be required to remove the stone from the duct. If minor stones are present, then special drug therapy is prescribed aimed at dissolving and removing stones from the gallbladder.
Treatment methods for biliary-dependent pancreatitis include therapy aimed at eliminating pain. In this case, antispasmodics and analgesics are used. They are infused intravenously in a hospital setting or prescribed in tablet form. In the acute stage of the disease, choleretic drugs are not used, otherwise the pathology can only worsen.
To improve pancreatic function, enzyme group drugs are prescribed. These include: Creon, Mezim, Pancreatin, etc. Such medications compensate for the insufficient production of active substances by pancreatic tissues, resulting in improved digestion. The medications are prescribed for a long term. However, as health improves, they are gradually canceled.
If there is excessive production of hydrochloric acid by the cells of the gastric mucosa, treatment is supplemented with proton pump blockers. These include: Omeprozole, Nolpaza, Emanera, etc. This line of products helps prevent hydrochloric acid from being produced in excessive quantities.
When biliary-dependent pathology is present, drug therapy plays only a secondary role. Proper nutrition is very important. During the acute period, it is better to generally fast, while drinking a sufficient amount of liquid with the exception of soda, which can lead to spasm of the sphincter of Oddi. As a result, the course of symptoms will only worsen.
In the chronic form, medications are prescribed that help the flow of bile. These are herbal medicines, for example Hofitol based on artichoke extract. This drug allows you to gently expel bile, preventing its pathological concentration.
Treatment of biliary pancreatitis
Biliary-dependent pancreatitis is a secondary disease, as it occurs against the background of problems of the organs of the hepatobiliary system. This determines the features of complex therapy of the disease.
Diet and general recommendations
The most important element of treatment is diet No. 5. It involves reducing the load on the pancreas and liver during digestion, which is achieved by a minimum content of fats and fast carbohydrates in the diet.
A diet for biliary pancreatitis requires frequent meals of small portions of food, which is steamed or boiled.
The diet must be balanced and contain the required amount of vitamins and microelements, for which:
- during periods of exacerbation, pureed vegetable and meat dishes and pureed soups are recommended;
- among vegetables, beets, zucchini, squash, carrots are preferable; white cabbage is prohibited;
- Only lean meats (veal, rabbit, turkey) are consumed boiled or steamed; chicken is cooked after removing the skin;
- even during the period of remission, raw vegetables and fruits (non-acidic) are eaten without peeling;
- You can drink weak black or green tea, low-mineralized still water, juices, compotes;
- porridge (buckwheat, wheat, rice, oatmeal) is prepared in water, and milk is added during remission.
Patients should not drink coffee and alcoholic beverages; it is necessary to exclude canned food, marinades, various pickles, sweets and spices.
Drug therapy
Treatment of inflammation includes several stages:
- pain relief;
- therapy of primary diseases;
- treatment of pancreatitis;
- normalization of the patient's condition.
Since acute biliary pancreatitis is accompanied by severe pain, painkillers are prescribed (Sedalgin, Ibuprofen, Diclofenac). If the pain does not decrease, narcotics (Tramadol) are used.
The sooner a patient consults a doctor, the more likely he is to eliminate all the negative consequences of this serious disease.
To relieve spasms in the biliary system, antispasmodics (No-Shpa, Spazmalgon) are used; herbal preparations (Hofitol) help ensure the outflow of excess bile.
The decrease in the production of digestive enzymes is compensated by prescribing enzyme agents (Pancreatin, Festal, Mezim). Taking Ranitidine or Omeprazole will help reduce hydrochloric acid levels.
Small cholesterol stones are dissolved with Ursosan or Henochol, and Allochol and Holosas enhance the motility of the biliary organs. These remedies are used for a long time. They are contraindicated for kidney disease, stomach ulcers, and pregnancy.
Surgery
The movement of stones through the bile ducts causes severe pain. Sometimes, besides surgery, there is no other way to relieve a person from suffering.
Small stones are broken up with ultrasound or laser radiation, which does not prevent subsequent stone formation.
The presence of stones with a diameter of more than 3 cm requires surgical intervention. The least invasive methods are:
- Laparoscopic cholecystectomy, when punctures are made in the abdominal wall and an endoscope and instruments are inserted through them to remove the gallbladder along with stones. The operation is performed under video control.
- Biliary stenting is recommended for blockage of the bile ducts. Using the thinnest stents, the passage is widened, which ensures unhindered removal of stones.
Carrying out such procedures saves the patient from further relapses. Postoperative recovery takes 1-3 weeks. Subsequently, specialist supervision and strict adherence to his recommendations are necessary.
Folk and alternative methods
Chronic biliary-dependent pancreatitis can be treated with medicinal herbs from which teas are prepared:
- St. John's wort has a choleretic effect and is included in liver preparations;
- dandelion roots stimulate the production of bile and its evacuation;
- goldenrod leaves and flowers can dissolve gallstones;
- Wormwood has an antispasmodic effect, suppresses inflammation, and dissolves stones.
You need to drink herbal tea for at least 4 weeks. Folk remedies often have contraindications, so you should consult a doctor before taking them.
An alternative to drug therapy is juice treatment, for which freshly squeezed vegetable juices are used. They are diluted with water in a ratio of 1:1 or 2:1. Cucumber, pumpkin, beet, and carrot juices can be drunk individually or mixed into cocktails.
Acupuncture and acupressure give positive results. These procedures not only relieve inflammation of the gland, but also improve the general condition of the gastrointestinal tract.
Symptoms of the disease
Biliary-dependent pancreatitis manifests itself with a number of symptoms. The most characteristic symptom is pain in the abdominal cavity, which can be diffuse. Discomfort often affects the left and right hypochondrium. Pain occurs when eating certain foods that are irritating. These are fatty, fried, smoked, spicy dishes.
For symptoms of hepatitis, characterized by the presence of yellow sclera and skin, it is necessary to determine the absence of blockage of the bile duct with a stone. Biliary pathology has certain symptoms similar to other gastrointestinal pathologies. A sick person often feels the urge to defecate. In this case, the stool is liquid with a characteristic consistency. Undigested food particles may be present.
With this type of pancreatitis, vomiting often occurs. It may be accompanied by heaviness in the stomach and pain that resembles a spasm. Long-term lack of appetite provokes weight loss. Liquid stool, which accompanies a sick person every day, leads to impaired absorption of fats and beneficial microelements.
The skin becomes yellow. The difference between biliary lesions and other types of pancreatitis of different etiologies is an increase in body temperature and the constant presence of nausea. Other symptoms of pathology may be joint pain, general poor health, weakness and the addition of a depressive disorder.
Even small portions of food can cause disgust and nausea. The occurrence of biliary pancreatitis, the symptoms of which are so pronounced that they require urgent medical intervention, can be primary or secondary. The pathology sometimes becomes chronic with a long, severe course.
When making a diagnosis, it is important to exclude nonspecific ulcerative colitis, inflammatory processes in the stomach and liver pathologies. The disease is determined using abdominal ultrasound and endoscopic examination.
Complications of the disease
Untimely contact with a specialist, neglect of medical recommendations, dietary violations are the main causes of complications.
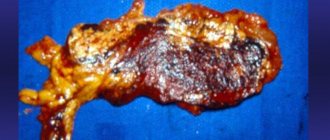
Progressive inflammation destroys gland cells and reduces its secretory functions. The production of digestive enzymes and hormones decreases, causing a condition called pancreatic insufficiency. The consequences are serious pathologies:
- renal and liver failure;
- peritonitis with subsequent blood poisoning;
- diabetes;
- jaundice;
- cysts and tumors;
- pancreatic necrosis.
Metabolism is gradually disrupted, and general intoxication of the body develops.
Prognosis and prevention
People with biliary chronic pancreatitis need to follow diet No. 5 for life, periodically see a doctor, and undergo sanatorium treatment. Compliance with all prescriptions prolongs periods of remission even after cholecystectomy (removal of the gallbladder), which is considered a favorable prognosis.
Complications, especially necrotic ones, concomitant cirrhosis of the liver, and chronic diseases of other organs often lead to death.
To prevent pancreatitis, it is necessary to follow the following preventive measures:
- do not overeat;
- reduce consumption of fatty, fried, spicy foods;
- do not abuse sweet and starchy foods;
- eat more vegetables and fruits;
- give up alcohol.
At the first signs of disturbances in the functioning of the digestive organs, consultation with a gastroenterologist is necessary.
Prevention
Currently, secondary prevention of the disease is very developed in medicine. In order not to cause relapses and progression of the disease, the patient must adhere to the recommendations of the treating doctor. To prevent biliary-dependent pancreatitis, the patient must follow these rules:
- strictly follow a diet;
- undergo regular treatment aimed at preventing the formation of gallstones;
- if necessary, surgical sanitation - cholecystectomy, papillosphincterotomy.
To completely prevent the occurrence of pathology, a person needs to maintain a healthy lifestyle, stop drinking alcohol, monitor their diet, not get carried away with physical activity, and undergo timely examination.
Встречаются только в пределах полного разврата, проверенные индивидуалки Владивостока, фото свои, не типаж - yesvladivostok.ru. Если говорить конкретно, то с проститутками можно заняться не только классическим сексом, но и всем, чем пожелаете. Красивые проверенные индивидуалки Владивостока, сладкие и ухоженные, они такие активные и молоденькие, что ты не устоишь перед ними. Они ждут твоего звонка.