Inflammation of the pancreas, or pancreatitis, is considered a serious medical and social problem. It is diagnosed quite often: the incidence of this pathology is quite high and amounts to up to 40-50 people per 100 thousand population, and most often able-bodied people suffer.
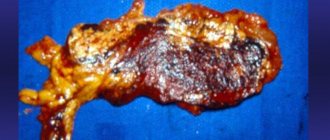
A quarter of patients with pancreatitis have destructive forms of the disease, accompanied by dangerous complications, the mortality rate of which reaches very significant rates. Therefore, timely diagnosis of pancreatitis is of great importance. A disease identified in the initial stages of destruction of the pancreas can still be successfully treated, preventing the pathological process from spreading, becoming chronic or affecting other internal organs.
Study of the content (activity) of pancreatic enzymes in blood and urine
Determination of amylase and isoenzymes in blood and urine
Determination of amylase levels in blood and urine is the most common diagnostic test. The low sensitivity of amylase determination in blood and urine is associated with the short duration of hyperamylasemia and hyperamylasuria in pancreatitis. Thus, the level of blood amylase begins to increase after 2-12 hours from the onset of exacerbation of the disease, reaches a maximum after 20-30 hours, and normalizes after 2-4 days with a favorable course of the disease. The amylase content in the urine begins to increase 4-6 hours after the onset of the disease, and after 8-10 hours, according to some reports 3 days, it can already return to normal. In severe exacerbation of CP, amylase activity can be “depleted” to normal and subnormal values.
Determining amylase levels in urine is more informative than in blood, since hyperamylasuria is more persistent than hyperamylasemia. The availability of urine allows the study to be repeated many times and therefore even a slight increase in the indicator can be detected. More sensitive than the amylazuric test is the calculation of uroamylase flow rates, when urine collected at certain periods of time before and after a food load is examined.
The sensitivity of these flow rates for HP is 49-73%.
- To increase the sensitivity of studying the level of amylase in the blood and urine of A.I. Khazanov recommends studying them on the first day of hospital stay for patients with chronic pancreatitis (CP), then at least twice after instrumental studies, as well as at the time of intensification of abdominal pain.
At the same time, in his opinion, the sensitivity of the test increases from 40 to 75-85%.
There is no level of amylase in the blood that is pathognomonic for pancreatitis. Due to the significant reserve of the enzyme in acinar cells, any violation of their integrity or the slightest difficulty in the outflow of pancreatic secretions can lead to a significant release of amylase into the blood, even with mild pancreatitis. On the contrary, with severe destruction of the organ parenchyma, hyperamylasemia may not be detected. Thus, in some cases there is no direct connection between the severity of pancreatitis and amylasemia.
- To increase the specificity of the study of amylase in the blood, it is necessary to determine not the total content of the enzyme, but pancreatic isoamylase.
In healthy people, p-amylase accounts for up to 40% of total serum amylase, the remaining 60% is represented by salivary isoamylase. In chronic pancreatitis, this ratio changes: pancreatic isoamylase accounts for 75-80% of total blood amylase.
- Determination of pancreatic isoamylase activity is especially important in CP in patients with normal levels of total amylase.
- An increase in the indicator indicates an exacerbation of CP, and a decrease indicates exocrine pancreatic insufficiency.
In general, the specificity of determining pancreatic amylase in CP does not exceed 88.6% with a sensitivity of 40-96.9%.
Treatment of acute and chronic pancreatitis
If a person encounters acute pancreatitis for the first time, treatment is quite simple. On the first day, you must refuse all food, replacing it with water. You need to drink often and a lot. It is better to apply a heating pad with ice to the pancreas area, this will relieve swelling and discomfort. For severe pain, medications containing narcotic substances may be prescribed.
After a fasting session, the patient needs to get out of this state and begin to gradually eat food. To do this, the doctor must create the right diet, adherence to which is a prerequisite. If there is sufficient damage to the pancreas, the patient is prescribed surgery.
When treating chronic pancreatitis, you must adhere to a diet. If a person fulfills all the conditions set by the doctor and monitors his diet, then pancreatitis will not bother him. For patients who have pancreatitis, the first thing they need to do is monitor their diet.
Serum lipase
The method for determining serum lipase is also not sensitive and informative enough. Data on the duration of hyperenzymemia. It is impossible to determine the severity of the current exacerbation of pancreatitis and the immediate prognosis based on serum lipase levels. Hyperlipasemia is recorded in 60% of patients with diseases of the hepatobiliary system, intestinal obstruction, renal failure, prostate cancer and other non-pancreatic diseases.
- More specific is a decrease in the level of lipase in the blood in relation to pancreatic fibrosis, as an outcome of CP and cystic fibrosis.
Diagnosis of the disease
To establish an accurate diagnosis, laboratory tests are necessary:
- a biochemical blood test allows you to see the whole picture of the disease;
- assessment of water and electrolyte balance helps to see a deficiency of calcium, potassium and sodium in the patient’s blood;
- A general blood test allows you to determine the presence of inflammation;
- general urine analysis. If there is an excess of amylase in the body, then this indicates this disease;
- coprogram is a method used for childhood pancreatitis and allows one to determine the degree of enzyme production by the child’s pancreas to determine the quality of processing of food particles;
- Stool analysis is used to determine the diagnosis of chronic pancreatitis in children. If starch, fats and protein fibers that have not been processed by the body are found in stool particles, then the disease is confirmed.
In addition to laboratory methods for determining the disease in adult patients, the diagnosis of pancreatitis also involves instrumental methods.
These methods allow you to visually see the pancreas.
- Ultrasound examination is considered indispensable in making a diagnosis. With its help, the pancreas is visualized.
- X-ray examination. It is used to determine the presence of stones in the pancreas.
- CT scan. A very capacious method that makes it possible to obtain information about the size of the gland and the presence of fluids in the pleural cavity. The method is applicable only in the largest clinics due to its considerable cost.
- Laparoscopy. The method is applicable in a well-equipped operating room, where the affected organ is examined and the extent of the pathology is determined. This diagnostic method is used in particularly advanced cases.
- Endoscopy. With this method, internal organs are visualized using a video camera. The degree of organ pathology is determined. A contrast agent is injected into the body and the level of patency of the bile ducts and pancreatic ducts is determined using radiography. It is necessary to administer a contrast agent with caution, as it itself can become a provocateur of another exacerbation
Serum elastase 1
The activity of this enzyme in the blood increases in chronic pancreatitis earlier than the level of other enzymes and lasts longer.
- Determination of elastase 1 activity is considered the “latest” sensitive test for diagnosing exacerbations of CP, since elevated blood levels persist for 8-10 days after the attack. During this period, the activity of elastase 1 in the blood was increased in 100% of patients, the level of lipase in 85%, pancreatic isoamylase in 43%, and total α-amylase in 23% of patients.
However, there is an opinion that the specificity of hyperelastasemia does not correspond to the degree of destruction of pancreatic tissue and does not have much diagnostic value for functional failure in patients with long-term CP.
Rehabilitation
During periods of remission, patients must adhere to the correct work and rest regime. Drinking alcohol and smoking is strictly prohibited. In case of stable remission, sanatorium-resort treatment at balneological resorts is indicated. You can use hydrocarbonate mineral water. Physiotherapeutic procedures are possible only with stable remission.
In cases of acute pancreatitis, disability is most often prolonged. It is connected not only with the patient’s well-being, but, to a greater extent, with the disappearance of pathological symptoms. Sometimes further employment through VKK is required. Such patients are contraindicated to work where physical exertion is great, and also where there are obstacles to diet, and they should not come into contact with poisons.
- How is pancreatitis diagnosed?
- Chapter 3. Surgical treatment of chronic pancreatitis (historical review)
- How to cure gastritis and pancreatitis. Gastritis and pancreatitis at the same time
- Voskresensky's symptom in acute pancreatitis
Assessment of exocrine pancreatic function
Tests to assess exocrine pancreatic function may be required to support the diagnosis of CP. They are almost always combined with ultrasound, x-ray and other studies, but can also be used independently for diagnostic purposes.
They can be divided into two groups: tests that require the insertion of an intestinal tube, and non-invasive tests without tubes. The latter have clear advantages in terms of patient comfort and risk and are also less expensive than probe tests. Unfortunately, there is no probeless test that has been successfully used as a standard method; all of them have both insufficient sensitivity and specificity. Almost all of these tests are based on determining the reduced secretion of pancreatic enzymes, however, due to low sensitivity, they are effective only with a very significant decrease in enzymatic secretion.
Carrying out probe and probe-free methods for determining the exocrine function of the pancreas is not mandatory for every gastroenterology department; in a particular case the necessary choice must be made. At present, it is probably reasonable to strive for a range of imaging tests, together with the Lund test and one non-invasive study. In such cases, imaging tests should be performed first, followed by functional tests in patients with suspected but not confirmed CP.
Probe methods
Direct probe method - secretin-pancreozymin (secretin-cholecystokinin) test.
In general, if all necessary technical conditions are met, the diagnostic accuracy of the method is extremely high; The sensitivity and specificity of the method are more than 90%. Most scientists recognize the role of this test as the gold standard for determining disorders of the exocrine function of the pancreas; some of them believe that the direct probe method is mandatory when diagnosing CP. Using the test, it is impossible to carry out differential diagnosis with other diseases of the pancreas, since with pancreatic cancer, cystic fibrosis and other diseases of the pancreas, pathological results of this test are recorded in 75-90% of cases.
Interpretation of the results of a probe study , identification of pathological types of pancreatic secretion (according to N.A. Skuya):
- Hyposecretory – decreased production of enzymes and bicarbonates with a normal volume of secretion. This type is characteristic of diffuse fibrosis of the pancreas (late stages of CP), cystic fibrosis, and is less commonly detected in pancreatic cancer.
- Hypersecretory - normal or increased volumes of secretion and bicarbonate flow, increased enzyme activity. This type is characteristic of initial inflammatory processes in the pancreas without signs of acinar cell atrophy and severe fibrosis. It is observed in the initial stages of CP, with a short-term and slight delay in the outflow of pancreatic secretions (with duodenal ulcer, short-term spasm of the sphincter of Oddi, etc.).
- The obstructive type is divided into 2 subtypes:
- lower block - a decrease in the volume of secretion at a normal concentration of bicarbonates and enzymes, which leads to a decrease in their flow rate. Characteristic of pancreatitis that has developed as a result of processes that impede the outflow of pancreatic secretions (persistent spasm of the sphincter of Oddi, papillitis, tumors of the Vater's papilla or head of the pancreas, obstruction of the gastrointestinal tract with a calculus);
- upper block - decreased secretion volume, increased enzyme concentration (but their flow rate is still reduced), normal bicarbonate content. This option indicates swelling of the pancreas and is characteristic of edematous pancreatitis (AP, exacerbation of CP).
Ductular - decreased secretion volume, normal enzyme production, sharp increase in bicarbonate concentration. Perhaps such changes are associated with inflammation of the ducts and impaired bicarbonate reabsorption.
The disadvantages of the method include the need for duodenal intubation, which is burdensome for the patient, the large amount of work of the laboratory assistant, the high cost and low availability of pancreatic stimulants. Thus, the cost of the secretin-pancreozymine test in the USA is $610, which is comparable in cost to CT and MRI.
Indirect probe method (Lund test)
The fact that the Lund test, developed in 1960, is still used in most gastroenterological laboratories indicates its general acceptance; it has been around longer than any functional test designed to routinely assess RV function. The sensitivity of this test is 90% in patients with CP. Individual false-positive results may be detected in patients with small intestinal malabsorption, ciliacia, gastrostomy, and diabetes mellitus. However, depending on the degree of exocrine pancreatic insufficiency in CP, the sensitivity of the test ranges from 66-94%.
- The Lund test is less sensitive in the early stages of exocrine pancreatic insufficiency.
The Lund test is cheaper, easier to perform, and more convenient for the patient. The disadvantages of the method include the need for duodenal intubation, the inability to determine the volume of secretion and concentration of bicarbonates, the influence on the test results of intraduodenal acidity and endogenous secretion of hormones from the duodenum.
Tubeless methods for diagnosing exocrine pancreatic insufficiency
Indirect methods without duodenal intubation are based on the oral administration of specific substrates for pancreatic enzymes. After the interaction of the latter with pancreatic enzymes, cleavage products are determined in urine and/or blood serum, the quantity of which is used to judge exocrine pancreatic insufficiency.
What are the preventive measures for gastrointestinal diseases?
To prevent this disease, you must adhere to proper nutrition. The diet should include all necessary vitamins and microelements. Be sure to eat fruits and vegetables. The restriction includes fatty and fried foods; you should avoid excessively salty and sweet foods. Avoid carcinogenic substances, preservatives and other chemical additives.
Treatment measures for pancreatitis
Pancreatitis is a life-threatening pathology, so treatment should only be prescribed by a doctor.
If we are talking about acute pancreatitis, the patient must be hospitalized in a surgical hospital. For the first three days, it is necessary to observe fasting: to the point that all the contents of the stomach are removed by a tube. An ice pack is applied to the abdomen and bed rest is prescribed. This classic formula is called “cold, hunger and rest,” and it is the starting point for treatment for both acute pancreatitis and exacerbations of chronic pancreatitis.
Of course, in the first case such measures are not limited. To reduce pain and restore normal outflow of pancreatic juice, antispasmodics are prescribed. Since the pain can be very severe, narcotic analgesics are sometimes used. To reduce the activity of the pancreas, somatotropin antagonists are prescribed, for example, octreotide or lanreotide, and for associated bleeding, somatostatin or terlipressin.
Depending on the patient’s condition, they resort to symptomatic treatment to correct certain changes in his body. May be prescribed:
- drugs that normalize blood pressure;
- means that support normal heart function;
- antibiotics for purulent inflammation, etc.
To remove toxic inflammatory products from the blood, infusion therapy (so-called droppers) is used. If pancreatic necrosis develops, the patient is operated on to remove dead areas of the pancreas.
In case of exacerbation of chronic pancreatitis, as already mentioned, the “cold, hunger and rest” regime is also recommended in the first three days. After this period, if your condition allows, you can start eating. At first - well-cooked porridges, jelly, pureed soups. Gradually it is allowed to switch to solid food.
The diet should contain a lot of protein, preferably milk or soy. It is recommended to limit the consumption of products with refractory animal fats (pork, lamb), but vegetable and milk fats are not prohibited. Moreover, it is not advisable to choose low-fat dairy products. Fatty desserts, peanut butter and other products of this kind are not only allowed, but even recommended (subject to the use of enzymes and normal tolerance to such foods). Alcohol is strictly prohibited. You cannot eat sour, fried, smoked, salty foods on an empty stomach, or start your meal with fatty broths rich in extractive substances.
Meanwhile, not only diet is necessary, but also medication. To relieve pain, it is recommended to take analgesics and antispasmodics. Pancreatic enzymes also have an analgesic effect - they provide rest to the affected organ[5] during meals. Enzyme preparations are prescribed on an ongoing basis for exocrine pancreatic insufficiency. They restore normal digestion, allowing all necessary nutrients to be absorbed. And to maintain their effect and restore a normal environment in the duodenum, H2 blockers, or proton pump inhibitors, are prescribed, which reduce the acidity of gastric juice.
Preparation with pancreatic enzymes
Preparations containing pancreatic enzymes have been around for quite some time. But thanks to their modern form, and these are microspheres, or microgranules, with a diameter of up to 2 mm, maximum effectiveness of these drugs is possible.
Mikrazym ® [6] is a product containing lipases, proteases and pancreatic amylases of animal origin, as well as enzymes that digest fats, proteins and carbohydrates, respectively. Enzymes are placed in microgranules with an acid-resistant shell, which protects them from inactivation in the stomach. In turn, microgranules are “packed” into capsules containing 10,000 units or 25,000 units of active enzymes.
Once in the stomach, the gelatin capsule dissolves. Under the influence of peristaltic movements, microgranules are evenly mixed with food and gradually enter the intestinal lumen. In the alkaline environment inside the duodenum, their membrane dissolves and the enzymes begin to “work.” Maximum enzyme activity is observed within 30 minutes after eating.
You need to take Mikrasim® during every meal - with the exception of snacks that do not contain fat (vegetable salad without dressing, fruit juice, tea with sugar without milk, etc.). Usually one capsule is enough with meals, as it contains a sufficient amount of enzymes that help normalize digestion. If it is difficult to swallow the capsule, you can open it, but under no circumstances should you chew or otherwise crush the microgranules: this will destroy the protective shell and the enzymes will lose their activity.
The main indication for the use of Mikrasim® capsules is chronic pancreatitis without exacerbation. In addition, the drug is used for exocrine pancreatic insufficiency of any origin: due to cystic fibrosis, after operations on the pancreas, after resection of the stomach or small intestine. Healthy people can use Micrasim® to reduce the stress on the pancreas when overeating, especially when eating fatty foods.
Mikrasim® is contraindicated in acute pancreatitis and exacerbation of chronic pancreatitis, as well as in case of individual intolerance.
The drug is included in the list of Vital and Essential Drugs and is available without a prescription.
Bentiramide test (NBT-PABA test)
This probeless test is based on the fact that N-benzoyl-L-tyrosyl-p-aminobenzoic acid (NBT), which is essentially a synthetic, chymotrypsin-specific tripeptide, is hydrolyzed by this enzyme to form p-aminobenzoic acid (PABA). The isolated PABA is absorbed, conjugated in the liver and excreted in the urine, where it is determined. The actual estimate of PABA in urine reflects the amount of chymotrypsin excreted by the pancreas.
The sensitivity of the method is 83%, and the specificity is 89%. False-positive results were observed in a quarter of patients with diseases of the small intestine, renal failure, gastric resection, celiac disease, Crohn's disease, impaired liver function, renal failure, and diabetes mellitus.
- The fundamental disadvantage of non-invasive methods is the weakening of their sensitivity in cases of moderately severe exocrine pancreatic insufficiency.
Despite these limitations, the NBT/PABA test can claim the greatest significance and stability among indirect methods.
Qualitative scatological research
A qualitative scatological study is carried out while patients follow a standard diet (for example, the Schmidt diet, including 105 g of protein, 135 g of fat, 180 g of carbohydrates) provided that multienzyme drugs are not used during this period of time.
- The criteria for exocrine insufficiency are an increased content of neutral fat and soap in the feces with a slightly changed content of fatty acids. An increased content of muscle fibers indicates the presence of creatorrhoea.
Quantitative determination of fat in feces
Normally, after taking 100g of fat with food, up to 7g of neutral fat and fatty acids are released per day. An increase in the amount of fat indicates disorders of the digestion and absorption of fat, most often of pancreatic origin. Determining the severity of steatorrhea is used as a simple and reliable indicator of severe exocrine pancreatic insufficiency. This test is widely used. Its reliability decreases with incomplete (incorrect) stool collection and against the background of an inadequate diet, especially in outpatients. The test is nonspecific for a number of diseases, which does not allow it to be used to determine the pancreatic nature of steatorrhea. The test data almost always does not fit into normal values in cases of damage to the ileum and bacterial contamination of the small intestine.
Determination of fecal elastase 1
Over the past decade, the enzyme immunoassay method for determining elastase 1 in the stool of patients with CP has become widespread. The sensitivity of the elastase test in patients with severe and moderate exocrine pancreatic insufficiency is close to that of the secretin-pancreozymin test, and according to most foreign researchers it is 90-100%, and in mild cases - 63%, specificity - 96%.
This method is simple, fast and inexpensive, has no restrictions in application, and allows us to determine the state of the exocrine function of the pancreas at earlier stages than before.
- The method in many cases provides diagnostic sensitivity and specificity close to those of direct methods for assessing the exocrine function of the pancreas.
Differential diagnosis of pancreatitis
All symptoms of the presence of the disease in the body are signs of an “acute abdomen”. There is a need to differentiate pancreatitis from various pathologies of the abdominal cavity:
- perforated ulcer. The difference with pancreatitis is the feeling of “dagger pain” in the case of an ulcer. There is no vomiting with an ulcer. A patient with an ulcer cannot bear to move, while a patient with pancreatitis rushes about in pain. The final diagnosis is based on laparoscopy or ultrasound;
- acute cholecystitis. These two pathologies are difficult to distinguish. Sometimes pancreatitis accompanies cholecystitis. The only difference is the presence of pain on the right side in a patient with cholecystitis, which radiates to the right shoulder;
- acute intestinal obstruction. It differs from the nagging pain of pancreatitis by cramping pain plus intestinal seething;
- mesothrombosis. Elderly people with cardiovascular diseases are susceptible. Pathologies are not related to nutrition;
- myocardial infarction. All doubts about the diagnosis are dispelled by an electrocardiogram.
Tumor markers
An increase in the level of tumor markers (CA19-9, CEA) above the value acceptable for inflammation is an indirect sign of the transformation of CP into pancreatic cancer. These tests are used for the differential diagnosis of pseudotumor forms of pancreatitis. Patients with pancreatic cancer have high levels of carcinoembryonic antigen (CEA), but its standard measurement lacks specificity; positive results are observed with other tumors and with exacerbation of CP. The sensitivity and specificity of determining CA19-9 in the diagnosis of pancreatic cancer ranges from 70-95% and 72-90%, respectively. Although most pancreatic cancers cause elevated serum levels of CA19-9, the specificity of this tumor marker never approaches 100%.
Chronic pancreatitis and its causes
There are two types of chronic pancreatitis: primary and secondary. In practice, secondary pancreatitis is a fairly common disease. As a rule, other diseases of the gastrointestinal tract lead to inflammation of the pancreas.
The main causes of chronic pancreatitis:
- Improper functioning of the gastrointestinal tract;
- The patient neglects the necessary diet and eats fried, fatty, spicy foods.
- Alcohol abuse.
In addition to the main classification, there are a number of other series. For example, the Marseilles-Roman classification. According to which the following types of disease are distinguished:
- Calcific inflammation is the most popular form. In this case, damage to the pancreas can be characterized as the formation of individual points that differ in size. The ducts that leave the pancreas become clogged and often die.
- Obstructive inflammation usually affects the entire pancreas, with obstruction occurring in the largest ducts. This disease requires immediate surgery. Since local treatment methods sometimes do not give a positive result.
- Pancreatic fibrosis is a condition in which the organ cannot perform the function of producing secretions.
Clinical blood test
With an exacerbation of CP, a general blood test may reveal leukocytosis, a shift of the formula to the left, neutrophilia, and accelerated ESR syndrome. During treatment, there is a rapid, clear reduction in leukocytosis; somewhat later, ESR numbers normalize, which is one of the favorable clinical signs.
- Long-lasting leukocytosis with a shift to the left and elevated ESR numbers can serve as one of the nonspecific markers of the development of complications.
In patients with CP with exocrine insufficiency, leukocytosis is rarely detected. Moreover, moderate leukopenia is characteristic, indicating the presence of trophological deficiency. In this case, long-term indicators of accelerated ESR may be observed, which is most often due to dysproteinemia. In patients with severe forms of malabsorption syndrome, signs of iron deficiency, B6-, B12- and folate deficiency, and more often, mixed anemia may be observed.
How to determine the acute form?
Diagnosis of acute pancreatic inflammation in adults includes a visual examination. There are several clinical signs by which an experienced doctor can almost accurately identify the disease. These characteristic symptoms even received names after their discoverer:
- Gray-Turner. Bluish spots are detected on the skin in the epigastric zone.
- Cullen. Bluish spots near the navel indicate the accumulation of breakdown products and toxins due to the failure of fats to be broken down.
- Voskresensky. With pancreatitis, the aorta (its pulsation) under the sternum is practically not palpable.
- Shchetkin-Blumberg. Use your entire palm to gently press on the abdominal wall. In a normal state, a person does not experience any particular discomfort. But if there is pathology in the pancreas, the patient screams sharply.
- Razdolsky. Identification of the painful area by palpation of the upper part of the peritoneum.
- Kertom. Thanks to the method, the so-called pancreatic zone is specifically palpated.
If several similar symptoms are present at the same time, even a visual examination gives a classic clinical picture of acute inflammation of the pancreas. And when there is very little time for analysis and hardware research, this method sometimes plays a decisive role.
Blood chemistry
A reduced level of total blood protein, albumin, transthyretin, transferrin, ferritin and other proteins characterizing the visceral pool of proteins and the degree of trophological deficiency may be observed. Dysproteinemia is recorded, characterized by a decrease in the albumin-globulin ratio and a relative increase in α1-α2-globulins.
Elevated levels of blood transaminases, gammaglutamyltransferase, and lactate dehydrogenase are often recorded.
- An increase in bilirubin, mainly direct bilirubin, cholesterol and alkaline phosphatase is characteristic of the developed cholestasis syndrome, which may be due to a block of the common bile duct and the development of reactive hepatitis.
In patients with alcoholic CP, an increase in liver function tests in the blood may be due to independent liver pathology (toxic hepatitis, liver cirrhosis). Hypocalcemia is often observed, the degree of which can serve as one of the criteria for the severity of the disease. Hypercalcemia suggests the presence of hyperparathyroidism as a causative factor of CP.
© I.V. Maev, A.N. Kazyulin, A.A. Samsonov, Yu.A. Kucheryavyi. Chronic pancreatitis: (Algorithm for diagnosis and treatment tactics). A manual for general practitioners, therapists, gastroenterologists: A textbook. – M.: GOU VUNMTs MH and SR RF, 2006. – p.
The educational and methodological manual was developed by the staff of the Department of Propaedeutics of Internal Diseases of the Faculty of Medicine and Gastroenterology of the Moscow State Medical University (head of the department - Doctor of Medical Sciences, Professor I.V. Maev): Doctor of Medical Sciences, Prof. I.V. Mayev, Doctor of Medical Sciences, Prof. A.N. Kazyulin, Doctor of Medical Sciences, Prof. A.A. Samsonov, Ph.D., Yu.A. Curly. Edited by prof. I.V. Maeva.
Forecast
Chronic pancreatitis is a serious disease. However, if you follow the recommendations of the supervising physician for the prevention of exacerbations (compliance with dietary recommendations, preventive courses of treatment, etc.), chronic pancreatitis proceeds “calmly”, without frequent exacerbations and has a favorable survival prognosis.
If the diet is violated, alcohol intake, smoking and inadequate treatment, degenerative processes in the gland tissue progress and severe complications develop, many of which require surgical intervention and can be fatal.