In medical practice, reactive pancreatitis is usually called acute inflammation of the human pancreas. This happens in most cases with diseases of other organs of the digestive system. The symptoms of the disease are pronounced, can significantly worsen the patient’s quality of life, and also lead to serious consequences, sometimes incompatible with life.
Related articles:
Acute pancreatitis: symptoms, causes and treatment Exacerbation of chronic pancreatitis Pancreatitis: treatment with medications Pancreatitis in men: symptoms and treatment Correctly treating pancreatitis with herbs
Reactive pancreatitis, the symptoms and treatment of which we will discuss below in the article, is a fairly common disease that occurs in both men and women. When pathology appears, it is extremely important to consult a specialist in a timely manner. This will help avoid serious consequences and the disease becoming chronic.
Important! On our website you can find out what pancreatic pancreatitis is and how to treat it.
Why does pancreatitis occur?
Thanks to the pancreas, the human body produces enzymes that are essential for normal digestion and neutralization of stomach acid. Often the functions of the gland are disrupted under various influences. Most often, pancreatitis can develop against the background of the following pathologies:
- hepatitis A;
- cholecystitis;
- gastritis;
- various intestinal infections;
- damage to the digestive organs during operations or injuries;
- liver cirrhosis;
- infectious diseases of the gastrointestinal tract.
Important! You can learn about exacerbation of chronic pancreatitis here.
Reactive pancreatitis occurs more often in adults, this is explained by the presence of various provoking factors, which include:
- smoking;
- consumption of alcoholic beverages;
- excessive amounts of fatty foods in the diet;
- unbalanced diet;
- regular or incorrect use of certain medications.
Important! If you want to learn about how pancreatitis manifests itself in men and how to treat it, read with us.
Pancreatitis is much less common in children. In most cases, the causes of the disease in childhood are congenital pathologies and various disorders in the functioning of the digestive system.
Important! Often the disease develops against the background of congenital anomalies. In such cases, a person is forced to radically reconsider his lifestyle and diet.
Prevention
There are no special prophylactic agents for reactive pancreatitis. People are advised to completely give up bad habits, follow nutritional recommendations, and take medications only as prescribed by a doctor with strict adherence to dosage. In addition, the main thing is to promptly eliminate those gastrointestinal diseases that can cause the appearance of such a disease.
The prognosis of the disease with early diagnosis and treatment is favorable. In almost all cases, after starting therapy, all clinical manifestations quickly disappear. There is a possibility of relapse, but only if the diet for reactive pancreatitis is not followed.
Main manifestations of reactive pancreatitis
At first, the symptoms of the disease may be mild. The patient does not experience any particular discomfort, and does not pay attention to such manifestations as nausea, periodic bloating, and heaviness in the stomach. Such patients also rarely go to the doctor, attributing the manifestations of the disease to overeating, indigestion and some other factors.
Important! You can find out more about the first signs of pancreatitis here.
With further development of the disease, the symptoms of the disease worsen significantly. These may be the following signs:
- severe bloating;
- frequent belching with an unpleasant odor;
- feeling of heaviness and discomfort in the stomach;
- nausea and repeated vomiting;
- pain in the left hypochondrium and stomach.
Important! Find out in our article about the symptoms of pancreatitis in women.
Also, reactive pancreatitis is accompanied by a rise in high temperature, the patient experiences all the signs of intoxication - weakness, malaise, depression.
In addition, characteristic of this type of disease is the addition of signs of the disease that provoked pancreatitis. For example, with cirrhosis, the liver can be significantly enlarged in size, cholelithiasis causes sharp or aching pain in the right hypochondrium, food poisoning can cause high fever and diarrhea.
Important! If you detect the first signs of pathology, you should immediately seek qualified medical help. If not treated in a timely manner, the consequences of pancreatitis can be very negative.
Symptoms and clinical picture
The first symptoms of the disease appear 2-3 hours after exposure to the causative factor. The main manifestations are as follows:
- pain in the left hypochondrium, which can be girdling in nature and spreads to the back. When eating food, the pain intensifies;
- bloating with heartburn and belching;
- dyspepsia: nausea and vomiting. Vomit may contain bile and mucus. After vomiting, the pain intensifies.
If left untreated, intoxication syndrome develops. Patients ask what it is. This is a condition that develops due to the release of pancreatic enzymes into the blood and is characterized by increased temperature, pale skin, increased heart rate and decreased blood pressure. Patients with such clinical signs require hospitalization.
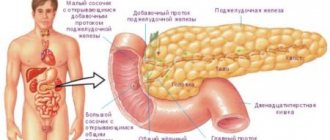
To understand the occurrence of the incident, let’s imagine the daily work of the pancreas. The main function of the organ is to produce pancreatic juice, intended for digesting food. The juice contains enzymes and bicarbonates; the substances create an alkaline environment that can completely neutralize acidic gastric juice. The created juice “floats” into the intestines through special ducts and, reaching its destination, interacts with the substances located there.
By reacting with products that accidentally end up in the pancreatic ducts, the juice begins to negatively affect the pancreas. The organ begins to digest itself, and inflammation begins. Enzyme receptors, not perceiving digestive enzymes, begin to intensify the production of reagents, as the body prompts: there are not enough enzymes.
Inflammation is due to the fact that the pancreatic ducts simply do not have an entrance to the intestine. The juice does not enter the intestines, remains at the site of origin, and the organ becomes ill.
Such pancreatitis always occurs in an acute form and does not become chronic. Chronic reactive pancreatitis awakens on its own, without external irritants.
Sometimes the tail of the gland can become enlarged - the stimulated work of the pancreas causes intensive division of cells rushing to fill the broken space. This has a negative effect on the patient's condition.
Often, while in hospital, a patient is prescribed various medications and procedures to ensure that reactive pancreatitis does not develop.
- hepatitis;
- gastritis;
- gallstones;
- hepatic cirrhosis;
- cholecystitis;
- bile duct dyskinesia;
- injury to organs located in the abdominal cavity;
- infection in the intestines.
A process that disrupts intestinal function can cause reactive pancreatitis. Only then is the disease diagnosed and treatment selected.
Risk factors
There are known groups of people with the possibility of getting inflammation of the pancreas more often than others. These include:
- smokers;
- alcoholics;
- people who prefer fatty foods in their diet;
- people who care little about nutrition and eat irregularly;
- patients taking medications despite contraindications.
If the patient seems to have a genetic predisposition to a type of disease, it is better to get rid of bad habits in time, before undesirable events develop.
The disease is dangerous due to its blurred clinical picture in the first days of its onset. The patient may complain of discomfort in the intestines, increased gas formation, flatulence and bloating, heaviness in the stomach after each meal. There is also bitter or rotten belching, hiccups, a bitter taste in the mouth and abdominal pain without clear localization. At first, the pain is subthreshold in nature, the patient relieves it with the usual analgesics.
On the second or third day, the pain intensifies and becomes clearly localized. The patient is restless, cannot find a comfortable position, and nothing can stop the attack of pain. Vomiting occurs, which can appear both at the height of the pain symptom and after it. Distinctive feature: vomiting does not bring any relief to the patient. The patient has a fever (body temperature rises to 38-39 C), weakness and sweating are noted.
Against the background of the above symptoms, there are signs of an underlying disease.
- Symptoms of gastric damage: pain in the epigastric region that occurs after eating or on an empty stomach. Hiccups and belching with reflux of gastric contents into the oral cavity, heartburn.
- Symptoms of damage to the duodenum: pain in the epigastric region, mainly on the left, radiating to the back and scapula. Pain occurs half an hour after eating or on an empty stomach at night, forcing the patient to wake up. Digestion and absorption disorders, weight loss, dyspeptic disorders (loose stools, flatulence).
- Symptoms of gallbladder damage: pain in the left hypochondrium and radiating to the left shoulder blade, occurring immediately after drinking alcohol or fatty, fried foods. Loose, frequent stools, steatorrhea (increased fat content in stool), flatulence.
- Symptoms of liver damage: swelling of the legs, abdomen, enlarged veins of the anterior abdominal wall, visible to the naked eye, enlarged liver. Weakness and malaise. Unpigmented feces, dark urine (beer-colored urine).
Diagnostics
Upon admission to a hospital, a diagnosis of the disease is carried out, which involves the following measures:
- Questioning the patient.
- Inspection by palpation.
- Laboratory blood tests.
- Stool analysis.
Important! Find out which doctor treats pancreatitis.
The specialist finds out the features of the course of the disease, the chronology of the onset of symptoms, and how acutely the signs of pathology manifested themselves. After examination by a doctor and receipt of laboratory test results, the patient is diagnosed and prescribed the necessary treatment.
Causes of the disease
Attacks of this type of pancreatitis occur more often in men than in women. They consume more junk food and strong alcoholic drinks, which leads to blockage of the pancreatic ducts and, as a consequence, pathology of the digestive tract. Here is a list of factors that can cause reactive pancreatitis in adults:
- prolonged stress;
- presence of bad habits (smoking, frequent drinking of alcohol);
- binge eating;
- consumption of unhealthy foods (fried, fatty, spicy, smoked foods, fast food, soda);
- long-term use of medications (hormonal, Metronidazole, Furosemide, NSAIDs);
- internal abdominal injuries, which are accompanied by rupture of the epithelium of the gland.
The problem may arise against the background of pathological processes in the gastrointestinal tract with:
- helminthiasis;
- blockage of ducts with gallstones;
- viral hepatitis;
- food poisoning, in particular, mushrooms, industrial and household poisons;
- liver cirrhosis;
- stomach ulcer or gastritis;
- chronic cholecystitis.
As a result of the appearance of all these factors, pancreatic enzymes begin to destroy pancreatic cells, an inflammatory process begins, as a result of which breakdown products enter the bloodstream. This is fraught with swelling of the gland and poisoning.
Treatment methods
Treatment of pancreatitis is complex and consists of the following methods:
- Drug treatment.
- Surgical intervention.
- Use of traditional medicine.
- Dieting.
Nutrition rules for pancreatitis
One of the most important aspects of the treatment of reactive pancreatitis is diet. At the first stages of the disease, the patient is recommended to drink only boiled water for several days. This is done in order to maximally relieve the pancreas and digestive organs, as well as remove accumulated toxins.
Important! It’s interesting to know: is it possible to eat watermelon if you have pancreatitis? Read our article.
In cases where the disease is not so pronounced, the patient is given a diet consisting of food low in fats and carbohydrates. Alcoholic drinks are strictly prohibited, and doctors also recommend excluding foods with strong tastes from the diet. This is explained by the fact that such dishes increase the production of enzymes, that is, they increase the load on the pancreas.
The best option for people suffering from pancreatitis is split meals. A person should eat small portions 5-6 times a day. This will minimize the load on the diseased organ. Dishes can be as follows:
- porridge without oil;
- vegetable soups;
- low-fat fermented milk products;
- steamed vegetables;
- baked apples;
- steam omelettes.
Important! Acute pancreatitis: symptoms, causes and treatment are described in detail in our article.
An important rule of diet is also to drink enough clean water. The amount of liquid and food is selected for each person, taking into account his individual characteristics and the severity of the illness.
There are often cases when a patient requires surgical intervention. An indication for surgery may be the formation of false cysts.
Another type of therapy is the administration of nutrients and vitamins through a vein. This treatment is carried out in conditions where the patient cannot eat on his own.
Important! What folk remedies I use for chronic pancreatitis, see here.
Use of medications
Treatment with medications involves the use of the following:
- Anti-bloating drugs - espumizan.
- Enzymes – mezim, pancreatin, creon.
- Agents that have an antispasmodic effect - no-spa, spasmalgon.
- Antibiotics – titracycline, Ormax.
- Painkillers - diclofenac, ketanov.
If a person is in serious condition, medications are administered through a vein. Droppers, the composition of which is determined by a specialist, quickly relieve the main symptoms of the disease and normalize the patient’s condition.
Treatment of pancreatitis in children also requires special attention. Therapy is carried out strictly in a hospital setting with adherence to diet and drinking regime. For patients in the younger group, medications of a certain group are used, which are selected exclusively by a specialist.
Important! Only a doctor can select medications and their dosage. Self-medication often provokes serious consequences and complications.
Traditional treatment
Treatment with folk remedies is often used at home. This type of therapy is mainly used as an auxiliary method. Popular recipes include the following:
- Freshly squeezed carrot and potato juice relieves the symptoms of the disease well. To do this, vegetables can be grated or minced. The juice is squeezed through a fine sieve or gauze. You need to drink this drink on an empty stomach for two weeks.
- Take a few fleshy leaves of the golden mustache and pour 500 ml of boiling water over them. The product should be simmered over low heat for 5 minutes, then cooled and strained. The medicine should be taken three times a day before eating.
- Herbal treatments are also often used. To prepare the decoction, you need to mix chamomile, plantain, calendula and corn silk, 1 tbsp each. l. Next, the plants are poured with one liter of boiling water and cooked over low heat for 10-15 minutes. Take the resulting decoction half a glass twice a day after meals.
- 200 g of viburnum berries are poured into 500 ml. boiling water The product is boiled for 5-10 minutes and then consumed as tea with the addition of a small amount of honey.
Important! More information about treating pancreatitis at home can be found here.
Pancreatitis is a common disease affecting the pancreas and digestive system. Reactive pancreatitis is one of the severe types of the disease, accompanied by pronounced symptoms. When this pathology develops, it is very important to begin timely treatment, which will help avoid many complications in the future.
Nutrition
Since the digestive system is disturbed, the patient needs to adhere to a gentle diet.
It is necessary to include in the diet:
- Crackers, preferably white bread.
- Lean meat broths.
- Boiled liver.
- Porridge: buckwheat or oatmeal.
- Compotes.
- Boiled vegetables.
- Mineral water: Essentuki, Borjomi.
Be sure to consume fermented milk products, but only those with low acid content.
Prohibited products:
- Sausages.
- Canned fish and meat.
- Spices and sweets.
- Sour fruits and juices.
- Chicken eggs.
- Fatty meats and fish.
Also read: Chronic pancreatitis symptoms and treatment
Remember, if you eat right and follow the recommendations of your doctor, you can quickly cure pancreatitis.
Chief gastroenterologist of the Russian Federation: “PANCREATITIS does not go away?! A simple treatment method has already healed hundreds of patients at home! To cure the pancreas forever you need...” Read more »
At home, you can prepare not only a tasty, but also a healthy drink . Take 200 grams of viburnum berries and pour boiling water over them. If you are not allergic to honey, then you can add 1 teaspoon to the drink and drink it instead of tea.
Now you know how to treat this disease. But remember, if you notice the first signs of illness, you must immediately consult a doctor.