Human bile plays an important role in the process of life. It tastes bitter, has a specific smell and characteristic color, and is important for the digestion of fatty foods. The secretory function belongs to hepatocytes. It is produced in the liver and stored until a certain point in the gallbladder. The role of bile in the digestion of food is enormous. It ensures a change in digestion from gastric to intestinal and minimizes the harmful effect of pepsin on the pancreas and its enzymes.
General information, composition, fractions
The bitter taste substance is green, brown and yellow. Its color is given by bile pigments (porphobilinogen, bilirubin), formed during the breakdown of red blood cells. Thanks to them, feces are colored in a specific color. The secretion emulsifies and breaks down fats, helping them digest and absorb. Promotes intestinal motility. The following types of bile are distinguished:
- Liver (young) is secreted directly into the intestines.
- The gallbladder (mature) is stored in the gallbladder and is secreted by it.
The composition includes main active and auxiliary substances. The main ones are primary and secondary bile acids. When combined with glycine and taurine, they form paired acids, which are considered “bile salts.” Excipients include bilirubin, phospholipids, proteins, water, bile pigments, mineral ions, and bicarbonates. The abundance of potassium and sodium ions contributes to the alkaline reaction of the secretion.
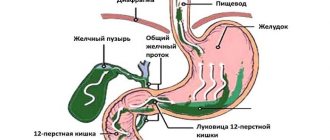
Bile flows from the gallbladder into the intestines.
The structure of bile has 3 fractions. Hepatocytes form the 1st and 2nd, bile duct epithelial cells - the 3rd. The 1st and 2nd fractions provide 75% of the total volume of the substance, performing a secretory function, the 3rd - 25%. The latter is formed due to the ability of epithelial cells to secrete digestive juice and the possibility of reabsorption of water and electrolytes from the common duct.
Bile acids
The composition of human bile includes two types of acids - primary and secondary. The former are secreted directly by the liver; these include chenodeoxycholic and cholic acids. The second ones - lithocholic, allocholic, deoxycholic, ursodeoxycholic, are formed in the colon from primary ones under the influence of microbial enzymes. Not all secondary acids participate in sufficient quality to influence physiological processes in the intestine, only deoxycholic acid. They are absorbed into the bloodstream, then the liver produces them again. All bile acid molecules contain 24 carbon atoms.
Functions in the digestive cycle
The functions of bile are diverse. Bile acids are surfactant compounds necessary for the solubilization of fat droplets. Before pancreatic enzymes break down fat, it must dissolve. The products of fatty hydrolysis are then absorbed by enterocytes via fatty acids. Enzymatic functions include:
- neutralization of the irritating effect of pepsin;
- fat emulsification;
- promoting the formation of micelles;
- stimulation of the release of intestinal hormones;
- promoting mucus formation;
- activation of gastrointestinal motility.
Secondary functions are absorptive and excretory. Bile in the body acts as an antiseptic in the intestines and helps in the formation of feces. It absorbs fats, fat-soluble vitamins and minerals, removes lecithins, cholesterol, toxic compounds, and medications. Salts of fatty acids normalize lipid metabolism. The antiseptic properties of the substance prevent the development of pathogenic flora.
Symptoms of the disease
Often, diseases associated with bile formation and bile secretion are formed based on the volume of secretion produced, its release into the small intestine, as well as the quality of the release. Usually, it is the insufficiency of bile formation and the return of secretions into the stomach that are the main causes of diseases of the gastrointestinal tract. The main ones include:
- Stone formation. Gallstones are formed when the composition of the secretion is unbalanced (otherwise known as lithogenic bile), when bile enzymes are severely deficient. The lithogenic properties of bile fluid manifest themselves as a result of the lack of a diet, when eating plant and animal fats in large quantities. Other reasons are endocrinological disorders, especially against the background of neurological disorders, disorders of fat metabolism in the body with a tendency to increase body weight, liver damage of any origin, and hypodynamic disorders.
- Steatorrhea. The disease occurs in the complete absence of bile or in bile insufficiency. Against the background of pathology, the emulsification of fats stops, they are formed unchanged along with feces and are excreted in the form of feces. Steatorrhea is characterized by a lack of fatty acids and vitamins in the body, when the structures of the lower intestines are simply not adapted to undigested fats in the food bolus.
- Reflux gastritis and GERD. The pathology consists of the backflow of bile into the stomach or esophagus in a noticeable volume. With duodenogastric and duodenogastroesophageal refluxes, bile enters the mucous membranes, causing their necrotization and necrobiotic changes. Damage to the upper layer of the epithelium leads to the formation of reflux gastritis. Gastroesophageal reflux disease (abbr. GERD) is formed due to damage to the esophageal mucosa against the background of an acidic pH in the esophagus. Bile penetrating into the esophagus provokes the formation of various variations of GERD.
When bile is formed, almost all organs close to the liver and gallbladder are involved. This proximity is due to the severity of pathologies with insufficiency or absolute absence of bile.
Considering the polyetiology of diseases due to disturbances in the processes of formation and release of bile fluid in the required volumes, comprehensive diagnostics are carried out, consultations with other specialists in the field in case of a burdened clinical history of the patient. In addition to a physical examination, studying the patient’s medical history and his complaints, palpation of the peritoneum and epigastrium, a number of laboratory and instrumental studies are carried out:
- esophagogastroduodenoscopy (to identify bile);
- ultrasonography (abdominal) (determining the diameter of the bile ducts at the time of eating);
- ultrasound of the liver, gall bladder and abdominal organs;
- dynamic echography;
- X-ray gastroscopy;
- gastrography with contrast;
- hydrogen test;
- endoscopic studies.
Endoscopic examinations allow the collection of stomach tissue and cavity contents for detailed study. Using the endoscopic method, doctors determine the degree of narrowing of the small intestine, the rhythm of peristalsis, possible congestion, atrophic metaplasia of the epithelium, and a decrease in the propulsive intensity of the stomach.
Bile secretion plays an important role in the body of any person, as well as warm-blooded animals. Bear bile (ursuholic acid) is especially important for the treatment of various diseases. Due to its complex composition, there are no similar substances in the world that could perfectly replicate all the components in one liquid.
Excess bile in the stomach is characterized by certain symptoms that can be independently identified:
- Belching. Having accumulated in the stomach, bile begins to interact with gastric juice, which leads to the formation and release of gases. As a result, heartburn may occur, and a yellow coating may appear on the tongue, because... bile has a yellowish color.
- Stomach ache. Bile has an irritating effect on the walls of the stomach, which can cause severe sharp pain in the epigastric region associated with inflammation.
- Diarrhea and vomiting. Bile acids exhibit toxic effects in the stomach, so the body strives to remove this biological fluid as quickly as possible.
- Bloating and feeling of heaviness. Prolonged presence of bile in the stomach causes the formation of gases, as a result of which the patient suffers from flatulence.
These symptoms not only cause severe discomfort, but can also lead to more serious illnesses.
We will talk about the structure of the gallbladder and its functions in one of the following articles on this site. For now, let us note one more important circumstance.
The cystic duct begins at the exit of the gallbladder and ends at the confluence with the common hepatic duct.
It is this duct that carries bile directly into the duodenum.
Bile contains many different substances. Its composition is such that it does not contain enzymes, as in other digestive juices from the gastrointestinal tract. Instead, it is mainly represented by bile salts and acids, which can:
- Emulsify fats and break them into small particles.
- Help the body absorb fat breakdown products in the intestines. Bile salts bind to lipids and are then absorbed into the blood.
Another important function of bile is that it contains broken down red blood cells. This is bilirubin, and it is usually produced in the body to get rid of old red blood cells rich in hemoglobin. Bile also transports excess cholesterol. It is not only a product of liver secretion, but also removes various toxic substances.
Which organ produces it?
The formation of bile in humans, called cholerosis in medicine, is a continuous process carried out by hepatocytes of the liver parenchyma. Liver cells produce a golden fluid that is isotonic with plasma with a pH of up to 8.6. Hepatocytes border bile capillaries, which collect into ducts. Together, the latter form a common duct between the liver and the gallbladder. Digestive juice moves along this path from the moment it is produced by hepatocytes until it enters the intestinal tract.
Every day our body produces 0.5-1 liters of bile. Failure of the bile formation process causes significant harm to health.
During the process, acids are synthesized from cholesterol, hepatocytes release phospholipids, cholesterol and bilirubin into the bile capillaries. The membranes of liver cells transport bilirubin through themselves into the capillaries. The last stage of formation occurs in the bile ducts due to the reabsorption of electrolytes from the general flow, the removal of water and bicarbonates by epithelial cells. Many facts are known about the harm from impaired bile formation. For example, if vitamin K is not absorbed, blood clotting is impaired.
Where is it stored?
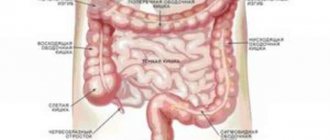
Bile production by a healthy liver occurs continuously. The gallbladder is the reservoir organ where it is stored. It moves there through special ducts, if the digestive process is not started, until a pressure of 200-300 mm Hg is created in it. Filling of the duodenum with food particles is a signal for the gallbladder to dump its contents into it. After the movement of food masses into the next section of the intestine, the duct between the duodenum and the VT closes until the next meal.
Concentration
The volume of the bladder in adults is relatively small - 50-60 ml. It looks like a pear in shape. In order to accommodate the entire volume of bile produced by the liver, the gallbladder processes it, absorbing water and some salts from the secretion through its walls. This is how bile thickens and concentrates. This bile is called mature due to its composition of 133.5 g/l of dry matter and only 80% water. As the fluid is absorbed, the pressure in the entire biliary system equalizes.
Physical properties
Bile is usually yellow in color, with shades of greenish-brown (due to the decomposition of coloring substances).
At the same time, it is transparent and viscous, which is directly related to the period during which it remains in the gallbladder.
It tastes bitter, smells very peculiar, and after a long stay in the gallbladder it develops an alkaline reaction.
Its weight is about 1005 in the bile ducts, however, it can increase to 1030 if it is in the gallbladder for a long time, due to the addition of mucus and other components to it.
Human bile has a rich yellowish color, turning greenish-brown (due to the decomposition of dyes). It is transparent, more or less viscous, depending on the length of time it remains in the gallbladder. It has a strong bitter taste, a peculiar odor, and after being in the gall bladder it has an alkaline reaction.
Bile secretion
The continuous flow of bile through the system is ensured by the pressure difference in its sections, the tone of the sphincters and the contraction of smooth muscle fibers of the ducts and gallbladder. Nervous and humoral regulation coordinates the process. Cholikinesis is regulated by conditioned and unconditioned reflexes through receptors in the mouth, stomach, and intestines using the vagus nerve. Humoral regulation refers to the influence of various digestive hormones on the biliary system.
When eating, conditioned and unconditioned stimuli stimulate the secretion of bile. The main one is the hormone cholecystokinin. The muscles of the walls of the gallbladder are influenced by hormones produced by the cells of the digestive organs under the influence of chyme. Excitation of nerve fibers triggers motility of the gallbladder and common bile duct with simultaneous relaxation of the sphincter of Oddi. The sphincter relaxes, the walls of the bladder contract and the bile concentrate freely enters the intestine, where emulsification occurs. The process lasts 3-6 hours. Irritated sympathetic nerve fibers relax the gallbladder muscles and contract the sphincter of Oddi. Bile secretion stops.
Bile acids
It is from this moment that the journey of bile from the liver to the duodenum begins. From the place where bile is produced to the place where it is used. And our journey begins too!
So, in a complex plexus of liver cells, tiny blood vessels and tiny bile ducts, bile was born. Having left the place of its birth - the liver cell - the bile enters the smallest and thinnest bile duct.
These microscopic bile ducts penetrate the entire thickness of the liver, leaving each of its cells and gradually merging with each other. And, merging, they form larger ducts, which, in turn, receive new and new flows of bile from other ducts into their channel.
Is it any wonder that, in the end, the smallest and invisible tubes - the bile ducts - merge with each other to form quite large ducts.
There is one important point to note here.
Before bile enters the right or left hepatic duct, its path passes through the bile ducts located in the thickness of the liver.
The right and left hepatic ducts leave the thickness of the liver. The bile that has entered these ducts also leaves the liver.
Bile, which was synthesized by the cells of the right lobe of the liver, enters the right hepatic duct, bile from the left lobe of the liver enters the left hepatic duct. These two ducts leave the thickness of the liver, exiting it in the area of the so-called porta hepatis. And just below the gate of the liver they merge with each other and form the common hepatic duct.
The chemical structure of bile includes bile acids. The synthesis of these components is the main direction of cholesterol catabolism in the body of mammals, as well as humans.
Certain enzymes that promote the secretion of bile acids are active in most cells of the body, but the liver is the exclusive organ in which their transformation takes place. Acid synthesis is the main process in which excess cholesterol is removed from the body.
But at the same time, the removal of cholesterol, which is expressed in the form of bile acids, is not enough to completely eliminate their excess intake from food.
Moreover, the appearance of these components expresses the process of cholesterol catabolism; these compounds are important for the solubilization of cholesterol, as well as lipids, fat-soluble vitamins and other elements, helping them get into the liver.
This process requires the presence of 17 specific enzymes. Some bile acids act as metabolites of cytotoxic substances, and based on this, their synthesis occurs under strict control.
Certain metabolic failures occur due to defects in genes that are responsible for the synthesis of bile acids. These disorders develop liver failure at a young age, and also manifest as progressive neuropathy in older people.
Some results of the study indicate that bile acids take part in the regulation of their metabolism, regulate lipid metabolism, as well as glucose metabolism, and are responsible for the course of various processes during the implementation of regenerative processes in the liver. At the same time, they regulate the overall expenditure of energy.
Stagnation of bile, even if there is no gallbladder, does not go away. The problem is only getting worse. Stones that cause stagnation occur both in the gallbladder and in the bile ducts. After removal of the gallbladder, the liver has a difficult time working - it performs functions that it did not perform before. Therefore, the liver requires restoration and careful treatment. Proper nutrition plays a central role here. Diet No. 5 remains a lifelong companion after removal of the gallbladder.
Internet discussions
The chemical composition of bile is mainly represented by bile acids. The synthesis of these substances is the main route of cholesterol catabolism in mammals and humans. Some enzymes involved in the production of bile acids are active in many types of cells in the body, but the liver is the only organ where their complete conversion occurs. Bile acids (their synthesis) are one of the dominant mechanisms for removing excess cholesterol from the body.
However, the excretion of cholesterol in the form of bile acids is not enough to completely neutralize its excess intake from food. Although the formation of these substances is a pathway for cholesterol catabolism, these compounds are also important in solubilizing cholesterol, lipids, fat-soluble vitamins and other essential substances, thereby facilitating their delivery to the liver.
The entire cycle of bile acid formation requires 17 individual enzymes. Many bile acids are metabolites of cytotoxic substances, so their synthesis must be strictly controlled. Some inborn errors of their metabolism are caused by defects in genes responsible for the synthesis of bile acids, which leads to liver failure in early childhood and progressive neuropathy in adults.
Recent studies have shown that bile acids are involved in the regulation of their own metabolism, regulate lipid metabolism and glucose metabolism, are responsible for the control of various processes in liver regeneration, and also regulate overall energy expenditure.
Clinical relevance
Bile is necessary for the breakdown and absorption of fats. Thanks to it, the digestive system digests fatty foods. If the secretion is not produced or does not enter the intestines, a pathological condition develops - steatorrhea. Symptoms of the disease: fats are excreted unchanged in the feces, feces acquire white and gray shades. The proportion of fats excreted in feces is 5 g and above. Useful components from food are not received enough, the body suffers from their deficiency.
For the absorption of water-insoluble fatty acids, cholesterol, calcium salts, increased protein and carbon hydrolysis, resynthesis of triglycerides at the cellular level is achieved through bile. Its activity during digestion at the parietal level secures enzymes on the inner walls of the intestine. The secretion of the pancreas, gastric mucus, the work of the small intestine, proliferation, and desquamation of pseudostratified epithelial cells are stimulated by bile in the human body. It is needed to prevent fermentation and rotting of waste products in the intestines.
Main functions
Most of the different substances include bile. It does not include elements that are found in digestive juices formed in the gastrointestinal tract. But at the same time it has enough bile salts and acids that:
- Emulsify fats, while dividing them into small particles.
- Help the body absorb various elements in the intestines. Bile salts interact with lipids and then enter the blood.
Another serious function is the presence of destroyed red blood cells. That is, bilirubin, which appears in the body in order to eliminate old red blood cells in which hemoglobin is present. Bile transports excess cholesterol. It acts as a product of liver secretion, and helps to extract various toxic substances.
- Bile ensures a change from gastric digestion, carried out with the help of pepsin, to intestinal digestion, in which the leading role is played by enzymes produced by the pancreas.
- Bile contains bile acids, which emulsify fats found in digested food, and thereby promote their rapid breakdown, absorption and assimilation.
- The next thing that bile does when it enters the intestines is stimulate its motor function and accelerate peristalsis, resulting in an increased rate of nutrient absorption.
- Bile has a beneficial bacteriostatic effect on the intestinal microflora and prevents the development of unwanted putrefactive processes in it.
- Bile is also of great importance in regulating electrolyte and protein metabolism, removing bilirubin and cholesterol from the body, which are not filtered by the kidneys and are removed from the body exclusively with its help.
Bile examination
The condition of the biliary tract can be assessed using the results obtained from the study of duodenal contents, during which decompression of the bile ducts is carried out. Diagnosis is carried out only on an empty stomach. The procedure is carried out with a thin probe with a metal olive at the end, 1.5 m long. The probe is immersed into the patient’s gastrointestinal tract in stages, to a certain mark, first in a sitting, then in a lying position. The doctor checks whether the probe has reached the duodenum. Its contents are transparent, green-yellow. The material is collected by suction using a syringe with a volume of 10-20 g.
Biological material mixed with gastric juice cannot be used for bacteriological analysis. Flakes in the sample and an acidic environment indicate incorrect sampling.
The process consists of pumping out the contents of the duodenum into different sterile tubes at intervals of 15 minutes. If you need to take a bile sample directly from the gallbladder, Magnesium sulfate in the form of a solution is administered through a probe. The drug stimulates the contraction of the walls of the gallbladder with the subsequent release of bile from it, a dark brown sample of which is collected in a second tube. The contents of all test tubes are carefully examined in laboratory conditions. Laboratory analysis of samples reveals the presence of pathological processes and their causative agents. In addition, the contractility of the gallbladder is checked.
Normal indicators
Normally, the first sample should be transparent, slightly alkaline, light in color and with a density of no more than 101, contain fatty acids from 17.4 to 52 mmol/l, bilirubin - no more than 0.34. Healthy indicators of gallbladder bile: density - up to 1035, acidity - 7.5 pH. It is transparent, dark green in color, contains FA from 57 to 184.6 mmol/l, bilirubin - up to 8. The liver test is transparent golden, with an acidity of up to 8.2 pH and a density of 1011. The FA content in it is normal 13-57, 2 mmol/l, bilirubin - up to 0.34. There should be no mucus, epithelial cells, cholesterol crystals, or a large number of leukocytes. Healthy bile is inherently sterile.
Patients are referred for bile testing if helminthic infestations are suspected. Among protozoa, Giardia is detected in most cases. Cholelithiasis and bile stagnation are often indicated by elevated cholesterol and excess calcium crystals. The presence of cylindrical epithelial cells indicates an inflammatory process occurring in the gallbladder or duodenum.
Components
Bile consists of the following elements: water (about 85%), the presence of bile salts (10%), mucus, as well as pigments (3%), fats (about 1%), various inorganic salts (0.7%), cholesterol (0.3%). ), is located in the gallbladder, and after eating it splashes into the small intestine, passing through the bile duct.
There is hepatic and also cystic bile, which consist of the same components, but their quantity is different. After analysis, the following elements were identified:
- water;
- bile acids and salts;
- bilirubin;
- cholesterol;
- lecithin;
- sodium, potassium, chlorine, calcium ions;
- bicarbonates.
How does it work?
Some composition, as well as the work of bile, allows it to work as a surfactant, helping to emulsify fats in food, similar to the principle of dissolving soap in water.
Bile salts have a hydrophobic and a hydrophilic end. When water containing fats enters the small intestine, bile salts form near the fat droplet and also bind the water together with the fat molecules.
This allows for a larger surface area of fat, which allows access to pancreatic fat-dissolving enzymes. Since bile allows fats to be absorbed more quickly, it also promotes the rapid absorption of amino acids, as well as cholesterol, calcium and various vitamins (D, E, K and A). Alkaline bile acids can remove excess acids in the intestines before they reach the ileum.
Consequences
Having discovered symptoms of excess bile, you should think about what dangerous consequences this phenomenon may entail:
- Reflux gastritis. Gastritis is an inflammation of the walls of the stomach, which can be caused by prolonged stagnation of bile in its cavity.
- Inflammation of the esophagus (esophagitis). Sometimes bile acids can be thrown into the esophagus, which leads to irritation and inflammation of its walls.
- Oncological diseases. As a result of the effect of bile on organ tissue, their cells can change and mutate, which is a prerequisite for a precancerous condition.
Thus, excess bile is indeed a very serious disorder that is important to diagnose correctly and promptly.
- Vomiting bile - causes, what to do, treatment methods
- Bile is thrown into the stomach symptoms
- What is the fine for a seller for selling alcohol to minors?
- How harmful is vaping without nicotine?
Concentration
The gallbladder concentrates bile, as it has the ability to store bile salts, as well as waste fluids that are produced by the liver. These elements (water, sodium, as well as chlorides or electrolytes) then diffuse through the bubble.
Research results show that the structure of bile in the bladder is equivalent to that of the liver, but is 5-20 times more concentrated. This is argued by the fact that bile includes bile salts, while bilirubin, cholesterol, as well as lecithin and other electrolytes, when in the specified container, are absorbed into the blood.
The gallbladder concentrates bile because it can store bile salts and waste products from the fluid produced by the liver. Constituents such as water, sodium, chlorides and electrolytes then diffuse through the bubble.
Studies have shown that the composition of human bile in the bladder is the same as in the liver, but 5-20 times more concentrated. This is explained by the fact that gallbladder bile mainly consists of bile salts, and bilirubin, cholesterol, lecithin and other electrolytes are absorbed into the blood while in this reservoir.