In order to diagnose a disease such as pancreatitis in a patient, a specialist must refer the patient to undergo a full examination, which includes not only laboratory tests, but also instrumental diagnostic methods.
Ultrasound for pancreatitis also plays an important role in the process of establishing an accurate diagnosis.
Since the pancreas is a non-hollow, solid organ, its structure, shape, size and echogenicity can be easily assessed using ultrasound. There are a number of signs indicating the presence of chronic or acute pancreatitis.
Before undergoing an instrumental examination, several prerequisites must be met:
- Do not eat food 12 hours before ultrasound diagnostics.
- If possible, do a bowel cleansing procedure on the day of the examination (in the morning).
- Three days before the ultrasound examination, do not consume foods that contribute to fermentation and gas formation in the gastrointestinal tract: legumes, cabbage, pears, baked goods made with yeast, carbonated drinks, etc.
- You can take espumisan or a drug with a similar effect to reduce flatulence.
- Immediately in the morning before the ultrasound, do not take any medications, drink or smoke anything.
Compliance with these rules for preparing for an ultrasound scan of the pancreas for pancreatitis will help you obtain the most reliable information.
In emergency cases, the patient undergoes this study without a preparatory stage, which can significantly affect the obtained diagnostic results.
When performing an ultrasound scan of the pancreas, it is necessary to know what indicators are characteristic of the normal functioning of this internal organ.
If the pancreas is healthy, it has clear and even contours, consists of three mandatory parts - the head, body and tail, which normally must correspond to certain sizes: body - not exceed 21 mm, head - 32 mm, tail - 35 mm.
The structure of the gland should be homogeneous, with small areas of increased or decreased echogenicity - a characteristic that shows how capable the organ under study is of absorbing or amplifying the ultrasound signal. In the image, this property is shown as dark (decreased echogenicity) or light (increased echogenicity) areas.
The pancreatic duct of a healthy organ has smooth walls and does not exceed 2 mm in diameter.
Ultrasound for acute pancreatitis
Whether pancreatitis is visible on ultrasound primarily depends on the form and stage of the disease. Acute pancreatitis is more easily diagnosed by ultrasound, since certain signs are pronounced, among which the following can be noted:
- noticeable increase in pancreas size;
- the presence of fuzzy and uneven contours;
- the pancreatic duct is more than 2 mm, also having blurred and uneven outlines of the walls.
In addition, with acute pancreatitis, changes occur in the internal organs located near the pancreas. They increase in size and become swollen. Possible complications include the presence of fluid in the abdominal cavity, as well as ulcers in the abdominal wall and omentum.
Ultrasound for chronic pancreatitis
If a person suffers from a disease such as chronic pancreatitis, an ultrasound will display a certain picture, characterized by a change in the structure, shape, size, and outline of the diseased organ.
What signs will be used to diagnose this disease during an ultrasound examination?
Firstly, the size of the affected organ is very important. With prolonged chronic pancreatitis, the size of the pancreas will decrease over time, this is associated with the development of fibrotic and atrophic processes. If, at the time of the study, the patient experiences an exacerbation of chronic pancreatitis, the diseased organ will be enlarged.
The specialist conducting the diagnosis should be attentive to a significant increase in the diseased organ or its tail. This sign may signal the presence of not only chronic pancreatitis, but also a possible neoplasm.
Secondly, echogenicity. Pancreatic tissue will also change during the course of the chronic form of the disease. Ultrasound for chronic pancreatitis will show heterogeneous increased echogenicity of the internal organ due to its atrophy and fibrosis. But this figure is normal for people who are elderly or obese. Therefore, increased echogenicity of a heterogeneous nature is a sign of chronic pancreatitis only in conjunction with other indicators of the disease.
The outer edges of the gland in chronic pancreatitis will be fuzzy, uneven and bumpy (“jagged”). The contour is deformed as a result of retractions of some external areas damaged due to fibrosis.
A characteristic sign of the presence of a chronic form of the disease is an expansion of the Wirsung duct up to 3 mm in diameter or more, which can be either uniform or uneven.
At the initial stage of chronic pancreatitis, the echostructure will be more homogeneous. As the disease develops, the glandular tissue will be characterized by heterogeneity of the parenchyma.
The results of ultrasound in chronic pancreatitis should be carefully studied by a medical specialist, as some important points should be taken into account:
- The diagnosis of chronic pancreatitis cannot be established solely on the basis of an ultrasound examination of the pancreas. It is necessary to take into account the manifestation of the main symptoms of the disease, as well as the results of all laboratory tests;
- the doctor should also avoid automatically transferring the diagnosis from the ultrasound report to the patient’s chart without conducting additional differential diagnosis of the patient;
- the information from the study will be reliable only if there are at least 4-5 signs (simultaneously) characteristic of the chronic form of the disease.
- Chronic pancreatitis is sometimes more difficult to determine by ultrasound than acute pancreatitis, so additional examinations are often prescribed - CT and MRI of the abdominal cavity, endoscopy, biopsy of the damaged area in case of a tumor;
- for older people, as well as for those who are overweight, some of the same changes in the pancreas are characteristic as for patients with pancreatitis, so it is worth taking this factor into account when examining the patient.
The conclusion of an ultrasound scan for pancreatitis provides additional information about the extent of the disease and the condition of the pancreas, but cannot be taken as a basis for making a diagnosis without the patient undergoing a full comprehensive examination.
It should be remembered that the results of an ultrasound examination can be both false-negative and false-positive, since it is not always possible to visualize the diseased organ due to the large amount of adipose tissue or due to increased gas formation.
However, this method of instrumental research is excellent for diagnosing other diseases of the gastrointestinal tract or complications caused by the underlying disease.
At the initial stage of the disease, ultrasound will not provide accurate information, since the signs of pancreatitis are not yet pronounced: the contours have not lost their clarity, the pancreas has slightly increased in size, and the echostructure has not changed.
The most reliable results can be obtained during exacerbation of chronic pancreatitis or in the acute form of the disease.
Click on pictures to enlarge.
Pancreatic cysts on ultrasound
Single small simple cysts occur as incidental findings in the healthy pancreas. In chronic pancreatitis, small simple cysts are quite common. If a cyst is suspected, note the enhancement of the contour of the far wall and the effect of signal enhancement in the tissue behind. Simple cysts are isolated from the parenchyma by a smooth thin wall. There should be no partitions or wall irregularities inside; the contents of the cyst are anechoic. Simple cysts are always benign. But, if the cyst is not obviously “simple”, further investigation is required.
| Photo. Simple pancreatic cysts on ultrasound. A, B — Single simple cysts in the area of the body (A) and neck (B) of the pancreas with a thin smooth wall and anechoic contents. B - Classic signs of chronic pancreatitis: the main pancreatic duct is dilated against the background of parenchymal atrophy, the contour of the gland is uneven with notches, there is calcification and small cysts in the parenchyma. | ||
Important!!!
Simple pancreatic cysts are common, but don't forget about cystic tumors. Cancer is the most dangerous disease of the pancreas.
There are two types of pancreatic cystic tumors: benign microcystic adenoma and malignant macrocystic adenoma. Microcystic adenoma consists of many small cysts and appears as a dense formation on ultrasound. Macrocystic adenoma usually includes fewer than five cysts larger than 20 mm. Sometimes polypoid formations can be seen in such cysts.
| Photo. A, B - Benign microcystic adenoma of the pancreas: a large cystic formation in the head of the pancreas. B - Pancreatic adenoma with macro- and microcystic components. |
With pancreatitis, pancreatic secretions digest surrounding tissue and pseudocysts form. Pseudocysts from the abdominal cavity can extend into the chest and mediastinum. Pseudocysts are often found in patients who have suffered acute pancreatitis (see below).
As a result of pronounced dilation of the pancreatic duct, retention pseudocysts may form distal to the site of obstruction.
Analysis of results
The ultrasound conclusion contains the most important information for a specialist: based on the information received, the doctor has the opportunity to confirm or refute the initially assumed diagnosis. If a patient has pancreatitis, as evidenced by the procedure performed, the doctor determines the severity of the disease, as well as its degree. If the picture is not entirely clear or provides incomplete data, the patient is referred for further examination (CT or MRI). Especially more accurate and extensive diagnostics are necessary when identifying neoplasms in the pancreas.
Normal indicators
The patient should not worry at all about the health of his pancreas if his report contains the following entries:
- The size of the pancreas is from 14 to 22 cm (any indicator that is included in this limitation);
- Well-visualized segments: organ head, body, tail;
- The size of the head is no more than 30 mm, the body is no more than 17 mm, the tail is up to 20 mm;
- Homogeneous granular structure of the parenchyma;
- Smooth and clear edges of the walls of the pancreas;
- Wirsung's duct is not dilated, its diameter is 2 mm;
- Absence of anechoic inclusions;
- Uniform echogenicity and average organ density.
However, even this ultrasound result must be shown to a specialist. If there are no obvious changes in the pancreas, and pain still bothers the patient, then the examination must be continued. Most likely, the reason lies in some other pathology, which is highly not recommended, because untimely treatment is sometimes fraught with the most disastrous consequences.
Currently reading: Is it possible or not to eat cauliflower for pancreatitis of the pancreas?
Deviations from the norm
The nature of any violations primarily depends on the severity of the disease. And if at the initial stage of the pathological process these changes may be insignificant or mildly expressed, then the picture that is visualized in severe pancreatitis is replete with a whole set of deviations. In addition, it is easier for an uzist to determine the acute course of the disease than the chronic one, since during an exacerbation the parameters of the pancreas are changed quite strongly.
In general, such violations include:
- Significant increase in the size of the pancreas, swelling;
- Unclear boundaries of the walls, unclear contours of the organ;
- Heterogeneity of the pancreas structure;
- Seals, which are signaled by increased echogenicity;
- Dilatation of the Wirsung duct up to 3 mm;
- Presence of fluid in the abdominal cavity;
- Complications: cyst, pseudocyst, necrotic foci, tumor;
- Enlargement of nearby organs.
The chronic form of the disease is characterized by slightly different signs:
- The size of the pancreas, on the contrary, decreases - this is due to fibrosis and atrophic changes in tissue, which occurs as a result of a long course of the disease;
- Heterogeneous structure of the parenchyma - this is indicated by numerous hyperechoic inclusions, which are foci of fibrosis;
- Changes in the contours of the pancreas due to retraction of external areas;
- Dilation of the Wirsung duct (over 2 mm), which does not narrow further - as a rule, this is evidenced by subsequent ultrasound results.
Acute pancreatitis on ultrasound
Acute pancreatitis is a severe complication of gallstone disease or a consequence of toxic effects, such as alcohol.
Mild pancreatitis is not visible on ultrasound (CT is a more sensitive method). Severe pancreatitis is easily detected by ultrasound. When an unusually clear and contrasting pancreas stands out from the surrounding tissue, edema of the parenchyma and surrounding fatty tissue can be assumed. If a thin layer of free fluid is visible around the pancreas, along the stomach, at the hilum of the liver and spleen, pancreatitis can be confidently diagnosed.
| Photo. Acute pancreatitis on ultrasound: A - Swelling of the pancreatic parenchyma (p), the contour of the pancreas is unusually clear, a small accumulation of fluid along the border (arrows). B, C - Accumulation of fluid along the contour of the body of the pancreas, a thin rim of fluid along the splenic vein (arrows), the parenchyma is heterogeneous, the surrounding tissue is hyperechoic - swelling and inflammation, the common bile duct is dilated (B). In this case, gallstone disease must be excluded. |
Almost all pancreatic tumors are hypoechoic compared to the normal pancreas. It is impossible to distinguish between focal pancreatitis and pancreatic tumor using ultrasound alone. A tumor and pancreatitis can be combined.
| Photo. Acute pancreatitis on ultrasound: The pancreas is unusually contrasted against the background of hyperechoic surrounding tissues, a thin strip of fluid along the contour (A), a hypoechoic focus in the tail (B), fluid in the hilum of the spleen (C). A hypoechoic tail can be mistaken for a tumor. |
In severe cases of pancreatitis, pancreatic fluid digests surrounding tissue, forming pseudocysts. Such cysts can be single or multiple. They may increase in size and rupture.
On ultrasound, pseudocysts are defined as oval or round hypoechoic formations with clear contours. In the early phases of cyst formation, it is a semi-liquid formation and has a complex echostructure with internal reflections and unclear contours. Later, due to autolytic processes and sedimentation of a suspension from blood and pus, clear signs of liquid contents appear and a false capsule with smooth walls is formed. Infection of pseudocysts often occurs, then internal echo structures or thin delicate septa can be detected. When a cyst is detected, it is important to trace the connection of the cyst with the duct, as this is important for determining treatment tactics. When a pseudocyst is more than 10 cm in size, difficulties arise in determining its source.
| Photo. A - Large pseudocyst between the head of the pancreas and the liver after pancreatitis. B, C - Severe necrotizing pancreatitis longitudinal (B) and transverse (C) sections: extensive necrosis, melting of the surrounding fat in the tail area, accumulation of fluid around the gland. |
Healthy pancreas results
During the examination, ultrasound will show the overall picture using medical indicators that are unclear to the patient. The main numbers by which it is possible to guess the existence of pathology are the parameters of the pancreas - shape and size. The information is available for comparison to any patient. Then ultrasound reveals other points characteristic of the diagnosis of pancreatitis.
When the pancreas is scanned with the machine, the components of the organ are clearly visible: the body, tail and head. For an adult, the following sizes are considered normal:
- body up to 21 mm;
- tail up to 35 mm;
- head up to 32 mm;
- The width of the duct is no more than 2 mm, the walls are smooth.
The silhouette of the pancreas itself is outlined with a clear line, the structure is uniform. An important indicator is the echogenicity of the organ, which determines the ability of the gland to increase or absorb the signal from the device’s sensor. The screen is identified by image parameters, brightness and clarity. The normal value coincides with the data for the liver and spleen.
Let's take a closer look at the indicators determined for pancreatitis. For different types of pancreatitis, an individual picture is displayed on the screen.
Calcifications in the pancreas on ultrasound
Important!!!
If there is dilatation of the pancreatic duct, you should look for stones in the pancreatic duct and in the common bile duct.
Calcifications inside the pancreas can give an acoustic shadow, but if they are small, they appear as a separate bright echostructure without an acoustic shadow. In chronic pancreatitis, calcifications are distributed diffusely throughout the pancreas. Stones in the duct are located along the duct. Gallstones in the distal common bile duct may be mistaken for calcifications in the pancreas. Calcifications are clearly visible on CT, and for non-calcified stones, MRI or ultrasound is preferable.
| Photo. A - There is a small stone in the dilated duct. B - In the dilated pancreatic duct there is a row of several stones with shadowing behind. B — A patient with chronic pancreatitis has huge stones in the dilated duct. Note the intense shading behind. |
| Photo. A, B — Calcifications in the pancreatic parenchyma in patients with chronic pancreatitis. Some calcifications have a shadow. B — A 5-year-old boy with chronic hereditary pancreatitis: calcifications (small arrows) and dilatation of the pancreatic duct (large arrow). C - confluence of the superior mesenteric and splenic veins. |
What should a healthy organ look like?
Normal pancreas levels are the same for both women and men.
During an ultrasound examination of this organ, the uzologist evaluates many parameters.
- The shape of the pancreas: in the normal state, it looks like an English letter; any change indicates an isolated defect or other pathologies that have a negative effect on the pancreas.
- Organ dimensions. The length of the pancreas in an adult varies from 14 to 22 cm, and the weight ranges from 70 to 80 g. Since the organ is anatomically divided into 3 parts, the parameters of each of these segments have their own standards. So, the natural length of the head should not be less than 25 mm and more than 30 mm. Body sizes range from 15 to 17 mm, and the tail reaches a length of 20 mm.
- Diameter of Wirsung's duct. This section of the pancreas is designed to transport pancreatic juice into the digestive tract. 2 mm is exactly the value that is typical for this channel in the absence of pathologies. With inflammation, the indicator most often increases (up to 3 mm), but narrowing indicates that the duct from the outside is being compressed by something, for example, a stone, cyst or tumor.
- Smooth and clear contours of not only the pancreas as a whole, but also all its parts separately.
- The average density of the organ, which should approximately correspond to the density of the liver or spleen - this parameter is determined by uniform echogenicity, allowing for small inclusions.
- Granular structure of the parenchyma.
Currently reading: Life expectancy with chronic pancreatitis
The given indicators may vary slightly, which is not a deviation from the norm. In this case, the values determined by the upper limits are taken into account.
Dilated pancreatic duct on ultrasound
The internal diameter of the normal pancreatic duct is less than 3 mm. The duct is better visualized with transverse scanning in the middle third of the body of the pancreas. In order to make sure that you have found the duct, you need to see the pancreatic tissue on both sides of it. The splenic vein posteriorly or the gastric wall anteriorly may be falsely interpreted as the pancreatic duct.
The walls of the pancreatic duct should be smooth and the lumen should be clean. When the duct is dilated, the walls become uneven; scan not only the head of the pancreas, but also the entire biliary tract.
The main causes of dilatation of the pancreatic duct: tumor of the head of the pancreas or ampulla of Vater's papilla (combined with jaundice and dilatation of the biliary tract); stones of the common bile or pancreatic duct; chronic pancreatitis; postoperative adhesions.
| Photo. A man with insulin-dependent diabetes mellitus complains of weight loss and abdominal pain for several months. Ultrasound shows an enlarged common pancreatic duct with an uneven wall. Upon further examination, calcifications with a shadow behind them are clearly visible in the duct (B). |
| Photo. A patient with acute pancreatitis: a large pseudocyst has formed at the level of the tail (see above), the dilated pancreatic duct opens into a pseudocyst. |
Experience in the use of echography in acute pancreatitis and its complications
Ultrasound scanner PT60A
Portable device for emergency care, intensive care and sports medicine
. Research of the musculoskeletal system, monitoring of anesthesia, etc.
Introduction
In Russia, in recent years, there has been a tendency towards an increase in the number of patients with acute pancreatitis, the frequency of which reaches 2.5 - 8.4% among patients with acute surgical diseases of the abdominal organs [1]. In Western European countries, in particular in Denmark, from 1979 to 1992, the incidence of acute pancreatitis increased from 26.8 to 35.4 per 100,000 population [15], i.e. by 25%. According to M.V. Grinev [8], of all patients with acute pancreatitis, destructive forms were noted in 16.2%, which, with progression, lead to mortality in almost 50% of cases [4].
Thanks to new research methods (ultrasound, CT, NMR), the early diagnosis of acute pancreatitis and its complications has improved, and it has become possible to dynamically monitor patients during treatment. Ultrasound diagnostics is of particular interest for wide practice - a non-invasive, non-ionizing method that can be used repeatedly without causing harm to the patient. With the help of echography, it has become possible to effectively carry out not only diagnostic, but also therapeutic minimally invasive interventions on the pancreas - biopsy, drainage of pathological formations, etc. [4, 6, 8].
Despite the intensive introduction of echography into practice and certain successes in studying the capabilities of the method, the literature has not yet sufficiently covered issues related to the details of ultrasound semiotics of acute pancreatitis. The echographic picture of acute pancreatitis depending on the stage of the disease is not specified; issues related to the diagnosis of complications of acute pancreatitis, especially rare but clinically significant ones, are poorly reflected [2, 5, 9 - 14, 16]. In patients treated surgically for acute pancreatitis, the problem of ultrasound monitoring in the postoperative period remains relevant. The role of ultrasound data for developing individual treatment tactics and predicting possible complications in each individual patient has been practically not studied.
Materials and methods
The work is based on data from 534 ultrasound examinations of 278 patients with acute pancreatitis who were treated at City Clinical Hospital No. 9 for the period 1992-1995. The studies were carried out using an ultrasonic scanner equipped with a 3.5 MHz convex sensor and a 5 MHz sector sensor.
results
Based on our observations, the following sonographic features of acute pancreatitis were identified:
Changes directly in the pancreas:
- an increase in the size of the pancreas (Fig. 1) was noted in 88% of cases. Normal dimensions of the pancreas: head 3-4.5 cm; body 2.5 - 3 cm; tail 3-4 cm;
- blurred contours - 90.6% of cases;
- an increase in the distance between the posterior wall of the stomach and the anterior surface of the pancreas over 3 mm and reaching 10 - 20 mm, which characterizes swelling of the parapancreatic tissues, was noted in 53% of cases (Fig. 1);
- change in the echogenicity of the gland: increase - 85.6% of cases (Fig. 2); normal - 8.6% of cases; decrease - 5.8% of cases.
Rice. 1.
Acute pancreatitis, destructive form. An increase in the size of the pancreas, blurred contours, an increase in the distance between the posterior wall of the stomach and the pancreas.
Rice. 2.
Acute pancreatitis, increased echogenicity of the pancreas (compared to the echogenicity of the liver).
Changes in the abdominal cavity, which are indirect signs of acute pancreatitis and related to its complications:
Omentobursitis
(Fig. 3) occurs in 28.4% of cases (of which 48% in men and 52% in women). Some authors designate this pathology as “pancreatic pseudocyst.” The volume of such formations has been noted to range from 5 ml (small volumes must be differentiated from vascular aneurysms) to 3 liters or more. The rate of formation of omentobursitis in acute pancreatitis is from 2 to 4 days. from the onset of the disease to 2 - 4 weeks. During ultrasound examination, omentobursitis is presented as an anechoic formation with clear contours, irregular or rounded shape, often with a homogeneous structure, with a wall thickness of 0.2 - 0.4 cm. With echographic monitoring, wall thickening is up to 0.5 - 1.0 cm with the appearance of structural heterogeneity should be regarded as a sonographic sign of abscess formation.
Rice. 3.
Pancreatic pseudocyst in acute pancreatitis in the form of an anechoic formation with clear contours, a homogeneous structure, with the presence of hyperechoic inclusions (detritus of the pancreas).
Free fluid in the abdomen
- noted in 18% of cases (Fig. 4), of which 80% in men and 20% in women. Fluid in a volume of up to 100 ml is detected only in one anatomical area (usually in the pelvis), more than 100 ml - in the lateral canals and in other parts of the abdominal cavity. In the first days of development of acute pancreatitis, the fluid is homogeneous, after 6-12 days. often the structure is heterogeneous due to “thread-like” inclusions (usually fibrin).
Rice. 4.
Dilated loops of the small intestine up to 3.5 cm, filled with liquid contents against the background of free fluid in the abdominal cavity.
Biliary hypertension
- occurs in 13% of cases, of which 25% in men and 75% in women. Echography reveals dilation of the intrahepatic bile ducts, common hepatic duct and common bile duct. In the absence of choledocholithiasis, biliary hypertension is usually observed with focal pancreatic necrosis in the area of the head of the pancreas.
Abdominal infiltrates
- found in 5.4% of cases (Fig. 5, 6), including 64% in men and 36% in women. As a rule, the greater omentum is infiltrated (omentitis), visualized as a formation of increased echogenicity with unclear uneven contours, a heterogeneous structure, with areas of reduced echogenicity, which may indicate the formation of abscesses in it. The sizes of infiltrates range from 5 to 15 - 20 cm.
Rice. 5.
Infiltration in the abdominal cavity in the projection of the greater omentum is represented by an irregularly shaped formation with unclear contours, a heterogeneous structure, and the presence of hyper- and hypoechoic areas. The size of the infiltrate is 8.5 x 3.9 x 5.3 cm.
Rice. 6.
Infiltrate in the projection of the greater omentum with an anechoic inclusion up to 4 cm (abscess formation).
Retroperitoneal phlegmon
- occur in 4.3% of cases (Fig. 7), of which 67% in men and 33% in women. In 95% of cases, left-sided localization of phlegmon was diagnosed, which was determined in the form of an anechoic or hypoechoic formation, often slit-like or oval in shape. As a rule, the cause of the development of this complication is the spread of pancreatic secretion through the retroperitoneal space from the pseudocyst, sometimes reaching the groin area. Pancreatogenic paranephritis can be considered as a variant of retroperitoneal phlegmon.
Rice. 7.
Retroperitoneal phlegmon on the left is an anechoic formation of irregular shape with unclear contours. The scan was performed from the left lumbar region.
Hydrothorax
- occurs in 2.2% of cases, equally often in men and women, with predominantly left-sided localization.
Thrombosis in the portal vein system
- noted in 1.5% of cases (Fig. 8 a, b) and can be determined quite well, in our opinion, without a Doppler study. If there are signs of portal hypertension, a targeted ultrasound examination of the vessels of the portal vein system must be performed. Thrombi can be single or multiple. They are localized both in the portal vein itself and in the splenic and superior mesenteric veins.
Rice. 8.
Portal vein thrombosis. The lumen of the vein is completely obstructed by an isoechoic formation with clear contours, heterogeneous structure, up to 4.7 cm long (a - sagittal section, b - transverse section).
Intestinal paresis
- occurs in 1.4% of cases (see Fig. 4), of which 75% in men and 25% in women. It is characterized by the expansion of the loops of the small intestine up to 3 - 5 cm with their filling with liquid contents and recorded “pendulum-like” peristalsis.
Hydropericardium
- occurs in 0.4% of cases.
Ascending mediastinitis
, noted by other authors, was not observed by us.
Pancreatic abscesses
- usually occur against the background of existing ultrasound signs of chronic pancreatitis.
Ruptures of pancreatic pseudocysts
during ultrasound diagnostics were observed in 2 patients (0.7%).
Hemorrhage into a pancreatic pseudocyst with the formation of an organized hematoma
(Fig. 9) was noted in 1 patient (0.35%).
Rice. 9.
A pancreatic pseudocyst in the form of an anechoic formation with clear contours, in which another anechoic formation with a capsule of 0.2 - 0.3 cm is identified (at surgery - a pseudocyst with an organized hematoma).
Pancreatic pseudocysts with atypical localization
(in the liver, spleen, periduodenal, etc.) were detected in 2 patients - 0.7% (Fig. 10).
Rice. 10.
An atypically located pancreatic pseudocyst (paraduodenal) in the form of an anechoic formation of a round shape with clear contours, a homogeneous structure, up to 4.5 cm in size, located next to the duodenum.
Splenic infarctions
(1 patient - 0.35%) - against the background of portal vein thrombosis with portal hypertension.
Splenic ruptures
due to portal hypertension (we did not observe).
Pancreatogenic paranephritis
— found in 2 patients, which amounted to 0.7% (Fig. 11).
Rice. eleven.
Left-sided pancreatogenic paranephritis, visualized as a liquid formation surrounding the kidney on all sides. Cross section.
Conclusion
The study shows that ultrasound diagnostics should be a mandatory element of the diagnostic algorithm in patients with acute pancreatitis. To increase the diagnostic value of echography, a certain sequence in performing an ultrasound examination is necessary: a detailed examination of the parapancreatic tissues and the gland itself; examination of all parts of the abdominal cavity for free fluid and infiltrates; examination of the pleural cavities and pericardial cavity for the presence of effusion; detailed examination of intra- and extrahepatic bile ducts; targeted examination of the vessels of the portal vein system; examination of the retroperitoneal space; dynamic observation (the frequency of repeated ultrasound is determined by the severity of the disease and the likelihood of complications).
To improve ultrasound results, the following techniques can be recommended:
- if visualization is poor, it is better to examine the tail of the pancreas through the spleen or left kidney;
- to improve visualization of the pancreas, you can fill the stomach with 500 - 800 ml of degassed liquid (water);
- use sensors with different radiation frequencies for a more detailed study of pathological foci located at different distances from the sensor;
- use polypositional scanning with dosed compression on the abdominal wall to improve visualization of the organs being examined, which allows you to “spread apart” the intestinal loops, thereby creating an additional “acoustic window”;
- use ultrasonic fistulography with liquid and gas-forming solutions (furacilin, novocaine, Echovist) to determine cavities in the presence of pancreatic fistulas [7], which may be the subject of separate studies.
Literature
- Skuya N. A. Diseases of the pancreas. - M.: Medicine, 1986.
- Zubarev A. R., Grigoryan R. A. Ultrasound angioscanning. - M.: Medicine, 1990.
- Filin V.I., Kostyuchenko A.A.. Emergency pancreatology. - St. Petersburg, 1994.
- Nesterenko Yu. A., Mikhailusov S. V., Imanaliev M. R. Ultrasound in the diagnosis and treatment of pancreatic necrosis / Sat. scientific tr. Plenum of the problem commission on emergency surgery. - M.: 1994. - P. 26 - 29.
- Baranov G. A., Mogutov M. S., Zavyalova N. I. Ultrasound diagnosis of portal vein thrombosis as a rare complication of acute pancreatitis / Sat. scientific tr. international conference “New technologies in diagnostics and surgery of the biliopancreaticoduodenal zone”. - M.: 1995. - P. 4 - 5.
- Belokurov GO. Ya., Utkin A.K., Zhokhov V.K., Belokurov S.Yu., Mogutov M.S. Prerequisites for the use of precision technology in the treatment of false cysts of the pancreas/ Sat. scientific tr. international conference “New technologies in diagnostics and surgery of the biliopancreaticoduodenal zone”. M.: 1995. - P. 78.
- Builov V. M., Mogutov M. S., Karpov N. R. Ultrasound fistulography with “Echovist-300” in surgery and urology. — Materials of the II Congress of the Association of Ultrasound Diagnostics in Medicine. - M.: 1995. - P. 80.
- Grinev M.V., Krasnogorov V.B., Ryss A.S., Veselov V.S., Smelyansky A.I., Alekseenko E.N. Effective tactics for the treatment of destructive pancreatitis based on early plasmapheresis and minimally invasive surgical interventions/ Coll. scientific tr. "Minimally invasive interventions in surgery." M.: 1996. - P. 257.
- McCormick P.A., Chronos N., Burroughs A.K., McLaughlin N., McLaughlin J.E. Pancreatic pseudocyst causing portal vein thrombosis and pancreatico-pleural fistula. In: Gut (1990 May) 31(5):561-3.
- Fernandez-Cruz-L., Margarona-E., Llovera-J., Lopez-Boado-MA, Saenz-HT. Pancreatic ascites. Hepatogastroenterology. 1993 Apr; 40(2): 150-4.
- Nishida-K., Terai-Y., Nojiri-L, Kato-M., Higashijima-M., Takagi-K., Adashi-R. A case of pancreatic pseudocyst with intracystic hemorrhage and repeated gastrointestinal bleeding. Nippon-Ronen-Igakkai-Zasshi. 1993 Aug; 30(8): 714-9.
- Sonak-R., Stock-W., Janzik-U., Hayduk-K., Borchard-F. Duodenal duplication cyst is a rare cause of acute recurrent pancreatitis. Leber-Magen-Darm. 1993 Sep; 23(5): 211-5.
- De-Ronde-T., Van-Beers-B., de-Canniere-L., Trigaux-JP., Melange-M. Thrombosis of splenic artery pseudoaneurysm complicating pancreatitis. Gut. 1993 Sep; 34(9): 1271-3.
- Hamm-B., Franzen-N. Atypically located pancreatic pseudocysts in the liver, spleen, stomach wall and mediastinum: their CT diagnosis. Rofo-Fortschr-Geb-Rontgenstr-Neuen-Bildgeb-Verfahr. 1993 Dec; 159(6): 522-7.
- Worning-H. Acute pancreatitis in Denmark. Ugeskr-Laeger. 1994 Apr 4; 156(14): 2086-9.
- Yasuda I., Tomita E., Nishigaki Y., Ino Y., Shimizu H., Yamada T., Kawamura H., Kuroda T., Takahashi T., Nagura K. A case of portal vein thrombosis subsequent to acute pancreatitis. Nippon Shokakibyo Gakkai Zasshi (1995 Apr) 92(4):820-5.
Ultrasound scanner PT60A
Portable device for emergency care, intensive care and sports medicine
. Research of the musculoskeletal system, monitoring of anesthesia, etc.
Pancreatic tumors on ultrasound
In most (50-80%) cases, the tumor affects the head of the pancreas. Tumors of the head compress the common bile duct. In cancer of the pancreas, the contour of the pancreas is unclear; local enlargement or bulging of the gland is characteristic, sometimes penetrating into the surrounding tissue in the form of tongues or pseudopodia.
In most cases, a pancreatic tumor is a hypoechoic formation, almost devoid of internal echo structures. However, there are tumors with diffusely scattered echo signals and with high-intensity echo signals in the center and their absence in the periphery. Despite the fact that the boundary between the tumor and the rest of the parenchyma of the gland is unclear, it can always be approximately drawn due to the difference in the echogenicity of normal tissue and the tumor focus.
Although the hypoechoic structure of the tumor, especially in the absence of small areas of increased density in it, resembles that of cysts, the absence of the effect of distal enhancement allows us to exclude the liquid nature of the formation. In addition, cysts are characterized by a much smoother and clearer border.
| Photo. Carcinoma of the head of the pancreas (arrow): the common bile duct (A) and pancreatic duct (B) are dilated, and a hypoechoic tumor surrounds the superior mesenteric vein (C). |
With tumors of the head of the pancreas, the common bile and pancreatic duct is often dilated, unlike chronic pancreatitis, its walls are smooth and not compacted.
Important!!!
Visualization of the main pancreatic duct within the hypoechoic zone is in favor of local edema and against tumor.
Sometimes, with pancreatic cancer, typical signs of chronic pancreatitis are revealed, as well as pseudocysts distal to the site of tumor obstruction. This is a consequence of obstruction. Intrahepatic metastases, enlarged celiac, periportal and retroperitoneal lymph nodes indicate cancer.
| Photo. Carcinoma of the head of the pancreas: the contour of the head is uneven due to a volumetric hypoechoic formation, the parenchyma of the body is very thin (atrophy), the pancreatic (A) and common bile (B) ducts are dilated, and there is a large round lymph node (C) at the porta hepatis. |
| Photo. A large lymph node (arrow) next to the pancreas may be mistaken for a tumor of the head. Enlarged mesenteric lymph nodes are round in shape, hypoechoic and without a central scar, which indicates their malignancy. |
| Photo. Large neuroendocrine tumor(arrows) of the pancreas with calcification and liver metastases (B). |
Take care of yourself, Your Diagnosticer
!
Problems with the pancreas are familiar to a fairly wide range of people. Pancreatitis affects neither adults nor children. And the earlier the disease is detected, the more effective the treatment will be.
Ultrasound examination helps to clearly see the clinical picture. The picture on the monitor screen will show what the pancreas looks like and how rooted the disease is in the body.
Diagnosed stages of disease development
Different stages of the disease show different results during examination and require a special approach to treatment.
Normal pancreas size
Edema
It is characterized by complete or partial swelling of the pancreas, not always accompanied by an enlargement of the organ. The disease in this case does not contribute to the accumulation of fluid and is eliminated by removing the swelling. It does not entail pathological changes in internal organs and can characterize both chronic and acute pancreatitis.
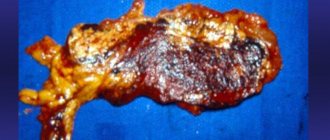
Hemorrhagic - necrotic
Symptoms of inflammation in this case can be classified as signs of chronic pancreatitis in the absence of proper treatment or acute. Inflammatory processes at this stage occur with microhemorrhages and tissue death. As a result, pseudocysts are formed, and necrotic changes occur inside the pancreas.
Destructive
The inflamed pancreas at this stage is difficult to scan. It has blurred contours and becomes loose, invisible to ultrasound. The bile ducts are blocked, and digestion is significantly impaired. The disease can be identified precisely by these signs, as well as by accompanying symptoms.
Types of pancreatitis
Inflammation of the pancreas has three types: acute, chronic and reactive. The acute form of the disease is characterized by changes in the tissue (it disintegrates), hemorrhage and accumulation of purulent substance are possible.
In the chronic form, the disease progresses slowly. A constant diet and medication are required.
A disease is called reactive if an attack of acute pancreatitis occurs along with the onset of diseases of the liver, stomach, duodenum, and gall bladder.
What does acute pancreatitis look like?
A number of forms of acute pancreatitis are known; pathology implies mild and severe course of the disease. In the first case, the organ is slightly damaged; when the symptom is first removed, it becomes difficult to identify the seriousness of the situation. The severe form manifests itself in the form of certain indicators.
Indicators of acute pancreatitis
The general picture of signs of acute pancreatitis on ultrasound comes down to the following:
- the overall size of the organ is increased;
- the boundaries of the pancreas have an unclear contour, with curvatures;
- increased echogenicity in sources of inflammation;
- the structure is heterogeneous;
- the duct is much wider than normal;
- liquid conditions are detected in the organ area, changes in neighboring organs;
- in severe cases, cysts, areas of decay, and other uncharacteristic changes may be detected.
Changes in the abdominal cavity indicate acute pancreatitis. Along with laboratory tests, analyzing each symptom along with an ultrasound examination, confirmation of the diagnosis of acute pancreatitis will be reliable.
Symptoms of the disease
In the chronic form, the patient experiences pain in the upper abdomen. Painful sensations can be felt in the left, less often the right hypochondrium. Appear due to poor diet and alcohol consumption. The pain can be either dull or sharp. There is also a feeling of nausea and bouts of vomiting.
The acute form is characterized by the following picture:
- sudden, severe pain in the upper abdomen, leading to shock, can radiate under the left shoulder blade;
- debilitating vomiting;
- diarrhea.
With reactive pancreatitis, the patient experiences pain, cutting and dull, of a girdling nature. There is a taste of bile in the mouth, and vomiting is also characteristic.
What can be determined using ultrasound
All patients with inflammation of the pancreas are prescribed an ultrasound examination. It is carried out for both acute and chronic pancreatitis, and if the disease is suspected.
An ultrasound will show the condition of the contours and tissues of the gland:
- if the contour is blurry, it means that inflammatory changes are occurring in the pancreas and swelling has begun. But it may also be evidence of a disease of the stomach or duodenum;
- the contour is convex, but at the same time smooth - a cyst has formed on the gland;
- uneven outlines are characteristic of pancreatitis and neoplasms;
- lumpy, blurry edges indicate cancerous formations.
An ultrasound examination also demonstrates the condition of the pancreatic tissue. In a healthy person it is of medium density. If the density is increased, it means that the connective tissue has grown. This condition is typical for chronic pancreatitis, but may be evidence of age-related changes. There are white areas on the screen.
If the fabric density is reduced, the image on the screen will be black. This condition is typical for the acute form of pancreatitis.
At each stage of the disease, the contours of the pancreas and its structure change. In the first stage of the acute form of the disease, the contours of the pancreas are blurred and uneven, the density is reduced, and the duct is dilated.
At the second stage, a cyst or abscess may appear. The contour will be rounded, the density of the tissues will decrease.
With chronic pancreatitis, the contours become unclear. If stones appear in the gland, the contour will become rounded, and the density in this place will increase.
Purpose of the procedure
An ultrasound examination is primarily carried out for the purpose of diagnosing pancreatic pathology; ultrasound can also be used at the control stage, when it is necessary to confirm positive changes in the treatment of the disease.
When diagnosing, doctors are able to establish:
- The presence or absence of acute or chronic pancreatitis.
- Determine organ deviations from the norm.
- Determine the stage of the disease.
- Note what pathological changes have occurred in other organs.
- What complications threaten the organ in the future as the disease progresses (often an abscess, pseudocyst, vascular thrombosis, etc.).
Ultrasound examination allows to identify abnormalities in the organ
If ultrasound of acute or chronic pancreatitis was performed at an early stage, then ultrasound diagnosis may not yield results.
Cyst and tumor
If a black tumor with smooth, well-defined edges is visible on the pancreas during an ultrasound, this is evidence that fluid has accumulated in these places (a cyst has grown) or pus has accumulated.
Cancers of the gland appear as black or white spots. It depends on what type of cancer is developing in the body. Mixed cases are possible.
With anomalies of the pancreas, two pancreatic ducts and a blurred structure are visible that unevenly transmit ultrasound flows.
How to prepare for an ultrasound
First of all, it is necessary to organize proper nutrition. Do not consume foods that promote gas formation: soda, sweets, legumes, mayonnaise, cabbage, etc. Gases inflate the intestinal loops, which, in turn, close the pancreas. The study may fail.
To reduce gas formation, it is appropriate to take adsorbents, pancreatic enzymes, and carminatives.
During the period of preparation for ultrasound examination, you should reduce the consumption of meat and meat products, dairy products, and fish. And it also follows:
- exclude alcoholic drinks;
- forget about smoking;
- you can take medications that reduce gas formation;
- The last meal should take place 6–8 hours (in children 3 hours) before the start of the study.
What is the ultrasonography procedure and how to prepare for it?
This procedure is carried out in a medical office using an ultrasound diagnostic device. In order for the study to be successful, it is worth following a number of rules before going on it.
- Patients are often interested in the question of whether they can eat any food before the examination. You cannot eat anything before the ultrasound. The last time the patient is allowed to eat is the day before going to the doctor for dinner. In the morning before the abdominal ultrasound procedure, you are prohibited from even drinking water.
- In the morning, before going to the clinic, you need to empty your bowels. If this cannot be done naturally, you will have to resort to an enema. If this is not done, then there will be masses in the defined areas that will significantly affect the outcome of the study, not for the better.
- The ultrasound procedure is carried out exclusively in the morning, and there is a logical explanation for this: in the morning hours there is the least amount of air in the human body, because it has not yet had time to enter there with food. This fact is worth taking into account, since air bubbles can significantly distort the picture of the disease.
- The study must be planned in advance, since three days before it you should abstain from food that causes fermentation in the intestines. Such foods include black bread, legumes (beans, peas, beans, corn), cabbage, grapes, and fresh baked goods with yeast. Avoid drinking any carbonated drinks.
- In order to reduce gas formation in the intestines, you need to take tablets like Espumisan, and it is also possible to drink activated charcoal.
- Before going to the doctor for this procedure, do not take any medications and completely abstain from smoking.
Attention! If a patient suddenly has an attack (reactive pancreatitis), then an ultrasound procedure can be prescribed without prior preparation, when there is no time to waste, since reactive pancreatitis develops very quickly, and there is a direct threat to the patient’s life. However, doctors must be aware that information about the patient's health status obtained in this way will not be completely accurate.
When ultrasound is prohibited
The doctor will not prescribe an ultrasound if there is an allergy to the gel used or if the patient’s life is at risk. When the patient's condition has stabilized, an ultrasound examination can be performed. Patients who are obese in the third stage do not undergo such testing, since there is no good overview.
If there are abrasions and wounds, an ultrasound will also not be performed. This is because it is impossible to get good contact. The result is a bad review.
In case of problems with the pancreas, it is necessary to organize treatment correctly and in a timely manner and undergo tests determined by the attending physician. Relying on your own strength and grandmother's remedies is a dangerous game with your health.
Makes up about 2% of all tumors. There are cancers of the pancreas, cancer of the head, body, and tail of the pancreas.
Malignant tumors of the pancreas - carcinoma, adenocarcinoma, sarcoma, carcinosarcoma - develop from immature epithelial tissue. Primary pancreatic cancer occurs in 0.1% of all patients referred for inpatient treatment. Most often, pancreatic cancer is observed at the age of 50 - 60 years, although in some cases it occurs in early childhood and adolescence. Pancreatic cancer affects men more often. The ratio of men to women is 2:1. Cancer of the head is more common (70%), less common is cancer of the body and tail (30%).
Macroscopically, pancreatic cancer has the appearance of a tuberous node, which can spread diffusely, over varying lengths, or infiltrate the gland, affecting the vessels and causing necrosis of the parenchyma. Necrotic areas can liquefy, forming something like pseudocysts. Often, even during treatment, it is difficult to differentiate this form of pancreatic cancer from chronic pseudotumor pancreatitis. The latter has a longer history of the disease. Only a biopsy, and even then not always, can detect tumor cells that determine the correct diagnosis. Microscopically, cancers are distinguished from the ductal epithelium, gland parenchyma and islet epithelium. The most common are scirra, less common are adenocarcinomas, mucous, and squamous cell carcinomas.
The types of tumor spread beyond the gland and the nature of metastasis deserve some assessment. A distinction is made between direct spread and tumor invasion of the entire pancreas and neighboring organs with compression of the latter (common bile duct, duodenum); hematogenous metastasis, in particular through the portal vein with subsequent thrombosis; spread of tumor elements perineurally (with the development of pain) and metastasis along the lymphatic tract with damage and enlargement of the lymph nodes at the porta hepatis, para-aortic and other nodes.
The first place in the metastasis of pancreatic cancer is the liver, followed by the abdominal lymph nodes of various locations.
Cancer of the body and tail of the gland usually does not cause jaundice, is diagnosed less frequently, is not accompanied by disturbances in liver function, and proceeds relatively more safely, although the prognosis is unfavorable.
How effective is the endoscopic ultrasound procedure in diagnosing abdominal diseases?
Using ultrasound for pancreatitis, a detailed description of the appearance of the organ being examined is analyzed. The use of this type of research is considered a strictly mandatory component in the diagnosis and treatment of any type of inflammation. Using ultrasound, it is convenient to monitor the dynamics of treatment of the inflammatory process.
This procedure will show pancreatitis in the earliest stages and begin to treat it in time, because preventing the disease is much easier than curing it.
Symptoms
Pancreatic cancer has no pathognomonic signs; most often it is a question of the correct clinical assessment of combinations of these signs. Pancreatic cancer is determined by a number of causes. The most important of them are the size and location of the tumor, the degree of compression of nearby organs and anatomical formations by the tumor, and the patient’s previous condition.
Other parameters in the formation of the disease are the nature of tumor growth, the presence or absence of jaundice, the degree of development of intoxication, the nature of changes in external and internal secretion, and features of metastasis. In 80% of cases, pancreatic cancer is accompanied by jaundice. The anicteric form of the disease is much less common, which usually occurs when the tumor is localized in the area of the body and tail of the gland.
Early signs of pancreatic cancer, which do not have specificity, should include loss of strength, fatigue, decreased performance, weight loss (up to 10 kg per month), aversion to food, lack of appetite, “unreasonable” loose stools, dull discomfort throughout the abdomen , radiating to the lumbar region, gastric discomfort. The appearance of jaundice often makes one think about Botkin's disease, and therefore the patient may end up in a bed in the infectious diseases department. Consultation often reveals the second, unfortunately, late sign of the disease - an enlarged, sometimes large, gallbladder, which in combination with jaundice (Courvoisier syndrome) makes one think about pancreatic cancer.
When cancer is localized in the body and tail of the gland, the clinical symptoms of the disease are even less pronounced. The symptom of pulsation of the abdominal aorta, similar to Voskresensky’s symptom in acute pancreatitis (transmission of aortic pulsation through a tumor of the body of the pancreas), is assessed and the Shoffard-Leriche form is identified, when a tumor of the body and tail of the pancreas is manifested by weakness, cachexia and girdle pain.
There are forms of the disease that are diagnosed already in advanced stages. In these cases, the clinical picture is formed not by a tumor of the gland, but by its metastases to various organs, for example, to the pleura (chest pain), to the liver (jaundice), to the lymph nodes of the peritoneum (peritonitis, abscess), to the portal vein area (ascites), in the stomach (bleeding), in the spine (lumbosacral pain simulating radiculitis).
Pancreatic cancer may be accompanied by the development of multiple peripheral thrombophlebitis in the patient, and then the diagnosis of the disease is difficult.
Ultrasound for pancreatitis: what shows how it is done
If a gastroenterologist suspects a patient has pancreatitis, he usually prescribes a comprehensive examination, including an ultrasound examination of the pancreas. It is worth noting that ultrasound for pancreatitis does not always give unambiguous results.
For example, with age and under a number of other circumstances, the pancreas increases echogenicity. The doctor may interpret it as a sign of illness. But a radical excess of the norm for this indicator does not become an unambiguous symptom of pathology.
Doctors also pay attention to stones and cysts in the pancreas and to an enlargement of the Wirsung duct. In addition, the results of the ultrasound examination are reviewed by specialists along with the results of the entire range of tests and examinations.
Before going through an ultrasound scan of the pancreas for pancreatitis, doctors recommend carefully preparing. It is advisable not to eat anything at all for twelve hours before visiting the doctor. It is also advisable to cleanse the intestines well on the morning of the examination.
For three days before this, foods that promote the formation of gases and fermentation in the gastrointestinal tract are prohibited from consumption:
- cabbage;
- any legumes;
- pears;
- grape;
- rich yeast baked goods;
- carbonated drinks and so on.
To reduce flatulence, doctors allow you to take a drug like espumisan. But in the morning before the ultrasound examination, you should not take medications, smoke or drink.
Whether an ultrasound will show the presence of pancreatitis, and how accurately this will be done, depends on the quality of following the specified preparation rules. In emergency cases, patients are examined without preparatory manipulations, but the accuracy of the results is greatly reduced.