In recent years, mortality from pancreatitis has increased greatly. The problem, of course, concerns the acute form of this disease. Statistical studies show that 40% of cases of acute pancreatitis are fatal for the patient.
The disease spares neither women nor men, and most often death occurs in the first week of exacerbation. If a patient is diagnosed with hemorrhagic or mixed form of pancreatitis, then the possibility of dying in this case remains quite high.
The disease is accompanied by total pathological changes in the pancreas. The patient must be constantly on alert, because it is known that pancreatitis does not belong to the category of ordinary diseases, and neglect of its symptoms poses a mortal danger to humans.
Main signs of pancreatitis
Vomiting, nausea and girdle pain in the upper abdomen that appear immediately after eating are the first and main symptoms of chronic and acute pancreatitis. Moreover, even severe vomiting does not bring the patient the slightest relief.
In the chronic form of pancreatitis, the symptoms do not appear so sharply, but the painful processes last much longer than in the acute form. Pain that initially occurs in the abdomen further spreads to the lower chest.
Pancreatitis is often accompanied by paroxysmal pain, the occurrence of which is characteristic of the acute form of the disease, the outcome of which can never be predicted.
What types of diseases are there?
There are two types of pathology - chronic and acute pancreatitis.
Chronic pancreatitis manifests itself due to the acute form of the disease. The disease progresses over the years, becoming more and more deformed.
In the acute form, inflammation of the organ occurs almost instantly. The form of the disease is rare. At risk are more often male patients aged forty to fifty years. Chronic alcoholism is often a risk factor for this pathology.
Types of pancreatitis
Acute form
Acute pancreatitis is the most dangerous form of this disease, in which death is a common outcome. A patient with this type experiences localized pain in the left or right hypochondrium. If the entire pancreas is affected, girdling abdominal pain may be observed. Acute pancreatitis is also characterized by other signs, such as:
- belching,
- nausea,
- hiccups,
- dry mouth,
- frequent vomiting of food masses mixed with bile, and getting rid of the stomach contents does not bring relief to the patient.
Pancreatitis must be diagnosed as early as possible, since seemingly insignificant problems can lead to irreversible consequences.
If the disease develops rapidly, the patient’s condition deteriorates sharply in a very short time, and death may occur, and the following symptoms are observed:
- Decreased blood pressure.
- Increased body temperature.
- Cardiopalmus.
- Paleness of the skin.
- Severe shortness of breath.
- White coating on the tongue.
- The patient's facial features become sharper.
- Bloating.
- Signs of paresis of the stomach and intestines.
- In the later stages of the disease, palpation of the abdomen reveals symptoms of peritoneal irritation.
It should always be remembered that pancreatitis is dangerous due to sudden death.
Cholangiogenic form of pancreatitis
In patients with cholangiogenic pancreatitis, symptoms of the disease appear immediately after eating. This type of disease is caused by the presence of stones in the bile ducts. Choleretic ingredients consist of alkaloids, fatty acids, essential oils, proteins, totopin and sanguinarine.
Chronic alcoholic form of pancreatitis
This form is often diagnosed in those people who openly abuse alcohol. It is clear where this name came from. Signs of alcoholic pancreatitis are very pronounced and appear after eating fresh fruits, vegetables and any spicy or sour foods.
The early stage of the disease may be accompanied by frequent constipation in combination with hypomotor dysnesia of the large intestine and biliary tract. Very soon constipation is replaced by unstable, pronounced loose stools. Diarrhea in the alcoholic form of pancreatitis is an invariable companion and a typical symptom.
Are there any chances of surviving the disease?
To survive pancreatic necrosis, emergency hospitalization in the surgical department is necessary. The painful process of cell death occurs rapidly, can be lightning fast and be completed within one to two hours. If necrosis has become total, death occurs in 100% of cases. To interrupt the vicious pathological circle, urgent resuscitation measures and surgery are needed. In this case, life can be saved.
Initially, the patient is admitted to the intensive care unit, where all emergency treatment measures are carried out to bring the patient out of shock. Detoxification and pain relief are carried out, and complete functional rest is created for the pancreas. Approximately on the 5th day, when the boundaries and extent of organ damage become clear, necrectomy is performed.
But this does not always happen in such a time frame. If the lesion is total and the clock is ticking, the operation is performed immediately, sometimes the pancreas is completely removed - pancreatotomy. The patient must be secured for further manipulations to flush the installed drainage systems, and he may remain in this position for a long time.
The duration of treatment after surgery is long, taking more than six months or a year. It is mandatory to follow the prescribed diet - table No. 5 according to Pevzner. In the future, under the supervision of a gastroenterologist, it can be changed to table No. 1 and its modifications. Only a specialist can determine how long you need to be on a strict diet.
In addition to the diet, enzyme preparations that have a good review of the treatment of pancreatitis are prescribed, as well as a number of medications that are necessary for good health. All instructions must be strictly followed - this is the only way to improve the quality of life after surgery.
Reasons for high mortality among patients
It has already been noted above that both men and women die from pancreatitis. Most often, death occurs in the first week of illness.
In this case, doctors diagnose a hemorrhagic or mixed form of pancreatosis, which is accompanied by total pathological changes in the pancreas. The death of a patient from pancreatitis can occur in the following cases:
- If the structure of the tissues or cells of the pancreas is changed.
- In case of exudate and formation of necrotic foci.
- With reactive pathological processes in the foci - necrosis of the pancreas.
Usually in these cases the time of death is calculated in several hours or days. In rare cases, the patient can survive for about a month. An organ called the pancreas secretes extremely aggressive digestive juice that can digest any protein, including the pancreas itself.
The nature of the human body has provided for the process of digesting food, during which pancreatic juice is transported to the duodenum and mixed with other substances.
If there are some obstacles to the juice entering the duodenum, as a result of which the aggressive product will remain in its own ducts, then the process of self-digestion of the pancreas, called pancreatosis in medicine, is possible, and necrosis of the pancreas is an extremely severe form of pancreatitis.
From the above it follows that the cause of death in pancreatitis is clogged pancreatic ducts. The main factors for high mortality from pancreatitis include:
- alcoholism;
- unhealthy diet (too spicy and fatty foods, inclusion of foods containing preservatives in the diet);
- cholelithiasis;
- constant stress.
Frequent nervous strain and chronic stressful situations can cause spasms in the bile ducts, which will certainly inhibit the natural processes of food digestion. The consequence of this is all kinds of pathological changes in the pancreas.
The cause of death from pancreatitis can also be called food products characterized as “socogon”. This is a combination of very fatty and spicy foods with large doses of alcoholic drinks; you need to understand that alcohol and pancreatitis simply do not go together. Death can be caused by a strong blow to the solar plexus, followed by the development of pancreatosis.
Pancreatitis is a severe inflammatory process in the pancreas. This pathological condition affects the organs of the digestive tract, in addition, serious problems arise with the condition and functions of all organs and systems of the human body. Death from pancreatitis, unfortunately, often occurs, especially in the acute course of the disease, and also if severe complications develop, disruption of the vital functions of the body.
What is pancreatic necrosis of the pancreas?
According to statistics, pancreatitis ends in death in 40% of the total number of cases. In other words, due to acute inflammation of the pancreas, 4 out of 10 people suffering from this disease die. In general, there are many pathologies of this organ that are fraught with the most unfavorable prognosis.
Lyudmila Senchina
Soviet and Russian singer and actress, recognized as People's Artist of the Russian Federation and Honored Artist of Ukraine, was born on December 13, 1950 in Ukraine, in the Nikolaev region. Thanks to her father, the director of the village cultural center, Lyudmila first appeared on stage. At first these were amateur performances and festive performances, but after graduating from the Leningrad Music College, fame gradually began to come to her.
At the same time, Senchina began acting in films; she rarely appeared in Soviet films, but always played the main roles. The actress gained particular popularity after the release of the film “Armed and Very Dangerous” in 1977; it was from that moment that a major turn came in Senchina’s biography. In the 80-90s, her popularity as a pop singer reached its apogee: her songs “Fragrant bunches of white acacia...”, “Pebbles”, “Love and separation”, “Wild flowers” were sung by the whole country.
Lyudmila Senchina was married 3 times. In her last interviews, she admitted that she regretted divorcing her first husband, with whom she had been married for 10 years. According to the singer herself, there was a period in her life when she was in a seriously depressed state. During this time, she began to rapidly gain weight, although a little later she quickly got into shape.
Many of her fans are inclined to believe that it was these two factors: depression and the possible use of fat-burning drugs that served as a serious impetus for the development of a terrible disease - pancreatic cancer. The artist had a courageous character, she performed even when she was undergoing chemotherapy, and continued to make plans for her creative activity.
Oleg Yankovsky
A brilliant performer of a variety of roles, both comedic and heroic, and simply a charismatic personality, Oleg Yankovsky. Film director, theater, film and television actor of the USSR and Russia was born in the Kazakh SSR on February 23, 1944. He received his education at the Minsk Theater Institute, but began his career in Saratov.
It was there that he worked for some time in the city theater, where he was taken at the request of his wife Lyudmila Zorina. At first, Yankovsky was in her shadow, however, in 1967 the situation changed dramatically: the artist was noticed by Vladimir Basov, a famous film director who at that time was filming the film “Shield and Sword” and was looking for an actor with a handsome and courageous image for the main role.
In the run-up to 2009, Yankovsky sought medical help, complaining of severe abdominal pain. By then he already looked very exhausted. Doctors discovered that he had a late-stage malignant tumor of the pancreas - it was then that it became clear that the actor would not be able to live long.
For some time, Yankovsky was treated in Germany, but treatment even in such a country with fairly developed medicine did not bring a positive result, and a month later he returned to Moscow, having managed to play in his last performance. In April, Yankovsky became significantly worse: he suffered internal bleeding. Already on May 20, Oleg Ivanovich passed away - less than a year passed from diagnosis of the disease to death.
Svyatoslav Belza
Born on April 26, 1942 in the city of Chelyabinsk. His father devoted his entire life to musicology, so the boy grew up in this atmosphere from an early age and soon began to show interest not only in music, but also in world literature. He was especially interested in the work of William Shakespeare.
After graduating from the Faculty of Philology at Moscow University and going to work at the Gorky Institute of World Literature, Belz began writing for Literary Gazette - these were essays and reviews of the works of foreign authors, as well as works devoted to the topic of the influence of European culture on Russian literary creativity.
Since 1987, Belza began working on television, he hosted his own program “Music on Air”, together with Maria Maksakova he was the presenter of “Romance of a Romance”, working in tandem with Alla Sigalova, he hosted the programs “Bolshoi Ballet” and the Bolshoi Opera.” In the literary, musical and educational fields, Belza was awarded many prizes and awards.
There were no signs of trouble, but at the end of 2013 Svyatoslav Igorevich felt unwell and had abdominal pain. According to Belza himself, before this he was in excellent physical shape and had not been to the doctors for about 20 years. Busy days with work did not allow the literary scholar to seek help: a visit to specialists was constantly postponed.
In the spring of 2014, Belza received a disappointing diagnosis - pancreatic cancer. In the first week of May, the presence of the disease was confirmed in one of the clinics in Germany, where the writer remained for further treatment. However, the life span allotted to him turned out to be very short: on June 3, 2014, Svyatoslav Belza died right in a Munich hospital.
Lyubov Orlova
A terrible disease - pancreatic cancer - also claimed the life of the Soviet theater and film actress, pianist, dancer and singer Lyubov Orlova. She was born on January 29, 1902 in Zvenigorod. She devoted her whole life to theater and music, studied at the Moscow Conservatory and Gitis, taught music for a long time and worked in the capital’s cinemas.
In 1933, her career as a movie star began, which began with Grigory Alexandrov’s film “Jolly Fellows.” Thanks to her wonderful soprano and excellent playing on the piano and grand piano, she became famous for such films as “Volga-Volga”, “Shining Path”, “Meeting on the Elbe”, “Russian Souvenir”, “Starling and the Lyre”. The artist was twice awarded the Stalin Prize, for her services she received two Orders of the Red Banner of Labor, as well as the Order of Lenin.
On January 26, 1975, Lyubov Orlova died; the cause of her death was a malignant tumor of the pancreas. Doctors, wanting to protect the singer from stress, hid the diagnosis from her for a long time, for which she was hospitalized. At a certain period, Lyubov Petrovna began to recover, but the disease still took over.
Steve Jobs
World famous inventor, entrepreneur and industrial designer from San Francisco, Steve Jobs also died of pancreatic cancer. This man is known to many as the founder of the large Apple corporation, the creator of both the iPhone and iPad.
In 2003, when Steve was 48 years old, he was diagnosed with islet cell cancer. Despite the aggressive nature of the disease, the type of this pathology was very rare and amenable to surgical treatment. However, for 9 months, Jobs refused surgery because he did not want his body to be opened.
All this time, he tried to recover using unconventional methods: he followed the principles of a vegan diet, took courses in herbal medicine and acupuncture, and visited mediums. But the disease continued to progress, and in July 2004, Steve agreed to surgery; he underwent pancreaticoduodenectomy, as a result of which the malignant tumor was successfully removed. It would seem that the disease had subsided, but metastases were discovered in the businessman’s liver.
Over the next 3 years, Steve’s health deteriorated, he lost noticeable weight, but continued to engage in activities, gave presentations and stubbornly kept silent about the whole truth about the state of his health, attributing the deterioration in appearance either to dysbiosis or hormonal imbalances. In fact, due to immunosuppressants and painkillers, Jobs had practically no desire to eat, but instead he was overcome by terrible depression, for which Steve refused to be treated.
In 2009, Jobs made his problem public by handing everything over to Tim Cook, Apple's chief sales officer. His departure lasted until the beginning of 2010, however, on January 17, 2011, it was announced again that the head of the company was taking medical leave. On August 24 of the same year, Steve officially announced his resignation from his post, and on October 5 he died: due to complications of the disease, he suffered respiratory arrest. Steve Jobs died surrounded by his family: his wife, sister and children.
Marcello Mastroianni
Italian actor, winner of Italian and European film awards, was born in the village of Fonatana Liri in 1929. He devoted his entire life to cinema, his personality is recognized from such films as “White Nights”, “Intruders Unknown”, “Sweet Life”, “Night”, “City of Women”, “Black Eyes”.
For the last few years before his death, the actor struggled with a dangerous disease - pancreatic cancer. Mastroianni had a strong character, despite severe pain and general malaise, he continued filming and regularly appeared on stage. The film star’s last work was a role in the play “Last Moons.” To continue to please the audience and his fans, Marcello had to receive chemotherapy and play in front of the public that same evening.
Despite desperately fighting his illness, on a rainy December morning in 1996, in Paris, the capital of his other homeland, the actor died. This is exactly how he spoke about France. On the front page of the Italian newspaper Republica a collage was published with Fellini, who had died a little earlier, depicted on a cloud and calling his favorite actor with the words “Come here, Marcello, it’s beautiful here.”
Patrick Swayze
Pancreatitis: probable mortality from the disease
Mortality due to inflammation of the pancreas accounts for 40 percent of all cases of acute inflammation of the pancreas. These are very high numbers, indicating the danger of this pathology, the need for timely diagnosis, treatment and prevention of pancreatitis.
Patients die due to severe acute inflammatory pathology or exacerbation of a chronic inflammatory process, with the development of severe complications:
- pancreatic necrosis;
- internal bleeding, especially in the case of its severe complication - hypovolemic shock;
- acute intoxication with decay products as a cause of infectious-toxic shock, often relevant for pancreatitis of alcoholic origin;
- abscesses, ulcers on the surface of the pancreas or nearby organs (omentum, liver, gall bladder, stomach), purulent inflammatory process in the ducts of the gland, when ruptured or spread, a serious condition develops - peritonitis;
- pain shock;
- pancreatic cancer due to long-term chronic pancreatitis.
If you do not seek medical help in time, do not diagnose these serious conditions in a timely manner and do not begin to treat the patient correctly, then the risk of death is very high.
Organ complications of pancreatic necrosis
Necrosis of pancreatic tissue without immediate emergency assistance leads to the release of a large number of enzymes into the vessels, causing them to dilate. Due to increased permeability of the walls, enzymes enter the intercellular spaces. The gland swells, hemorrhages appear in its tissues and retroperitoneal tissue, which leads to irreversible processes, among which the earliest and most common are:
- infiltrate;
- hemorrhagic effusion;
- peritonitis;
- retroperitoneal abscess or phlegmon.
Infiltrate
The development of parapancreatic infiltrate occurs not only in the gland, but also in neighboring organs. Affected:
- duodenum;
- stomach;
- spleen.
The process can spread to the gallbladder, liver, and cause changes in the lower intestines. They are soldered together with the participation of exudate, filling the upper part of the abdominal cavity or its entire space. The formation of an infiltrate is a reaction of the body’s immune system to necrotic tissue of the gland. The process itself is aseptic at this stage, there is no infection. Therefore it is possible:
- reverse development - resorption;
- formation of cysts;
- purulent option.
If the infiltrate does not disappear within 3 months, cysts appear. This is a warning of a possible serious complication.
The addition of infection leads to:
- to purulent lesions of the pancreas;
- peritonitis;
- abscess;
- phlegmon.
Signs of severe pancreatitis
Inflammation of the pancreas manifests itself in a variety of symptoms that significantly worsen the patient’s condition and reduce his quality of life, judging by their reviews. Diagnosis of the disease is often difficult due to the similarity of the symptoms of pancreatitis with other gastrointestinal pathologies, especially in children who cannot make complaints on their own. The main signs of severe complicated inflammation:
- Severe abdominal pain of different localization: in the peri-umbilical, hypochondrium region on the left or on both sides. Often the pain is girdling in nature, radiating to the lower back, right and left shoulder, and chest. The pain syndrome during an attack of pancreatitis can be so intense that it can lead to painful shock with impaired consciousness and the development of fatal multiple organ failure.
- Dyspeptic syndrome, manifested by several signs: nausea, vomiting, which does not bring relief, increased gas formation in the intestines, bloating, stool disturbances (more often in the form of diarrhea). Severe dyspepsia with prolonged profuse vomiting and diarrhea leads to dehydration of the patient and loss of essential microelements and vitamins. This is especially common when infusion therapy is insufficient or untimely. Dehydration of body tissues, lack of minerals (magnesium, potassium, calcium, iron and others) negatively affects the functioning of all organs and systems (especially the heart and blood vessels), and in severe cases it is life-threatening.
- General intoxication syndrome, manifested by many severe symptoms, indicating damage to all systems of the human body. The main signs of intoxication: increased body temperature, weakness, decreased blood pressure to the point of collapse, shortness of breath, changes (pallor, cyanosis, icterus) in skin color, headaches, dizziness, impaired consciousness and many others.
- Deterioration of laboratory and instrumental research data in the case of severe inflammation of the pancreas. The CBC reveals pronounced leukocytosis with pathological changes in the leukocyte formula, a sharp increase in ESR due to inflammation. Due to liver damage or the development of internal bleeding, anemia and thrombocytopenia may develop. According to the results of a biochemical blood test, the level of liver enzymes, amylase and other indicators indicating damage to the pancreas increases. When performing an ultrasound, CT scan of intra-abdominal organs, signs of edema, destruction of gland tissue, abscesses and other pathological changes are revealed.
Causes of death
We can safely say that the cause of death from inflammation of the pancreas is the carelessness of patients. They are forced to die from related problems arising from significant disruption of the functioning of all organs and systems. Some people develop pain shock, while others develop an abscess. Often in older people, the heart simply cannot cope with increasing loads. No one can predict how the disease will behave, but in a hospital setting under the strict supervision of highly qualified doctors, the patient has a much better chance of a quick full recovery and a long life.
If a patient is in critical condition, the main task of doctors is to stabilize him and remove him from the risk zone. This is achieved in different ways in intensive care conditions. At this time, minutes count, so you can’t hesitate. In order not to waste time, the fight against the main ailment begins there. doctors are doing everything possible to reduce inflammation of the pancreas and relieve the patient of pain. If they succeed, the patient is transferred to the gastroenterology department, where the further struggle for health continues.
Death from acute inflammation: how to prevent tragedy?
Acute pancreatitis develops most often due to alcohol abuse and fatty foods. It is very difficult and often leads to life-threatening complications.
Mortality statistics from acute pancreatitis state that 20% of patients with this diagnosis may die, especially in the absence of proper timely therapy.
In order to avoid tragedy, it is necessary to make a timely correct diagnosis and choose the right treatment tactics: surgical intervention according to indications or conservative treatment in the intensive care unit.
Early diagnosis
If a person is diagnosed with chronic pancreatitis, he is familiar with the symptoms of exacerbation and the need for urgent hospitalization in a hospital. With the development of acute pancreatitis, the condition can be underestimated. The slightest delay in medical care can lead to irreparable consequences (disability or death of the patient). Therefore, if you develop any digestive problems, acute abdominal pain, especially against the background of fever, or a deterioration in your general condition, you must consult a specialist or call an ambulance.
To establish a diagnosis, a doctor (gastroenterologist, therapist or surgeon) will conduct a survey to clarify the medical history of the disease, identify risk factors for the disease, and bad habits. Then the specialist will examine the patient and examine him using physical methods: palpation, percussion, auscultation.
To identify an acute inflammatory process, it is necessary to conduct a laboratory examination (CBC, OAM, biochemical blood test, coprological study). Instrumental methods for diagnosing pancreatic pathology will require ultrasound, CT or MRI, and x-ray examination of the digestive organs.
Prevention of pancreatic inflammation
To prevent the development of acute pancreatitis (primary prevention), as well as to prevent exacerbations of chronic inflammation of the pancreas (secondary prevention), all people are recommended to follow certain rules:
- Proper nutrition based on the principles of mechanical, chemical and temperature sparing of the mucous membranes of the digestive tract. Fatty, fried, salty, spicy, and sour foods are excluded. The temperature of food and drinks is within body temperature. Dishes are served to the patient in liquid, puree, or mushy form to facilitate digestion.
- Categorical refusal of bad habits (alcohol abuse, smoking) is one of the most important rules for disease prevention.
- Maintaining a healthy lifestyle, playing sports (specially selected gymnastics), frequent walks in the fresh air.
- Compliance with the work and rest regime, exclusion of heavy physical activity and stressful situations. Sleep should be at least 8 hours a day.
- Timely diagnosis and treatment of other gastrointestinal diseases. Gallstone disease, chronic cholecystitis, any pathology of the biliary system, gastritis, duodenitis are especially important for the development of pancreatitis. Taking prescribed medications in tablets or parenterally to treat concomitant pathologies is extremely important for the prevention of pancreatitis.
Disease prevention
Preventive measures make a significant contribution to preventing the development of pancreatitis and the occurrence of complications against its background. Experts advise adhering to a number of rules that will prevent inflammatory processes in the pancreas.
Refusal of alcohol abuse. It has long been known that alcohol causes irreparable harm to the organ responsible for the production of enzymes. Regular ingestion of ethyl alcohol into the body causes various changes in the pancreas: swelling, formation of stones, pancreatitis, necrosis, etc. It is for this reason that doctors advise minimizing the consumption of alcoholic beverages, and in the best case, eliminating them completely.
To give up smoking. Toxic substances and nicotine that are part of tobacco smoke have a negative effect on absolutely all human organs, including the pancreas. This effect is especially enhanced by the simultaneous combination of alcohol and smoking - irritation of the mucous membranes of the gastrointestinal tract and inflammation of pancreatic cells occurs, which inevitably leads to the development of an inflammatory process of the pancreas, called pancreatitis.
Proper nutrition is an important factor on which the health of all organs and systems depends. Fatty foods, spicy and salty dishes, carcinogenic foods - all these are foods that have a detrimental effect on the condition of the pancreas. Regular consumption of such food not only provokes damage to the cells of the organ, but also significantly reduces the chances of its further recovery. Nutritionists and gastroenterologists advise taking easily digestible foods as the basis of the diet, which will not put a strain on the pancreas, but at the same time will become an excellent lever to maintain the health of this organ at the proper level.
A healthy lifestyle is another component of the normal functioning of the pancreas. Daily stay in the fresh air, moderate physical activity, proper sleep and rest, avoidance of stressful situations - these are the basic measures that will help avoid dangerous and terrible diagnoses.
You shouldn’t write off traditional medicine recipes either. Healing plants and substances such as mantle grass, walnut leaves, chamomile, calendula, potato juice, royal jelly, corn silk, dill or flax seeds will be excellent helpers in protecting the body from pancreatitis.
Inflammation of the pancreas and various complications of this disease are a serious pathology that has claimed the lives of many people, including celebrities. In most cases, the disease manifests itself suddenly; cancer of this organ, often occurring against the background of inflammatory processes, is particularly insidious.
A malignant tumor can progress for years in the human body without showing any signs
This is why it is so important to undergo annual medical examinations and monitor your own health.
Main causes of death from pancreatitis
Mortality due to inflammation of the gland depends on its type (etiology, pathogenesis, symptoms of the inflammatory process).
Alcoholic pancreatitis
Among those who died from alcoholic pancreatitis, many were young; this diagnosis was especially often given to men, since they are the ones who most often suffer from alcoholism.
Regular consumption of ethanol leads to toxic damage to the cells of parenchymal organs - liver, pancreas.
Alcoholic pancreatitis is characterized by the development of necrosis of the pancreas and disruption of its functions.
Acute pancreatitis
The statistics of death from acute pancreatitis with severe symptoms is considered the highest. Death occurs within the first week from the onset of the disease, sometimes even with timely initiation of therapy. The main conditions in which a patient dies due to acute pancreatitis are considered to be massive necrosis of the pancreas and internal bleeding.
Chronic pancreatitis
A long-term chronic inflammatory process in the pancreas is considered not as dangerous as an acute one. But, due to the inevitable damage to the organ during exacerbations, it is impossible to completely exclude the development of severe complications. In addition to death, during an exacerbation of the disease, death is also possible due to the development of a malignant tumor in the pancreas and the progression of cancer to stage 3-4, which cannot be cured.
Hemorrhagic pancreatitis
Inflammation of the pancreas, accompanied by bleeding, is a very dangerous pathological condition. It develops when the wall of a vessel is damaged due to the possible influence of pancreatic enzymes on it.
If internal bleeding (especially from a large artery) is not diagnosed in time and abdominal surgery is not performed, blood loss can quickly become massive, hemorrhagic shock will develop, and the patient will die.
Pancreatic necrosis
Necrosis (destruction) of pancreatic tissue occurs for various reasons. Most often this happens due to acute destructive pancreatitis that develops after abuse of alcohol or junk food. Due to inflammation, swelling of the gland or the presence of stones in the excretory ducts, their lumen decreases, and pancreatic juice, aggressive to any tissue, remains inside the pancreas itself. Proteolytic enzymes destroy the gland and adjacent organs.
With the lightning-fast course of pancreatic necrosis and untimely provision of assistance to the patient, death is almost inevitable.
Death after pancreatic resection
For the formation of abscesses, ulcers, fistulas, and the development of pancreatic necrosis, surgical intervention is considered the only effective treatment. The operation is performed in several ways. The volume of intervention depends on the degree of damage to the pancreas: excision of necrotic tissue, resection of one section or (less often) the entire organ. But even after successful surgical treatment, death is also possible for several reasons:
- Postoperative bleeding.
- Reactive postoperative pancreatitis.
- Infectious complications and postoperative peritonitis.
- Diabetes mellitus, its complications (hyperglycemic coma and others) due to incorrectly selected insulin replacement therapy or the patient’s failure to comply with the recommendations of the attending physician.
What leads to death in pancreatitis?
Such an unfavorable prognosis depends on many factors: the severity, pathogenesis, nature and type of the disease, as well as the severity of the symptoms that appear in the patient.
- Alcohol abuse. This circumstance is the cause of death of people at a young age, especially for men, since they are the ones most susceptible to alcohol dependence. The mechanism of this connection is quite simple. With the regular intake of ethanol into the body, intoxication of organs such as the pancreas and liver occurs, as a result of which their tissues are inevitably destroyed. As a consequence, necrosis occurs, that is, the death of those structures in which the lesions are localized. The combination of alcohol and fatty foods becomes a real rocket bomb, which is why the majority of attacks, including fatal ones, occur during the holidays.
- Acute pancreatitis is the most common cause of death. The pathology in its acute form is quite complex; the patient experiences severe symptoms of a pronounced nature: severe pain in the abdominal area, incessant vomiting, diarrhea, and physical exhaustion. The first week of an exacerbation is a rather difficult period for the patient, during which various kinds of complications can arise, for example, necrosis and internal bleeding, and against their background - death. It is noteworthy that this can happen even after a timely diagnosis and the start of proper treatment.
- Chronic pancreatitis. In itself, this form of the disease is not as dangerous as the acute phase. However, it is characterized by periods of remission, which sooner or later give way to exacerbations, accompanied by the same severe symptoms. In addition, in conditions of a sluggish ongoing inflammatory process, the risk of developing complicating factors increases significantly: it can be either a cyst or a malignant tumor.
In general, the onset of death is preceded by:
- Changes in the cellular structure of the pancreas with subsequent necrotic processes;
- The penetration of enzymes into the blood vessels located near the organ, which occurs due to the impossibility of the outflow of pancreatic juice into the duodenum and its forced search for an outlet - as a result, enzyme substances are carried throughout the circulatory system and the patient dies.
Sometimes such a destructive process only takes a few days or even hours to take a person’s life.
What are the prognosis for a favorable treatment outcome?
Timely seeking medical help and timely initiation of treatment increases the patient’s chance of recovery or stabilization of the condition. A favorable outcome after pancreatitis depends on many reasons:
- severity of the disease, severity of complications of inflammation;
- the age of the patient (the older the person, the harder it is for him to recover from pancreatitis or surgery for pancreatic pathology);
- the presence of concomitant diseases in humans (endocrinological, neurological, cardiovascular, gastrointestinal and others);
- qualification of the attending physician;
- patient adherence to therapy, compliance with preventive measures.
Pathology of the pancreas rarely goes away without a trace. Dangerous complications of the inflammatory process (pancreatic necrosis, internal bleeding, severe intoxication and others) can lead to the death of the patient. In order not to be afraid of a tragic outcome, the patient needs to pay attention to his condition in a timely manner and seek medical help. Prevention of the disease is extremely important, especially to prevent exacerbations of chronic pancreatitis.
Is it possible to die from pancreatitis? This question is asked by many people who have been diagnosed with this disease. To better understand the consequences of the disease, patients need to carefully study information about it. The article describes the causes and characteristic symptoms of the pathology, as well as how to avoid complications.
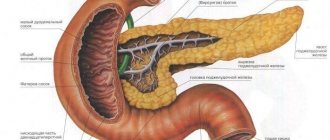
What functions does the pancreas perform?
This small organ, similar to a willow leaf, is very important for normal human life.
It is necessary to carry out the following tasks:
- Excretion of juice to process nutrients.
- The production of hormones that affect the cells of the human body. The main one is insulin. This substance regulates the concentration of glucose in the blood.
As a result of inflammatory processes, the activity of the organ is disrupted. Is it possible to die from pancreatitis? This question is quite natural, since the condition of almost all systems of the human body depends on the health of the pancreas.
Diagnostics of pancreatitis
When conducting diagnostics, various methods are used to identify pathology.
When conducting a general blood test, an increase in ESR is detected, the number of leukocytes in the blood increases, in addition, other signs of an inflammatory process in the patient’s body are observed in the blood. Additionally, a glucose test is performed.
Carrying out a biochemical blood test allows you to determine the degree of activity of amylase, trypsin and other enzymes produced by the pancreas.
A urine test can reveal the presence of an inflammatory process in the body.
Analysis of feces makes it possible to identify the presence of undigested residues and inclusions of fat in them, which indicates a violation of the digestive processes.
The use of ultrasound of the abdominal organs reveals the presence of pathologies in the gland and changes in its structure and size.
In addition, if necessary, the attending physician will prescribe the following examinations to clarify the diagnosis:
- abdominal radiography;
- esophagogastroduodenoscopy;
- endoscopic retrograde cholangiopancreatography.
The choice of treatment method is made by the attending physician after a complete examination of the body and receipt of the examination results.
Potential danger of the disease
Experts say that in recent years they have often encountered cases of death in patients with this disease. In 40% of people suffering from acute pancreatitis, the pathology leads to death. The disease affects people of both sexes equally. However, the greatest likelihood of its occurrence is present in middle-aged and elderly men who regularly drink alcohol.
The answer to the question of whether people die from pancreatitis is generally positive. As a rule, death occurs in the first week of an acute attack. The most dangerous are hemorrhagic and mixed types of the disease. Some people believe that pancreatitis is a common ailment of the digestive system and take their health lightly. However, inflammation of the pancreas is not a common pathology. It can provoke serious complications. Only regular examinations and compliance with all the specialist’s instructions can protect a person from tragic consequences.
Is it possible to die from pancreatitis: how long do patients live, the likelihood of death
Pancreatitis is a serious disease of the pancreas that involves tissue destruction. To a greater extent, inflammation occurs due to alcohol abuse. Typically, tissue breakdown progresses even if the patient stops drinking.
It is difficult to answer the question of whether the mortality rate from pancreatitis is high. The answer depends on the factors influencing the individual patient's life expectancy. You can live with this diagnosis if you treat your health carefully and carefully.
The organ is small in size, shaped like a willow leaf and exhibits two important functions:
- takes part in the digestion of food thanks to digestive juices;
- produces hormones that affect cells in the human body.
Insulin, which controls sugar levels, has become the main pancreatic hormone.
There are two types of pathology - chronic and acute pancreatitis.
Chronic pancreatitis manifests itself due to the acute form of the disease. The disease progresses over the years, becoming more and more deformed.
In the acute form, inflammation of the organ occurs almost instantly. The form of the disease is rare. At risk are more often male patients aged forty to fifty years. Chronic alcoholism is often a risk factor for this pathology.
Cause of death
Can a patient die from pancreatitis? In recent years, deaths from such a diagnosis have occurred less frequently—there are more opportunities for treatment.
The prognosis of chronic pancreatitis largely depends on the stage of the disease. In the first stage, death from pancreatitis occurs less frequently. In the third stage, death is more common. If pancreatitis is not treated, the prognosis is likely to be fatal.
Alcoholic pancreatitis develops due to alcohol abuse. The type and cost of alcohol does not affect the course of the disease. You can get sick from both beer and expensive cognac if you drink regularly.
In chronic pancreatitis, mortality has been recorded for twenty years. During this period, half of the population suffering from pancreatic disease dies. Moreover, people of mature and young age have to die. The causes of death are not the disease, but the diseases that appear due to alcohol abuse.
As a result of alcohol entering the body, pancreatic cells are deformed. The cause is substances formed during the breakdown of ethyl alcohol or surrogates.
Pathogenesis
Cell deformation occurs through the activation of enzymes produced directly by the gland. Then the enzymes act on the organ itself.
The result is necrosis, the death of large areas. The gland becomes inflamed and increases to pathological sizes.
The pancreatic tissue is deformed and replaced by fat cells, destroying the endocrine system. Diabetes develops due to pathology.
The functions associated with the functioning of the pancreas are interconnected. It is impossible to say that the patient died from pancreatitis without finding out the true cause of death.
The pathology is divided into two stages - acute and chronic. As a result of one-time consumption of alcohol in large doses, intoxication of the body occurs. This happens in the acute form of the disease. Signs of the acute form of the disease are similar to those of a conventional diagnosis.
The causes of chronic pancreatitis are mostly due to alcohol abuse. Symptoms of this type of disease may not appear for a long time. If you drink alcohol in small doses but regularly, the disease progresses daily. With chronic pancreatitis, patients live without realizing the presence of the disease for many years.
During attacks of pain, many patients complain of acute pain in the upper abdomen, arising in the back and hypochondrium. Painful sensations intensify in the “lying on your back” position.
Due to impaired absorption of nutrients into the body, patients experience a sharp weight loss. To avoid death, you need to consult a gastroenterologist.
Complications that arise lead to the formation of cysts and abscesses. With pancreatitis, if the disease is not treated, adenocarcinoma, pancreatic cancer, develops. The result of the pathology is often fatal.
Treatment of the disease occurs under the strict supervision of a number of doctors. Professionals in the field of gastroenterology, endocrinology, and surgery are considered competent. In severe cases, ask for help from a radiologist or psychotherapist.
The main condition for effective treatment is the exclusion of alcoholic beverages from the diet. You cannot drink beer or other low-alcohol drinks.
The prognosis of chronic pancreatitis is often unfavorable. Pancreatic necrosis, or death of gland cells, is especially difficult to treat. A fatal outcome in the described case is likely.
To avoid tragedy, patients need to clearly understand that the causes of chronic pancreatitis depend on the quality of food. When diagnosed, you should not drink alcoholic beverages or eat fatty foods. The diet includes protein (mandatory) and a minimum amount of fat.
How long do people with pancreatitis live is a question that worries every sick person. Life expectancy is influenced by a number of reasons:
- Patient's age. The earlier a person gets sick, the higher the chance of recovery.
- Drinking pattern - how often ethanol is consumed.
- The degree of damage to the gland.
A young guy who recently turned 20 years old and does not drink alcohol can live with this diagnosis into old age. A man in his declining years who regularly drinks alcohol shortens his life by ten or more years.
Factors influencing life expectancy:
- Life expectancy depends on the form of the disease. Acute attacks are often fatal. In severe forms, death from pancreatitis occurs in thirty percent of patients.
- The severity of the disease affects the general condition of the body.
- Complications in the form of cyst formation, bleeding from a damaged organ, and problems with the gastrointestinal tract aggravate the situation, mainly in older patients. The mortality rate reaches 20%.
- Age category of patients.
- Regular, thoughtful treatment.
- Compliance with the doctor's requests for treatment.
- Consumption of products prescribed by a gastroenterologist.
- Refusal to drink strong and low-alcohol alcoholic beverages.
This pathology is characterized by the death of pancreatic tissue. As a rule, with this type of disease, the mortality rate among patients is high. The cause of the disease is surgical interventions, various wounds and injuries, and alcoholism. With pathology, a sharp enlargement of the gland occurs, resulting in hemorrhage and the formation of blood clots.
If acute hemorrhagic pancreatitis is suspected, patients feel chills and the temperature rises. Vomiting and weakness in the body appear. Pain sensations radiate to the shoulder blades and back. Sometimes the pain reaches the heart area.
As a result of pressure on the front of the abdomen, acute pain occurs. Most patients with this type of disease are in serious condition. If treatment is not provided in a timely manner, the patient runs the risk of dying.
Causes
Why do people die from pancreatitis? First of all, it should be remembered that the disease can lead to a process of tissue damage. In many cases, inflammation of the pancreas is associated with excessive consumption of products containing ethanol. Further destruction of the organ is observed even if the person gives up the addiction. However, addiction to alcohol is not the only cause of the disease.
Other factors contributing to its occurrence include:
- Excessive amounts of fatty foods in the diet.
- Eating large amounts of food.
- Physical inactivity.
- Taking medications.
- Mechanical damage to the peritoneum, surgical interventions.
- Viral pathologies of the liver.
- Mumps.
- Parasitic infestations.
- Hormonal imbalance.
- Presence of pancreatic tumors.
- Pathological processes in the intestines.
- Stones in the gall bladder.
- Emotional overload.
- Passion for strict diets.
- Bad heredity.
Is it possible to die from pancreatitis? How long does a person with this pathology live? Patients are often interested in these questions, but they cannot be answered accurately. The prognosis is determined by the influence of many factors. One of them is the patient’s attitude to his state of health.
How to save a patient's life?
In acute pancreatitis, death occurs from collapse (a sharp drop in blood pressure and disruption of the blood supply to all organs) and painful shock.
The very first thing you need to do is call an ambulance!
While the ambulance is traveling, the condition can be alleviated using the following measures:
- lie in a horizontal position (on your side if possible);
- take an antispasmodic (No-shpa, Drotaverine);
- stop eating;
- place a cold object or ice on the pancreatic area.
Thus, first aid consists of observing 3 rules: cold, hunger and rest. A person with signs of acute pancreatitis should be urgently hospitalized. In inpatient conditions, diagnostics are carried out and a treatment regimen is formed. If destructive processes during pancreatitis have affected not only the pancreas, but also neighboring organs, the only chance to avoid death is surgical intervention.
Partial or complete resection of the pancreas is performed, the patency of blood vessels and bile ducts is restored, and tissue drainage is performed.
At the recovery stage, treatment with enzyme preparations and vitamin therapy is prescribed. The patient must follow a special diet for life. You will have to give up bad habits forever. Many diseases, including pancreatitis, occur with physical inactivity and obesity. Movement is life. The patient must remember this constantly after discharge from the hospital. Bringing your weight back to normal and increasing physical activity to the best of your ability are the top priorities on the path to recovery.
podzhelud.ru
Varieties of the disease
There are several categories of pancreatitis. The disease can be primary, secondary, acute and chronic. The latter type, in turn, is divided into periods of deterioration and remission. Signs of pathology and their intensity depend on its type. The chronic type occurs against the background of an acute illness. In this case, the patient’s condition gradually worsens, and the tissues undergo a process of decay. Another type of pathology is quite rare. This is an inflammation of the pancreas that has an acute course. The disease is usually diagnosed in middle-aged men. The main reason for its development is the systematic consumption of alcohol-containing drinks.
People with alcohol dependence have a high probability of dying from acute pancreatitis. This is especially true for those patients whose disease was diagnosed at a late stage.
Inflammation of the pancreas associated with alcohol consumption
Alcoholic drinks have a detrimental effect on the condition of the entire body, including the digestive system. The type and cost of such products do not affect the likelihood of the disease occurring. Pancreatitis can develop both from cheap beer and from expensive liquor or cognac. The main factor contributing to the development of pathology is the regularity of alcohol consumption. Is it possible to die from chronic pancreatitis caused by alcohol addiction? The answer to this question is definitely yes. According to statistics, many people who have a craving for alcohol die as a result of complications.
Features of the acute course of the pathology
This type of disease is characterized by the fact that the pancreas begins to destroy its own tissue. This process is accompanied by inflammation. Symptoms of acute pathology may vary depending on factors such as the patient’s age, the presence of diseases of the myocardium, liver, brain, kidneys, general condition and external influences. One of the first signs of pancreatitis is pain.
The discomfort can be so severe that the person loses consciousness. Unpleasant sensations become more intense after eating or coughing. A person experiences pain of the girdling type, which radiates to the back, shoulder blades, right and left hypochondrium, and chest. Patients often confuse the manifestations of pancreatic pathology with myocardial diseases and inflammation of the gallbladder. A symptom characteristic of the acute type of pancreatitis is vomiting, which further worsens health. Bile is found in the contents of the gastrointestinal tract. The patient has a fever. In the later stages of the disease, central nervous system disorders are possible, which are expressed in anxiety, hallucinations, and tremors of the limbs. Do people die from acute pancreatitis? A high probability of death is present in elderly patients suffering from concomitant pathologies.
Development of pathology as a result of injury to the gland
As a result of injury, the organ may suffer a tear or rupture; in such a situation, only a formed cyst, which has been located in the tissues of the organ for a long time, can burst. As a result of injury, enzymes produced by the gland begin to destroy the tissue of the organ. In the event of such an injury, it is very difficult to stitch the tissue tear.
Stitching a damaged gland is an emergency surgical procedure. The location of the gland provides it with relatively reliable protection from external traumatic influences.
The organ is protected by the abdominal muscles, the organs of the abdomen. Spine, back muscles and lumbar muscle structures.
The main cause of open injuries is penetrating wounds with sharp piercing objects, as well as as a result of gunshot wounds. When injured, thrombosis of the veins surrounding the organ occurs, and the gland tissues swell; thrombosis, which develops very quickly, leads to the development of necrosis.
If the head and body are damaged, the tail does not undergo necrosis, since this part of the organ has an autonomous blood supply.
When the gland is injured, a sharp deterioration in health occurs, the reason for this deterioration is the development of acute pancreatitis against the background of injury.
If a complete rupture of the organ occurs, suturing the main duct is almost impossible.
Other manifestations of the disease
There are several indirect symptoms of this pathology. These include the following:
- Yellow coloration of the skin. This symptom is due to the fact that the volume of the pancreas increases during inflammation. The organ compresses the liver ducts. In addition, the symptom may appear as a result of the formation of stones in the gallbladder and the simultaneous development of pancreatitis.
- A bluish tint to the skin. The sign is typical for patients with diseases of the heart muscle. It is accompanied by respiratory disorders. At the same time, the face, arms, and legs are painted blue. If such a shade is observed in the area of the upper peritoneum and left hypochondrium, it can be argued that the patient is in serious condition.
- Paleness of the skin. It indicates the development of a state of shock, intoxication, bleeding and ulcers in the digestive organs.
- Formation of swelling in the upper part of the peritoneum, bloating.
- Blood pressure fluctuations. At the beginning of the attack it is slightly elevated, and then decreases greatly. As the symptoms of chronic pathology develop, an acceleration of the heart rate, a decrease in body weight, a feeling of weakness and loss of appetite are observed.
Chronic course of the disease
This form of the disease occurs as a result of exposure to various factors. This condition is characterized by the gradual destruction of the pancreas, transformation of its tissues, and the formation of stones and cysts. As a result of these processes, the organ cannot function normally and nutrients are not absorbed. In addition, insulin production is disrupted, which often causes the development of diabetes.
Is it possible to die from pancreatitis of the pancreas that has a chronic course? The probability of death with this type of pathology is quite high. The disease is quite insidious. Sometimes patients do not pay attention to the occurrence of discomfort in the upper part of the peritoneum and attribute the deterioration in health to the consumption of fatty foods and alcoholic beverages. However, pathology can lead to sad consequences, for example, the development of a malignant tumor.
What can cause acute hemorrhagic pancreatitis?
This pathology is characterized by the death of pancreatic tissue. As a rule, with this type of disease, the mortality rate among patients is high. The cause of the disease is surgical interventions, various wounds and injuries, and alcoholism. With pathology, a sharp enlargement of the gland occurs, resulting in hemorrhage and the formation of blood clots.
If acute hemorrhagic pancreatitis is suspected, patients feel chills and the temperature rises. Vomiting and weakness in the body appear. Pain sensations radiate to the shoulder blades and back. Sometimes the pain reaches the heart area. As a result of pressure on the front of the abdomen, acute pain occurs. Most patients with this type of disease are in serious condition. If treatment is not provided in a timely manner, the patient runs the risk of dying.
Pancreatitis is a disease whose course can be controlled. If you follow doctors' recommendations, there is no risk of death. Among other things, you need to monitor your emotional state, follow healthy eating rules, avoid stressful situations and undergo scheduled examinations on time. It is possible to live with such a diagnosis if the patient has a desire to live.
Methods of diagnosis and therapy
In order to identify this disease, the following medical measures are taken:
- Biomaterial analyses.
- Assessment of the condition of the peritoneal organs using an ultrasound machine.
- Examination using an endoscope.
The answer to the question of whether people die from pancreatitis largely depends on how timely diagnostic measures were carried out. If the patient consults a doctor at an early stage of the development of pathology, he can avoid such consequences as necrosis of organ tissue and acute inflammation of the peritoneum, which leads to death.
As for therapy, it involves the patient staying in a hospital. For about a week, the person is under the supervision of specialists who give him medications and put on IVs to eliminate intoxication. After discharge, you must strictly adhere to the diet recommended by the doctor. You should avoid fresh bread, raw vegetables, and strong broths. Patients need to eat cottage cheese, lean meat, cereals, and some types of fish.
It is recommended to eat often, but in small portions. It is also necessary to take tablets and herbal decoctions prescribed by the doctor.
Complications and severe forms of the disease
After diagnosing acute pancreatitis, improper treatment and ignoring the diet leads to the development of a number of complications, one of which is pancreatic necrosis. This disease is also called “the disease of decent people”, since it does not develop against the background of frequent alcohol consumption, but becomes a consequence of heavy feasts. So, if a few days after a satisfying birthday or holiday you experience nausea, vomiting, rapid heartbeat, accompanied by shortness of breath, immediately call an ambulance.
Purulent inflammation of the pancreatic ducts is also a common cause of death. In this case, pus entering the blood and abdominal cavity leads to intoxication, and the proper functioning of internal organs becomes impossible. As a result, a rapid deterioration of the patient’s condition, without emergency intervention, leads to multiple organ failure (impaired functioning of more than two organs) and death. The entry of pus into the bloodstream provokes sepsis (blood poisoning), which also threatens death.
Against the background of chronic forms of pancreatitis, pancreatic cancer can develop. Ignoring the symptoms of pancreatitis does not allow cancer to be diagnosed on time. And unfortunately, when a patient consults a doctor with a deterioration in his condition, the cancer may no longer respond well to treatment or may not respond at all.
One of the possible consequences of an acute attack of pancreatitis may be blockage of the veins that supply the liver and spleen. This disrupts the functioning of organs, provokes the death of liver tissue and liver failure. A number of these complications lead to cirrhosis and portend death. Perhaps, in most cases, liver cirrhosis and high mortality from it arise from periodic attacks of pancreatitis.
Surgery
Many patients are admitted to the hospital with a diagnosis of acute pancreatitis. Is it possible to die from this pathology? The answer to this question depends on how timely and competently the assistance was provided to the patient. If there is a threat of death, surgery is performed. The surgeon drains and excises dead organ tissue. The person is then transferred to the intensive care unit where other treatments are used.
In the later stages of the disease and in acute cases, it is difficult to answer the question of whether it is possible to die from pancreatitis of the pancreas. Even after surgery, there is a possibility of renewed tissue necrosis.
Reasons for the breakup
All the reasons why the pancreas ruptures can be divided into three main categories. These include:
- Open injuries . They most often lead to a violation of the integrity of the organ. Their cause can be a gunshot, stabbing or cutting wound, or an accident. In this case, rupture of nearby tissues and organs often occurs.
- Closed. They are caused by a strong blow to the body, squeezing it with damage to the gland from fragments of the ribs or spine. The second internal factor is oncopathology, gastric ulcer or embolism. Most often in this case, the body of the pancreas suffers.
- Operating rooms. Appear after surgical treatment of the gland itself or nearby organs (gastric resection, removal of the spleen or cyst, biopsy). Such cases occur extremely rarely and are explained not by a surgeon’s error, but by the high sensitivity of the organ.
These are not all the reasons why the pancreas can burst. But it is they who most often lead to a violation of its integrity. There are also isolated and combined organ lesions. In the latter case, several internal organs are injured at once.
What does the forecast depend on?
Life expectancy is determined by the following factors:
- Age category.
- Degree of tissue damage.
- Frequency of use of products containing ethyl alcohol. If a person has an alcohol addiction, the answer to the question of whether it is possible to die from pancreatitis will be more likely to be affirmative than negative.
- Type of pathology.
- Complications.
- Compliance with doctor's orders.
The question of whether you can die from pancreatitis is largely determined by a combination of these factors.
Индивидуалки встречаются с воспитанными джентльменами для взаимного и приятного отдыха, реальные феи Владивостока, очень любят пошалить. Проявите фантазию и развлекитесь с проституткой по полной. Изящные реальные феи Владивостока, горячие и прелестные, они такие интересные и стройные, что у любого появится желание. Не упусти свой шанс.