The small intestine of each person is inhabited by an individual set of microorganisms responsible for digestive processes and the activity of the immune system. Dysbacteriosis (dysbiosis) is a change in the ratio of these microbes. According to the international classification of diseases, this condition is not considered a pathology.
Dysbacteriosis in infants - causes
During intrauterine development, the baby's intestines are completely sterile. During childbirth, the first microorganisms (from the mother) enter it. Their number and variety gradually increases thanks to breastfeeding, kissing and touching. These microbes form the normal microflora of the small intestine. Dysbacteriosis in a child can develop in the following cases:
- taking antibiotics (by a woman or a child);
- infections;
- lack of breastfeeding;
- late application;
- surgical interventions;
- prematurity;
- rickets;
- malnutrition;
- primary immunodeficiency;
- anemia and other unfavorable factors.
Is dysbiosis possible in a newborn?
This diagnosis is often made in newborns and children in the first month of life. In what cases is this justified?
- Late breastfeeding. Breast milk is a source of bifidobacteria and the best prevention of dysbacteriosis. About a week after the first breastfeeding, about 95–98% of beneficial milk bacteria are found in the newborn’s intestines. If for some reason breastfeeding begins later or does not begin at all, the intestines become colonized with opportunistic bacteria. It cannot be said that dysbacteriosis immediately develops. Rather, the preconditions are being created for further disruption in the microflora.
- Forced use of antibiotics. Unfortunately, there are situations when a baby cannot do without antibiotics. Then you have to choose the lesser of two evils - side effects during treatment with antibacterial drugs. Broad-spectrum antibiotics are the most destructive to the newborn's microflora. If antibiotic therapy is carried out while breastfeeding, the intestinal microflora is restored much faster. One conclusion can be drawn: a woman should try to maintain breastfeeding for at least six months.
All other reasons are not significant and do not deserve attention. Mom has so much trouble and worry that she shouldn’t bother herself with a non-existent diagnosis.
Dysbacteriosis in a child - symptoms
It is impossible to reliably detect the condition in question in an infant. Modern doctors emphasize that dysbiosis in a newborn is an incorrect diagnosis. The microflora in babies is just beginning to form, so it is wrong to draw any conclusions about its condition. Quantitative and qualitative indicators of intestinal biocenosis are very individual and constantly changing; they cannot be adequately assessed even in an adult.
In severe cases of microflora disturbance, its obvious signs appear, but in this situation they speak of acute bacterial infections, and not dysbiosis. Specific symptoms of pathology:
- unpleasant oral odor;
- excessive secretion of saliva;
- allergic dermatitis;
- vomit;
- increased body temperature;
- slow weight gain;
- anxiety;
- frequent diarrhea followed by constipation;
- stomatitis;
- candidiasis of the oral mucosa;
- lethargy;
- lack of appetite.
It is important not to confuse an intestinal infection with the standard adaptation of the baby’s digestive system to new conditions. The following manifestations are quite normal for a baby:
- yellow, greenish, brown and dark feces;
- the presence of a small amount of mucus, foam and bloody streaks in the feces;
- short-term bloating and flatulence;
- regurgitation after feeding;
- periodic colic in the intestines;
- frequent changes in the consistency and quantity of bowel movements.
What tests are given to a child for dysbacteriosis?
Gastroenterologists and pediatricians prescribe laboratory testing of the contents of the diaper. The classic stool test for dysbacteriosis in infants is considered not very informative, and some progressive doctors call it absolutely meaningless. The necessary microorganisms are located on the parietal mucous membranes of the intestine. They ensure normal digestion of food and absorption of beneficial chemical compounds into the blood. Feces are formed in the intestinal lumen from waste food debris.
Testing for dysbacteriosis in infants has one more drawback - upon contact with air, which inevitably happens when collecting feces, most anaerobic microbes die. Their concentration in the results of a standard bacteriological study is always underestimated and does not reflect reality. If the material was delivered to the laboratory later than the recommended time, there will be no anaerobic microorganisms left in it.
A more informative analysis is a biochemical study of feces. During its implementation, bacteria are not counted, but the concentration of their metabolic products is determined. All microbes secrete metabolites of volatile fatty acids (propionic, acetic, butyric). Having determined their volume, we can assume a qualitative and quantitative relationship between the microflora.
What does the analysis show?
A transcript of the stool test for dysbacteriosis is issued after 7 days. The long processing time is due to the technical features of the study: the sample is placed in an environment whose characteristics are ideal for the growth of bacteria. Within a few days, colonies of microorganisms grow. The material is then examined under a microscope, and a laboratory assistant counts the number of representatives of each strain.
The final transcript contains indicators reflecting the number of colony-forming units of bacteria per 1 gram of feces (CFU/g). The form contains information on the number of E. coli, bifidobacteria, lactobacilli, enterobacteria, Klebsiella, fungi, and so on. In addition, the resistance of microorganisms to various pharmacological substances is tested.
Interpreting the results of an analysis for dysbacteriosis in an infant is the doctor’s task. Let's consider the meaning of the main indicators.
How to get tested for dysbiosis in a baby?
For the procedure under consideration, it is necessary to bring to the laboratory the freshest possible morning stool obtained no earlier than 2 hours before. How to get tested for dysbacteriosis in a child:
- For 4-7 days before collecting the material, do not introduce new foods into the baby’s diet.
- Temporarily avoid taking any medications, especially those affecting digestion. Do not administer suppositories or give enemas.
- Collect at least 8-10 g of feces.
- Place it in a special sterile container with a lid.
- Take the feces to the laboratory immediately. If it's hot outside, use a cool pack or bag.
Test for dysbiosis in infants - how to collect?
In this case, it is not advisable to donate feces from a disposable diaper. Pediatricians recommend performing an analysis for dysbacteriosis in infants using the most pure biological material without impurities. To do this, you will need certain equipment and the attentiveness of parents. How to properly test for dysbacteriosis in an infant:
- If the baby poops at a certain time, it is necessary to remove his diaper during this period and put him on a clean oilcloth. After bowel movement, collect feces.
- Massage, gymnastics (bending the legs towards the navel), and laying on the stomach will help speed up the process of defecation.
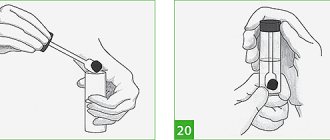
- When your baby has problems with bowel movements, you will have to stimulate him. It is necessary to place the child on a clean oilcloth and insert a sterile gas outlet tube 0.5-1 cm into the anus. The end of the device is lubricated with petroleum jelly. A bowel movement should occur within 3-5 minutes.
- The resulting biomaterial is collected with a spoon, which comes with the medical container.
How to take the test correctly?
Tests for dysbacteriosis can be taken both in public clinics and in private laboratories. At the same time, parents should remember that public medical institutions have their own opening hours and do not conduct research on weekends.
A stool sample is collected from a baby who has already passed a baby. It is important that urine particles do not end up in the test container. It is advisable to thoroughly wash the child’s bottom before collecting the material.
You need to take at least 10 milligrams of stool for analysis - it is sent to a sterile jar, which can be purchased at a pharmacy. It is recommended to take stool particles from various parts of the deposit. If certain impurities are detected, it is also recommended to send them to the container in order to find out about the composition of these particles during analysis and make sure that they are safe.
If a homemade jar for feces is used, it must be sterilized - just bake the container in the oven. After sending the feces there, you need to tightly close the jar with a lid so that no external bacteria get inside.
Stool jars
The rules for preparing for a stool test for dysbacteriosis are simple, but they must be followed. If you miss or ignore some point, the information content of the study can be significantly reduced.
We invite you to familiarize yourself with Regidron bio for children from one year old
A baby’s feces cannot be submitted for examination “right now,” as certain preparation is required.
| What not to do | What to do |
|
|
Preparing containers
For storage and transportation, you need to either purchase a ready-made container at the pharmacy, or find a glass jar with a tight lid in your household. A cardboard box will not work. The pharmaceutical container does not need to be processed, but the home jar needs to be thoroughly washed, boiled and dried under natural conditions.
Collection of material
It is necessary to collect baby feces from a clean diaper or disposable paper napkin. Collecting diapers, potties, and plumbing equipment from the membrane is not allowed. There should be no urine in the stool.
A small volume is sufficient to successfully complete the analysis. This is approximately 20-25 g, that is, an amount equal to a tablespoon.
We recommend reading:
Steatorrhea: types, causes, symptoms and treatment
For research, a portion of feces is suitable, which is collected in the morning on the day of the study or, in extreme cases, in the evening, stored under certain conditions.
The less biological material is stored, the better, since when it comes into contact with the air, some bacteria (anaerobic) die. The collected biological fluid (already in a transport container or jar) can be placed in the refrigerator on the middle shelf away from the freezer. The storage period should not exceed 7-8 hours (night time).
Analysis of stool for dysbacteriosis - interpretation in children
A specialist must explain the results of laboratory tests; independent attempts to do this and start treatment will not lead to anything good. Parents should not take the test for dysbiosis in their infants too seriously - deciphering the composition of feces does not reflect the real state of the flora in the intestines. While the biocenosis is in the process of formation, even pathogenic microorganisms can be present in the baby’s feces without harming the baby’s health.
Interpretation of the analysis for dysbiosis in infants - norms
It was mentioned above that the composition of the intestinal microflora is individual and in the case of young children its determination is meaningless. These indicators are provided for informational purposes. Laboratory standards for testing for dysbiosis in infants:
- lactobacilli – 106-107;
- bifidobacteria – 1010-1011;
- Escherichia – 106-107;
- peptostreptococci – 103-105;
- bacteroids – 107-108;
- enterococci – 105-107;
- clostridia – up to 103;
- saprophytic staphylococci – up to 104;
- candida – up to 103;
- pathogenic staphylococci and enterobacteria are absent.
Enterococci in the analysis for dysbiosis in infants
This type of microorganism is needed for the proper breakdown of carbohydrates, the production of vitamins and immune support. It is good if they were revealed by an analysis for dysbacteriosis - the decoding in children with an acceptable value of enterococci indicates the correct digestion of food and the normal colonization of the intestines with the necessary microbes. When the bacteria described are greater than the established indicator, it’s also not scary. Analysis for dysbiosis in infants is a relative diagnostic parameter. Exceeding generally accepted norms is not considered a sign of illness.
Clostridia in the analysis for dysbiosis in infants
The presented microbes are involved in protein processing. They secrete special chemicals that stimulate intestinal motility and ensure regular evacuation of feces. An analysis for dysbacteriosis in children must necessarily contain clostridia in the results. There is no need to worry if their number is higher or lower than normal. The concentration of these microorganisms varies depending on the amount of protein consumed by the baby.
Proliferation in the analysis for dysbiosis in a child
This term often scares new parents, but there is nothing dangerous about it. Proliferation is often indicated when an analysis is performed for intestinal dysbiosis - decoding in children means that the number of some microbes exceeds the normal value. Colonies of these microorganisms tend to actively grow and reproduce in favorable conditions.
Decoding
Deciphering the analysis for dysbacteriosis in some cases reveals an excess of the normal level of opportunistic bacteria. The reasons for their growth are similar to those that lead to a decrease in beneficial microorganisms.
However, in certain quantities, some bacteria from this group can play a positive role in the functioning of the body:
- Peptostreptococci are involved in the production of hydrogen necessary to maintain acid balance. Their insignificant role in carbohydrate and protein metabolic processes is noted.
- E. coli is involved in the synthesis of bilirubin, cholesterol, vitamins K, B, and various types of acids. Uses oxygen, which has a negative effect on positive microorganisms.
- Bacteroides are indispensable in the process of fat processing.
- Clostridia are involved in protein processing. A small concentration of metabolites resulting from this process stimulates intestinal function.
- Candida in small quantities maintains acidity levels.
The source of harmful bacteria entering the body is dirty water, undercooked meat and fish products, and spoiled milk. Distributors: cockroaches, flies. You can suspect the penetration of harmful microorganisms by upset stool, vomiting, weakness, or stomach pain.
The results of an analysis for intestinal dysbiosis in a child serve as the basis for prescribing treatment. Therapy is aimed at eliminating pathogenic bacteria from the body and increasing beneficial ones.
Rate this article:
Is it necessary to treat dysbiosis in infants?
The condition in question is not a disease, and therefore does not require therapy. Progressive pediatricians do not even prescribe a stool test for dysbiosis in a child, considering it uninformative. While the baby is growing, the intestinal microflora is constantly changing, adapting to new food. It will finally be established in adulthood. Analysis of feces for dysbiosis in an infant makes sense only if there is a suspicion of an acute intestinal infection, but in such cases specific symptoms are present.
Dysbacteriosis is a special pathological condition during which the number of pathogenic or conditionally pathogenic microorganisms increases. Read more about this
Features of collecting feces for analysis
In order to properly collect stool for analysis, it is recommended to abandon the disposable diaper for a while and use a cloth one. In such a diaper, liquid feces are absorbed more slowly, and it becomes possible to collect biomaterial. Useful articles on the topic - how to properly test feces for dysbacteriosis.
If the room is warm, you can leave the child on the oilcloth, this makes it much easier to collect liquid stool in a special container. However, this method can only be used if the room is warm and the parent is sure that the child is going to defecate. To ensure that the liquid fecal mixture is successfully collected, you can purchase a urine collector to attach to the baby’s bottom. This is done only when the baby is sleeping, otherwise he will start knocking his legs and remove the urine bag.
If dysbacteriosis is suspected, the child will experience frequent, profuse regurgitation, colic in the intestines, diarrhea with green and red streaks, as well as skin rashes. In such a situation, it is urgent to conduct an analysis for the pathology of the gastrointestinal tract, which will determine the ratio of bacteria in the microflora. This analysis can detect staphylococcus and thrush. The main feature of such an analysis is that the stool must be fresh.
In addition to the above recommendations, you can use a gas outlet tube. If you don't have one, you can use a pipette by removing the rubber tip. Before use, the pipette should be thoroughly disinfected. With the help of such devices, you can help your child poop at the right time. For this purpose, the baby is placed on its side, the legs are bent to the tummy, the tube is carefully and smoothly inserted 1 centimeter, and slightly scrolled clockwise.
For what purposes is the study prescribed?
Testing for dysbiosis in a child is one of the ways to promptly identify the occurrence of problems associated with the digestive tract in children. Using this analysis, the development of an imbalance in the intestinal microflora can be determined.
Very often, the phenomenon of dysbacteriosis occurs in infants. It can appear in older children as a sign of the presence in the body of various diseases associated with the digestive system.
The main feature of dysbiosis is its specific symptoms. It is expressed in skillful camouflage, as a result of which it can be mistaken for any other disease associated with the gastrointestinal tract. It is for this reason that in order to diagnose dysbiosis in children, a serious examination should be carried out and all the necessary tests should be taken.
In some cases, this disease in children can be temporary, which means that the body has enough reserves to heal on its own, restoring the desired balance of microflora in the intestines. If recovery does not occur, the baby may be prescribed tests as part of a general examination.
It is worth saying that the intestines of a newborn baby are sterile. And then, up to a year, he gradually gains microflora for the full functioning of the intestines.
Tests for dysbacteriosis are prescribed for children under one year of age if the following symptoms are observed:
- with diarrhea and constipation observed in young children. And also in the case of alternation of these signs;
- identifying diseases associated with the digestive system, which include gastritis, cholecystitis, pancreatitis, etc.;
- allergic rashes often appear;
- Gastrointestinal infections occur very often;
- intolerance to a number of foods has arisen;
- was treated with antibiotics;
- Abdominal pain with flatulence are common.
Basic requirements for preparing a study
In order for the interpretation of the analysis for dysbacteriosis in children to be adequate and accurately correspond to reality, certain requirements for preparing and conducting the analysis must be met. You can submit quality material in the following cases:
- Preparation of a child up to one year takes place within three days, before the analysis itself. To do this, it is worth preserving foods that are familiar to the baby;
- if the baby has undergone drug treatment, then, on the doctor’s recommendation, you need to stop taking the medication a few days before;
- It is prohibited to use cleansing enemas, as well as laxatives and rectal suppositories.
It is very important to correctly collect feces to carry out analysis for a baby under one year old.
Indications for the purpose of analysis
Indications
The main indicators of the norm in the analysis of dysbiosis in a baby of the first year of life are the quantitative correspondence of bacteriological representatives. As the obtained indicators are deciphered, the specialist will be able to compare the results and assess the patient’s current condition.
We suggest you read: If your child’s temperature does not go down: what to do, quick help, review of medications, advice from pediatricians
The number of beneficial bacteria - bifidobacteria, lactobacilli and Escherichia should not be underestimated. Accordingly, their presence can fluctuate within 1010 (the lowest figure) - 1011 for the first, 106 - 107 for the second, 107 -108 for the third. Low indicators indicate a low concentration of beneficial intestinal inhabitants, which ultimately affects its functionality.
Opportunistic pathogens are present in every human body. It is considered normal if the population of these representatives does not exceed the description specified in the table. On average it is {amp}lt;=104. An increased number of opportunistic bacteria most often becomes the cause of dysbiosis.
In a normal state of microflora, pathogenic microorganisms should be completely absent. Even a small amount of such bacteria leads to intoxication of the body, causing severe symptoms. For infants, pathogenic infection is dangerous and can lead to irreversible consequences. The analysis helps to recognize such a disease in time.
The main task that can be set for researchers
Children under one year old need to be tested for dysbiosis to obtain complete information about the condition of their intestines. Doctors prescribe such a study to obtain the exact symptoms of the disease and determine the main concentration of both beneficial and pathogenic bacteria.
This study, followed by deciphering the bacteriological state in the intestines, is usually performed within 7 days. To do this, the provided stool sample will be examined using a special culture. This will allow us to further develop a strategy for effective treatment of dysbiosis. After some time has passed, the total number of bacteria can be counted. Usually the decoding indicates how many microorganisms will be contained in 1 gram of feces or COG/g.
Most often, such a study for children under one year is carried out using a biochemical method. Its main difference from bacteriological is that it produces results faster, which means it will allow you to start treatment earlier.
When decrypting, the following parameters are taken into account
| Essential gut bacteria | Current norms for a healthy infant |
During decoding, specialists take into account the presence of deviations from the natural norm. A stool sample should be taken correctly. Only in this case is it possible to examine all the bacteria present in the intestines.
All this will make it possible to correctly prescribe effective treatment for children under 1 year of age, allowing them to get rid of a disease such as dysbiosis.
Dysbacteriosis is a digestive disorder due to disturbances in the intestinal microflora. Accompanied by problems with bowel movements, abdominal pain, rash, and decreased immunity. Tests for dysbiosis in children are carried out to detect pathogens and diagnose a deficiency of beneficial bacteria. Informative data allows you to begin effective treatment.
How to submit material correctly
Before submitting material for tests for dysbacteriosis in adults or children, you must familiarize yourself with the established rules
, otherwise the decryption will show erroneous data.
Let's consider the main ones:
- 4 weeks before submitting the material, stop taking probiotics and eubiotics.
- Antibiotics are prescribed after the study or a day after administration.
- 4 days before collecting the material, you should avoid all drugs that can affect the microflora of the gastrointestinal tract, except for the necessary ones, as well as rectal suppositories.
If in doubt, it is better to visit a specialist and consult which medications can be temporarily excluded.
- Before collecting material, it is prohibited to use any creams, give an enema or use other stimulants.
Defecation should be natural
- When collecting stool, urine should not get into the material container.
- To avoid research errors, it is recommended to use only sterile containers. The lid of the jar must be tightly closed to prevent other microorganisms from getting inside.
- Only fresh material is suitable for analysis; it must be submitted to the laboratory no later than 3 hours later.
- Storing the material for 5 hours or more, as well as freezing it, is prohibited.
It is important to know!
When collecting material onto a diaper or towel, the fabric must be ironed with a hot iron; this is necessary to sterilize the surface.
Features of the analysis
Tests for dysbiosis are components of the diagnosis of intestinal disorders in children. A timely study allows us to identify the causes of disturbances in the functioning of the body. During the laboratory procedure, the number of beneficial bacteria, the concentration of opportunistic bacteria, and the presence of dangerous pathogens are determined.
To obtain complete results, 3 types of tests for dysbacteriosis are used.
- Coprogram is a stool test that allows you to determine the body’s ability to digest food. Detects the presence of parasites, blood and mucus. The study is prescribed for suspected intestinal disorders.
- Biochemical fecal analysis determines the level of bio indicators of acetic, butyric and propionic acid metabolites produced by various gastrointestinal bacteria.
- Stool culture for dysbacteriosis (tank culture) is a laboratory test in which the state of the intestinal microflora is determined as a percentage. The biomaterial is sown on a favorable environment in which colonies of bacteria grow. Afterwards, the number of bacteriological inhabitants is calculated per 1 gram of feces. The data is entered into a table from which the doctor assesses the state of the microflora.
Who needs analysis?
If there are frequent complaints about stool upset or digestive problems in children, a stool test for dysbacteriosis is prescribed.
However, it is worth mentioning that the disease “dysbacteriosis” does not exist in medical practice. This concept hides a microflora disorder that causes pathological symptoms of a digestive disorder.
Analysis for dysbacteriosis is indicated for:
- Long-term stool disorder - diarrhea, constipation, their alternation;
- Slow weight gain in infants;
- Suspicion of intestinal infection;
- Pathologies associated with the gastrointestinal tract;
- Allergies;
- Intolerance to certain foods;
- Frequently observed episodes of bloating, pain, flatulence;
- The appearance of a skin rash.
It is advisable to get tested for dysbacteriosis if the child is taking antibiotics. Oral administration of antibacterial drugs causes the death of all microorganisms that are sensitive to them and inhabit the intestines. As a result, not only pathogenic bacteria die, but also beneficial bacteria necessary for the normal digestion process.
How to properly test stool for dysbacteriosis in a child
Subsequent test results depend on how correctly the child’s stool is tested for dysbacteriosis.
Preparation for the event must be carried out in compliance with the standards. On the eve of the upcoming procedure, avoid taking antibiotics, laxatives, sorbents and probiotics. Simplify your child's menu - remove meat dishes, add vegetables and fruits. There is no need to introduce a new product into your baby’s diet before testing. This may distort the results of the diagnostic examination.
It is advisable to collect stool in the morning - after waking up. You should wait until the child empties his bladder. Afterwards, the baby needs to be washed to prevent urine from getting into the stool intended for analysis. There is no need to stimulate bowel movements with laxatives or enemas. The child must defecate on his own. You can help by giving a abdominal massage.
If the baby does not go to the toilet on his own, but relieves himself in a diaper, lay out a clean (preferably sterile) diaper or gauze. It is not advisable to take feces from a diaper. If the baby is potty trained, treat with boiling water before use.
The resulting feces are placed in an airtight container - a glass jar or container for analysis. In the first case, sterilization with hot water is necessary. The material should be submitted for research within 3 hours from the moment of bowel movement. If the parents do not have one, the bowel movements can be placed in the refrigerator provided the temperature is no more than 4°C. In this way, you can maintain the suitability of the material for another 4-5 hours. The more time passes from the moment of defecation to the start of the procedures, the greater the likelihood of distorting the results.
How to collect stool for analysis for dysbacteriosis?
To collect material for testing for dysbacteriosis, it is recommended to use a special disposable sterile container for coprogram, which can be purchased at any pharmacy. This container is easy to use and comes with a stick for collecting feces.
Collecting feces from a diaper or oilcloth is a bad idea, since with this method foreign substances (for example, the antiseptic contained in the diaper) can get into the fecal sample, which will distort the analysis result.
To collect biomaterial from loose stools, it is better to use a special children's urine collector, which is also sold at any pharmacy.
The biomaterial sample must be brought for testing while still fresh, preferably within two hours after collection. Due to the irregularity of feces in newborns, it is possible to store a sample of biomaterial for a short period of time at a low temperature (in the refrigerator). To provoke the release of bowel movements at the right time, you can use physiological stimulation: the parent lightly presses on the lower part of the abdomen and smoothly strokes the abdomen clockwise.
Interpretation of analyzes
The results of laboratory tests are entered into a table where the values of normal indicators are preliminarily indicated.
| Existing pathogenic flora | |
| Various types of E. coli | Within 300 – 400 million/year |
| Hemolyzing Escherichia coli | |
| Escherichia coli present in the body, characterized by normal enzymatic activity | Within 10⁷ - 10⁸ |
| Various lactose-negative enterobacteria | No more than 5% |
| Escherichia coli present in the body with reduced enzymatic activity | No more than 10% |
| Presence of cocci, taking into account the total number of intestinal bacteria | No more than 25% |
| Presence of bifidobacteria | No more than 10⁹ |
| Enterococci | Within 10⁵ - 10⁷ |
| Lactobacilli | Within 10⁶ – 10⁷ |
| Clostridia | No more than 10³ |
| Candida mushrooms | No more than 10³ |
| Conditionally – pathogenic flora (Klebsiella, Enterobacter, Graffinia, Serration, Proteus, Morganella, Citrobacter) | No more than 10⁴ |
| Non-fermenting bacteria (pseudomonas, acinetobacter) | No more than 10³ |
| Representative of microflora | Norm value |
| Bifidobacteria | >10 (9) |
| Lactobacilli | 10 (6) – 10 (7) |
| Escherichia | 10 (5) – 10 (7) |
| Typical Escherichia coli | 10 (7) — 10 (8) |
| Lactose-negative Escherichia coli | (7) — 10 (8) |
| Peptostreptococci | 10 (3) — 10 (5) |
| Staphylococcus saprophytes | (4) |
| Clostridia | (3) |
| Candida fungi | (3) |
| Proteas | (2) |
| Pathogenic enterobacteria | — |
| Staphylococcus aureus | — |
| Total number of cocci | (4) |
| Pseudomonas and Acinetobacter | (3) |
The number of beneficial bacteria, the concentration of opportunistic bacteria and the presence of pathogenic ones are taken into account.
Bifidobacteria are the main inhabitants of the intestines. They are responsible for the processes of food digestion, the full functioning of organs and systems, and the body’s immune defense. The number makes up 95% of the intestinal microflora. It is important that the number of representatives in the analysis shows at least 10 to the 9th power. Lactobacilli are no less important for the body. They create an acidic environment in the gastrointestinal tract. Escherichia is responsible for the production of vitamins and the absorption of microelements.
Pathogenic microorganisms, hemolytic bacillus or Staphylococcus aureus, must be absent from the child’s smear.
What does proliferation and Staphylococcus aureus mean in a child’s analysis?
The pediatrician deciphers the analysis after receiving the results from the laboratory.
While the analysis of stool for dysbacteriosis in children is being deciphered, the parents of the baby may encounter a variety of terms that are incomprehensible to a person without a medical education. One of these is the concept of proliferation. Can be seen next to the indicators of opportunistic bacteria. The meaning of proliferation is reproduction, growth. It indicates an excessive number of microorganisms of a particular type and indicates the need for a therapeutic course in order to reduce the number of representatives of the intestinal microflora.
The presence of Staphylococcus aureus (Staphylococcus aureus) in a smear is an alarming sign. The pathogen is a pathogenic bacteria and causes intoxication, inflammatory processes, and sepsis in the child. Staphylococcus is dangerous for infants, whose bodies are more sensitive to the effects of the toxins produced. Its appearance is influenced by neglect of personal hygiene rules - unwashed hands, dirty food, swimming in stagnant waters. The bacterium can be transmitted through medical instruments, from breast milk from mother to newborn baby, or directly from the carrier, through wounds on the body. If a pathogen is present, treatment with antibiotics is necessary.
Dysbiosis tests are a procedure that allows you to determine disturbances in the intestinal microflora. The study helps to identify infectious pathogens and begin timely, relevant treatment. To check the condition of the child’s body, it is recommended to carry out diagnostics in order to prevent various ailments.
Proliferation in the analysis for dysbacteriosis, what is it?
For many people, the word "bacteria" connotes imminent evil.
However, among these microscopic living forms there are different species. Some always bring only disease, so they are very dangerous. Others, on the contrary, do good, performing functions important for the life of people and animals. Representatives of the third group, which includes lactose-negative E. coli bacteria, can be both beneficial and dangerous, and therefore are called conditionally pathogenic.
Some patients, seeing the presence of incomprehensible “E. coli" are very upset and rush to start treatment immediately.
This is not advisable to do in all cases, since these bacteria must be present in the intestinal microflora, but their number should always be normal. Both its excess and its decrease cause a disease - dysbacteriosis.
What is E. coli
To make it clear what will be discussed in the article, we will explain the name of the microorganisms - E. coli lactose-negative. They are also called E. coli because they live in the intestines of humans and some species of mammals. In Latin it sounds like Escherichia coli.
The name “Escherichia” is given to microorganisms in honor of the Austrian scientist Theodor Escherich, who was the first to discover them. The term “lactose” means that they reproduce well on lactose, that is, in milk media, and “negative” emphasizes their activity that is harmful to the human body. In group E.
coli, in addition to lactose-negative ones, secrete enterohemorrhagic, enteroinvasive, enterotoxigenic and enteropathogenic Escherichia coli. Any amount of them in the intestines is dangerous for health.
A microscope allows you to see what they look like. E. coli lactose-negative and other Escherichia actually look like short rods with rounded ends. They are up to 0.8 microns wide and up to 3 microns long. Sometimes these bacteria end up connected to each other, forming chains.
On the outside, their shell is covered with pili - villi, which help the microbe to attach to the intestinal walls and be insensitive to many antibiotics. At the end, Escherichia has a flagellum, with the help of which they move quite quickly.
Therefore, once they enter, for example, the genitals, they are able to move to the kidneys, prostate, and bladder.
Lactose-negative E. coli are facultative anaerobes, that is, they do not need oxygen for their life, but they tolerate its presence without difficulty.
These bacteria, like all Escherichia, have many strains that differ from each other in some external characteristics, reaction to antibiotics, secreted toxins and other characteristics.
The benefits of E. coli
Some sources indicate that lactose-negative E. coli enter the fetal gastrointestinal tract in the mother’s womb, but most bacteriologists are inclined to believe that they colonize the baby’s intestines in the first two days after birth. In the stomach E.
coli do not linger because the environment there is not suitable for them. Having penetrated the intestines, they attach to its walls, where they live as long as their carrier is alive.
While there are 10*5 CFU/g of them (this is only 1% of all microorganisms in the intestines), they are doing useful things:
- produce B vitamins, lactate, succinic, formic, acetic and lactic acids, biotin, vitamin K;
- process oxygen, thereby promoting the vital activity of bifidobacteria, without which there can be no normal digestion of food;
- prevent many pathogenic bacteria from settling in the colon.
In other words, these bacteria are necessary in certain quantities. Some strains are even used as a probiotic and are purposefully introduced into the intestines for certain diseases. Therefore, if the analysis showed their presence is normal, then there is no pathology.
E. coli lactose-negative: proliferation. What it is?
In medicine, the term “proliferation” means the growth of tissue. In relation to bacteria, this is their excessive growth. Normally, E. coli colonizes the large intestine. When they proliferate, they migrate in large quantities into the thin tissue, causing dysbacteriosis in it.
E. coli begin to ferment (ferment) carbohydrates, which leads to the formation of methane, hydrogen and CO2. Because of this, the patient experiences bloating. Fermentation also produces fatty acids, which stimulate the formation of water in the intestines. As a result, the person begins to experience diarrhea.
Proliferation of microbes into the small intestine causes deconjugation and loss of fatty acids, which provokes cholelithiasis.
If overly multiplied bacteria manage to penetrate into the blood through ulcerations in the intestinal walls, they spread to many organs, causing various diseases, such as meningitis, gastroenteritis, peritonitis, and sepsis.
Dysbacteriosis in infants: causes and symptoms
In normal condition, babies must have beneficial bacteria in their intestines. If lactose-negative E. coli is elevated, the infant may develop dysbiosis. This occurs due to low immunity in newborn babies and the inability of their body to control the number of bacteria. Signs of the disease:
- bloating;
- flatulence;
- frequent regurgitation, sometimes vomiting;
- rumbling in the stomach;
- diarrhea (watery, foamy stool with a characteristic odor);
- allergic dermatitis;
- weight loss.
Undigested grains of food and mucus may be observed in the stool.
If your baby defecates too often, he or she may become dehydrated. Its symptoms:
- rare urination;
- weakness;
- dry lips, tongue.
In addition to the disturbance in the number of opportunistic E. coli, in the first days and weeks after birth, dysbiosis can begin due to the entry of enteropathogenic E. coli into the infant’s gastrointestinal tract.
You can become infected with them through mother's milk, through a dirty pacifier, toys, medical instruments, poorly washed hands of the mother or medical staff, or an insufficiently treated bottle. In infants on artificial feeding, infection with pathogenic Escherichia occurs if milk formulas are prepared in violation of technology.
In addition to the general symptoms of dysbacteriosis (diarrhea, vomiting, bloating), fever and bloody streaks in the stool are added.
Diagnosis and treatment of dysbiosis in infants
If an intestinal disorder is suspected in children, stool tests are taken for dysbacteriosis and coprogram. It is better to collect material for analysis from a diaper, rather than from a diaper.
If tests show that lactose-negative E. coli is elevated in an infant, but his condition is normal, treatment is not carried out. In some cases, the doctor prescribes probiotics, such as Bifidumbacterin, and prebiotics, such as Hilak-Forte, Duphalac.
If the condition of a child under one year of age is serious, he must be hospitalized. The hospital provides complex therapy aimed at preventing dehydration (young children are given IVs with rehydration solutions) and reducing E. coli levels.
If there is excessive proliferation of E. coli and the child develops meningitis or other severe complications, treatment is carried out with antibiotics.
In cases where pathogenic E. coli are detected in the feces of a baby, treatment is mandatory. It is carried out with antibiotics, rehydration solutions, probiotics and prebiotics.
Dysbacteriosis in children over one year old
It is believed that in children over 1 year of age, intestinal dysfunction occurs for the same reasons as in adults. E. coli lactose-negative levels are elevated in a child in the following cases:
- very weak immunity;
- long-term use of antibiotics, especially if treatment with these drugs is carried out on the initiative of the parents, and not as prescribed by the doctor.
Source: https://tsitologiya.su/zheludok/proliferacija-v-analize-na-disbakterioz-chto-jeto