According to its anatomical structure, the connective tissue of the pancreas consists of a body, tail and head. As a human organ, it is indispensable in metabolic processes and performs two functions: endocrine and exocrine. The endocrine function consists of producing hormones that promote metabolic processes, and the exocrine function of the pancreas is to ferment food in the stomach. Laboratory studies show that the pancreas produces more than 70% insulin and 22% glucagon. Therefore, chronic diseases of the pancreas can lead to weakening of its function, changes in connective tissue and the ability to produce insulin. Under what conditions does this happen? How to prevent pancreatic hormone deficiency?
What is insulin
The enzyme insulin is produced in beta cells. This protein hormone consists of polypeptide chains and disulfide bridges. Insulin is produced under the influence of proinsun, which is localized in the beta cells of the connective tissue of the pancreas. According to its functional characteristics, insulin reduces blood sugar. The mechanism of this effect is to reduce the production of glucose in the liver, and this in turn triggers the mechanism for the absorption of sugar by cell membranes. Thus, the process of breakdown of glucagon, which is part of the polymer chain of molecular glucose, slows down.
Insulin plays a huge role in providing vital mechanisms of life:
- helps build muscle tissue;
- activates ribosomal compounds that synthesize protein;
- protects muscle tissue and regenerates their cellular composition;
- transports amino acid compounds into cellular tissue and nourishes it.
When the insulin production mechanism is disrupted, the blood glucose level increases, and in this case diabetes mellitus is diagnosed. Insulin hormone can provoke acromegaly and obesity.
1.5.2.9. Endocrine system
| Table of contents of the topic “Parathyroid hormone. Pineal gland hormones. Pancreatic hormones. Gonadal hormones. Thymus hormones.”: 1. Parathyroid glands. Parathyrin. Parathyroid hormone. Calcitriol. Regulatory functions of parathyroid hormone. 2. Epiphysis. Melatonin. Pineal gland hormones. Regulatory functions of pineal gland hormones. 3. Pancreatic hormones. Islets of Langerhans. Somatostatin. Amylin. Regulatory functions of pancreatic hormones. 4. Insulin. Physiological effects of insulin. Scheme of glucose transport through cell membranes. The main effects of insulin. 5. Glucagon. Physiological effects of glucagon. Main effects of glucagon. 6. Sex glands. Gonadal hormones. Regulatory functions of gonadal hormones. 7. Androgens. Inhibin. Estrogens. Testosterone. Lutropin. Follitropin. Hormones of the testes and their effects in the body. 8. Female sex hormones. Ovarian hormones and their effects in the body. Estrogens. Estradiol. Estrone. Estriol. Progesterone. 9. Hormones of the placenta. Estriol. Progesterone. Chorionic gonadotropin. 10. Thymus hormones. Thymosin. Thymopoietin. Timulin. Regulatory functions of thymus hormones. Endocrine function in The number of islets in the gland of an adult is very large and ranges from 200 thousand to one and a half million. There are several types of hormone-producing cells in the islets: alpha cells produce glucagon , beta cells - amylin is synthesized in beta cells , which has effects opposite to insulin. The blood supply to the islets is more intense than to the main parenchyma of the gland. Innervation is carried out by postganglionic sympathetic and parasympathetic nerves, and among the cells of the islets there are nerve cells that form neuroinsular complexes. Rice. 6.21. Functional organization of the islets of Langerhans as a “mini-organ”. Solid arrows - stimulation, dotted arrows - suppression of hormonal secretions. The leading regulator, glucose, with the participation of calcium, stimulates the secretion of insulin by β-cells and, on the contrary, inhibits the secretion of glucagon by alpha cells. Amino acids absorbed in the stomach and intestines stimulate the function of all cellular elements of the “mini-organ”. The leading “intraorgan” inhibitor of insulin and glucagon secretion is somatostatin; activation of its secretion occurs under the influence of amino acids and gastrointestinal hormones absorbed in the intestine with the participation of Ca2+ ions. Glucagon is a stimulator of both somatostatin and insulin secretion. Insulin is synthesized in the endoplasmic reticulum of beta cells first in the form of pre-proinsulin, then the 23-amino acid chain is split off from it and the remaining molecule is called proinsulin.
The amount of insulin deposited in granules is almost 10 times higher than the daily requirement for the hormone. Insulin secretion occurs by exocytosis of granules, with an equimolar amount of insulin and C-peptide entering the blood. Determining the content of the latter in the blood is an important diagnostic test for assessing secretory capacity (3-cells. Insulin secretion is a calcium-dependent process. Under the influence of a stimulus—an increased level of glucose in the blood—the beta cell membrane is depolarized, calcium ions enter the cells, which triggers the process of contraction of the intracellular microtubular system and the movement of granules to the plasma membrane, followed by their exocytosis. Secretory function of different islet cells is interconnected and depends on the effects of the hormones they produce, and therefore the islets are considered as a kind of “mini-organ” (Fig. 6.21). Stimulated insulin secretion is a response of Under the influence of glucose, the energy receptor of beta cells is activated, which increases the transport of calcium ions into the cell, activates adenylate cyclase and the cAMP pool (fund). Through these intermediaries, glucose stimulates the release of insulin into the blood from specific secretory granules.
The vagus nerve and acetylcholine stimulate insulin secretion, and the sympathetic nerves and norepinephrine, through alpha-adrenergic receptors, suppress insulin secretion and stimulate glucagon release. A specific inhibitor of insulin production is the islet delta cell hormone, somatostatin. . This hormone is also formed in the intestines, where it inhibits the absorption of glucose and thereby reduces the response of beta cells to a glucose stimulus. The formation of peptides similar to mosg, such as somatostatin, in the pancreas and intestines confirms the existence of a single APUD system in the body. Glucagon secretion is stimulated by a decrease in blood glucose levels, gastrointestinal hormones (GIP gastrin, secretin, cholecystokinin-pancreozymin) and a decrease in Ca2+ ions in the blood.
The cells of the gastrointestinal tract that produce hormones are a kind of “early warning devices” for the cells of the pancreatic islets about the entry of nutrients into the body, which require the participation of pancreatic hormones for utilization and distribution. This functional relationship is reflected in the term “ gastro-entero-pancreatic system” ». – We also recommend “Insulin. Physiological effects of insulin. Scheme of glucose transport through cell membranes. The main effects of insulin.” | ||
| Scroll back | Table of contents | Scroll forward |
Hormones are substances produced by the endocrine glands and released into the blood, their mechanism of action. The endocrine system is a collection of endocrine glands that produce hormones. Sex hormones.
For normal life, a person needs many substances that come from the external environment (food, air, water) or are synthesized inside the body. With a lack of these substances in the body, various disorders occur that can lead to serious diseases. These substances, synthesized by endocrine glands inside the body, include hormones
.
| Most hormones are produced by the endocrine glands . |
First of all, it should be noted that humans and animals have two types of glands.
the secretion they produce
outward and are called exocrine (from the Greek
exo
- outside, outside,
krino
- to secrete).
The glands of the second type release the substances synthesized in them into the blood that washes them. These glands were called endocrine (from the Greek endon
- inside), and substances released into the blood are hormones.
Thus, hormones (from the Greek hormaino
– set in motion, induce) – biologically active substances produced by endocrine glands (see Figure 1.5.15) or special cells in tissues.
Such cells can be found in the heart, stomach, intestines, salivary glands, kidneys, liver and other organs.
Hormones are released into the bloodstream and have an effect on cells of target organs located at a distance or directly at the site of their formation (local hormones).
Hormones are produced in small quantities, but remain active for a long time and are distributed throughout the body through the bloodstream. The main functions of hormones are:
– maintaining the internal environment of the body;
– participation in metabolic processes;
– regulation of growth and development of the body.
A complete list of hormones and their functions are presented in Table 1.5.2.
Table 1.5.2. Basic hormones
HormoneWhich gland produces itFunction
| Adrenocorticotropic hormone | Pituitary | Controls the secretion of hormones from the adrenal cortex |
| Aldosterone | Adrenal glands | Participates in the regulation of water-salt metabolism: retains sodium and water, removes potassium |
| Vasopressin (antidiuretic hormone) | Pituitary | Regulates the amount of urine excreted and, together with aldosterone, controls blood pressure |
| Glucagon | Pancreas | Increases blood glucose levels |
| A growth hormone | Pituitary | Manages the processes of growth and development; stimulates protein synthesis |
| Insulin | Pancreas | Lowers blood glucose levels; affects the metabolism of carbohydrates, proteins and fats in the body |
| Corticosteroids | Adrenal glands | Have an effect on the entire body; have pronounced anti-inflammatory properties; maintain blood sugar levels, blood pressure and muscle tone; participate in the regulation of water-salt metabolism |
| Luteinizing hormone and follicle stimulating hormone | Pituitary | Control reproductive functions, including sperm production in men, egg maturation and the menstrual cycle in women; responsible for the formation of male and female secondary sexual characteristics (distribution of areas of hair growth, volume of muscle mass, structure and thickness of skin, timbre of voice and, possibly, even personality traits) |
| Oxytocin | Pituitary | Causes contraction of the muscles of the uterus and mammary ducts |
| Parathyroid hormone | Parathyroid glands | Controls bone formation and regulates the excretion of calcium and phosphorus in urine |
| Progesterone | Ovaries | Prepares the inner lining of the uterus for the implantation of a fertilized egg, and the mammary glands for milk production |
| Prolactin | Pituitary | Induces and maintains milk production in the mammary glands |
| Renin and angiotensin | Kidneys | Control blood pressure |
| Thyroid hormones | Thyroid | Regulate the processes of growth and maturation, the speed of metabolic processes in the body |
| Thyroid-stimulating hormone | Pituitary | Stimulates the production and secretion of thyroid hormones |
| Erythropoietin | Kidneys | Stimulates the formation of red blood cells |
| Estrogens | Ovaries | Control the development of female genital organs and secondary sexual characteristics |
The structure of the endocrine system.
Figure 1.5.15 shows the glands that produce hormones: hypothalamus, pituitary gland, thyroid gland, parathyroid glands, adrenal glands, pancreas, ovaries (in women) and testes (in men). All glands and cells that secrete hormones are combined into the endocrine system.
Endocrine system
works under the control of the central nervous system and, together with it, regulates and coordinates the functions of the body. Common to nerve and endocrine cells is the production of regulatory factors.
Through the release of hormones, the endocrine system, together with the nervous system, ensures the existence of the body as a whole. Let's consider this example.
If there were no endocrine system, then the entire body would be an endlessly tangled chain of “wires” - nerve fibers.
In this case, through many “wires” it would be necessary to sequentially give one single command, which can be transmitted in the form of one “command” transmitted “by radio” to many cells at once.
Endocrine cells produce hormones and release them into the blood, and cells of the nervous system ( neurons
) produce biologically active substances (
neurotransmitters
-
norepinephrine
,
acetylcholine
,
serotonin
and others) released into
synaptic clefts
.
The link between the endocrine and nervous systems is the hypothalamus, which is both a nerve formation and an endocrine gland.
| The hypothalamus is the highest center of the endocrine system. |
It controls and combines endocrine regulatory mechanisms with nervous ones, being also the brain center of the autonomic nervous system
.
The hypothalamus contains neurons capable of producing special substances - neurohormones.
regulating the release of hormones by other endocrine glands. The central organ of the endocrine system is also the pituitary gland.
The remaining endocrine glands are classified as peripheral organs of the endocrine system.
Source: https://www.rlsnet.ru/books_book_id_2_page_39.htm
Types of insulin
The gland produces two types of insulin: stimulated and basal.
The basal type of insulin ensures the presence of the hormone in the blood without stimulating factors. That is, the insulin hormone enters the blood without food fermentation. In this case, when analyzing blood sugar in healthy people, it is 5.5 mmol/l with an insulin enzyme level of 69 mmol/l.
When hormone production is stimulated, the enzyme is redirected into the blood with the help of amino acids and glucose, which enters the human body along with food. The mechanism of the presence of insulin in the blood consists of two stages: short and long. During the short phase, insulin enters the blood with the help of amino acids and sulfonylureas, and during the long phase, insulin is broken down.
Causes of insulin deficiency
The reasons for the lack of insulin production by the pancreas may be as follows:
- disruption of cellular composition due to exposure to toxic agents or potent drugs;
- disturbances in the secretion of gastric juices;
- damage to the gland ducts;
- pathological changes in the functioning of the pancreas;
- insufficiency in the functioning of the biliary tract;
- disturbances of intestinal microflora due to dysbacteriosis;
- ulcerative processes in the stomach and duodenum, as well as cholelithiasis.
With high levels of the hormone in the blood, disturbances in the functioning of the receptors that carry out the carbohydrate process are observed. In this case, type 2 diabetes mellitus develops. In this case, the gland, producing excess enzyme, acts on the receptors. But their work is disrupted and carbohydrates are not sufficiently absorbed by the body and the sugar level gives quite elevated results. This fact must be taken into account when prescribing insulin. In this case it is not used.
Low insulin in the blood - how to increase it
The hormone insulin is vital for the human body. Therefore, when its deficiency occurs, it causes a disruption in almost all processes that occur in the body. Especially low insulin in the blood affects glucose levels.
Insulin content norm
Insulin is produced by the pancreas. Thanks to it, the correct movement of amino acids and carbohydrate metabolism in the body occurs. Due to the decrease in level, not only these, but also other processes are disrupted. Therefore, you need to periodically check this indicator and try to ensure that the lower limit is the norm. It is measured in μED
- in children: 3-20,
- in adults: 3-25,
- for women expecting a child: 6-27,
- in elderly people over 60: 6-35.
Why is there not enough insulin?
The lack of the hormone is greatly influenced by poor nutrition, especially its excess. In addition, other reasons can be identified:
- stress, excessive tension of the central nervous system,
- hereditary predisposition,
- chronic diseases or infections,
- insufficient amount of protein and zinc,
- increased iron and carbohydrate content,
- absence or vice versa, excessive physical activity,
- dysfunction of the pancreas,
- after pancreatic surgery.
Types of hormone deficiency
Reduced insulin levels usually occur during diabetes. Insufficient hormone levels are divided into 2 types:
- Absolute (pancreatic). This lack of insulin is caused by type I diabetes. It causes the destruction of insulin production, causing irreversible changes in the cells of the pancreas. Insulin is released in much smaller quantities or not produced at all, so blood sugar levels rise. To maintain insulin at a normal level, the patient needs to give himself injections.
- relative (non-pancreatic). This type of deficiency is caused by type II diabetes. This type of disease is characterized by normal insulin secretion (or even its excess). But it does not interact with tissues and cells, as a result of which it cannot perform its job correctly. It is because of this type of deficiency that the metabolic processes of glucose are destroyed and hyperglycemia begins. In other words, the body is unable to use the hormone correctly because sensitivity to it is insufficient.
If insulin is reduced and the sugar level is normal, this means an increased content of glucagon, thyroxine, and adrenaline in the patient’s body.
Symptoms of insulin deficiency
First of all, the patient will be told about insufficient insulin levels by the following symptoms:
- wounds do not heal well,
- the patient is haunted by a feeling of weakness and constant fatigue,
- strong thirst that is almost impossible to quench,
- frequent urination, mainly at night,
- elevated glucose levels.
Insulin deficiency in children
By age 5, the pancreas is usually fully developed. Therefore, the most dangerous age from the point of view of improper insulin production is the age of 5-11 years.
Treatment for low insulin
Type I disease requires daily hormonal injections. Lack of production of the hormone in question causes increased glycemia. This occurs because there is not enough insulin to transport glucose into the cells, and excess sugar accumulates in the blood.
Sugar levels become higher at night. If there is not enough insulin, “extra” glucose enters the urine, which causes polyuria (increased urination).
The doctor, depending on the condition and individual characteristics of the body, prescribes treatment. If there is a complete absence of hormone production, the patient is recommended to undergo subcutaneous insulin injections. They can be done in a clinic, but because... The procedure is carried out several times a day; it is more convenient to learn how to administer the medicine yourself.
Most often, the doctor prescribes the following medications:
- “Civilin” helps restore pancreatic cells, as a result of which insulin levels increase.
- “Medzivin” improves immunity and restores hormonal levels.
- “Livicin” opens the walls of blood vessels.
In addition, your daily diet should include the following products:
- cabbage,
- parsley,
- apples,
- blueberry,
- kefir,
- lean red meat.
They help stimulate the pancreas, causing insulin levels to rise and sugar levels to drop.
Only a doctor can take any of these drugs or prescribe other treatment after studying all the features of the patient’s disease.
Symptoms of insulin deficiency
In the pancreas, insufficiency of insulin production is presented in the form of the following symptoms:
- frequent dysbacteriosis;
- bloating;
- pain;
- nausea and gag reflexes;
- decreased appetite;
- general weakness;
- sudden weight loss;
- developmental delay;
- constant thirst, as excess glucose levels absorb all the moisture and dehydrate the cells.
The first thing you should pay attention to is changes in stool. This occurs when there is a lack or excess of insulin. According to laboratory studies, when insulin production decreases, insulin deficiency can reach up to 250 thousand units per day. With such indicators, patients experience voluminous and plentiful stools with a grayish tint and the appearance of a putrid odor.
Other diseases of the pancreas
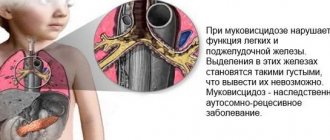
Cystic fibrosis can lead to the development of insulin-requiring diabetes.
In a person with cystic fibrosis, sticky mucus causes scar tissue to form on the pancreas, and scarring can prevent the organ from producing enough insulin. As a result, a person may develop cystic fibrosis-related diabetes (CFRD).
The signs and symptoms of CFRD may resemble those of cystic fibrosis. A person may not know they have CFRD until they take a diabetes test.
Increased amount of insulin
An increase in insulin levels in the gland is provoked by the following organic processes:
- Interferes with the production of lipase. This enzyme is responsible for the breakdown of fats. With a lack of lipase, adipose tissue accumulates in muscle tissue and thus. fat mass accumulates.
- Fatty acids are synthesized in the skin. An excess of insulin provokes the formation of triglycerides. They activate the sebaceous glands. As a result, the secretion of oil increases, acne, pimples, seborrhea of the scalp and dandruff form.
- With increased insulin, cholesterol plaques form in the lumens of blood vessels. Lipid compounds cannot cope with such a load and the walls of blood vessels are destroyed or deformed. Such a narrowing can lead to pathology of the heart muscle.
- Excess insulin leads to increased blood pressure. Why is this happening? It has not yet been established. But increased insulin somehow affects the functioning of the kidneys and nerve endings, which intensively constrict blood vessels. The result of this action is increased blood pressure.
- Elevated insulin can stimulate the development of cancer. Excessive levels of the hormone contribute to the increase in malignant tumors. This fact increases the risk of developing cancer.
The source of heart disease, strokes, asthmatic bronchitis, inflammatory processes in the respiratory tract, and the formation of trophic ulcers can be a chronic increase in the hormone insulin.
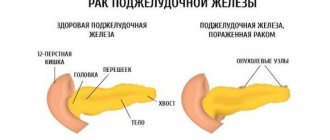
Diabetes and pancreatic cancer
According to the Pancreatic Cancer Network, people who live with diabetes for 5 years or more are 1.5 to 2 times more likely to develop pancreatic cancer.
The onset of type 2 diabetes later in life may be a symptom of this type of cancer.
The relationship between diabetes and pancreatic cancer is complex. Diabetes increases the risk of developing this type of cancer, and pancreatic cancer can sometimes lead to diabetes.
Other risk factors for pancreatic cancer:
- obesity
- aging
- poor nutrition
- smoking
- genetic inheritance
In the early stages, this type of cancer may not cause any symptoms. Doctors often diagnose it when it is more advanced.
Prevention of increased hormone production in the gland
Insulin provokes the formation of serious diseases that are difficult to treat. In order to avoid such a somatic problem, you should take preventive measures and thus lower your blood sugar levels. Among the preventive measures, doctors highlight the following:
- eat throughout the day at intervals of 10-12 hours. Thus, you will be able to eat 2 times;
- apply fasting once a week. In this case, the insulin hormone decreases, and the necessary energy resources are directed to ensure the body’s energy activity. At the same time, a person loses extra pounds and this will also prevent cancer;
- use less food in your diet that contains the insulin index. Among such products, dairy products stand out especially. In this case, plant fiber is considered an excellent insulin-absorbing product;
- increase physical activity or play sports. Exercising in the gym or on the sports ground also reduces the formation of the hormone in the gland.
For normal levels of the hormone insulin in the gland, provided that you have a predisposition to such a defect, it is important to constantly monitor the condition of the gland and the production of hormonal insulin. This analysis can be carried out independently at home on an empty stomach. A glucometer is used for this. This compact medical device can be purchased at a pharmacy or a specialty medical equipment store. But if you eat rationally and exercise, then this correction of the hormone level in the blood will be useful to you, and you will probably not get sick.