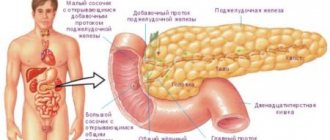
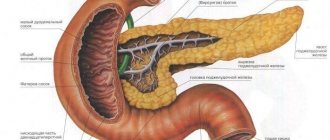
The pancreas is an essential part of normal digestion. It produces enzymes that promote the breakdown of organic substances: proteins, carbohydrates and fats. In addition, this organ secretes the hormone insulin. It contributes to the normal functioning of the human body as a whole and also maintains normal blood glucose levels. Under the influence of certain harmful factors, the functions of the organ are disrupted, which leads to certain disorders and the development of corresponding symptoms.
Causes
Problems with the pancreas can be caused by the following factors:
- eating disorders, consumption of fatty, fried and spicy foods;
- alcohol abuse;
- disorder of the hepatobiliary structure: reflux of bile into the excretory ducts of the pancreas, inflammation of the gallbladder, cholelithiasis, biliary dyskinesia;
- inflammatory diseases of the digestive organs: gastritis, colitis, duodenitis, peptic ulcer;
- poor nutrition, in which the body receives few vitamins and protein.
Pathological signs of pancreatic dysfunction can occur during the development of many diseases, so it is worth carefully examining the patient to determine the correct diagnosis. An inflammatory process is often diagnosed - pancreatitis, occurring in acute or chronic form, diabetes mellitus, a malignant process in an organ. Somewhat less often, it is possible to detect pancreatic necrosis - cell death, cystic fibrosis and cysts.
Symptoms and pathologies
These are the first symptoms that may appear when there are problems with the gland, and ignoring them can only lead to aggravation of the problem.
Most often, problems with the gland begin suddenly, without bothering the patient until a certain time. Typically, symptoms of a particular disease of this organ begin between the ages of 30 and 45 years.
During this period, many are actively involved in their careers, families, and homes, and with such a busy life, the first symptoms of the disease may go unnoticed.
Let's talk about what pancreatic pathologies are the most common today, what their symptoms and first signs are.
Pancreatitis
Pancreatitis is an inflammatory process localized in the mucous membrane of the organ. When the exits to the duodenum are blocked by protein plugs, the enzymes of the gland cannot penetrate the intestines and begin to irritate the tissues of the organ from the inside.
As a result, inflammation begins, and the gland cannot fully synthesize digestive enzymes.
In acute pancreatitis, a person feels very severe pain, attacks of which are accompanied by nausea and vomiting. In general, the condition of the body in such a situation is very poor and requires emergency medical care. Symptoms of development depend on the form, but the classic ones include:
- Painful sensations
- Nausea,
- Heartburn,
- Belching,
- Flatulence,
- Diarrhea.
The development of chronic pancreatitis occurs gradually and for some time practically does not manifest itself at all. The pain is usually not very severe, but hemorrhage and swelling may occur.
If the symptoms are not recognized in a timely manner and the inflammatory process is not stopped, then the death of gland cells and the development of pancreatic necrosis will begin, this complication is also called pancreatic necrosis. Signs of this condition include severe pain and increased body temperature. This pathology is life-threatening and must be accompanied by immediate treatment.
Diabetes
Diabetes mellitus can be the result of a variety of reasons. Type 1 diabetes is associated with insufficient insulin synthesis or the presence of pancreatitis during menopause.
Signs and symptoms of diabetes:
- thirst,
- frequent urge to urinate,
- weight loss,
- numbness of the limbs,
- general weakness.
Stones in the pancreas
The formation of stones - this problem also occurs quite often and its causes have not yet been fully established. But the patient can feel the symptoms and signs quite clearly.
There are several assumptions why stones occur in the pancreas; this happens when:
- changes in the digestive tract,
- presence of bad habits,
- metabolic disorders,
- hormonal imbalances.
The symptoms of stones may vary depending on the location of the deposits (pain in the lower back or upper abdomen, jaundice).
Symptoms
In almost any disease that spreads to the pancreas, the following clinical signs occur:
- Pain. It is localized in the epigastric region, can affect the navel, and is encircling in nature. In most cases, the symptom is associated with errors in diet or alcohol consumption. During painful attacks, the patient tries to take a position in which his condition will improve at least a little.
- Yellowing of the eyeballs and skin.
- Dyspeptic disorders. Patients complain of bloating, nausea, vomiting, diarrhea, and a feeling of heaviness.
- Severe hyperthermia.
- A rash on the skin in the form of spots in the area of projection of the organ.
If the problem is associated with a disorder of insulin production and diabetes mellitus develops, the following pathological manifestations develop:
- Intense thirst that does not go away after drinking liquid.
- Sudden and persistent loss of body weight.
- Visual and hearing disorders.
- Sensation of thorns in the limbs.
- Reduced blood clotting, which manifests itself in bleeding even with minor injuries.
- Constant weakness, fatigue for no apparent reason.
If you experience any of the above symptoms, you should consult a specialist to diagnose and treat the problem. Diseases of the pancreas cannot be neglected, since the organ controls many important processes for life. If they are violated, complications from other organs and even death can occur.
Pancreatic diseases
Problems with the pancreas can be the result of various factors. Organ diseases can be divided into consequences of developmental anomalies, injuries, inflammation, tumors. Many of them have similar symptoms and you can suspect organ dysfunction on your own. But only a doctor can make an accurate diagnosis based on hardware and laboratory diagnostics. Let's look at the most common problems that arise with the pancreas, their probable causes and clinical manifestations.
Inflammatory processes
The most common disease of the pancreas is pancreatitis - inflammation of the organ tissue. According to the nature of its course, it can be acute or chronic.
Forms of acute pancreatitis:
- interstitial;
- hemorrhagic;
- purulent;
- pancreatic necrosis.
Find out about normal blood sugar levels during pregnancy, as well as ways to correct abnormalities.
The reasons for low hCG in early pregnancy and the dangers of hormone deficiency are written on this page.
The most common causes of pancreatic inflammation are:
- alcoholism;
- unhealthy diet, especially excess fatty foods;
- cholelithiasis;
- cholecystitis;
- taking certain groups of medications (sulfonamides, cytostatics).
Often the diagnosis of acute pancreatitis is difficult due to the variety of clinical symptoms that may be inherent in a number of other gastrointestinal pathologies. In this case, differential diagnosis is very important.
Clinical signs of acute inflammation of the pancreas:
- sharp pain in the epigastrium, which can radiate throughout the abdominal region and into the spine;
- dyspeptic disorders: nausea, vomiting, diarrhea;
- dehydration of the body.
The severity of symptoms of inflammation of the pancreas depends on the form of acute pancreatitis and the degree of its neglect. Pain is not correlated with food intake, but may decrease after the use of analgesics and NSAIDs. Dyspeptic disorders often occur in the initial stage of development of pancreatitis against the background of poor diet or alcohol abuse. Vomiting is a sign of intoxication of the body. First, remnants of undigested food are detected in the vomit, then bile impurities appear.
Chronic pancreatitis often becomes a consequence of untreated acute pancreatitis. Its symptoms are more vague. The pain is often aching in nature. Exacerbations of the disease usually occur with malnutrition.
Cysts and stones
Cysts are benign hollow formations filled with fluid inside. They can be localized in any part of the gland. By origin, cysts can be congenital, parasitic, neoplastic, caused by inflammatory processes or a consequence of pancreatic injuries.
In most cases, as long as the formation is small and does not affect nearby organs, it may not cause any symptoms. As the cyst grows, pain occurs in the upper abdomen, digestion is disrupted, which leads to weight loss. These are not typical signs of a pancreatic cyst, so patients need to undergo a thorough diagnosis to find out whether there really is a tumor.
Pancreolithiasis (stones in the pancreas) is not common. The pathology can develop against the background of prolonged deposition of salts in the tissues of the organ or as a result of other pancreatic diseases. Usually stones are found in the head of the gland. Signs of pancrolithiasis may include epigastric pain radiating to the back; they may be paroxysmal and become stronger after eating. When a stone obstructs the bile ducts due to its movement, acute pain, signs of obstructive jaundice, attacks of vomiting and nausea occur.
Treatment
If the functioning of the organ is disrupted, treatment is carried out, including medications and adherence to the correct diet. If you suddenly experience symptoms of a gland disease, and it is not possible to urgently seek medical help, you should fast to relieve the burden on the digestive tract and allow the organ to rest. First of all, patients must follow nutritional recommendations. You need to eat often, but little by little. Food should be warm; you should avoid hot and cold dishes.
Treatment of pancreatic diseases
The method of treatment will depend on the stage of the disease. In case of exacerbation, the patient must be hospitalized.
The three main components of treatment are hunger, cold and rest.
In the first two to three days, it is forbidden to eat any food; you can only drink alkaline mineral still water or herbal decoctions.
It is necessary to maintain bed rest, and to reduce pain, apply an ice pack to the area of the gland. To eliminate spasms, no-spa (drotaverine) is prescribed.
During the recovery period, a gentle diet should be followed, painkillers and anti-inflammatory drugs, as well as pancreatic enzymes, should be prescribed.
Diet
You should not eat fried, spicy, fatty foods, alcohol, confectionery, sweets, chocolate, boiled eggs, sour cream, cream, fatty cottage cheese, cheeses, pearl barley and millet porridge, whole milk, cocoa, coffee and alcohol. Among vegetables, it is prohibited to include sauerkraut and fresh cabbage, radishes, radishes, legumes, mushrooms and sorrel in the diet.
It is allowed to eat lean meat (rabbit, chicken, turkey, veal) and fish (cod, hake, pike perch, carp, perch), low-fat fermented milk products, vegetables, fruits baked without skin, as well as compotes, day-old bread, crackers, dry biscuits, honey, porridge (semolina, buckwheat, rice, oatmeal), shortcrust pastry products, tea, jelly, weak coffee with milk. All food should be boiled, baked, stewed or steamed. Temperature of dishes: 30 – 40 degrees.
Diagnosis and treatment
The diagnosis of pancreatic disease is made based on a detailed medical history. To clarify the diagnosis, blood tests (general and biochemical), urine and stool tests may be prescribed. An increase in the number of leukocytes and erythrocyte sedimentation rate indicate the presence of an inflammatory phenomenon in the gland.
Important information: Symptoms and treatment of pancreatic inflammation
A biochemical study of blood composition for enzyme content is also very informative. Acute pancreatic inflammation is characterized by increased elastase activity. In a urine test, the most specific indicator of pancreatic pathology is an increase in amylase activity, the presence of ketone bodies and sugar. Analysis of stool for pancreatic pathologies reveals the presence of residues of fatty foods, muscle fibers, and carbohydrates.
A common instrumental method for examining the pancreas today is ultrasound. This method allows you to assess the size, shape, density of the organ, identify pathologies of the ducts, and determine the presence of tumors and stones. In addition, radiography, computed tomography and magnetic resonance imaging (CT and MRI) can be used to diagnose pathology.
Since the pathology of the pancreas negatively affects many vital processes in the body, when its slightest signs appear, immediate treatment is necessary. Mild inflammation is easily treatable, and relief occurs in a short period of time. Severe forms of inflammation require longer treatment. When diagnosing various neoplasms or blockage of the ducts with stones, surgical intervention is prescribed. In parallel, treatment of concomitant or provoking pathologies is mandatory.
In case of an acute attack of pancreatitis, it is first recommended to provide rest to the organ through fasting. For several days you can drink only boiled or slightly alkaline mineral water.
To relieve acute inflammation, antibiotics are prescribed: Tsiprolet, Ampiox, Ciprofloxacin, Doxycycline. Spasms are relieved with Atropine, No-Spa or Gastrocepin. For severe pain, painkillers Baralgin and Ibuprofen are prescribed. If nausea or vomiting is present, Cerucal or Metoclopramide is prescribed. Violation of secretory function is stabilized by the administration of enzyme-containing drugs Festal, Pancreatin, Creon, Vigeratin.
Treatment of pancreatitis with homeopathy is practiced. Although this process takes a longer time, it has a general strengthening effect on the body, and with a careful and responsible approach it allows you to completely get rid of even chronic pancreatitis.
If problems with the pancreas occur, a special diet is required - a strict diet with the exception of fatty, fried, spicy foods, especially alcoholic beverages. It is recommended to exclude from the diet plant foods rich in organic acids, for example, spinach, sorrel, radish, radish, pomegranate and sauerkraut. You should also refrain from consuming chocolate, coffee, cocoa, whole milk, legumes and mushrooms. Dishes allowed for pancreatitis must be boiled or steamed. It is advisable to eat food only warm, since cold and hot dishes can provoke an exacerbation of the condition.
Meals are fractional - 5-6 times a day and in small portions.
Solid food must be crushed. After the acute condition is relieved, it is allowed to eat lean meat, fish, chicken, baked and boiled vegetables, day-old bread and crackers. The diet should include various cereals, of which the most valuable are buckwheat and oatmeal. Carrots are very useful, which can be consumed both raw and as part of dishes.
Important information: What are moderate diffuse changes in the pancreatic parenchyma
Drug therapy
Medications prescribed include Omeprazole, Quamate, and Ranitidine. These drugs reduce the production of gastric juice. For pain syndrome, antispasmodics are indicated: Drotaverine, Papaverine, No-shpa. If there is pathology of the biliary tract, Urolesan is used. Enzymatic agents are also used - Creon, Mezim, Pancreatin, Panzinorm. You can drink heated mineral waters - Borjomi, Essentuki. During the period of remission, it is recommended to undergo sanatorium-resort treatment.
It is impossible to identify the pathological condition of the pancreas on your own, but it can cause a number of complications. Therefore, if any of the above symptoms occur, you should consult a specialist.