Hyperfunction and hypofunction of the pancreas, regardless of the cause, pose a health hazard. Malfunctions are associated with a disorder of the secretory activity of the organ. Diabetes mellitus is especially difficult - a condition with impaired synthesis or production of insulin, which develops with hypofunction of the pancreas, leads to severe damage to many organs and systems, changes the patient’s lifestyle and takes a long time to be treated.
During therapy, another disorder may occur when the amount of hormones produced increases sharply. With hyperfunction of the pancreas, a life-threatening condition often develops if the amount of synthesized hormonal substances becomes critically high. In such cases, emergency assistance is necessary.
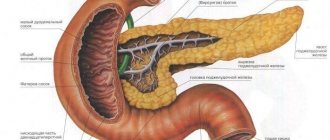
The structure of the pancreas and the main functions of the gland
The pancreas (P) is an organ that simultaneously belongs to the digestive and endocrine systems and performs excretory and incretory functions. This is due to the structure of tissues, which are strictly divided according to structure and functions.
The endocrine part of the pancreas consists of a cluster of cells that produce hormones. It makes up 1.5% of the organ’s volume, called the islets of Langerhans; in humans there are 1-1.5 million of them. They consist of several types of cells that produce strictly defined hormones:
- α (25%) – glucagon;
- β (60%) – insulin and amylin;
- δ (10%) – somatostatin;
- PP (5%) – vasoactive intestinal polypeptide (VIP), pancreatic polypeptide (PP);
- g-cells - gastrin, which affects gastric juice and its acidity.
Among all hormones, insulin plays the most important role both in normal and pathological conditions.
The rest of the pancreas (90%) performs an exocrine function. It is represented by glandular cells that produce pancreatic juice enzymes. They break down food entering the body:
- trypsin;
- lipase;
- amylase.
In addition to these main representatives, each group includes several more enzymes. All of them are aimed at ensuring exocrine function - maintaining the process of normal digestion. During inflammation of the pancreas, enzymes that are aggressive towards any tissue can cause self-digestion of the gland due to their high activity. The prognosis may be unfavorable if complications occur.
Pancreatic hormones
hyperfunction of insulin in the pancreas
The endocrine part of the pancreas produces 3 hormones:
Insulin is responsible for the synthesis of glycogen and accompanies the oxidation of sugar in muscles. When the islets of Langerhans stop functioning, the concentration of sugar in the blood increases sharply. This condition is called hyperglycemia. When sugar appears in urine, glucosuria develops. If its concentration in the blood decreases, hypoglycemia develops. Regulation of hormone secretion is carried out through neurohumoral and nervous mechanisms.
Glucagon is an insulin antagonist. It accompanies the development of hyperglycemia and reduces the concentration of glycogen in the liver. Lipocaine accompanies the removal of fats from this organ. The activity of the hormone helps inhibit the transformation of carbohydrates into fats.
There are several ways in which gland hormones influence carbohydrate metabolism. Thanks to insulin, glucose penetrates the cell membrane. This hormone helps induce enzyme synthesis. They synthesize glycogen and oxidize glucose. Thanks to the activity of glucagon, the content of the enzyme that breaks down glycogen increases.
Pancreatic hyperfunction
Hyperfunction of the pancreas depends on which part of the organ is pathologically altered. A manifestation of increased exocrine activity of the pancreas is enzyme release, the development of pancreatitis and all manifestations associated with its exacerbation. If left untreated, hyperfermentemia can lead to pancreatic necrosis and other life-threatening complications.
If intense secretion of pancreatic hormones occurs, this most often causes symptoms of hypoglycemia (with high synthesis of insulin by the gland). It is dangerous for the central nervous system.
Causes
There are three global reasons for the development of increased endocrine function of the pancreas:
- Errors in the treatment tactics of diabetes mellitus or treatment: insulin overdose or administration on an empty stomach.
- Pancreatic tumor - insulinoma. This is a general concept that unites all neoplasms from the islets of Langerhans. Includes the development of insulinoma, glucagonoma, gastrinoma, somatostatinoma and others. Insulinoma most often develops, but it is extremely rare among the population - 1 case per 250 thousand people per year. The remaining insulinomas, accordingly, occur with even less frequency.
- Tumors localized in the brain.
Insuloma
Most often, cells of different types are involved in the development and growth of insulinoma. About 60% of tumors produce insulin, but the secretion of gastrin, somatostatin, and pancreatic polypeptide may predominate. Insuloma develops as an adenoma, a benign neoplasm, or as adenocarcinoma, a malignant, rapidly progressive tumor. In the latter case, death is possible due to complications that arise due to the effect of large amounts of insulin on the body and the spread of the tumor.
According to statistics, among those diagnosed with insulinoma the following are identified:
- 80% – benign adenomas;
- 9% – with signs of malignancy;
- 11% – malignant adenocarcinomas.
The tumor develops at the age of 35-50 years, is detected 2 times more often in women than in men, and is practically never found in children. It is not a hereditary disease.
Types of insulinoma
- Insulinoma is an insulinoma with increased insulin production (when only pancreatic β-cells are involved in the process). In cases of insulinoma: 70% is adenoma, 30% is adenocarcinoma.
- Glucagonoma (one of the types of insulinoma) is extremely rare. It comes from the α-cells of the pancreas; when they grow, diabetes mellitus develops with all its signs. This is explained by the fact that glucagon, when secreted in excess, can significantly increase blood sugar levels by breaking down glycogen stores in the muscles and liver. The tumor is prone to malignancy, after which it acquires uncontrollable growth.
- Gastrinoma from g-cells producing gastrin. The hormone affects the condition of the stomach. In 90% of patients, it manifests itself with severe gastric damage in the form of Zollinger-Ellison syndrome (ulcerogenic syndrome). It is detected in men over 50 years of age. It is the most malignant (70%) among pancreatic tumors. Clinical symptoms are ulcers and diarrhea. Abnormally high levels of gastrin stimulate parietal cells. A large amount of gastric juice with a high content of hydrochloric acid is produced, which causes the formation of peptic ulcers.
- Somatostatinoma is a tumor of δ-cells of the pancreas. The rarest among insulinomas. Somatostatin, produced in excessive amounts, inhibits the secretion of somatotropic (GH - growth hormone, produced in the pituitary gland), thyroid-stimulating (thyroid hormone), insulin, glucagon, gastrin. The formation is prone to multiple metastases (in 74%) and is a genetic disorder. The clinical picture is varied, there is no specific picture (cholelithiasis develops due to the antispasmodic effect of somatostatin on the smooth muscles of the gallbladder, diabetes mellitus, anemia, diarrhea with rapid dehydration, weight loss). A sharp decrease in growth hormone (GH) leads to blocking the entry into the blood of the main hormone of the thymus (also called the thymus gland), thymosin. It affects calcium metabolism and neuromuscular transmission. In childhood, this slows down the sexual development and growth of the child.
Primary symptoms of the disease
Symptoms of the pathology depend on the prevalence of secretion of a particular hormone. Most often, insulin production increases.
The clinical picture is individual, but there are a number of disturbances in the condition that can be used to suspect pathology. This is Whipple's triad - symptoms associated with a drop in blood sugar:
- Spontaneous hypoglycemia (low sugar is determined after a night's sleep, hard work, or after fasting with loss of consciousness).
- Vegetative manifestations (excessive sweating, severe weakness and trembling in the body, palpitations, anxiety, fear, nausea, dizziness, vomiting, feeling of extreme hunger, in severe cases - coma).
- Rapid improvement after glucose administration.
Over time, neurological symptoms, hearing and vision impairment occur. More often appear:
- disorientation in the morning;
- convulsive attacks, prolonged in time, reminiscent of epileptic ones;
- autonomic disorders progress and become more frequent: hyperhidrosis (excessive sweating), severe weakness, facial flushing, lethargy, increased blood pressure (BP), attacks of tachycardia or arrhythmia;
- psychomotor agitation with incoherent speech and meaningless movements, similar to a state of intoxication;
- disturbance of consciousness up to coma.
The disease is dangerous because in the initial stages there are no specific symptoms. The condition resembles deep fatigue, asthenic syndrome, or occurs as vegetative-vascular dystonia. In many cases, the clinic develops gradually: absent-mindedness, lack of concentration appears, sometimes a person cannot concentrate and answer a simple question correctly.
Subsequently, as blood sugar levels drop, cases of psychomotor agitation occur (throwing, senseless searching, uncoordinated movements, inability to communicate). Elements of confusion with disorientation appear, which become more frequent and progress, states resembling a dream: a person goes somewhere or performs inexplicable and unconscious actions. Vegetative attacks may also become more frequent: sudden increases in blood pressure to high levels, attacks of palpitations, sweating. The condition is accompanied by dry mouth, nausea, and vomiting. After a year, irreversible changes in the psyche develop due to frequent episodes of hypoglycemia.
Despite frequent bouts of hunger, overeating in between can cause obesity. In most cases, with a long course of the disease, exhaustion and muscle atrophy occur.
Exacerbation of the disease
With pancreatic hyperfunction associated with increased insulin production, hypoglycemic states and coma occur. The deterioration associated with low blood sugar does not always occur gradually. Often this occurs suddenly and manifests itself as stupor, convulsions or an acute form of psychosis.
Signs of the initial stage are acute hunger, hand tremors, and autonomic disorders. If the development of hypoglycemia is not immediately stopped with carbohydrates (food or glucose administration), the attack will continue to develop. The following will appear:
- profuse sweating;
- trembling in the body;
- diplopia (double vision);
- fixed gaze;
- hemiplegia.
It is possible to develop a mental state reminiscent of alcohol intoxication: inability to navigate, hallucinations. If the condition is not normalized, vomiting, convulsive syndrome with clonic and tonic convulsions, confusion, and coma occur. Repeated attacks lead to personality degradation.
Symptoms of chronic hypoglycemia
Chronic hypoglycemia is manifested by weakness, apathy, a feeling of unreasonable fatigue, weakness, constant drowsiness during normal sleep patterns, headaches, and inability to concentrate. The symptoms are mild, the clinical picture resembles hypothyroidism. Usually the patient does not see a doctor, and the onset of the disease is missed. The pathology becomes chronic. Each symptom increases over time.
Precursors of a hypoglycemic attack are sweating, tremors, anxiety, palpitations, a drop in blood pressure, and a strong feeling of hunger. The condition can be interrupted by taking glucose.
Symptoms
Hyperfunction of the pancreas does not have a pronounced clinical picture. That is why the disease continues to develop, and patients do not even suspect it. The formation of a disorder does not in any way affect the person’s usual rhythm of life or preferences. The first signs may remind patients of symptoms of simple fatigue or nervous anxiety.
The main symptoms of the disease include the following:
- weakness;
- rapid fatigue;
- drowsiness;
- apathy;
- cramps of the arms and legs;
- blurred vision.
The faster a person reacts to such manifestations and suspects pathology, the more effective the therapy will be. If treatment is not started on time, the patient may die.
Symptoms of pancreatic hyperfunction
As the disease progresses, the patient’s general symptoms begin to worsen and the following signs appear:
- loss of orientation after sleep;
- psychomotor agitation;
- convulsions become similar to epileptic seizures;
- disruption of the autonomic nervous system;
- loss of consciousness, the person may fall into a coma.
Between periods of acute manifestation of symptoms, the patient experiences chronic hypoglycemia, which manifests itself in mental and emotional degradation, memory deterioration and a decrease in professional skills.
If malignant insulinomas develop, the patient begins to develop signs characteristic of cancer - diarrhea, frequent painful attacks, intoxication.
Hypofunction of the pancreas
Since the main pancreatic hormone, on which the safety and normal functioning of other organs depend, is insulin, reduced β-cell function leads to irreversible changes in the body. All types of metabolism are disrupted: protein synthesis, lipogenesis and gluconeogenesis are reduced. Hypofunction of the pancreas is much more common than increased hormone synthesis and is manifested by diabetes mellitus.
Symptoms of hypofunction
A manifestation of reduced pancreatic function is diabetes mellitus. It is characterized by:
- constant dry mouth;
- strong thirst;
- polyuria (excretion of large amounts of urine);
- weight loss;
- constant fatigue and weakness.
If adequate treatment is not carried out or the diet is violated, the disease progresses and complications develop: almost all organs and systems are affected. The kidneys, eyes (blindness may occur), the cardiovascular and nervous systems are especially affected, the blood supply to the legs is disrupted, diabetic foot and gangrene develop. The most dangerous complication is diabetic coma.
Diabetes mellitus with insulin hypofunction, taking into account the mechanism of damage, is divided into 2 types:
- insulin-dependent (type I) - caused by the destruction of β-cells, characterized by an absolute deficiency of insulin (in 10% of patients);
- insulin-independent (type II) - develops in obese people, with physical inactivity, stress, existing genetic predisposition, and is associated with impaired sensitivity of receptors to insulin.
Hypofunction of hormones
Hypofunction of hormones with damage to the pancreas is observed more often and is manifested by impaired insulin production, as a result of diabetes mellitus. Currently, the structure and properties of insulin have been studied, it has been synthesized and is widely used in the treatment of this pathology. This makes it possible to prolong the life of patients. But patients have to take insulin replacement therapy and follow a special diet all their lives.
Adrenal glands and their significance
The adrenal glands are paired glands consisting of a cortex and medulla. They are responsible for the production of several hormones:
Each of these hormones is important, so proper functioning of the adrenal glands has a direct impact on the functioning of the entire body. For example, corticosterone maintains optimal levels of fats, proteins and carbohydrates, and also ensures the functioning of the immune system. Adrenaline is responsible for the speed of reaction in tense situations. The normal functioning of the reproductive system and the manifestation of secondary sexual characteristics depend on steroids. The adrenal glands perform several important functions:
- They normalize metabolism and prevent disruptions in this process.
- Provides rapid adaptation of the body to stress and rapid recovery from it.
If the functioning of the paired organ is disrupted, serious diseases may develop and a significant deterioration in the person’s general well-being.
Methods for diagnosing pancreatic dysfunction
If pancreatic dysfunction is suspected, a thorough examination is necessary. Among the laboratory methods prescribed for insulinoma:
- blood and urine test for sugar;
- if necessary, additional stress tests with a carbohydrate breakfast and insulin;
- During a spontaneous attack of insulinoma, the level of insulin in the blood is determined.
Functional methods used:
- Ultrasound of the obstructive tissue and cerebral palsy - to detect a tumor and changes in neighboring organs, if any;
- CT scan - if there are any doubts during an ultrasound examination.
When diagnosing glucanoma:
- blood and urine sugar;
- glucagon in the blood.
For gastrinoma:
- blood for gastrin on an empty stomach;
- X-ray and endoscopic examination to detect ulcers in the mucous membrane of the stomach and intestines;
- acidity of gastric juice.
The localization of the tumor is determined in a standard manner, as with insulinoma.
Hypofunction
In this case, we are talking about reduced hormone production. At the same time, it is noticeable how the internal organs gradually lose their functions. In the acute stage, the patient experiences a decrease in vital tone and disturbances in the functioning of vital systems. Chronic hypofunction has a secondary and tertiary form. The first develops when adrenal tissue is damaged. The second is diagnosed less frequently and leads to gradual atrophy of the gland.
Causes
Hypofunction occurs as a result of improper autoimmune reactions of the body, causing destruction of tissues and cells of the adrenal glands. This is the most common cause of the disease. Sometimes tuberculosis of the paired gland becomes a provoking factor. In addition, hypofunction can be caused by:
- bad heredity,
- cardiovascular pathologies,
- pituitary tumors,
- disorders of the immune system.
Symptoms
Hypofunction of the adrenal glands manifests itself in a number of symptoms. The main one is a change in skin color to a darker shade. The severity of the pathology and the duration of its course influence the severity of pigmentation. First, it is observed on open areas of the body - arms, face, neck. Sometimes white spots are observed, which are called “vitiligo”. Brown areas may form on the mucous membranes. Other manifestations include:
- chronic fatigue and muscle weakness,
- weight loss for no apparent reason,
- digestive disorders,
- low blood pressure,
- irritability, apathy,
- memory impairment, absent-mindedness.
Hypofunction and hyperfunction of the adrenal glands indicate the development of a serious disease, so you should not ignore the very first alarming symptoms. It is urgent to visit a therapist.
Treatment of the disease
Tumors (insuliomas) are treated surgically using the following methods:
- enucleation - successfully used in the early stages of the disease;
- distal resection of the pancreas;
- laparoscopy.
Gastrinoma is treated with drugs that suppress the secretion of hydrochloric acid:
- PPIs (proton pump inhibitors) - Pantaprazole, Rabeprazole, Omeprazole;
- H2 receptor blockers - Cimetidine, Ranitidine, Famotidine.
In severe cases, surgical intervention is used - gastrectomy.
To treat hypofunction, manifested by low blood sugar, a carbohydrate diet and glucose administration are necessary; when a tumor is diagnosed, surgical treatment and a course of chemotherapy are required. It is possible to prescribe drugs that suppress insulin - Diazoxide, Octreotide and the pancreatic hormone - Glucagon. Drugs that reduce insulin impair the exocrine function of the pancreas, so enzyme therapy is recommended at the same time.
In the treatment of diabetes mellitus, insulin, glucose-lowering drugs, and a strict diet are used - table No. 9 according to Pevzner. When insulin is prescribed, the patient is taught to use a special table indicating the carbohydrate content of foods and the number of conventional bread units, from which the required dose of insulin can be calculated in case of a nutritional disorder.
Treatment
If a patient is diagnosed with insulinoma as the cause of pancreatic hyperfunction, he is offered surgical intervention. If the location and size of the tumor allows, then the tumor itself is excised during surgery. In some cases, part of the gland is removed. If the tumor is malignant, then chemotherapy must be added to the complex of treatment measures. The effectiveness of surgical treatment for insulinoma is quite high - about 90%. However, operative mortality can reach 10%
Sometimes, for some reason, surgical treatment is not possible. In such cases, the main goal of therapy is to maintain a stable level of glucose in the patient's blood. For this purpose, medications are used that increase sugar - glucagon, corticosteroid hormones. Diazoxide and octreotide are used to suppress secretion. When prescribing octreotide, pancreatic enzymes are added, since the drug also suppresses the exocrine function of the gland.
Complications of hormone dysfunction
If pancreatic function is reduced, insulin production is reduced and diabetes mellitus develops, in the absence of adequate treatment or poor diet, the disease progresses. Complications develop in which the vessels and tissues of almost all organs and systems are affected. The kidneys, eyes (blindness may occur), the cardiovascular and nervous systems suffer greatly, the blood supply to the legs is disrupted, diabetic foot and gangrene develop. The most serious complication is diabetic coma.
It is impossible to completely cure pancreatic dysfunction, but with timely treatment and early therapeutic or surgical treatment, the quality of life can be improved, and in some cases, saved.
Bibliography
- Mikhailov V.V. Fundamentals of pathological physiology. Guide for doctors. M. Medicine 2001
- Joseph M. Henderson. Pathophysiology of the digestive organs. Beanom Publishers 1997
- Almazov V.A. Clinical pathophysiology: a textbook for university students. 3rd edition revised and expanded. St. Petersburg Peter 1999
- Starkova N.T. Clinical endocrinology. 3rd edition revised and expanded - St. Petersburg. Peter 2002
Is there prevention?
To prevent the occurrence of pancreatic hyperfunction, it is necessary to maintain its normal functioning. You need to eat right, give up bad habits, lead an active lifestyle, and watch your weight. If you have diabetes, you must strictly follow the dosage of medications prescribed by your doctor.
Pancreatic hyperfunction gradually progresses, its symptoms become more severe. Without treatment, attacks will worsen, affecting the kidneys, cardiovascular and nervous systems. The most severe complications are diabetic coma and, as a result, the death of the patient.
Hormones of the pituitary gland and hypothalamus: ratio, functions and possible diseases
The pituitary gland and hypothalamus are important components of the human endocrine system that produce various hormones. Almost everyone knows these complex names and understands their connection with the brain, but what do the hypothalamus and pituitary gland actually do and what is their role in human life and health?
Hypothalamic-pituitary system
The importance of the pituitary gland and hypothalamus in the human body
The pituitary gland is a cerebral appendage located under the cerebral cortex. It is tiny in size but performs very important functions. This endocrine gland regulates processes such as growth and development, sexual function and reproductive ability, and metabolism.
The tiny pituitary gland is divided according to its structure into lobes, each of which has its own functions. Each of the lobes (anterior, posterior and intermediate) has its own groups of cells that produce certain hormones that regulate various systems and functions of the body.
The concepts of gigantism and dwarfism are associated with underdevelopment or excessive action of the pituitary gland. The pituitary gland is connected to the hypothalamus, part of the diencephalon. This small area acts as a coordinator.
It produces hormones by communicating with the pituitary gland. Hormones affect the pituitary gland and provoke the production of other hormones that control almost the entire endocrine system of the body.
Conditions of the body such as hunger or thirst, as well as sleep, depend on the work of the hypothalamus.
Hormones of the pituitary gland and hypothalamus play an important role - this is a complex process of coordinating the work of the entire organism as a whole.
The posterior lobe of the pituitary gland is the receiver of signals sent by the hypothalamus. The intermediate lobe of the pituitary gland in humans is only a thin layer. In some animals it is very well developed.
More information about the hypothalamic-pituitary system can be found in the video.
Various malfunctions in the functioning of the hypothalamic-pituitary system lead to serious and irreversible disorders.
For example, a tumor of the pituitary gland leads to serious visual impairment, and the hypothalamus plays the role of an indicator of hunger or satiety.
There is a theory according to which obesity can be treated by directly influencing the hypothalamus. If the functioning of the hypothalamus was disrupted in childhood, the child's growth will be slowed down, and there will also be problems with the formation of sexual characteristics.
Functions of hormones
Description of the hormones of the pituitary gland and hypothalamus
Each section of the pituitary gland and the hypothalamus itself produce their own individual hormones (releasing hormones), which are vital for the body to function normally.
Let's look at some of them:
- Somatoliberin. This is a hormone of the hypothalamus that affects the pituitary gland. It is also called growth hormone. Its deficiency leads to short stature, and its excess leads to tall stature or even gigantism. This hormone enhances protein production and fat breakdown. During the day, the hormone level is not too high, but it increases during eating and sleeping.
- Prolactin. Prolactin is produced by the pituitary gland. It is of direct importance for reproduction and lactation. First of all, it affects the mammary glands, their growth, the production of colostrum and its conversion into breast milk. Immediately after childbirth, this hormone begins to be actively produced, provoking lactation. Around the third day, colostrum and milk begin to be released.
- Gonadotropic hormones of the pituitary gland. There are 3 such hormones that are responsible for the sexual functions of the body: follicle-stimulating (formation of follicles and formation of the corpus luteum), luteinizing (transformation of the follicle into the corpus luteum) and luteotropic (the already known prolactin).
- Thiroliberin. It is produced by the hypothalamus and affects the pituitary gland, which provokes the production of a similar hormone in it. The effect of this hormone on the nervous system and the reduction of depression at sufficient levels has been proven. An excess of this hormone can lead to sexual dysfunction.
- Corticotropin. Produced by the pituitary gland and controls the functioning of the adrenal glands, and is also responsible for the production of steroid hormones. It promotes the breakdown of fatty tissue. An excess of this hormone leads to disruptions in the functioning of almost all internal organs; muscles and bones undergo changes. Adipose tissue develops unevenly: in some areas of the body it is in excess, in others it is absent.
Diseases related to hormones
Gigantism - malfunctions of the hormonal system
Hormones of the hypothalamic-pituitary system must be in constant balance. This system is complex and has many different connections with other systems and organs. Any failure leads to serious consequences.
There are a lot of diseases caused by dysfunction of the pituitary gland and hypothalamus.
They have a complex system of symptoms and are quite difficult to diagnose and treat:
- Gigantism. This is a rare disease associated with excessive production of growth hormone by the pituitary gland. In addition to their incredibly tall stature, these people also suffer from other complications, such as severe joint pain, headaches, fatigue, infertility, heart failure, etc. This disease is treated with the hormone somatostatin, which controls growth. Unfortunately, most patients with this disease do not live to old age due to the large number of complications.
- Acromegaly. A disease similar to gigantism, expressed in enlargement of the bones of the skull, especially the facial bones, as well as the feet and hands. This disease does not develop immediately, but only after growth has completed. It can proceed slowly, changing a person’s appearance from year to year. Facial features become rough and large, and hands and feet become disproportionately large. In addition, hypertension, sleep apnea, and high blood pressure are observed.
- Itsenko-Cushing's disease. This is a serious disease caused by malfunctions in the hypothalamic-pituitary system. It is associated with excessive release of corticotropin. As a result, metabolic processes in the body are disrupted, fat is actively and unevenly deposited, stretch marks appear, hair on the body and face actively grows, bones become brittle, immunity drops, and the entire sexual sphere is disrupted. With a mild form of the disease, the prognosis is quite favorable. However, in severe cases, even after recovery, irreversible consequences remain, for example, renal failure.
Failures in the hypothalamic-pituitary system often lead to severe complications and are difficult to treat. A large number of diseases are associated with tumors of the pituitary gland, which determines the excess or deficiency of hormones secreted by it.
Source: https://DiagnozLab.com/analysis/hormones/gormony-gipofiza-i-gipotalamusa.html
Hyperfunction of the pituitary gland due to disruption of the body's endocrine system
Hypo and hyperfunction of the pituitary gland today is a fairly common phenomenon among people all over the world. The secret functioning is disrupted for various reasons. Hyperfunction and hypofunction are such diseases during which the pituitary gland produces too much or too little hormones, which affects the development of the body and its functions.
Hyperfunction of the pituitary gland is a disease in which the gland begins to produce large amounts of different types of hormones. Since the pituitary gland is the main gland of the endocrine system, which controls the work of all other secretions, if its work is disrupted, a malfunction occurs in the body.
Hormones secreted by the pituitary gland
Hyperfunction of the pituitary gland involves the production of a large number of different types of hormones by the gland. The pituitary gland can produce the following hormones:
- Thyroid-stimulating.
- Prolactin.
- Self-tropic.
Also, if the gland malfunctions, it can produce large quantities of other hormones.
Causes of pathology
Hyperfunction of the pituitary gland can manifest itself due to two main factors:
- Congenital.
- Purchased.
In the first type of pathology, it is transmitted from parents to children at the genetic level. Acquired hyperfunction can be caused by:
- Infectious diseases.
- Head injuries.
- Using medications for a long time.
- Stress.
- Blood flow disorders.
- Autoimmune processes.
- Tumors.
Signs of pathology
Hyperfunction can have different symptoms. Here everything will depend on which hormone is in excess in the body. Most often, a patient with this diagnosis may experience the following symptoms:
- Muscle weakness.
- Menstrual irregularities.
- Acceleration of metabolic processes.
- Increased blood pressure.
- Infertility.
- Frequent pulse.
- Fatigue. Mental disorders.
- Brittle nails and hair.
- Stretch marks on the skin.
Hyperthyroidism: diagnosis
Pituitary dysfunction is diagnosed when the patient undergoes tests. When examining the material in the laboratory, the specialist initially determines which hormone is in excess in the body. Next, the biochemical indicator of the material is tested.
If the doctor does not have enough data obtained in the laboratory to make a diagnosis, he may prescribe other types of examinations using special equipment. This:
After an accurate diagnosis and identification of the causes of dysfunction of the pituitary gland, the doctor prescribes appropriate therapy.
Treatment
If a person notices negative manifestations that happen to him, then it is important for him to get checked by a doctor. It is also worth visiting the clinic if the above symptoms are detected. When treatment is not diagnosed in time and treatment does not occur at first, this can cause complications and the manifestation of the following diseases:
- Diabetes.
- Disorders in the reproductive system.
- Violation of salt and water balance.
- Obesity.
- Violation of the structure of blood vessels.
- Osteoporosis.
- Thyrotoxicosis.
If a person has a large amount of hormones in the body that are produced by the adenohypophysis, the doctor will prescribe appropriate therapy. Medicines are prescribed depending on the type of pathology, its neglect and the general condition of the person.
Treatment is usually done with medications that can control the pituitary gland's production of hormones. Such medications are prescribed only by a doctor. Throughout the course of treatment, the patient must be constantly monitored by a doctor to monitor the treatment process.
If necessary, the therapy can be changed. The doctor will prescribe other medications. It all depends on the analysis.
It is also important to adhere to a certain diet during the course of treatment. Nutrition should be balanced and rich in vitamins or minerals. The patient should avoid eating large amounts of salty and fatty foods. You need to eat more foods that contain iodine.
Complications of pathology
When a person does not receive timely help when such a disease appears, he may have complications. They are:
- Intoxication.
- Malfunction of the endocrine system.
- Poor absorption of glucose.
- Rapid weight gain.
- Menstrual irregularities.
- Bone fragility.
- Infertility.
Preventive actions
To prevent the manifestation of such a disease, certain preventive measures must be followed. It is worth noting that it is impossible to prevent the congenital type of disease. By maintaining the correct lifestyle, you can only prevent the development of an acquired pathology.
To do this, doctors recommend taking the following measures:
- Avoid head injuries.
- Avoid stress.
- Treat all infectious diseases in a timely manner.
- Follow a diet.
- Live the right way of life.
- To refuse from bad habits.
- Monitor water and salt balance.
- Do not stay in the sun for a long time.
- Strengthen the immune system and strengthen the body.
- When the first negative symptoms appear, consult a doctor immediately.
Conclusion
Based on the above, it is clear that pituitary hyperfunction is a rather dangerous disease that requires timely treatment. Therefore, a person should be constantly monitored by a doctor, who can diagnose the pathology in a timely manner.
It is also important to lead a healthy lifestyle and follow all doctor’s instructions during treatment. This is the only way to get rid of the pathology in a short time, as well as prevent its development.
It is also worth noting that today it is possible to treat hyperfunction using folk remedies. For this you can use herbal decoctions. You can prepare this decoction yourself at home.
Before starting such treatment, you should definitely consult a doctor who will assess all the risks and give the right advice. It is also worth understanding that treatment with folk remedies cannot be the main type of therapy.
Herbal decoctions will help support the body, strengthen the immune system, improve metabolic processes and improve well-being. But herbs will not be able to control the secretion of hormones, and therefore you will need to take medications prescribed by your doctor.
If you approach the treatment of pathology responsibly and start it on time, and also adhere to all the doctor’s recommendations, then the prognosis will be positive. After completing the full course of treatment, a person will be able to lead a normal life in the future.
Knowing these points, everyone will be able to draw certain conclusions for themselves and make the right decision if necessary. Once again, it should be noted that successful treatment of hyperfunction is only possible if it is of an acquired type. Doctors do not yet know exactly the reasons for the manifestation of congenital hyperfunction, and therefore it is impossible to prevent such a disease.
Optimization of the thyroid gland Acceptance of a man's father Psychosomatics thyroid gland hyperfunction Psychosomatics of the endocrine system Vitamin D Calcium metabolism Pituitary gland Thyroid Ovaries Testicles Louise Hay. Health Affirmations – Hyperfunction
Source: https://endokrinologiya.com/diseases/giperfunkciya-gipofiza
Traditional treatment
For hyperfunction and hypofunction of the adrenal glands, in addition to the main therapy, alternative medicine recipes can be used. Among the most popular means are:
- Snowdrop tincture - pour dry inflorescences with vodka and send to a sunny place for forty days. Take the finished medicine twenty drops up to three times a day. If desired, you can add a spoonful of flower honey to it. The product improves the functioning of paired glands.
- Geranium infusion - pour boiling water over the crushed leaves of the plant, leave for ten minutes and cool. Take the medicine twice a day after meals.
- Horsetail – brew and let stand for ten minutes. Drink the herbal infusion like regular tea.
Adrenal dysfunction is a very dangerous condition. If alarming symptoms appear, you must urgently visit a doctor, otherwise serious consequences cannot be avoided.