The number of people who suffer from gastrointestinal diseases is growing every year. According to statistics, every 3 people have problems with the digestive system. Unfortunately, these statistics also include children. The pancreas is often affected. This important organ is “responsible” for the production of insulin and the secretion of pancreatic fluid, which is necessary for complete digestion.
Reactive changes in the pancreas are often diagnosed in children and adolescents. The problem lies in the fact that this particular category is very fond of “junk” food, such as crackers, chips, soda, etc. However, reactive changes are not always a consequence of dietary disturbances. Sometimes they appear against the background of antibiotic therapy, other gastrointestinal pathologies, as well as damage to organs localized in the abdominal cavity.
Any malfunction of the digestive system is already a pathology. It is important to know when this is just a minor deviation from the norm and when medical intervention is required. If a child begins to complain of pain in the left side or in the epigastrium, you should definitely show him to your doctor.
Development of pathology
Reactive pancreatitis is not an independent disease. Damage to pancreatic tissue is secondary changes that develop against the background of various pathological conditions.
They can lead to:
- poor nutrition with consumption of large quantities of semi-finished products, foods with preservatives and other chemical additives;
- infectious and autoimmune pathologies. “Children’s” infections are of great importance: measles, rubella, scarlet fever, etc.;
- damage to the biliary tract and gallbladder: duct dyskinesia, cholelithiasis, etc.;
- congenital anomalies of the structure of the pancreas;
- long-term use of medications from the group of antibiotics, cytostatics or glucocorticosteroids;
- traumatic injuries to the abdominal area;
- hereditary predisposition.
These conditions lead to premature activation of enzymes in pancreatic juice. This happens at the moment when they are located inside the ducts of the organ. Activated enzymes begin to damage cells and the connective tissue located between them.
As a result, ductal changes in the child’s pancreas contribute to even greater damage to the organ’s parenchyma and increased inflammation.
The reactive state is characterized by pathological processes such as dystrophy and necrosis. Necrosis is the irreversible death of a cell, in which the integrity of its membrane is disrupted and the contents are released into the extracellular environment.
Dystrophy is reversible and is manifested by metabolic disorders in the cells of the organ.
Healing procedures
The identified diffuse changes in the gland are secondary and do not require special treatment. With timely and adequate treatment of the underlying disease, the condition of the pancreas is normalized, so there is no need to prescribe an extra drug so as not to functionally burden the digestive organs.
The main treatment procedures for diffusely altered pancreas are:
- giving up alcohol;
- diet;
- limiting physical activity until complete remission occurs.
Drug therapy is prescribed taking into account the underlying pathology that caused changes in the gland. It is possible to use symptomatic treatment when abnormalities are detected in the tests and there are complaints and symptoms indicating a dysfunction of the pancreas. In such cases, depending on the patient’s condition and the degree of manifestation of symptoms of pancreatic damage, the following are used:
- enzymes;
- antispasmodics;
- carminatives - to reduce flatulence;
- antisecretory, reducing the production of hydrochloric acid - it stimulates the functions of the pancreas and increases its functional load.
Negative consequences
The prognosis for the child is favorable in cases where the disease is detected at the initial stages of development . With late diagnosis, pancreatitis becomes chronic due to diffuse reactive changes in the pancreas and an intense inflammatory reaction. In this case, the disease becomes cyclical with periodic exacerbations and remissions.
As the pathology progresses in the absence of treatment, pancreatic necrosis may develop, that is, total death of the pancreas and adjacent tissues. Against this background, aseptic peritonitis and pain shock develop. Without intensive care, most patients die.
The long course of the disease is characterized by exocrine and endocrine insufficiency. The pancreas secretes pancreatic juice, which contains enzymes necessary to digest food. Their deficiency leads to dyspeptic disorders (nausea, vomiting, etc.), since the products are not digested and are not absorbed from the intestines into the blood.
Children with chronic pancreatitis have an increased risk of developing diabetes because the organ contains cells that secrete insulin. This is a hormone that controls blood glucose levels.
Diagnosis
Reactive changes occurring in the pancreas can be diagnosed using ultrasound, which examines all organs that are possible causes of an attack.
On ultrasound, the parenchyma of a healthy pancreas is homogeneous. Its size is neither increased nor decreased, without any foci or diffuse changes.
Diffuse changes are not a diagnosis, but a condition of the pancreas. In this case, the changes are distributed evenly throughout the organ tissue. When the changes are focal in nature, then most likely the patient has tumors or stones in the gland.
In addition, during an ultrasound examination in a diseased organ, a different nature of diffuse changes can be revealed, due to which one or another diagnosis is established:
- diffuse decrease in the density of echogenicity and parenchyma (if the parameters of the organ have increased, this confirms the presence of an attack of acute pancreatitis;
- diffuse changes in the pancreas with increased echogenicity and density with a reduced or normal size of the gland (typical in the presence of fibrosis);
- diffuse decrease in echogenicity and decrease in parenchyma density, in which the organ does not increase (the phenomenon is typical for reactive and chronic changes);
- a diffuse increase in echogenicity with natural parameters of the gland may indicate lymphomatosis (the disease is characterized by partial replacement of fat parenchyma;
Due to the fact that, based only on ultrasound, it is quite difficult to establish an accurate diagnosis of the disease, it is necessary to carry out additional diagnostic studies, which include:
- endoscopy of the duodenum (carried out to examine the mucous membrane at the place where the duct enters);
- general and biochemical blood test (done to determine organ dysfunction and to diagnose or exclude the presence of inflammation);
- urine analysis for the content of digestive enzymes.
Afterwards, the results of all tests are carefully examined by a gastroenterologist. Then he announces the exact diagnosis and prescribes treatment to combat this or that ailment.
It should be noted that reactive changes do not require special therapy, therefore, when the main ailment of the gastrointestinal tract or liver is cured, not a trace will remain of them.
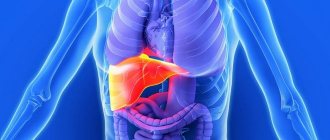
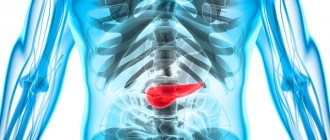
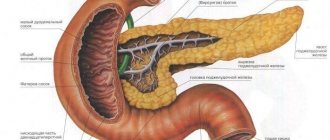
The pancreas is one of the largest organs of the digestive system; in size it is slightly second only to the liver. The gland consists of a head, tail and body, interspersed with one another.
The organ produces special enzymes that are directly involved in the process of digesting food; the pancreas also produces the hormone insulin, which is responsible for blood glucose levels.
The gland is partially covered by the stomach and is connected by ducts to the liver and biliary system. If any pathological process begins in it, it may well be the body’s reaction to chronic diseases of the abdominal organs. When reactive changes occur, a number of significant physiological disorders are observed that contribute to the development of a host of ailments.
The pancreas is assigned to perform two important functions:
In the first case, they talk about the production of the hormone insulin, in the second – about the secretion of pancreatic juice, without which a normal digestive process is impossible. When pathological changes occur in an organ, the entire body cannot function fully.
Clinical manifestations
Speaking about the symptoms of reactive changes in the pancreas in a child and what it is, doctors identify a number of characteristic signs of the disease. Their knowledge allows parents to suspect the disease at an early stage and promptly seek medical help.
The main manifestations of reactive pancreatitis:
- acute pain syndrome localized in the upper abdomen. Pain may radiate to the hypochondrium or lumbar region;
- low-grade fever - up to 38°C;
- dyspeptic disorders in the form of nausea, vomiting, diarrhea, bloating and lack of appetite;
- general weakness and fatigue;
- with a concomitant violation of the outflow of bile, yellowness of the skin and sclera develops.
If the disease occurs in young children, they cannot always describe their complaints to their parents. In this case, the child becomes restless, whiny and refuses to eat. A timely visit to the pediatrician can prevent the progression of pathology and the development of complications.
Reactive pancreatitis in a child
I received a letter asking me to tell you what reactive pancreatitis is in a child, what the symptoms are, how reactive pancreatitis in children is treated.
This letter was sent by a reader in response to the article “What does it mean to take care of the pancreas”
Here is the letter:
“Hello, please explain to me what reactive pancreatitis is, namely reactive pancreatitis in a child, symptoms and treatment of reactive pancreatitis in children. It all started when my daughter suddenly developed diarrhea at night. Temperature 37.2 degrees. The doctor diagnosed reactive pancreatitis, which arose due to existing cholecystitis.”
I will answer all the questions in this letter in this article.
The fact that reactive pancreatitis is a secondary disease, a disease caused by some primary disease, as a response was written earlier in the article “What is reactive pancreatitis?”
What can trigger the development of reactive pancreatitis was written in the previous article “What is reactive pancreatitis?” Today we will talk about reactive pancreatitis in children.
Causes of reactive pancreatitis in children
- The main cause of reactive pancreatitis in a child is gross violations of the rules and diet. The thoughtless introduction of new foods in infancy is especially dangerous.
Newly introduced products that are not age-appropriate cause increased gas formation and increased stress on the pancreas. The pancreas cannot cope and becomes inflamed.In infancy, reactive pancreatitis is often fatal.
Errors are also observed in the organization of nutrition for preschool and school-age children.
Malnutrition in children is one of the main causes of acute diseases, including the occurrence of reactive pancreatitis. Do not forget that chronic diseases begin to form at this age.
Chips, kirieshki, even store-bought juice, as well as any products that contain flavor enhancers and preservatives, can provoke inflammation of the pancreas in a child.
In addition, the causes of reactive pancreatitis in a child include:
- taking certain medications (metronidazole, furosemide);
- abdominal injuries;
- pathology of the development of the gastrointestinal tract, including abnormalities of the duodenal ducts;
- congenital pathology of the development of the pancreas and its ducts;
- infections;
- stress and emotional distress
Reactive pancreatitis in a child Symptoms
The symptoms of reactive pancreatitis in children and adults are the same. Inflammation of the pancreas manifests itself in an acute form, suddenly.
- burning and girdling pain;
- nausea, vomiting;
- elevated temperature
- heartbeat;
- weakness;
- diarrhea.
Behavior of parents when signs of pancreatitis occur in a child
You should know and follow the main rule - “cold, hunger, and peace”
- immediately call an ambulance;
- provide peace to the child;
- cold heating pad on the abdominal area, shifted to the left.
Since reactive pancreatitis is an inflammation of the pancreas, which results in destruction of the organ, treatment should be taken seriously and responsibly. The child is placed in a hospital to ensure constant medical monitoring. Treatment and nutrition are prescribed according to the severity of the disease.
Diagnosis of reactive pancreatitis in a child
Diagnosing reactive pancreatitis in a child is quite difficult; to do this, you must undergo the following procedures:
- undergo an ultrasound (ultrasound examination of the abdominal cavity);
- take a general urine test;
- take an x-ray of the abdominal cavity;
- do a gastroscopy;
- undergo a computed tomography scan;
- take a biochemical and clinical blood test.
All of these procedures are important, and each of them helps determine the extent of damage to the abdominal cavity. A clinical blood test is necessary to determine the number of leukocytes; with illness, its level increases. A biochemical blood test shows how elevated the level of the amylase enzyme is and allows for a final diagnosis.
Using gastroscopy, the doctor can take material for a biopsy, as well as determine the degree of inflammation of the stomach and duodenum. An abdominal ultrasound is used to determine what changes from the norm have occurred in the duodenum and organs of the gastrointestinal tract. To assess the general condition of the body, doctors perform a computed tomography scan.
Reactive pancreatitis in a child Treatment
Reactive pancreatitis most often manifests itself in an acute form. This fact does not mean that a non-acute form of reactive pancreatitis does not exist. Of course there is, but, on the one hand, patients do not pay due attention to this and do not consult a doctor, on the other hand, doctors often attribute symptoms to other diseases. Thus,
REACTIVE pancreatitis requires immediate treatment. Treatment should be carried out under the supervision of a physician. Self-treatment of the disease often leads to the transition of this form of the disease to chronic.
However, parents often fail to promptly begin treatment for reactive pancreatitis in young children. It happens that parents think that the child is capricious. They try to feed the child through force, and thereby aggravate the situation.
Basic treatment tactics:
- pain relief,
- providing rest (rest) to the pancreas,
- administration of enzymes similar to those normally produced by the pancreas,
- diet.
Diet for reactive pancreatitis in children
The goal of therapeutic nutrition is to eliminate inflammatory changes and restore functional disorders of the pancreas by ensuring maximum sparing of the pancreas.
The first 1-3 days. Depending on the severity of the disease, the patient is prescribed the first fast. At this time, food does not enter the esophagus, and there is no secretory activity of the digestive organs.
Provides peace and restoration of the inflamed organ. Allowed: Borjomi type mineral water. The volume of mineral water is calculated as 5 ml per 1 kg of child’s weight.
The water should be still, warm, taken 6 times a day.
The first option of diet No. 5p is gentle. Duration - about 2 weeks. Dishes are pureed. The transition to the first version of diet No. 5p should be gradual.
The volume and diet gradually increases - find out how here >>. The menu for reactive pancreatitis in the acute period corresponds to the menu for acute pancreatitis.
A sample menu is presented on the website, as well as in the article “Diet for pancreatitis. Sample menu."
The second option of diet No. 5p is beyond the acute stage . Duration 2-3 months. The dishes are not pureed. The transition from the first option of diet No. 5p to the second should also be gradual.
I offer you a sample menu for the second option of diet No. 5p
Diet No. 5 is the next stage. Shared table. With the doctor's permission, if the treatment was successful and chronic pancreatitis did not develop. You can read more about the first and second options of diet No. 5p on the pages of this project - diet No. 5p for pancreatitis.
A complete list of dishes recommended in medical nutrition will help you determine what you can eat with reactive pancreatitis. It is necessary to completely normalize the child’s diet and completely eliminate junk food from the diet. The main thing is to eat regularly, preferably 6 times a day in small doses.
It is necessary to completely remove sweets, flour, fatty, spicy, and salty foods from the child’s diet. You also need to exclude coffee, chocolate, cocoa, and concentrated juices from your menu.
Food must be steamed, it must be completely ground, and it is also very important to reduce the calorie content of food. When dieting, it is very important to consider weight, lifestyle, activity and chronic diseases.
So, it is very important to cure chronic and acute pancreatitis in a child in time so that serious health problems do not arise in the future.
In the treatment of reactive pancreatitis, special attention should be paid to nutrition.
List of allowed and prohibited foods in the diet for reactive pancreatitis
List of allowed productsList of prohibited products
| Soups | slimy soups prepared from various cereals in water; pureed vegetable soups; boiled chopped meat can be added to the soup. | meat, fish, mushroom or vegetable decoctions, broths; |
| Meat, meat dishes | Lean meat in the form of steam cutlets, meatballs; | Fatty meat - pork, lamb |
| Fish, fish dishes | Low-fat river fish in the form of steam cutlets, meatballs; | Fatty fish |
| Eggs | Steamed egg white omelette; | Fried eggs, scrambled eggs, boiled eggs |
| Cereals | porridge: Buckwheat, oatmeal, rice; | Millet |
| Potatoes and vegetables | Mashed potatoes. | Raw vegetables (especially cabbage, radishes, peas, beans and others) |
| Fruits and berries. Fruit and berry dishes | Baked apples of non-acidic varieties, | Fruits containing coarse fiber can cause bloating |
| Beverages | Fruit compotes, jelly, jelly, mousse. | Coffee, cocoa, sour fruit and vegetable juices, carbonated drinks. |
| Butter. Fats. | Butter can be added to prepared dishes in small quantities. | Fats are sharply limited |
| Bread and bakery products | The bread used is white, yesterday's bread, dry biscuits | Fresh bread, buns, cakes and pastries |
Sample menu for reactive pancreatitis in children
Below is a version of a one-day menu for pancreatitis:
| Approximate one-day MENU of diet No. 5p (mechanical sparing) | |
| Name of dishes | |
| 1 breakfast | Steam curd soufflé |
| Oatmeal milk porridge pureed without sugar | |
| Tea | |
| 2 breakfast | Fresh low-fat cottage cheese |
| Dinner | Vegetarian pureed vegetable soup, 1/2 serving without sour cream and cabbage |
| Vegetable puree | |
| Compote of pureed apples without sugar | |
| Afternoon snack | Steamed protein omelette |
| Rose hip decoction | |
| Dinner | Fish soufflé with cottage cheese |
| Mashed potatoes | |
| Mashed rice milk porridge without sugar | |
| Tea | |
| For the night | Kefir |
| All day: | White crackers |
A few more menu options for pancreatitis
I. In the article “Diet for pancreatitis. Sample menu" You will find three menu options:
Option I of diet menu No. 5p, a more strict option. Menu with mechanical sparing; II option of diet menu No. 5p, outside the acute stage, i.e. without mechanical sparing; Diet menu No. 5p for constipation.
II. Menu for pancreatitis beyond the acute stage
III. Menu for one day Recipes And also follow the “memo” on dietary nutrition for pancreatitis. I sincerely wish you health!
Using the list of permitted and prohibited foods and guided by a sample penalty, you can choose a diet so that your child eats with pleasure.
After the child recovers, the diet should be expanded. The food may no longer be pureed, but what is written in the table - “List of Prohibited Products” – remains prohibited. The baby should be fed frequently 4-6 times a day. All dishes are steamed, baked in the oven, or in a slow cooker.
Source: https://pancr.ru/pankcreatit/reaktivnyj-pankcreatit-u-rebenka.html
Diagnostic measures
Symptoms of reactive pancreatitis are similar to a large number of diseases: primary damage to the pancreas, bile duct dyskinesia, acute appendicitis, etc.
To clarify the diagnosis, the examination includes the following methods:
- clinical blood test. The study reveals inflammatory changes: leukocytosis (increase in the number of leukocytes) and acceleration of ESR (erythrocyte sedimentation rate);
- in a biochemical blood test, the level of inflammatory proteins (C-reactive protein, fibrinogen) and pancreatic enzymes (amylase, lipase, etc.) increases;
- in the coprogram a large amount of fat and undigested starch residues are detected;
- Ultrasound of the pancreas is the “gold standard” for diagnosis. The study makes it possible to make an accurate diagnosis by identifying echographic signs of pathology: heterogeneity of structure and the appearance of hypoechoic formations.
In complex diagnostic cases, computed tomography or magnetic resonance imaging, as well as endoscopic retrograde cholangiopancreatography, are performed. If necessary, consultations with a gastroenterologist, geneticist and other specialists are indicated.
Attention! Only a doctor should interpret research results and prescribe therapy. Attempts at self-medication can cause the progression of inflammatory changes and the development of complications.
Treatment approaches
Treatment of reactive changes is complex. It is based on the use of medications and a therapeutic diet. Among the medications prescribed are the following medications:
- painkillers and antispasmodics: “Baralgin”, “Drotaverin”, etc.;
- antiemetic medications: Metoclopramide, Ondansetron and their analogues;
- drugs that suppress the release of pancreatic enzymes: Pirenzepine, etc.;
- replacement therapy with enzyme agents: “Creon”, “Mezim”, etc.
To reduce intoxication phenomena, intravenous administration of glucose-saline solutions is carried out. It is important to note that all medications have contraindications for use. They are prescribed only by a doctor after examining the child.
Therapeutic diet
In the first 2-3 days of acute pancreatitis, the child is indicated for therapeutic fasting. It allows you to reduce the amount of pancreatic enzymes secreted by the gland and prevent the progression of pathology. A few days after the start of treatment, the diet is expanded: broths with lean meat, low-fat cottage cheese, steamed vegetables and fruits are added.
The diet implies the exclusion of any fatty, spicy, smoked and fried foods. It is also not recommended to eat fast food and snacks (chips, crackers, etc.). Children should limit their consumption of carbonated drinks.
Treatment of reactive changes in the pancreas
Changes in the tissues of the pancreas of a reactive nature require complex therapy. In severe cases, the patient is placed in a hospital, where he is under constant medical supervision. During the treatment period, strict bed rest and a special diet are observed.
Medications
Most often, the following drugs are used for reactive pancreatic diseases:
- painkillers (for mild cases of the disease - non-steroidal anti-inflammatory drugs, for severe cases - narcotic analgesics);
- antispasmodics (No-shpa, Platyfillin);
- medications that eliminate flatulence (Espumizan);
- enzyme preparations (Pancreatin, Mezim).
Read more about enzyme preparations for the pancreas in the article.
Traditional methods
Reactive changes in the pancreas are treated using the following natural remedies:
- Viburnum drink. 1 tbsp. l. berries pour 300 ml of boiling water, leave for 2 hours, mix with 1 tsp. honey Take 3 times a day for a month.
- Rosehip oil. The drug is taken in 15 ml doses for a week. After 2 months, the course of treatment is repeated.
- Dogwood juice. 0.5 tbsp. juice is diluted with warm water and drunk before each meal.
- Tincture of iris and wormwood. Herbs are taken in equal parts, 1 tbsp. l. collection, pour 200 ml of boiling water, leave for 3 hours, take 3 times a day, 4 tbsp. l.
- Potato juice. This remedy is taken 100 ml 2 times a day on an empty stomach. Over time, the dose is increased to 200 ml. A few minutes after drinking the juice, drink a glass of kefir. The course of treatment is 14 days, after a 2-week break it is repeated.
- Blueberry decoction. 1 tbsp. l. berries are boiled in 200 ml of water for 10 minutes, drunk 3 times a day.
- Immortelle tincture. For cooking you will need 2 tbsp. l. flowers and 0.5 liters of boiling water. The drug is boiled for 30 minutes, left to cool completely, and taken in 100 ml doses. half an hour before meals.
Diet
If you have diseases of the pancreas, you need to eat in small portions, 5-6 times a day. In the first days of an exacerbation, it is recommended to completely stop eating. After a few days, crackers, biscuits, unsweetened tea and oatmeal are introduced into the diet. Permitted for use:
- dairy products;
- jelly;
- stale bread;
- vegetable soups;
- boiled meat;
- fresh vegetables and fruits.
Proper nutrition for reactive changes in the pancreas means avoiding the following foods:
- chocolate;
- smoked meats;
- sausages;
- strong meat broths;
- food containing preservatives, flavorings and dyes;
- sour fruits.
Prevention
You can prevent the development of the disease in children by following simple recommendations:
- it is necessary to organize proper and rational nutrition, excluding foods with high fat content and large amounts of simple carbohydrates;
- the child should lead an active lifestyle: walk in the fresh air and play sports;
- It is important to promptly treat diseases of the digestive tract and other body systems.
When the first symptoms of reactive pancreatitis appear, parents should seek medical help. This will allow you to quickly make an accurate diagnosis and select therapy.
Diagnostics
Reactive pancreatitis can be diagnosed as follows:
- the doctor examines and listens to complaints;
- blood tests are taken, which will show the consequence of the inflammatory process;
- a biochemical blood test is performed, which will reveal an increase in the amount of enzymes;
- feces are submitted for analysis to determine the amount of increased fat and protein fiber;
- take an x-ray of the gastrointestinal tract;
- An ultrasound scan of the peritoneal cavity and digestive system organs is performed.
Return to contents
Куколки - путаны Бийска с yesbijsk.ru встречаются с достойными и интересными мужчинам. Вам требуется только ознакомиться с перечнем анкет и довериться своему вкусу, оценив привлекательность проститутки для себя по фотографиям. Красивые путаны Бийска, сладкие и ухоженные, они такие модельные и раскрепощённые, что тебе обязательно захочется секса. Не упусти свой шанс.