Pancreatic steatosis is fatty tissue degeneration (degeneration). Degenerated cells are not able to cope with their duties - secrete hormones and digestive juices. This condition is the result of an unhealthy lifestyle, in particular smoking and alcohol abuse. You can get rid of the disease only by giving up bad habits. If the pathology has just begun to develop, there is a chance to stop it, preventing dysfunction of such an important organ.
What is pancreatic steatosis
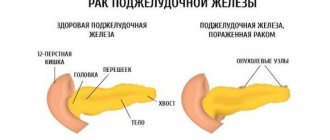
A pathological condition in which pancreatic cells are replaced by fatty tissue is called steatosis, or lipomatosis (obesity, fat deposition). Normal gland cells produce digestive enzymes and hormones. They are necessary for healthy human existence. Fat (lipid) cells have no purpose other than protective. After the healthy gland tissue dies, they do not allow the organ to lose its original volume. The replacement of functioning cells with fat cells leads to disruptions in the functioning of the pancreas and other body systems (liver, heart, nerves, gastrointestinal tract).
Pancreatic lipomatosis occurs:
- Focal - different sized islands of adipose tissue are observed on the surface of the gland.
- Diffuse - adipose tissue is evenly distributed over a certain part of the organ. In severe cases, it can occupy most of it.
Sometimes patients diagnosed with obesity of the gland use the expression “pancreatic hepatosis,” which is completely incorrect. The term “hepatosis” in medicine is used when talking about liver cell degeneration. The correct term is pancreatic steatosis or lipomatosis.
Causes, symptoms and treatment of steatosis in the pancreas
There is no single mechanism for the development of the disease for all cases. On the contrary, the etiology may vary greatly between patients. The causes of the disease can be divided into the following groups:
- Exposure to toxins.
- Features of metabolism.
- Consequences of unsuccessful surgical operations. The most dangerous in this regard are operations on the small intestine (removal of certain areas) and on the stomach).
- Diseases of the digestive system. Steatosis can be caused by chronic cholecystitis, cholelithiasis, fatty hepatosis, pancreatitis, after which the affected tissue can be replaced by adipose tissue.
The most common poison that has a detrimental effect on the organ is ethyl alcohol. Drinking alcohol, even in small quantities, can trigger the process of degeneration of the gland. Intoxication with potent medications, especially antibiotics, cytostatics and corticosteroid hormonal drugs, is less common.
Nicotine also negatively affects the activity of the gland. Smoking pipes, hookahs or cigarettes can cause the development of steatosis over several years.
The main factor influencing the development of steatosis is obesity and overweight. The root cause here is poor nutrition, namely an abundance of carbohydrates, fatty and fried foods, which leads to the fact that the pancreas and liver are simply unable to perform their functions.
There is a high risk of developing steatosis in patients with type II diabetes mellitus. This common disease is associated with a lack of insulin, which is produced by the islet apparatus of the pancreas.
In addition to an excess of high-calorie food, its deficiency can also lead to illness. Fasting or rapid weight loss (1.5-2 kg per week) lead to illness with the same probability as being overweight. Parenteral nutrition (intravenously, bypassing the gastrointestinal tract), practiced after certain types of operations, leads to a weakening of the functions of all organs of the digestive system, incl. and pancreas.
Pancreatic steatosis is a pathological condition in which normal pancreatic (pancreatic) cells are replaced by lipocytes (fat cells). Pathology is not an independent disease; it is a reflection of disrupted processes in the tissues of the gland. Occurs due to changes in the metabolism of lipids and glucose in the body.
The pathology develops slowly, and at the initial stages there are no clinical manifestations. This complicates diagnosis in the early stages and in this sense represents a danger: if changes are not detected, the process will progress and the organ will die. If most of the tissue is represented by fat cells, its shape will be preserved, but its function will not be restored.
Steatosis (lipomatosis) is the atrophy of an organ’s own cells and their replacement with adipose tissue. The process is irreversible, lasts for years, the organ gradually loses its functions due to the death of normally functioning cells.
If diffuse changes such as steatosis are detected on ultrasound, it is necessary, after consultation with a gastroenterologist, to immediately begin the prescribed treatment measures to prevent further tissue damage.
Untimely treatment can threaten the development of pronounced fibro-fatty deposits and complete loss of activity of the altered organs.
With pancreatic obesity, liver steatosis often occurs, or these processes develop sequentially. The condition requires treatment as it can cause serious consequences.
Alcoholic steatosis is more common in men, and non-alcoholic fatty liver disease (NAFLD) is more common in women. Since all digestive organs are interconnected by common functions, this pathology in the pancreas and liver occurs mainly simultaneously.
In the International Classification of Diseases ICD - 10 is coded:
- fatty hepatosis - k.70 - k.77;
- steatosis (lipomatosis) – k.86.
The exact causes of steatosis have not been identified by medicine, but a connection has been proven between existing fatty formations in the dermis (lipomas) and nearby organs. They often appear in the gallbladder area. There is a relationship between the development of lipomas and steatosis in the pancreas and liver.
Steatosis can be considered as a protective reaction of the body to unfavorable external and internal influences, when the body’s defenses run out and it stops fighting pathological processes in the pancreas, reacting to them with steatosis.
One of the main factors in the appearance of fatty infiltration of the pancreas is:
- eating disorders;
- bad habits (smoking, drinking alcohol).
Alcohol does not have the same effect on everyone: it has been proven that the development of steatohepatosis or steatonecrosis of the pancreas does not depend on the dose of alcohol. It is detected in people who regularly take large doses of alcohol-containing drinks, but for some, a few sips are enough to trigger the pathological process of degeneration of pancreatic tissue.
Junk food is also a powerful risk factor: not only regular consumption of large amounts of fatty foods and subsequent obesity cause the development of lipomatosis of the pancreas and liver. The trigger can be fried, smoked, too salty foods, hot seasonings.
Some diseases can lead to steatosis:
- pancreatitis;
- diabetes;
- cholecystitis;
- Housing and communal services
Inflammation in any digestive organ and primarily in the pancreas causes dystrophic changes in cells and their death. In their place, adipose tissue grows.
Some groups of drugs have a destructive effect. Sometimes one tablet can cause irreversible changes. Most often, steatosis is caused by antibacterial drugs, glucocorticosteroids (GCS), cytostatics, painkillers, although, in addition to them, there are many other groups of medications that trigger pancreatic necrosis.
Pancreatic tissue can degenerate as a result of surgical interventions: even in cases where the operation is not performed on the pancreas itself, but on nearby organs, this can cause transformation of the pancreatic tissue.
There is a possibility of inheritance of pancreatic lipomatosis. But the percentage of patients with a genetic factor for the transmission of steatosis is very low. It is more likely to say that the development of pathology depends on the person: his lifestyle, habits, nutrition, activity.
Symptoms of pathology
The danger of steatosis lies in the absence of early signs of its manifestation in the initial stages of the pathology. Over a long period of time (several months or years), no complaints or clinical symptoms may occur.
Minor discomfort appears when the pancreas parenchyma is already 25-30% fat cells. And even at this stage, the remaining healthy cells compensate for the missing part of the organ, and the functions of the pancreas are not impaired. This is the first degree of pathology.
As the degeneration of organ cells progresses, the condition may worsen. The second degree of parenchymal damage corresponds to the level of diffusion of adipose tissue in the pancreas from 30 to 60%. As the level of altered cells approaches 60%, functions are partially disrupted.
The first pathological manifestations are:
- diarrhea;
- abdominal pain - of varying localization and intensity;
- flatulence, belching air;
- nausea;
- allergies to previously normally perceived foods;
- unmotivated weakness, fatigue;
- reduced immunity, which is manifested by frequent colds;
- lack of appetite.
Not only exocrine functions with digestive disorders suffer, but also endocrine functions: the synthesis of insulin by the beta cells of the islets of Langerhans, the hormone responsible for carbohydrate metabolism, is sharply reduced. At the same time, the formation of other hormonal substances is disrupted, including somatostatin and glucagon (the pancreas produces 11 of them).
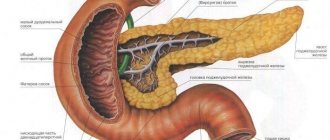
The development of steatosis is determined by the anatomical structure and functional significance of the pancreas. This is the main organ of the digestive system; it produces enzymes that, as part of the digestive juice, are involved in the digestion of fats, proteins, and carbohydrates. This occurs in special areas of the glandular tissue of the pancreas - acini. Each of them consists of:
- from cells that synthesize pancreatic juice;
- from vessels;
- from the duct through which the secretion is discharged into larger ducts, and then into the common duct (Wirsung).
The duct of Wirsung passes through the entire gland and connects with the duct of the gallbladder, forming an ampulla that opens into the lumen of the small intestine thanks to the sphincter of Oddi.
Thus, the pancreas is connected with the gallbladder, liver, small intestine, and indirectly with the stomach. Any disturbance in the gland leads to a change in metabolism in adjacent organs and causes:
- fatty hepatosis in the liver tissue;
- damage to the gallbladder, in which inflammation develops (chronic cholecystitis), and due to stagnation of bile, stones are formed (GSD);
- thickening of the walls and narrowing of the lumen of the common duct leads to increased pressure of pancreatic secretion, reverse release of enzymes and acute necrosis of the pancreas;
- the death of the islets of Langerhans due to developing necrosis leads to a sharp decrease in insulin, increased glycemia and the development of type 1 diabetes mellitus.
Pathological anatomy of the pancreas in diabetes mellitus describes alternating atrophy and hyalinosis of the islets with their compensatory hypertrophy.
At stages 2 and 3 of steatosis, a significant proliferation of fat cells occurs and disrupts the function of the pancreas.
But even with moderate damage to individual areas of the gland, the full clinical picture of pancreatitis can appear due to the development of autolysis (self-digestion) followed by necrosis and the formation of areas of compaction - fibrosis, combined with lipomatosis.
Tissue involution in the form of atrophic changes with progressive fibrolipomatosis is irreversible, most often it occurs in chronic pancreatitis. With this pathology occurs:
- proliferation of connective tissue infiltrates, which can compress ducts, vessels, and remaining functioning tissue;
- organ compaction due to diffuse damage.
Why does fatty degeneration of cells appear?
Pancreatic disease can be of alcoholic or non-alcoholic origin. Lipomatosis is provoked by frequent consumption of strong alcohol. It can also occur when:
- pancreatitis;
- diabetes mellitus;
- obesity;
- cholelithiasis;
- cholecystitis (inflammation of the walls of the gall bladder).
The common cause of these pathologies is metabolic disorders. Most often, this condition is observed in people who have been taking medications (hormonal, antibacterial, painkillers) for a long time or who eat fatty foods daily.
Alcohol does not have the same effect on everyone: it has been proven that the development of steatohepatosis or steatonecrosis of the pancreas does not depend on the dose of alcohol. It is detected in people who regularly take large doses of alcohol-containing drinks, but for some, a few sips are enough to trigger the pathological process of degeneration of pancreatic tissue.
Surgery on it or a neighboring organ can lead to degeneration of functioning pancreatic cells.
Development mechanism
Pancreatic steatosis develops under the influence of pathological factors that can work in combination and have a cumulative effect. Taking medications or alcohol is only one of the possible causes of pancreatic steatosis. The etiology associated with alcohol abuse and reasons not related to alcoholism are standardly distinguished. The most common in the latter case are diseases of the hepatobiliary system (gallbladder: cholecystitis or cholelithiasis) and the pancreas itself (pancreatitis).
The lack of enzymes necessary for digesting food, normally produced by the pancreas, leads to irreversible changes in the digestive system and the activity of other internal organs. Diabetes mellitus, obesity, and even surgery performed in close proximity to the pancreas can also provoke pathology:
- Primary pancreatic steatosis develops against the background of provoking factors inherent in intrauterine development (its mechanism is triggered at the gene level and is inherited). However, a time bomb can end up in a child’s body due to negative factors that influenced it in the womb. This explains the rapid necrotization of the gland in some patients with short-term alcohol consumption, and the persistent absence of the disease in heavy and long-term drinkers.
- Secondary is a natural consequence of diseases of the endocrine or metabolic system, the course of individual diseases or complications resulting from them.
Pancreatic steatosis is a complex process of changes occurring in the gland. Necrotization of the functional cells of the pancreas forms affected areas, which the natural defense mechanism tries to patch up with the help of fat cells. The volume of such replacements depends on the scale and nature of necrosis. Single cases provoke focal pancreatic steatosis; with constant and prolonged exposure to negative factors, diffuse steatosis develops, when the entire gland is covered with fatty abnormalities and has practically lost the ability to function.
Symptoms of fatty infiltration of the pancreas
Lipomatosis, or fatty degeneration, of the pancreas develops slowly. Its initial stage occurs without pronounced symptoms. Gradually, the scale of damage to pancreatic tissue increases. This is indicated by frequent problems with the gastrointestinal tract. They are manifested by abnormal stool and pain in the abdomen without a specific localization, radiating to the lumbar region.
If left untreated, clinical symptoms worsen. The patient feels sick for no reason, experiences heartburn, unpleasant belching, and bloating. A person gets tired quickly, gets irritated over trifles, and cannot sleep peacefully at night.
Symptoms
The most unpleasant fact for the patient and his attending physician remains the fact that the first clinical manifestations of the disease occur only when more than 30% of normal cells are replaced by fat. In some people, the disease is asymptomatic and with half of the active structures missing. Therefore, the diagnosis is often made too late, and the patient has to undergo full-fledged treatment instead of an elementary diet, which would help in the early stages. However, pancreatic steatosis is characterized by the following symptoms:
- fatty, frequent (diarrhea) stools,
- flatulence (bloating),
- dull aching pain in the left and right hypochondrium,
- loss of appetite,
- nausea,
- vomit,
- general weakness and mood swings,
- itching and rash on the skin.
All these signs indicate insufficient excretory function of the pancreas due to its replacement with adipose tissue. When the liver is involved in the pathological process, the following manifestations may additionally be present:
- bitter taste in mouth
- swelling in the legs,
- the appearance of characteristic spots on the skin,
- increase in organ size,
- pain in the right hypochondrium.
Association with obesity and fatty liver disease
Obesity occurs against the background of dysfunction of the endocrine part of the gland. Its cells produce hormones:
- insulin - participates in carbohydrate metabolism and controls blood glucose levels;
- lipocaine - is responsible for the formation of phospholipids in the liver.
Phospholipids support the structure of organ cells and ensure the restoration of its tissues. A lack of the hormone lipocaine leads to fatty degeneration of the liver with subsequent weight gain.
Also, a diagnosis of steatosis of the liver and pancreas is made if the exocrine part of the pancreas (produces digestive enzymes) does not function at full capacity. Normal liver cells are replaced by adipose tissue, but this phenomenon can be reversible if the cause of hepatosis is promptly eliminated and the necessary treatment is started.
Features of the manifestation of steatosis
The pancreas performs the most important work in the human body:
- Synthesizes and secretes enzymes such as amylase, chymotrypsin, trypsin, lipase, and other biologically active substances that are responsible for the digestion and consumption of carbohydrates, fats and proteins by the body.
- Produces glucagon and insulin, which control carbohydrate and lipid metabolism, as well as glucose levels in the blood fluid.
Steatosis of the pancreas (lipomatosis), or as it is also called pancreatic steatosis, is a pathology that damages the parenchyma of this organ and replaces healthy working cells with adipose tissue (lipids). To some extent, this disease in its development has some similarities with cirrhosis of the liver, in which hepatocytes are displaced by connective tissue and lose their original configuration.
The disease is characterized by three degrees, depending on the size of the pancreas area affected by the pathology:
- The first is 0-30%.
- The second is 31-60%.
- Third – 61-100%.
Lipomatosis can be:
- Small droplets (moderate).
- Large-droplet (pronounced).
Moderate steatosis of the pancreas is the initial stage of the disease, when the hepatocytes of the organ are not yet affected, but the pathological processes have already started.
Severe steatosis of the pancreas - when there is significant damage to the organ and the presence of a necrotic process, that is, cell necrosis is already observed.
Lipomatosis can be of two types:
- Alcoholic, as a result of abuse of alcohol-containing drinks.
- Non-alcoholic, which is formed against the background of diabetes and obesity.
Steatosis is classified according to the reasons for its development:
- Primary (congenital).
- Secondary (is a complication of other pathologies).
Medicine believes that lipomatosis is an eternal disease for which there is currently no effective treatment.
Possible consequences
Pancreatic lipomatosis can either manifest itself against the background of pancreatitis or cause inflammation. If left untreated, the disease leads to liver failure. The liver increases in volume, the patient constantly feels heaviness in the right side.
If liver tissue is capable of recovery, then changes in pancreatic cells are irreversible. Pathology affects the functioning of all internal organs and systems of the body. If fat cells damage the part of the organ that produces insulin, type 1 or type 2 diabetes may develop.
Treatment of steatosis
The pancreas is important for the body. It is entrusted with a large number of different functions, therefore, if there are deviations in the purpose of the gland, it will cause serious illnesses.
When patients are faced with the occurrence of steatosis, the question is often asked, is it possible to cure steatosis? Fatty infiltration cannot be eliminated; it is only possible to stop its formation and support the functioning of the pancreas with timely initiation of therapy.
It is unwise to carry out treatment on your own; it often provokes irreparable consequences. Find out what treatment for pancreatic steanosis is necessary from your doctor. The doctor will order a full examination.
Steatosis is diagnosed using a number of popular methods.
- Blood test, the analysis notes the level of alpha-amylase in the serum.
- Tumors and malignant and benign courses can be identified using MRI.
- The echogenic areas are determined by the ultrasound procedure.
- X-rays are taken to check the patency of the pancreatic ducts.
- The procedure is laparoscopy, biopsy.
blood analysis
Based on the results of the study, the degree of the disease will be determined in relation to the volume of the affected areas of the organ, and treatment will be prescribed.
Treatment methods for pancreatic steatosis include conservative or surgical solutions to the problem. The main principle of treatment is to get rid of the factors that cause fat imbalance in the pancreas. In an individual situation, the doctor develops a treatment strategy that takes into account a number of factors.
- Location of fat formations.
- The degree of their formation.
- General health of the patient.
- Age.
If the liver and pancreas are slightly damaged and are able to function normally, the treatment process can be managed with the use of medications, abstinence from alcohol, smoking, and a diet.
Drug therapy is carried out using the following means:
- enzymes - aimed at maintaining organ function, helping to normalize the digestive process;
- antisecretory drugs - necessary to block the formation of hydrochloric acid in the stomach;
- fat blockers – prevent fat from being absorbed and absorbed in the stomach and intestines;
- painkillers;
- antibacterial medications;
- anti-vomiting and diarrhea medications;
- vitamin complexes.
If the gland is severely affected by fatty lesions that prevent the organ from functioning normally, surgical treatment is prescribed.
The operation is performed using 2 methods; they differ in access methods. This is a laparoscopic and laparotomic procedure. Compared to conventional abdominal procedures, the process using an endoscope is much simpler, and recovery is quick and painless.
operation
Treatment of steatosis with folk remedies
Pancreatic steatosis is cured with the help of various herbs.
- Dandelion.
- Chicory.
- Plantain.
- Blooming Sally.
- Spiraea.
These herbs are recommended to be used in combination with rice broth. This will improve the action and give more noticeable results.
It is possible to use insulin-like plants. They are useful in gland therapy.
- Bean pods.
- Burdock.
- Elecampane.
- Blueberry leaves.
- Dandelion.
- Nettle.
- Corn silk.
nettle
Thanks to these herbs, it will be possible to reduce glucose levels in the circulatory system and improve liver and gland function.
For illness, a herbal mixture of sweet grass, corn silk, oat straw, fennel, burdock, anise, wormwood and plantain is used. These plants need to be finely chopped and poured with boiling water. For half a liter of water, add a large spoonful of the mixture. The drink is infused for 1 hour, filtered. Take the medicine 3 times a day for 14 days. Drink the infusion 30 minutes before meals.
A useful medicine is a decoction of blueberry leaves. It is necessary to chop fresh leaves 1 tablespoon, or take dry leaves in the amount of 1.5 large spoons. Pour boiling water over the product - 250 ml, boil for 10 minutes. Cool the medicine and express it. Treat with the drug 2 times a day, drinking 100 ml.
Diagnostic methods
Fatty infiltration of the pancreas is determined using the following studies:
- Biochemical and clinical blood tests, urine analysis - to assess the condition of the exocrine and endocrine parts of the organ.
- Coprogram (stool analysis) - allows you to clarify the presence of pancreatitis.
- Magnetic resonance imaging - prescribed if ultrasound results do not help make a diagnosis. The method helps to see and distinguish diffuse changes in the pancreas by type of steatosis.
- A puncture biopsy is performed to get an idea of the nature of the lesions affecting the gland.
Despite the hidden course of steatosis, pathological changes in the organ can be seen using ultrasound. This diagnostic method is not prescribed at an early stage of the disease due to the absence of symptoms.
Fat cells tend to grow and affect other organs. Therefore, it is very important to detect the disease at an early stage and begin treatment or prevent the disease.
In order not to miss the onset of fatty pancreas and liver (fatty hepatosis), doctors recommend that people with excess weight, digestive problems and diabetes undergo an ultrasound scan several times a year.
Methods for diagnosing pathology
The completeness of loss of function is determined by diagnostic studies, which consist of laboratory and instrumental methods. All necessary diagnostic methods are used to identify the degree of damage to organ tissues and to decide on further treatment tactics.
Modern medicine has not yet developed methods for restoring lost cells and functions. Dead cells are not restored. But it is possible to prescribe the correct replacement therapy to correct and improve the condition.
Laboratory diagnostics
Laboratory tests are an important part of diagnosis. To determine impaired functions of the pancreas and liver, analyze:
- blood and urine amylase;
- blood glucose;
- bilirubin - total, direct, indirect, transaminases, total protein and its fractions.
Additionally, you need to examine the stool - make a coprogram, which will reveal pancreatitis.
Instrumental diagnostics
To clarify pathological processes in the pancreas, the following is used:
- Ultrasound of the pancreas and other digestive organs;
- CT - computed tomography;
- MRI - magnetic resonance imaging.
Ultrasound is the simplest and most accessible method. It is safe and detects any changes in the parenchyma of organs.
With steatosis, the size of the pancreas remains the same, the clarity of the boundaries does not change, the echogenicity of certain structures increases, which confirms the developed pathology in the parenchyma of the organ.
Fibrolipomatosis is characterized by a high density of the organ structure due to the formation of scar connective tissue.
In the early stages of development, when there are no complaints and no clinical symptoms, as a rule, no one does an ultrasound. Fatty changes in the pancreas at the initial stages are detected as a finding during examination for another reason. The result is confirmed by a biopsy, after which treatment is prescribed - this makes it possible to prevent further progression.
An acute inflammatory process in tissues leads to necrosis, which is accompanied by edema, increased size and decreased density on ultrasound.
MRI is prescribed in unclear cases when ultrasound did not help in establishing an accurate diagnosis and doubts remain. The method accurately and in detail describes the structure and existing formations at any stage of change. In case of steatosis, MRI identifies the organ:
- with clear contours;
- with reduced density;
- with reduced dimensions;
- with an altered tissue structure (diffuse, nodular, diffuse-nodular changes are determined).
A puncture biopsy is performed when the liver is involved in the process.
Treatment of fatty infiltration
The doctor will be able to answer the question of how to treat steatosis only after making a diagnosis. Therapy for fatty infiltration of the pancreas is often carried out with medications. Traditional methods of treatment can be used as a supplement. Surgery is indicated only when lipomatosis of the gland can cause death.
Pharmacy medicines
Treatment of pancreatic steatosis is carried out with the following drugs:
- Festal, Panzinorm, Mezim Forte are enzyme agents that are prescribed if steatosis has disrupted the functions of the exocrine part of the gland.
- Cerucal, Motilium, Ganaton - medications relieve gag reflexes. For severe vomiting, they are used by injection.
- Papaverine, No-Shpa, Mebeverine - relieve spasm of smooth muscles, promote the penetration of enzyme drugs into the duodenum.
- Analgin, Ibuprofen, Baralgin - eliminate pain, dull the sensitivity of receptors that signal the brain about pain.
- Loperamide, Imodium, Diaremix - medications help with chronic and acute diarrhea.
- Humulin, Siofor, Formetin - hypoglycemic agents in injections or tablets. Prescribed if the disease is accompanied by a disorder of carbohydrate metabolism.
Traditional methods
Fatty infiltration of the liver or pancreas can be stopped using traditional methods, but in combination with dietary nutrition.
Effective medicinal infusions:
- Blackberry root. Pour 1 tbsp into a thermos. l. crushed dry raw materials, pour 250 ml of boiling water, after 3 hours the medicine is ready. Take the infusion 0.5 cups 3-4 times a day before meals. The product improves metabolic processes.
- Calendula, sage. Pour 1 tbsp into a thermos. l. herbs, pour 500 ml of boiling water, filter after 30 minutes. Drink instead of tea 3-4 times a day. The drink relieves inflammation and improves the functioning of the digestive system.
- Pharmaceutical chamomile. Pour 1 tbsp into a thermos. l. raw materials, pour a glass of boiling water. Take ⅓ glass 3 times a day 20 minutes before meals. Used for the treatment and prevention of glandular lipomatosis.
To improve the condition of the pancreas and liver, it is recommended to take infusions for lipomatosis continuously for at least a month.
Diet
Treatment of liver and pancreatic steatosis will not be effective if harmful foods remain on the menu. Smoking, pickling, spicy, fried, and sweet foods should be excluded from the diet. Strong coffee, chocolate, and alcohol are prohibited.
For steatosis, nutritionists recommend focusing on dietary table No. 5. It is based on proteins and carbohydrates:
- Soups - prepared from pureed vegetables and cereals in water or vegetable broth. No frying is done; a little butter is added to the soup.
- Porridges made from rice, buckwheat, oatmeal, semolina. Prepared with water or with the addition of a small amount of milk.
- Durum wheat pasta.
- Dishes made from dietary meat (veal, rabbit, turkey) and low-fat fish (hake, pike perch, pike) - steamed, baked in the oven, boiled. It is recommended to use it in crushed form.
- Fermented milk and dairy products with fat content not exceeding 25% up to 200 g per day. Sour cream is used only as a dressing.
- Bread - only stale bread, wheat or rye crackers.
- Drinks - rosehip decoction, weak black tea, fruit and vegetable juices, still water are recommended.
Compliance with diet No. 5 or 5p involves eating food only when it is warm. Meals should be fractional - 5-6 meals a day, but in small portions.
Other therapies
Treatment of fatty liver (hepatosis) and pancreatic steatosis through surgery is used if:
- Fat cells tighten surrounding tissues.
- Lipomatous lesions put pressure on the excretory ducts of organs.
- Steatosis is accompanied by the appearance of malignant or benign neoplasms.
Diagnostics
If pancreatic steatosis is suspected, a number of studies must be performed. Diagnosis begins with a general examination ; the doctor is obliged to listen to all complaints, find out the history of life and illness. With percussion and palpation the pain intensifies.
In a blood test, during active inflammation, an increase in the concentration of acute-phase proteins and liver enzymes (AST, ALT) is determined if destructive processes also occur in the liver. Leukocytosis with a shift of the leukocyte formula to the left is observed. A specific analysis of the functional activity of the pancreas is the determination of the amount of pancreatic enzymes, in particular amylase. In the initial stages, the indicator increases several times, after which it gradually decreases.
, ultrasound, computed tomography and magnetic resonance imaging are quite informative , as they allow one to fully study the area and depth of structural changes.
In order to speak with absolute certainty about the presence of steatosis in a patient, a biopsy - taking biomaterial during a person’s lifetime and its detailed morphological description.
What are the prognosis for the sick person?
The prognosis for recovery from lipomatosis depends on:
- stages of steatosis;
- the scale of the affected gland tissue;
- origin of the disease;
- timeliness of prescribed treatment;
- the presence of concomitant diseases;
- the patient's compliance with all doctor's instructions.
Early stages of pancreatic obesity can be successfully treated. As soon as a person changes his lifestyle, the functioning of the organ improves. If liver failure is added to an advanced form of lipomatosis, the risk of death increases.
Consequences and prognosis
The consequences of steatosis for the body are very serious; in advanced cases, gland dysfunction occurs and the prognosis in such cases is unfavorable , including death. Even after surgery, the situation may not change dramatically if the patient does not adhere to a diet or take medications that are already necessary for life.
If we consider the life expectancy with pancreatic steatosis, then each case is individual. If the patient consults a specialist already at stage 3 of the disease, then there is a high risk of complications leading to a significant decrease in life expectancy; sometimes the person cannot be saved even with all possible treatment measures. With positive dynamics, when the formation of fat cells is suspended or occurs extremely slowly, the patient’s age is up to 50-60 years, initially the organ is damaged no more than 35%, that is, the chances of leading a normal lifestyle, but subject to a certain diet and the exclusion of alcohol.
If you are overweight or have digestive problems, it is recommended to undergo periodic examinations, including tests and ultrasound. This will help in the early stages to detect the development of possible diseases not only of the pancreas, but also of other abdominal organs. Taking timely measures reduces the risk of consequences that are irreversible for the body.