Removal of the pancreas
The pancreas produces insulin and digestive enzymes. Without insulin, diabetes occurs, and without enzymes, food is partially absorbed. Is the pancreas completely removed?
If a patient is diagnosed with a malignant neoplasm of the gland, then part of it or the entire organ is removed. At this moment, there is no question of how a person will live after resection of this organ; the doctors have a goal - to save the patient’s life.
Let's consider in what cases pancreatic surgery is performed and further prognosis:
- In case of cysts, they are removed along with part of the organ.
- In case of organ injury, the omental bursa is opened and blood is removed from the damaged tissue. Then the bleeding vessels are bandaged and the tissues are stitched. A drain is placed to drain the blood. If the gland or its main ducts are completely ruptured, an anastomosis is performed between the pancreas and the small intestine.
- If there are stones in the ducts, then the gland is dissected, the stones are removed, the duct is drained and a suture is applied.
- Diseases of this organ.
- With an abscess.
- For tumors.
- For fistulas.
- With pancreatic necrosis.
- For bleeding from the vessels of the organ.
- With peritonitis.
If a small rupture of the gland occurs, then the following is carried out:
- removal of the resulting hematoma;
- stitch the gap;
- drainage is being installed.
If the left half of the gland is damaged and the ducts are disrupted, resection of the body and tail of the gland is performed. If the head of the pancreas is damaged and the main pancreatic duct is ruptured, then pancreaticoduodenal excision is performed. With this operation, the mortality rate reaches 80%.
A common reason for pancreas removal is cancer. It can occur for a number of reasons:
- diabetes;
- spicy and fatty foods;
- alcohol abuse;
- surgical interventions on the stomach;
- binge eating;
- unbalanced diet;
- smoking;
- pancreatitis;
- pancreatic necrosis;
- hereditary pathology.
At a certain stage of development of a malignant tumor, there is only one way to prolong life - surgery.
Surgeries on the pancreas are divided into several types:
- The surgeon restores the outflow of bile using endoscopy - biliodigestive anastomosis.
- During surgery, the stomach is attached to the small intestine - gastroenterostomy.
- Complete removal of the pancreas - pancreaticoduodenectomy -.
- Total pancreaticduodenectomy.
Complete removal of the pancreas is rarely done. Resection of the pancreas is classified as a complex operation, since access to the gland is hidden behind other abdominal organs - the stomach, small intestine, and liver.
Resection and progress of the operation
If an organ is completely removed, the procedure is as follows:
- First, the organ is examined using a laparoscope.
- Then the operation begins.
- An incision is made on the anterior wall of the abdominal cavity.
- Then a section of the pancreas or the entire organ is removed.
- The surgery lasts approximately 5 hours.
As soon as the patient opens his eyes, the question immediately arises: can they live without a pancreas and for how long. Life expectancy depends on how well a person was able to adapt to a decrease in quality of life. The help of a psychologist plays an important role during the rehabilitation period.
Postoperative period
After removal of the pancreas, the patient is sent to a separate ward. There he will be observed by a doctor during the rehabilitation period. On average, this time lasts 5-20 days. If unforeseen circumstances suddenly arise, this period is extended at the discretion of the attending physician.
Some patients experience pain after the anesthesia wears off. In this case, painkillers are prescribed.
When a person is discharged from the hospital, the doctor explains in advance what rules will have to be followed for some time. This includes the following recommendations:
- compliance with a certain dietary table;
- taking enzymes;
- insulin administration;
- Physical activity and heavy lifting are prohibited.
Important information: What to take for pancreatic pain
The help of loved ones is especially important for the patient, since for some time he will not be able to cope with all matters on his own.
How to live after surgery
The operation was completed. Life without a pancreas awaits you ahead. Can a person live without a pancreas? What awaits him? Life after removal of the pancreas becomes very difficult for the patient:
- There is a violation of carbohydrate metabolism.
- The body stops producing insulin, so you will have to take insulin injections for the rest of your life.
- The required digestive enzymes are also not produced.
After removal of the pancreas, there may be consequences. To avoid the appearance of new benign tumors, the patient is treated with chemotherapy and radiation therapy. After a patient has had their pancreas removed, the following complications may occur:
- the patient loses weight;
- an infectious complication may occur after surgery;
- Nerve damage is observed;
- bleeding;
- are diagnosed with diabetes;
- the digestive process is disrupted.
Early complications after surgery
Early complications can arise immediately at the time of surgery. These include:
- developed bleeding of varying intensity,
- intersection of nerve trunks,
- traumatization of closely adjacent organs and necrosis as a result of damage to them by active enzymes from the pancreas entering the abdominal cavity during surgery,
- a sharp drop in blood pressure as a reaction to anesthetic drugs,
- coma,
- infection.
The likelihood of developing complications is always higher in people:
- overweight
- alcohol abusers,
- with severe pathology of the cardiovascular system.
After the operation the following develop:
Diet
Can a person live without a pancreas if he does not adhere to a strict diet? Let us answer right away - no. After discharge home, the patient will be recommended the 5p diet. It is possible to live without a pancreas if, in addition to diet, the patient takes enzymes and injects insulin. The following products are strictly prohibited:
- Sausages and smoked products.
- Pickles.
- Spicy food.
- Fatty and sweet products.
- Strong tea and coffee.
- Fresh pastries and bread.
- Spices and seasonings.
- Fermented milk products.
- Flour products and potatoes.
- You can eat eggs, but very rarely.
Meals should be fractional, and food should be easily digestible. You can cook food by steaming, stewing, boiling or baking. After cooking, everything must be ground. It is advisable to stick to a protein diet.
Fresh vegetables and fruits can be eaten in unlimited quantities, without forgetting to chop them. Coarse plant fiber should be excluded. The patient should drink at least 2 liters per day.
Nutrition after surgery
After removal of the pancreas, special attention is paid to nutrition. On the third day you are allowed to drink sweetish weak tea and still mineral water. On days 4-6 add liquid vegetable soups and liquid porridges. Only towards the end of the first week do they begin to gradually add coarser food - bread, omelet, stewed vegetables. Two weeks after the operation, cottage cheese with a reduced percentage of fat content, lean types of meat and fish are allowed.
Dishes must be subjected to heat treatment. The diet does not contain fresh vegetables and fruits, baked goods, coffee, spicy and smoked foods, or canned products. Alcohol and smoking are unquestionably prohibited.
All portions are palm sized. You should eat frequently. Don’t forget about herbal medicine and vitamin-mineral complexes. These principles are followed for life.
To avoid serious complications and any type of surgery, you need to take care of yourself. It is better to prevent a disease than to treat it later.
Enzyme replacement therapy
After your pancreas is removed, the consequences are reflected in the digestive process as a whole. A lack of enzymes leads to the fact that food is no longer processed and absorbed through the intestines. Taking enzymes helps normalize digestion and should be taken with meals. Enzyme preparations are produced with different effects, here are some of them:
- Vestal – helps stimulate digestion.
- Alpha amylase - helps digest carbohydrates and is taken after meals.
- Mikrasim - it contains pancreatin, which helps proteins, fats and carbohydrates to be absorbed.
- Creon – has a complex replacement effect on the patient’s body in case of enzyme deficiency.
These medications should be taken with every meal. The effect of treatment is noticeable immediately - nausea goes away and intestinal function normalizes.
Is it possible to live without a pancreas?
After removal of the pancreas, the doctors' prognosis is not encouraging. Many people undergoing surgery die in the first year of life. The average lifespan of such patients is 5 years. Although some live to a ripe old age.
If the pancreas has been removed, the patient should buy a glucometer at the pharmacy to determine sugar levels and insulin pens for injection.
Sometimes, if a donor is available, an organ transplant is performed. But this surgical intervention requires high professionalism from the doctor.
After removal of the pancreas, the consequences and disappointment in life after surgery should not force operated people to withdraw into themselves. You should appreciate every day you live and try to perceive all life situations with a smile. Each person in life is given as much as he can endure - pain, tears, and love.
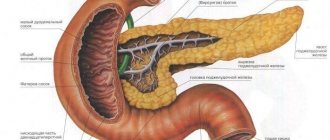
The pancreas is an important organ related to both the digestive and endocrine systems. In the area of its head, the glandular epithelium produces secretory fluid with enzymes for the breakdown of proteins, fats and carbohydrates. It is collected in a common duct, which opens into the lumen of the duodenum along with the bile duct, and mixes with food entering there from the stomach.
The tail part of the gland performs an endocrine function. It contains the islets of Langerhans, consisting of beta and alpha cells. Beta cells produce insulin, which is necessary for the metabolism of glucose in the body.
The pancreas performs a secretory function - produces digestive enzymes, and an endocrine function - produces the hormone insulin
The gland is very vulnerable and susceptible to diseases - inflammation and the development of tumors, when often the only possible treatment is surgery: removal of the entire pancreas or part of it.
Functions of the organ
The pancreas is one of the most important parts of the human body. It is presented in a single copy and is an indispensable component of the body. It is located slightly below the stomach, in the “horseshoe” of the duodenum. Performs the following essential functions:
- Secretion of digestive enzymes (lipase, trypsin, chymotrypsin, amylase, nuclease and others). The organ is the main “workshop” for the production of substances for digesting food. Without it, a person could not live, since proteins, fats and carbohydrates were simply not absorbed.
- Secretion of insulin and glucagon - hormones that respectively reduce and increase the amount of sugar in the blood. For this purpose, there are special endocrine B cells, which are grouped into islets of Langerhans. They ensure normal glucose levels in healthy people. If you cut out the gland, then type 1 diabetes will 100% form.
Indications for operations on the pancreas and their types
Due to the fragility and delicacy of the structure of the gland, surgical interventions on it are performed only as a last resort, when drug treatment is ineffective. Indications for surgery are:
- Severe forms of acute pancreatitis that are not amenable to conservative treatment.
- Hemorrhagic pancreatitis with hemorrhages into the body of the gland.
- Pancreatic necrosis is the necrosis of areas of the gland due to pancreatitis.
- Purulent inflammation, gland abscess.
- Large gland cysts.
- Pancreatic fistulas.
- Suppuration of the cyst.
- Traumatic injuries.
- Presence of stones in the gland ducts.
Complete removal of the gland is most often performed for cancerous tumors.
Important! Advanced chronic diseases (pancreatitis, cysts) lead to operations on the pancreas due to lack of treatment and non-compliance with diet.
The scope of operations may vary, depending on the nature of the disease:
- dissection of the capsule to reduce swelling;
- necrectomy - removal of individual dead areas;
- partial removal (resection of the pancreas - head, body, tail);
- complete removal - pancreatectomy.
Partial removal of the pancreas is performed in the presence of cysts, necrosis, hemorrhages, or a small tumor. Complete removal - for cancer, extensive pancreatic necrosis, purulent melting of the gland and severe damage when restoration is impossible.
In modern clinics, robotic gland removal operations are performed with increased accuracy and a minimum of errors.
Important! Is it possible to remove the pancreas if it is a much-needed organ? Yes, removal is possible to save the patient’s life, followed by permanent replacement therapy.
Indications for surgery and technique for performing it
Surgeries on the pancreas are performed for certain indications:
- abdominal injuries
- organ neoplasms (tumors, metastatic lesions)
- pancreatic necrosis (necrotic damage to organ tissue)
- presence of stones in the ducts
- exacerbation of chronic pancreatitis with the presence of irreversible changes in tissues
Removing part of the pancreas is the most gentle intervention, since the main functions of the organ are preserved. In case of injury or crushing of an organ, non-viable areas are excised, the bleeding is stopped, and the excision site is sutured with a continuous entwining suture.
Then the gland capsule is sutured. The final stage is peritonization - closing the peritoneal defect with an omentum. To prevent complications (in particular bleeding), tampons are left at the suturing site for several days.
For tumors, the technique is slightly different. After exposing the gland, part of the affected organ is excised, including healthy tissue, to prevent metastasis and spread of the formation. A histological examination of the removed material is necessary to establish an accurate diagnosis and exclude malignancy.
When removing the head, the Whipple technique is used. The operation is carried out in two stages - removal of the affected part and restoration of the digestive canal.
- The head of the pancreas, gallbladder, part of the bile duct and duodenum are resected. Sometimes the omentum, a small part of the stomach (about 10 percent) and nearby lymph nodes are cut out.
- restoration of patency between the body of the gland, stomach, bile duct and small intestine.
Consequences of operations
What are the consequences and life after surgery on the pancreas - complete or partial removal of it? There cannot but be consequences, because the body loses an organ or part of it, which is necessary for normal digestion and glucose metabolism. The larger the volume of the operation is performed, that is, the more gland tissue is removed, the more pronounced the disorders will be.
Consequences of pancreatic resection
When resection of the gland, its pathologically altered area is removed: the head, part of the body or tail, while surgeons always strive to preserve the glandular tissue as much as possible. If the head or part of the body of the gland has been removed, the digestive tract lacks enzymes.
When resection of the gland, its tail, part of the body or head may be removed
As a result, the absorption of nutrients is impaired, most of them are excreted undigested in the intestinal contents. The patient develops weight loss, general weakness, frequent bowel movements, and metabolic disorders. Therefore, mandatory correction of the digestive process is necessary through replacement therapy and adherence to a therapeutic diet. As replacement therapy, enzyme preparations are prescribed during meals: Pancreatin, Mezim-Forte, Creon, Wobenzym and their other analogues.
If a resection of the tail part of the gland, which produces insulin, was performed, then severe digestive disorders do not occur, but hyperglycemia develops, as in diabetes mellitus. Such patients should be constantly monitored by an endocrinologist, monitor blood sugar levels and constantly receive therapy with insulin or its analogues, as well as follow a diet.
Consequences after removal of the pancreas
Is the pancreas completely removed? Yes, they delete it. The operation of pancreatectomy is performed quite rarely, it is technically complex, fraught with consequences, but is performed in the name of saving the patient’s life.
Important! After surgery to remove the pancreas, the body is deprived of digestive enzymes and insulin, which, in principle, is a great threat to health and life. But practice shows that a full life without the pancreas is possible, and modern medicine allows this.
Creon is an optimal set of enzymes for gland replacement therapy after its removal
If you correctly replace its functions by taking combined enzyme preparations, correcting blood sugar and strictly following a diet, you can completely eliminate the danger, normalize digestion and restore quality of life.
Important! Complete removal of the pancreas is always a life-saving operation, and once it is saved, its level must be maintained by constant compliance with medical orders.
Nutrition after surgery
After surgery to remove the pancreas, all patients, without exception, are prescribed a strict diet. You will have to stick to it constantly. Remove from the diet once and for all:
- fried and fatty foods;
- smoked meats;
- pickles;
- flour;
- spices;
- canned food;
- semi-finished products;
- sausages;
- spicy dishes and sauces;
- carbonated and alcoholic drinks;
- chocolate;
- cocoa;
- legumes
The patient's daily diet must include lean meat and fish. However, they cannot be consumed together with the skin. He also needs to eat dairy and fermented milk products every day (their fat content should not be more than 2.5%).
You also need to eat food according to certain rules:
- for the first 3–4 months after surgery, it needs to be crushed to a puree-like consistency;
- you need to eat small portions at least 5 times a day;
- 30–40 minutes before meals you need to inject insulin (only if short-acting insulin is used), and while eating you need to take an enzyme preparation;
- food must be warm, hot and cold dishes are prohibited;
- The last meal should be taken 2-3 hours before bedtime.
If you strictly follow the diet and promptly use medications prescribed by your doctor, you can live a long and happy life even after complete removal of the pancreas. If you neglect the doctor’s recommendations, this can lead to serious consequences and significantly reduce your life expectancy.
When a person is faced with acute pancreatitis, he often looks for any way to get rid of the problem. The thing is that with this disease the patient experiences very severe pain, which literally does not allow him to live. Sometimes you even want to pull the organ out of the abdomen so that it does not disturb the patient. Therefore, people sometimes wonder whether it is possible to live without a pancreas, and what the consequences might be. To answer this question, you need to understand a little about the physiology of digestion.
Features of nutrition after removal of the gland
Dietary nutrition is a prerequisite for preventing severe consequences after removal of the pancreas. The patient should immediately understand that following a diet, along with enzyme replacement and glucose-lowering therapy, is a vital necessity, and this is forever, so that severe consequences do not develop after removal of the pancreas.
Immediately after the operation, the patient is prescribed a fast for 3 days, water is allowed in small portions up to 1 liter per day. Nutrients and vitamins are administered intravenously with a drip.
On the 4th day, you are allowed to eat a couple of dry biscuits or white bread crackers in small portions throughout the day, 1-2 glasses of non-hot, weak tea. On days 5-6, pureed soups, crackers, and tea are given. By the end of the week, boiled semi-liquid porridges - buckwheat or rice, dried bread - are introduced into the menu. From 7-8 days, in addition to soups, they serve main dishes - vegetable purees, steamed dishes from minced meat.
An approximate daily menu after removal of the pancreas should include foods rich in protein and vitamins
After 10 days, they gradually switch to food prepared in the usual way. Usually the patient is already discharged from the hospital by this time. What can you eat after pancreas removal? The products can be very diverse, the main thing is to strictly follow the following rules when creating a menu:
- meals should be fractional: 4-6 times a day with small amounts of food;
- you need to exclude fatty foods, confectionery products (cakes, pastries, chocolate);
- exclude smoked and canned foods, hot seasonings, sauces and ketchups from the diet;
- exclude strong coffee and tea, carbonated and alcoholic drinks;
- The menu should include both animal and vegetable protein, vegetable oils, fresh and stewed vegetables, fruits, and herbs.
Foods that need to be excluded from the diet if you have an operated pancreas
Stationary period
A very important stage of rehabilitation after removal of the pancreas is the recovery period in the hospital. It is here that the primary restructuring of the body’s functions occurs under the influence of new conditions, the assimilation of the algorithm of actions by the patient himself, and the selection of dosages of medications. At the same time, during the observation process, possible side effects are identified and eliminated.
Complications after pancreas removal
In the first hours or days, there is a high probability of consequences occurring:
- bleeding - if not the entire organ is removed during the operation, then the stump may bleed, as well as neighboring organs (stomach, spleen, gallbladder, liver) injured during the operation;
- inflammation - occurs when an infection occurs, which is treated by carefully treating the external sutures, and internal inflammation requires treatment with antibiotics or opening of the peritoneum with further disinfection of the lesions;
- suppuration and peritonitis are a rare but life-threatening complication after surgical interventions in the abdominal cavity; recovery will require time and effort.
Of the nonspecific consequences, there is a high probability of pneumonia: inactivity provokes congestion in the lungs. For prevention, breathing exercises are prescribed in the first days.
Diet after surgery
For the first 48-72 hours, the patient is prescribed complete fasting on water. During the day you need to drink water in small portions. The liquid will protect against dehydration, dissolve and remove the remains of anesthesia drugs, and prevent adhesions in the intestines at the sites of internal sutures.
Then, under the supervision of a doctor, food is gradually introduced into the diet. At first it is pureed food with many restrictions. And from this time on, replacement therapy must be started.
Important! All patients, as a consequence of complete removal of the pancreas, develop diabetes mellitus, which is compensated by the administration of insulin throughout their lives.
The level of digestive enzymes that allow food to be absorbed and the hormone insulin are set individually. In the hospital, the operated patient is taught how to take medications correctly (enzymes are taken with meals), as well as how to administer medications by injection (insulin is “injected” after eating). These simple procedures are accessible to everyone. However, the realization that drugs will have to be taken and administered throughout life has a depressing effect on the patient after removal of the pancreas. If necessary, a psychologist or psychotherapist is invited to help in adopting a new lifestyle.
If there are no complications or they are eliminated, some time after the removal of the external sutures (the internal ones dissolve over time, their removal is not required), the patient is discharged to the outpatient clinic.
The inpatient period lasts from 3 weeks to 2 months.
Gland transplantation
The modern level of transplantology makes it possible to perform pancreas transplantation. There are still no more than 1 thousand such operations performed in the world per year, in large foreign clinics, as well as in Russia, Belarus and Kazakhstan.
Pancreas transplantation is indicated after its removal, if there are no contraindications due to age and health. More often, the tail part with beta cells is transplanted to normalize glucose metabolism. Modern technology is used to implant these cells by injecting their mixture into a vein.
Transplantation of insulin-secreting beta cells after pancreatectomy surgery
Complete gland transplantation is rarely performed. This is a complex operation that requires, first of all, normal function of all other organs, and subsequently lifelong use of immunosuppressants to suppress donor organ rejection. The survival rate of patients with a donor gland still remains low (80% of patients survive to 2 years, and only 28% to 10 years).
The operation to remove the pancreas is performed for health reasons. Without the pancreas, life is possible, and even without consequences, if you scrupulously follow medical prescriptions and adhere to a diet.
The pancreas is an important organ of the human digestive system. It takes part in the regulation of protein, carbohydrate and fat metabolism.
In case of a number of life-threatening diseases and serious damage to an organ, a person may undergo surgery to remove it, which leads to certain consequences.
Functions of the pancreas
The pancreas in the human body performs two main functions:
Thanks to the first function, it takes part in the digestive process by secreting pancreatic juice, which then enters the duodenum.
The intrasecretory function is the production of the hormone insulin by the organ, which regulates the concentration of sugar in the blood. The gland also produces another hormone, glucagon.
It promotes the following processes in the human body:
- participates in the production of digestive enzymes;
- regulates metabolism in the body through insulin, which lowers blood sugar levels, and glucagon, which increases its concentration.
Damage to an organ, as well as the development of an inflammatory process in it, leads to metabolic disorders in the body. In case of severe diseases of the organ, a person may be prescribed its removal.
Indications for removal
The main indications for removal of a fragment of the pancreas or the entire organ are:
- malignant tumors;
- acute pancreatic necrosis;
- necrosis of the gland due to alcohol abuse;
- calculous pancreatitis.
Pancreatic cancer is the main indication for its removal. Much depends on the degree of tumor development. If it affects a certain area of the gland, then its resection (excision) is performed. If the tumor has spread extensively, complete removal of the organ may be a radical method.
Pancreatic necrosis is also one of the possible reasons for the elimination of the pancreas. With it, it produces juice, under the influence of which its actual self-destruction and digestion of itself occurs.
With prolonged alcohol intoxication, the organ may begin to die. In some cases, the patient will be prescribed complete or partial removal of the organ.
With calculous pancreatitis, calcium salts accumulate in the gland. The result is the formation of stones that can clog the ducts. With this disease, patients in life-threatening cases undergo removal of the gland.
Pancreatectomy (removal of the entire gland or its fragment) is a complex and radical operation with a high mortality rate. Moreover, the consequences of the operation are often unpredictable.
This is due to the special anatomical location of the organ. It is tightly covered by neighboring organs, which significantly complicates the surgeon’s access to it.
Often, pancreatectomy is not limited only to excision of the gland itself, but also requires the removal of adjacent adjacent organs (spleen, gallbladder and even part of the stomach).
Reasons and indications for removing part of the pancreas
Radical treatment methods for severe pancreatic pathology are the last choice in the absence of positive effects from therapy at the previous stages. Any severe disease of the pancreas, if conservative treatment is ineffective, is subject to surgical intervention.
Partial resection is performed in the presence of the following identified indications:
- tumor, fistula, cyst, stone, abscess,
- malignant neoplasms in a certain part of the organ or metastatic damage when the source of cancer is another organ,
- traumatic tissue damage,
- peritonitis, the source of which was inflammation of the pancreas,
- intense bleeding from the vessels of the gland,
- exacerbation of chronic inflammation in the gland.
Surgery is performed if there is:
- complications after cholecystectomy (without bile, deep disturbances in the digestion of food occur, which increases the load on the spleen and requires constant adherence to dietary restrictions; errors in diet cause deep pathology of the pancreas),
- dysfunction or complete cessation of activity of the spleen (necrosis occurs and there is an urgent need to remove the affected pancreas, but even with its absence you can live a long time, leading a full normal life),
- development of tumors: even an ordinary pancreatic cyst under the influence of unfavorable external factors (smoking, alcohol, unhealthy food) can turn into a malignant formation that requires urgent resection,
- entry of a stone from the gallbladder through the common duct into the pancreas during surgery for cholelithiasis (it is impossible to remove a stone from the pancreatic tissue without significant damage to it, usually the pancreatic tissue is not restored, the organ must be resected),
- chronic pancreatitis with frequent severe exacerbations and poor prognosis.
The cost of any elective resection, such as a pancreatic cyst, in hospitals and medical centers varies depending on the geographical location and the qualifications of the operating specialists.
Removal of the head of the pancreas
Statistics show that in 80% of the development of a gland tumor, its head is affected. A pancreaticoduodenal method of surgical intervention is performed, which is called by the author - the Whipple procedure. The operation is carried out in two stages:
- Removal of the affected fragment and part of the neighboring organs involved in the pathological process.
- Subsequent restoration of damaged ducts, gallbladder and patency of the digestive canal.
- impaired absorption of nutrients due to the removal of an important part of the organ that synthesizes digestive enzymes,
- failure in carbohydrate metabolism with subsequent development of diabetes.
The laparoscopic method is used and the operation is performed under general anesthesia.
A laparoscope is inserted through small incisions, the operated area is examined, the feeding vessels and duodenum are blocked and removed, nearby regional lymph nodes are removed, and sometimes it is necessary to partially remove adjacent organs.
After this, a new connection is created between the stomach and small intestine and the body of the pancreas.
The operation is difficult and entails dangerous consequences after removal of the head of the pancreas:
If the head is removed, the following often develop:
- damage to the nerves and vessels adjacent to the gland,
- bleeding,
- infections.
Postoperative pancreatitis with severe secretory insufficiency almost always develops. The recommended treatment regimen must be followed for years. It may consist of lifelong oral replacement therapy plus a special diet for a long period. After surgery, a person becomes disabled.
Operation Beger
Isolated resection of the affected head of the pancreas without removal of the duodenum was developed and introduced by Beger in 1972. During this operation, the stomach and duodenal bulb tightly adjacent to the gland are preserved, which does not interfere with the passage of the food bolus through the digestive canal. The gastropancreatoduodenal discharge of secretions from the gallbladder and pancreas through the small intestine is preserved.
As a result of the research, positive results were obtained in the postoperative period, on the basis of which the method received good feedback from specialists and was widely used. Using this technique, the pancreas is dissected in the area of the isthmus with isolation of the superior mesenteric and portal veins. There is a possibility of bleeding due to existing complications of chronic pancreatitis, in particular, with the development of regional portal hypertension. In these cases, manipulation of the veins is dangerous due to large blood losses.
Rehabilitation process after pancreatectomy
After pancreatectomy, the patient may experience complications such as:
- internal bleeding;
- seam divergence;
- infection at the removal site;
- the appearance of bedsores due to prolonged lying down.
The rehabilitation process after surgery includes providing the patient with special care in the first 3 days.
The first days after pancreatectomy are dangerous for patients due to possible reactions of their body to the administered anesthesia.
There is a high risk of damage to neighboring organs. The intensity of postoperative monitoring of the patient's condition does not depend on whether the entire gland is removed or only part of it.
In the future, the patient must adhere to certain rules:
- Follow a strict diet with the exclusion of spicy, fatty, fried and smoked foods from the diet.
- For the rest of your life, regularly take medications containing digestive enzymes. With their help, replacement therapy will be carried out.
- Regularly inject insulin into the body to maintain normal blood sugar levels.
A patient who has had their pancreas removed is especially in need of replacement therapy.
To maintain normal digestion, he is prescribed enzyme preparations, including:
- Micrazim - for the absorption of proteins, carbohydrates, fats;
- Vestal - to stimulate digestion;
- Creon - as a replacement for the lack of enzymes in the body.
Enzyme preparations are also necessary to eliminate nausea and intestinal disorders in patients. These symptoms are typical for the postoperative period.
All patients with a removed pancreas develop type 1 diabetes. They need constant injections of insulin, which will replace the lack of hormone in the body.
Particular attention is paid to the diet of such patients.
Recommendations are provided for them:
- strict diet;
- adequate fluid intake;
- eating only chopped boiled, stewed, steamed, baked food;
- fractional meals;
- exclusion of coarse fiber from the diet.
If the patient follows the rules of rehabilitation, it is possible to significantly prolong their life and improve its quality.
Video material about the pancreas and its importance for the body:
What to expect after the operation?
Until recently, it was believed that surgery to remove the pancreas was a myth, and the patient would not survive after it. Nevertheless, medicine has made huge strides forward. Now people can lead relatively good lives without this important organ. The main consequences that await patients are:
Strict adherence to the diet. Without careful monitoring of your diet, it will be impossible to achieve any satisfactory results. It is prohibited to eat any fatty, fried or smoked food. Basically, you can only eat dietary foods that are easily digestible. You can read more about the diet on the Internet. Lifelong use of enzyme preparations. Since the main digestive organ has been removed and they need to eat, patients are required to artificially replace proteolytic substances with tablets. Formation of type 1 diabetes mellitus. This consequence of the elimination of the gland develops in 100% of patients. It requires treatment with insulin injections and a strict diet. Psychological disorders. One of the most important points to work on. Often people who have undergone surgery do not want to exist like this. They withdraw and isolate themselves from others and feel inferior. At this stage, it is necessary to help such patients, to make them understand that many people in the world live well with the same problem.
Related Posts
Removing the pancreas is a radical solution. Under what conditions is surgery to remove the gland justified?
Can a person live without a pancreas? How will the surgery affect your quality of life? What to do after removal? The answers to these and other questions are presented in the article.
Life without a gland
Modern medicine gives a clear answer to the question of how to live after removal of the pancreas. Technologies have made it possible to increase the life expectancy of patients who have undergone organ removal.
After pancreatectomy, a person can live a full life, but with limitations. He requires a strict diet in the first weeks after surgery. In the future, his diet expands.
People who have undergone gland resection need daily monitoring of their health.
Three basic rules must be followed:
- Inject insulin into the body every day.
- Take medications containing digestive enzymes daily.
- Follow a strict diet, reducing your carbohydrate intake.
Those who have experienced removal of the head of the gland, its tail, or the entire organ will not be able to fully restore full health.
With the removal of an organ, the digestive system malfunctions and the production of certain hormones ceases. Replacement therapy and proper nutrition can smooth out the consequences of surgery and partially compensate for the functions of the removed organ.
Life expectancy for patients with a removed pancreas depends on the severity of the disease leading to pancreatectomy.
The least favorable prognosis is for patients who have undergone organ resection due to cancer. In the presence of metastases, removal of the gland can prolong the life of patients by only 1 year.
Many of them die within the first year after surgery.
The average life expectancy of patients with an organ removed is 5 years.
If patients carefully follow the diet, take insulin, enzymes and hormonal drugs in a timely manner, the overall life prognosis is unlimited - a person can live a long life.
The pancreas is one of the most important endocrine glands in our body, which consists of three parts - the head, body and tail. It secretes hormones such as insulin, glucagon, somatostatin and pancreatic polypeptide. The first two take part in the regulation of carbohydrate metabolism.
Insulin lowers the amount of sugar in the blood, while glucagon, on the contrary, increases it. Accordingly, in the absence or insufficiency of insulin, diabetes mellitus develops. It is this complication that is most dangerous when removing the gland.
In addition to hormones, the pancreas also secretes digestive enzymes: alpha-amylase, which helps break down proteins, lipase, which digests fat, and lactase, which is involved in the absorption of milk sugar (lactose). Without them, digestion deteriorates significantly, and a person simply does not receive enough nutrients and vitamins, in particular fat-soluble ones.
Somatostatin is a releasing hormone, or releasing factor, that reduces the effect of growth hormone on the body. In children, it directly slows down the processes of growth and physical maturation, and in adults it prevents the development of acromegaly, a disease in which there is disproportionate growth of the skeleton and soft tissues in adults and physically mature people due to an excess of somatotropic hormone.
Why can the pancreas be removed?
In various diseases and pathological conditions, the pancreas can no longer function and therefore must be removed, partially or completely.
Surgery is the most radical method.
This treatment method is used only when drug therapy does not produce the desired effect.
Removal of the gland (or pancreatectomy) is a complex operation that can be caused by the following reasons:
- cystic formations;
- organ injuries;
- blockage of gland ducts with stones (rarely – as a concomitant of cholecystitis)
- inflammatory processes in the gland (acute or chronic pancreatitis in the acute stage);
- oncological diseases (malignant tumors);
- fistulas;
- pancreatic necrosis;
- vascular bleeding;
- peritonitis;
- alcohol abuse.
The most common reason leading to pancreatectomy is cancer. Risk factors for cancer:
- Tobacco smoking.
- Eating large amounts of fatty and fried foods.
- Alcoholism.
- Previously undergone gastric surgery.
- Pancreatic necrosis;
In addition, the presence of a genetic predisposition may contribute to the occurrence of pancreatic cancer.
How is pancreatectomy performed?
Undoubtedly, the operation is complex and requires great care and experience of the surgeon. Since the gland is located behind the stomach, small intestine, and liver, access to it is difficult. It is performed using laparoscopy.
This method is based on the introduction of one or more special cameras into the patient’s abdominal cavity through small incisions in order to more clearly determine the location of any organ (in the described situation, the pancreas).
After this, a large incision is made and either part of the gland or its entirety is cut out through it. In total, the process takes about 5 hours.
The operation was not easy, and therefore there was a high risk of various complications. The following may occur immediately during and after surgery:
- bleeding;
- infection in the wound;
- seam divergence;
- Bedsores may appear in bedridden patients.
The most serious complication after removal of the pancreas is type 1 diabetes. It develops due to a complete cessation of insulin production, i.e. absolute insulin deficiency. All types of digestive processes are also disrupted due to a lack of enzymes.
In the postoperative period, patients experience severe weakness, weight loss, and there may be damage to nerves and nearby vessels.
Today, the prognosis is favorable with the correct surgical technique.
Specifics of the operation
The specificity of the operations lies in the structural features of the gland:
- its tissues are easily injured and do not recover after damage,
- enzymes during surgery on a damaged gland can enter the abdominal cavity and cause necrosis of neighboring organs, peritonitis, development of fulminant shock,
- The pancreas is susceptible to the influence of any factors - there are known cases of the development of pancreatitis as a result of operations on organs distant from the pancreas,
- The walls of the organ are fragile, the sutures on them are not securely fixed.
Is it possible to live without a pancreas?
The answer to this question is clear and simple: yes. Modern medicine helps to maintain life without a pancreas for people who have undergone the above-mentioned operation at a very high level. But in order for the body to adapt to a new life, you need to strictly follow some recommendations.
If diabetes mellitus occurs (and it occurs in almost 100% of cases), patients are prescribed lifelong insulin therapy. It is necessary because they no longer have insulin. If you refuse this, the blood glucose level rises to very high levels, and the person can easily die. Therefore, even with injections of the desired hormone, you should regularly check your sugar. Over time, you can learn to do this yourself using a glucometer.
Since it is necessary to maintain digestion, patients are prescribed drugs (Creon, Mezim, Pangrol) containing all pancreatic enzymes.
In addition to medications and hormonal therapy, you must follow a strict diet after surgery. Forbidden:
- Spicy and smoked products.
- Salted and pickled.
- Fatty dishes.
- Coffee and strong teas.
- Freshly baked bread.
- High fat dairy products.
- Potato
- Flour products.
- Excess carbohydrates.
- Eggs in large quantities.
- Alcohol.
- Carbonated and sweet water.
Meals should be small and high in protein. It is recommended to eat fresh fruits and vegetables that are low in carbohydrates. It is better to cook, stew or bake dishes.
In the first days after pancreatic surgery, it is recommended to drink only, and only still drinking water. After three days, you can start eating diet crackers and even drink tea, but it should be unsweetened.
A little later, the diet expands, and patients are allowed to eat thin, low-fat soups and even steamed omelettes. Then you can add slightly dried wheat bread, buckwheat and rice porridge.
Next, you can try a small amount of fish (in no case fried!), Vegetable puree of a liquid consistency.
An important condition of the diet in the postoperative period is to minimize the amount of salt and, if possible, eliminate sugar in its pure form.