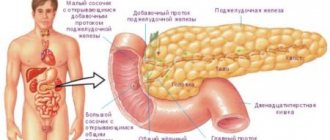
The pancreas is an organ that performs two very important functions for the entire body. The first is the production of food enzymes that help break down proteins, fats and carbohydrates and transport them to the duodenum. The second is endocrine, associated with the production of insulin.
But formations in the pancreas impair the performance of its functions.
Today, doctors note an increase in the number of patients with a similar problem by an average of 1% every year.
If a mass formation is noticed during an ultrasound of the pancreas, then this is a sure signal for an examination to check the presence or absence of a tumor.
Causes of development of ductal adenocarcinoma in the pancreas
- Extremely aggressive tumor; morbidity and mortality rates are almost identical;
- The average age of patients is 50-70 years;
- Ductal adenocarcinoma is the most common exocrine tumor of the pancreatic duct;
- Among exocrine tumors of the pancreas it is 80%;
- Adenocarcinoma is somewhat more common in men.
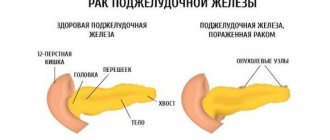
- This carcinoma most often occurs in the head of the pancreas (60% of all tumors).
What is the tail of the pancreas?
The tail is the final, narrowest part of the pancreas; it completes the organ. Like all glands, its parenchyma has a glandular structure, but there are some peculiarities. The tissue is represented by acini and islets of Langerhans.
Acinus (lobule) is the simplest functional unit of the pancreas, consisting of several types of different cells with enzyme-forming function. Each lobule has its own primary excretory duct with vessels; its cells produce several types of enzymes involved in the breakdown of proteins, fats and carbohydrates. A group of acini forms lobes with larger ducts flowing into a common one - the Wirsung. This structure provides exocrine function.
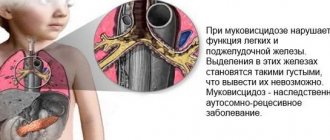
The islets of Langerhans are responsible for endocrine activity. They are located between the acini and also consist of different types of cells that synthesize hormones. Unlike enzymes, hormonally active substances enter the bloodstream immediately and begin to act. The most significant among them is produced by beta cells. This is insulin, which is responsible for carbohydrate metabolism. With its deficiency, diabetes mellitus develops - a serious disease leading to life-threatening complications with a poor prognosis.
The ratio of the exocrine and intrasecretory parts of the organ is 9:1. The peculiarity of the structure of the caudal part of the pancreas is the predominance of the islets of Langerhans in the parenchyma. The size of the islets of Langerhans is 0.1-0.2 mm, their total number in the human pancreas ranges from 200 thousand to 1.8 million. The cells of this structural unit produce hormones that control the basic metabolic processes in the human body. Insulin, glucagon and amylin, which affect carbohydrate metabolism, lead to severe disorders in any etiology of tail damage: first of all, diabetes mellitus develops, which requires lifelong treatment and adherence to a special diet.
Where is the tail of the pancreas located?
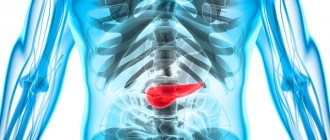
The pancreas, unlike other organs of the digestive system, is located retroperitoneally. This means that it cannot be palpated during an objective examination, and without special examination methods it is difficult to determine whether it is too large or pathological. In the projection onto the anterior abdominal wall, it is located 5-10 cm above the navel, the head is visualized during ultrasound in the right hypochondrium, and the tail borders the spleen, left kidney and adrenal gland.
The tail becomes narrower towards the spleen. It is stretched horizontally, slightly raised up. It is located in the projection of the left hypochondrium, is located deep, tightly closed by other organs - all this complicates the timely diagnosis of the inflammatory process and the detection of oncology.
Which method of diagnosing ductal adenocarcinoma to choose: CT, MRI, ultrasound
Selection Methods
- CT (the most practical method for diagnosis, staging and resectability assessment).
Pathognomonic signs
- Space-occupying formation with poorly defined edges;
- Adenocarcinoma is poorly vascularized;
- Dilatation of the pancreatic duct (early symptom) and bile duct (double duct symptom);
- Chronic obstruction of the pancreatic duct causes parenchymal atrophy;
- There is early infiltration of retroperitoneal fatty tissue, nearby vascular structures and neighboring organs;
- Adenocarcinoma often metastasizes to the liver and lymph nodes.
What will CT images of the abdominal cavity show for ductal adenocarcinoma of the pancreas?
- A hypovascular tumor can be most clearly differentiated from surrounding normal tissues during the parenchymal phase of contrast enhancement;
- Obstruction of the pancreatic duct and bile duct is clearly visualized, which makes the prescription of RCCP redundant.
Why is an abdominal ultrasound performed for ductal adenocarcinoma?
- Liver metastases can usually be detected in a fairly early phase.
- A hyperechoic tumor with cholestasis and obstruction of the pancreatic duct, usually easily identified;
- Good method for local staging;
- More preferable than CT and MRI for diagnosing small tumors.
Is MRI of the pancreas performed for ductal adenocarcinoma?
- Hypointense tumor on T1-weighted images with poor contrast enhancement;
- Slightly hypointense on T2-weighted images;
- In combination with MRCP, the pancreatic duct and biliary tract can be visualized in sufficient detail;
- The diagnostic information is almost equivalent to that of CT, but the technique is much more complex.
Ductal adenocarcinoma of the pancreas.
Hypovascular malignant tumor of the tail of the pancreas, growing into the hilum of the spleen and stomach. a, b Ductal adenocarcinoma of the pancreas. MRI: a) Dilation of the pancreatic duct, atrophy of the pancreatic parenchyma;
b ) Hypovascular tumor of the head of the pancreas.
Why is RCCP performed for ductal adenocarcinoma?
- Currently, it is practically not used for the diagnosis of pancreatic cancer and provides virtually no useful information about resectability
- Indicated for bile duct stenting.
Formations and treatment of the tail of the pancreas
Formations of the tail of the pancreas are much less common than other parts of this organ. Doctors say that this is only about a quarter of common pancreatic diseases. However, many tumors are malignant and very difficult to treat because they are detected late, having reached a significant size by the time they are detected. The tail of the pancreas is most often examined through the left kidney or spleen.
Signs of cancer in this area are very typical for cancer patients and yet have a number of their own characteristics. A dull pain radiates very strongly to the epigastric region. When the patient sits down and leans a little forward, the attacks of pain decrease, although not for long.
Treatment of tail formations is almost impossible. Patients usually require surgery. She uses a very complex technique called Distal Partial Pancreatomy. It is advisable to carry it out only in a good specialized medical center, because sometimes there are all sorts of complications that require a quick response from professional doctors and the use of special medical equipment. During such an operation, only the tail of the pancreas is removed after all the blood vessels that supply this gland are blocked. Sometimes nearby organs are also operated on. If the spleen or nearby vessels are affected, the surgeon immediately removes them too. All affected organs that have been removed are necessarily sent for histological examination in order to correctly and optimally prescribe further treatment for the patient.
Where does the tail of the pancreas project?
It is tightly sandwiched between the internal organs. Due to its anatomical features, it is covered in front by the stomach, the lower part by the duodenum, and behind by the spinal column and powerful back muscles. This explains the rarity of injuries and bruises to this organ. The tail of the pancreas is projected onto the anterior lateral abdominal wall and falls on the area of the left hypochondrium approximately in the middle of the navel-xiphoid process segment.
You can visualize the projection as follows: mentally draw vertical and horizontal lines through the navel. In the upper corner on the left side there will be a projection area of the tail of the pancreas. To the left of the white line of the abdomen and above the horizontal line.
Reasons for progression
As mentioned above, experts cannot yet say why exactly the pancreas is affected. But there are known factors that increase the risk of tumor formation on an organ. These include:
- hereditary predisposition;
- smoking. This factor increases the risk of tumor formation almost three times;
- obesity;
- history of diabetes mellitus;
- long-term use of alcoholic beverages;
- the presence of chronic pancreatitis in a person;
- harmful working conditions. The risk of tumor formation on the head of the gland increases if a person, due to the nature of his work, is forced to come into contact with carcinogenic substances.
How are hypodense formations treated in Germany?
Any of the diseases that are “hidden” under the phrase “hypodense formations” is treated in Germany. Methods have been developed that allow the most effective treatment of benign and malignant tumors of various organs. German clinics treat pancreatic cancer, liver and intrahepatic duct cancer, melanoma, non-Hodgin lymphoma, stomach cancer and many other malignant diseases. Treatment methods have been developed for even the rarest diseases. Depending on the specific type of disease, treatment may include medications, surgery, radiation therapy, and targeted therapy.
Specialized clinic
Doctor: Nadja Harbeck: specialist in breast cancer treatment
Oncology at the University Hospital Munich
9.8/10
Germany, Munich
Diagnostic examination
Diagnosis of pancreatic cysts includes a visit to a gastroenterologist. The doctor conducts an examination by palpating the abdominal area. Palpation of this area allows you to determine a round formation of dense elastic consistency with clear boundaries. The specialist interviews the patient, paying special attention to the following criteria: age, presence of chronic diseases, bad habits, lifestyle.
Instrumental and laboratory diagnostic methods help confirm the diagnosis:
- Laboratory tests: blood study, biochemistry. The presence of cystic formations will be reflected by shifts in ESR (erythrocyte sedimentation rate), increased bilirubin, increased activation of alkaline phosphatase, and an increased number of leukocytes. Inflammatory processes in cystic cavities reflect the presence of leukocytes and total protein in the urine;
- Instrumental methods:
- Ultrasound examination, which allows you to determine the size of the formations, location, degree of cystic lesion, complications that have arisen;
- Magnetic resonance imaging (MRI) reveals in detail the structural features of cystic formations, size, degree of impact on nearby tissues and structures;
- Endoscopic cholangiopancretography is a high-precision research method that allows you to study in detail the structure of the cyst, the features of its structure, the effect on surrounding tissues, and the connection with the ducts;
- Radionuclide imaging (scintigraphy). The method is used as an additional research method to clarify the location of the tumor in the pancreas;
- A general abdominal radiograph is used to determine the boundaries of cystic formations;
- Biopsy. The study is carried out in case of clarification of the nature of the internal contents of the formations. The examination reveals cancer cells. The biopsy is performed during a computed tomography scan or under ultrasound guidance. This type of examination allows you to accurately differentiate cystic formations, identify malignant tumors, and prevent the development of atypical cells.
Benign tumors
Benign formations are divided into:
- neurogenic tumors – ganglioneurinomas and neuromas;
- changes in the epithelial tissue of the pancreas - cystadenoma and adenoma;
- tumors formed in connective tissue - lipomas and fibromas;
- lesions of muscle tissue - leiomyomas;
- tumors formed in the islets of the pancreas - insulinoma;
- formations that affected the vessels of the organ - lymphangiomas, hemangiomas.
Breast cancer has a number of distinctive features:
- the structure of the gland tissue does not undergo changes;
- the tumor slowly increases in size;
- metastases do not appear;
- there is no germination into neighboring organs.
Scientists cannot name the reason why benign formations occur. But they identified several factors that more often than others can contribute to the growth of formations:
- unbalanced diet;
- harmful addictions;
- in case of genetic predisposition;
- poor ecology in the place of residence.
If a person has a benign formation in the pancreas, this is accompanied by a number of symptoms:
- jaundice;
- nausea and vomiting;
- profuse sweating, confusion, weakness, fear;
- pain in the navel area, radiating to the left side of the body.
A benign tumor can degenerate into cancer and cause bile intoxication, chronic pancreatitis, and diseases of the endocrine system.
Malignant tumors
This type of tumor is not only difficult to diagnose, but also difficult to treat. We can say that it cannot be cured. You can only extend a person’s life for a certain period. It is very difficult to determine the presence of a tumor, since in the early stages of its formation it does not appear at all. There are also situations when the symptoms of cancer are invisible until stage 4.
- squamous cell carcinoma;
- adenocarcinoma;
- endogenous cancer;
- acinar cell carcinoma;
- cystadenocarcinoma.
Due to the fact that the tumor on the head is located in close proximity to the gastrointestinal tract, it first of all makes itself felt by symptoms of digestive disorders. A person experiences nausea and vomiting, diarrhea, excrement becomes discolored, bloating is noted, and the urine darkens. In addition, there are several other symptoms:
- an increase in glucose levels in the bloodstream;
- decreased appetite;
- weight loss;
- obstructive jaundice. This symptom is considered characteristic. Obstructive jaundice occurs when a tumor compresses the bile duct.
The danger of a neoplasm also lies in the fact that it can grow into other organs. This is observed at the 2nd or 3rd stage of its formation. At 4, the spread of metastases to other organs is noted. In this case, surgical intervention is no longer performed. The basis of treatment is supportive therapy.