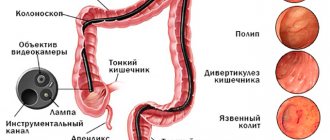
FGDS, what is it? This is a medical procedure that examines the upper part of the esophagus, stomach, and duodenum. It is carried out to assess the condition of these organs, as well as their contractile properties. In addition to studies during gastroscopy, tests can also be collected that allow the doctor to fully determine the picture of the disease.
This examination is one of the most accurate, and therefore the most common. Carrying out FGDS is simply necessary to identify diseases such as stomach ulcers or cancer. It is also prescribed in cases where the patient experiences symptoms such as nausea, accompanied by painful and frequent vomiting, and severe pain in the stomach area.
Indications for FGDS
Today, fibrogastroduodenoscopy (or FGDS)
is an indispensable method for studying the gastrointestinal tract. During the procedure, using a fiberscope, you can introduce a drug into the body, collect pathological material from the lesion for detailed diagnosis, and also carry out some surgical interventions.
There are the following indications for performing FGDS:
- pain in the stomach area that occurs after eating. This symptom may be a sign of diseases such as gastritis and peptic ulcer;
- nagging hunger pains that occur approximately six hours after eating. Hunger pains are usually a symptom of duodenitis (disease of the duodenum);
- prolonged heartburn;
- bloating;
- frequent belching;
- decreased appetite;
- sudden weight loss;
- recurrent (repeated) vomiting;
- dysphagia (swallowing disorder);
- as preparation for surgery (for example, surgery on joints, heart and others);
- if gastric bleeding is suspected.
Preparatory stage before the FGDS examination
At the very beginning, you should psychologically tune in to the fact that this examination is by no means pleasant, but also does not cause much pain. Before the examination, you must completely empty your stomach 12 hours before, do not eat or drink. Be sure to take a small towel and all the necessary documents with you.
It is worth understanding that during the examination, your clothes may be stained with the contents of the stomach, because regurgitation during FGDS is an absolutely normal phenomenon.
During the examination, the patient, as is customary, is positioned in a lying position on the left side. A person cannot talk during FGDS, but can hear the words and advice of the doctor and nurse, making the procedure more comfortable. If the device is already inside, it is strictly forbidden to make sudden movements and try to pull it out, as this can cause great harm to the body.
Ulcer
Ulcer
is a pathological formation characterized by deep damage to the mucous membrane. With this defect, the patient is bothered by severe sharp pain in the stomach area that occurs after eating. This symptom is a characteristic sign of diseases such as gastritis or peptic ulcer. The patient also has:
- nausea and vomiting that occurs after eating;
- heaviness and fullness in the stomach;
- sour belching;
- heartburn.
Destination purpose
— for stomach or duodenal ulcers, using FGDS, you can stop bleeding, administer medications, and also detect deep defects (ulcers) of the mucous membrane, which can reach several centimeters in diameter. Also during the study, inflammatory elevations are revealed along the edges of the ulcers, which indicate the intensity of inflammation.
After the procedure
After the procedure, mild abdominal pain may occur.
If short-term anesthesia was used during FGDS, then after the procedure the observed person is sent to a special ward, where he can safely remain until the effect of the drug completely wears off.
Read: What is Japanese honeysuckle and what are its healing properties?
If only local anesthesia was used during the examination, the patient can immediately go home or wait in the corridor for some time, which is necessary for the doctor to complete the examination. After an FGDS examination, some patients may experience symptoms such as:
- Minor pain in the abdominal area
- Mild nausea
Immediately after the procedure, you should not eat or drink water for several hours.
Gastroesophageal reflux disease
With this pathology, the lower part of the esophagus is affected due to the reflux of gastric contents into it. As a rule, with this disease the patient experiences heartburn and sour belching after eating.
Destination purpose
— with the help of diagnostics of the esophagus and stomach, a complete picture of what is happening is compiled, which subsequently determines the correct treatment algorithm for this disease.
Contraindications
There are some contraindications to performing any physiological procedures. Fibrogastroscopy is no exception. If at least one of the following points is present, the study may be canceled:
- serious condition of the patient;
- the presence of infectious and mental diseases;
- narrowing of the esophagus to a significant extent;
- diseases of the cardiovascular system in the acute stage;
- the presence of varicose veins in the esophagus;
- acute stage of bronchial asthma;
- disorders of the blood clotting process.
Inflammation of the esophageal mucosa
With this pathology, the patient may experience the following symptoms:
- heartburn;
- mouth pain;
- sensation of a foreign body in the throat;
- nausea;
- vomit.
Destination purpose
— with the help of FGDS, the form of esophagitis is determined, which makes it possible to prescribe the correct treatment in the future.
Frequently asked questions from readers
Most people who have health problems related to functional disorders in the digestive system and who are about to undergo an esophagogastroduodenoscopy procedure ask the following questions.
Is it painful and is anesthesia required for endoscopy?
Intramuscular or intravenous administration of painkillers is not required for this type of examination. Anesthesia is used only in extreme cases, when the patient suffers from mental disorders, has phobias and mental imbalance, which can lead to disruption of the gastrointestinal tract examination session itself. For the rest of the category of people who do not have such pathologies, it is enough to irrigate the mouth and larynx with a special spray that has mild pain relief. A person feels a slight numbness of the palate, throat and tongue, and the urge to vomit is dulled. The process of inserting the endoscope itself is not painful. Therefore, complete pain relief is not provided under the therapeutic protocol.
It goes without saying that the patient experiences some discomfort due to the presence of a foreign body and may begin to feel sick, but there is no acute or aching pain syndrome.
What are the differences between EGDS and FGDS?
The distinctive features of these two diagnostic procedures are that EGDS covers the study of three digestive organs at once (esophagus, stomach, duodenum), and fibrogastroduodenoscopy focuses only on the last two elements of the gastrointestinal tract. In addition, by performing an endoscopy, the doctor has the opportunity to take tissue samples for cytological examination.
A qualified doctor who examines the patient’s body using this type of diagnosis explains to the person the maximum amount of information obtained from the results of what he saw with the help of an endoscope.
Similar articles:
Inflammation of the gastric mucosa
This pathology is accompanied by the following symptoms:
- burning pain in the stomach;
- lack of appetite;
- belching;
- nausea;
- vomit;
- flatulence;
- weight loss.
Destination purpose
— FGDS allows you to identify hypertrophy of the folds, redness and swelling of the gastric mucosa.
What is diagnostic esophagogastroduodenoscopy and indications for it?
Esophagogastroduodenoscopy is a comprehensive study of the key elements of the digestive system, when the doctor simultaneously examines the health of the esophagus, stomach, and duodenum.
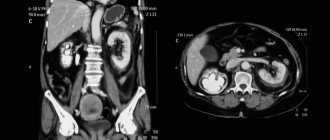
In the diagnostic process, special medical equipment is used, consisting of a multifunctional probe equipped with a miniature video camera. Thanks to this, the doctor is able to visually detect possible pathologies, ulcers, erosions, atrophic processes of the mucous membrane and foreign neoplasms (tumors of various origins, polyps, growths of viral origin).
In fact, EGDS is a type of endoscopic examination, but in just one procedure several organs of the gastrointestinal tract are examined at once. This type of diagnosis has its own indications for use and in most cases is prescribed to patients with the following pathologies:
- gastric ulcer that affects the mucous membrane with a single lesion or multiple wounds;
- gastritis and colitis of all types and nature of origin;
- hernias formed in the tissues of the esophagus;
- polypous formations that have arisen inside the duodenum, esophagus or stomach;
- eczema and papillomas of various locations;
- oncological processes of the digestive system, regardless of what stage of development they were discovered by a gastroenterologist.
Depending on the complaints received from the patient and the symptoms discovered during the examination, it is possible that the doctor will establish other indications for the use of this type of diagnosis in order to obtain the most detailed information about the health of the patient’s digestive organs.
Inflammation of the mucous membrane of the small intestine
With this disease, the patient may experience the following symptoms:
- abdominal pain;
- bloating;
- diarrhea;
- nausea;
- vomit;
- weakness.
Destination purpose
— using FGDS, the intestine is carefully examined and a biopsy is taken from the affected area for subsequent histological examination.
How is EGDS done?
The EGDS procedure is performed in a gastroenterologist’s office in a clinic or day hospital. Before the examination begins, the doctor examines the patient’s mouth and throat, after which he performs premedication: he irrigates the throat and root of the tongue with local anesthetics to reduce their sensitivity and avoid the urge to vomit during insertion of the device. After this, the patient is placed on the couch on his side.
The examination is carried out according to a single algorithm:
- A mouthpiece is inserted into the patient's oral cavity - a tab that will prevent the jaws from completely closing. In the middle of it there is a hole into which the doctor inserts a gastroscope tube.
- After inserting the tube into the oral cavity, the patient is asked to relax the larynx and throat, lower the tongue so that the device can easily penetrate the esophagus. Sometimes the doctor asks the patient to make swallowing movements. If the urge to vomit occurs, the patient is asked to breathe slowly and as deeply as possible. This technique reduces nausea.
- After inserting the tube into the esophagus, the doctor begins supplying air to expand its cavity and thoroughly examine the mucous membranes. At this moment, the patient may feel fullness, and after moving the gastroscope deeper, a kind of belching may appear.
- After examining the esophagus, the doctor gradually inserts the gastroscope tube into the stomach, and then into the duodenum. All this time he turns the tube to examine all the surfaces of the organs. At the same time, photographs are taken or video is recorded.
If necessary, during esophagogastroduodenoscopy, the doctor measures the acidity of gastric juice and the contents of the duodenum, and takes a pinch of the mucous membrane for histology.
A typical survey esophagogastroduodenoscopy lasts no more than 5 minutes. The procedure may take a little longer, during which the doctor will have to measure the acidity of the stomach. The longest diagnostic process awaits patients who require a biopsy. This study lasts up to 15-20 minutes.
Conducting studies with anesthesia during endoscopy is not widespread, since the procedure is generally painless and takes little time. The exception is children under 10 years of age. They always undergo esophagogastroduodenoscopy under sedation. This is a special type of anesthesia in which the patient is immersed in a short but deep sleep. Drugs that are used for endoscopy while the patient is asleep act more gently and have fewer side effects and contraindications.
Important! An examination under anesthesia is carried out for adult patients if they have a reduced pain threshold, an increased gag reflex, or severe mental instability.
Esophagogastroduodenoscopy shows almost any changes in the condition of the mucous membranes of the digestive tract:
- changes in the structure of the mucous membranes - erosion, stomach ulcers, erosive bulbitis and others;
- foci of inflammation, irritation of the mucous membranes of the esophagus and stomach;
- protrusions on the walls of the esophagus (diverticula);
- varicose veins of the esophagus;
- inflammatory processes on the mucous membranes - cholecystitis, bulboduodenitis, antral gastritis and others;
- changes in the functioning of valves and sphincters - reflux and their consequences;
- neoplasms - polyps, malignant tumors;
- foreign objects;
- sources of bleeding.
In addition, the doctor can assess the functional state of individual parts of the digestive tract.
Bleeding
With blood loss from the gastrointestinal tract, the patient may experience the following symptoms:
- bloody vomiting;
- feces with blood;
- general weakness;
- dizziness;
- pallor of the skin.
Destination purpose
- with the help of FGDS you can detect and stop bleeding.
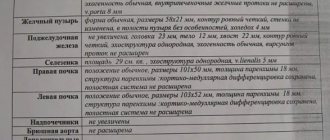
Interpretation of endoscopy results
After the esophagogastroduodenoscopy procedure is completed, the doctor views the video footage and describes all the organ segments that were studied using special medical equipment. In the document being drawn up, the doctor displays the following biological information:
- the condition of the mucous membrane, the saturation of its color;
- possible presence of foci of inflammatory etiology;
- describes detected ulcerative formations, erosions, trophic wounds, which are presented in the singular or plural;
- characterizes identified polyps, epithelial growths, papillomas or tumors that have all the signs of a malignant nature of origin;
- gives therapeutic recommendations that form the basis for further treatment regimens.
Each case of diagnostic examination is individual in nature and the clinical picture of the internal organs to be studied using the EGD method is also displayed differently. Therefore, the content of the conclusion of the transcript of the procedure is almost never repeated. Only the generally accepted plan and the above points are retained, which must be disclosed by a gastroenterologist.
Preparing for the study
Since during the procedure the doctor conducts a visual examination of the mucous membrane of the walls of the gastrointestinal tract, it is necessary to provide conditions for a full examination. To do this, it is recommended to start preparing the day before the study.
The day before the procedure
Meals should be eaten no later than 8 pm. It is not recommended to eat heavy foods: meat, potatoes, eggs, etc.
Such food takes a long time to digest, which means that by the time of the examination there will be leftover food in the stomach. This will complicate the examination, and in addition, in case of possible vomiting, you can choke on the vomit.
After dinner, you should not consume dairy products.
On the day of the examination
The examination is carried out on an empty stomach, so you should skip breakfast. Smoking is also not recommended . If there are no special instructions from your doctor, you can drink still water, but in small quantities.
As a rule, they try to schedule the procedure for the first half of the day. But if the examination must take place after lunch, then a light breakfast is acceptable. In this case, at least 8 hours must pass from breakfast to the examination.
After the procedure
You can eat food no earlier than 10 minutes later if the feeling of a lump in the throat has passed. If a biopsy was performed during the procedure, you should not eat cold or hot food on the day of the examination.
Within about half an hour after the procedure, the anesthetic substance stops working. A sore throat may persist throughout the day, as can bloating.