Main symptoms:
- Pale skin
- Abdominal pain
- Hungry pain in the stomach
- Constipation
- Heartburn
- Sour taste in mouth
- Malaise
- Belching
- Diarrhea
- Vomit
- Weakness
- Nausea
- Heaviness in the stomach
- Deterioration of general condition
Gastropathy is a pathological process of a gastroenterological nature, manifested by changes in the gastric mucosa. In most cases, gastropathy of the gastric antrum is caused by taking non-steroidal anti-inflammatory drugs, however, the influence of other pathological processes cannot be excluded.
- Etiology
- Classification
- Symptoms
- Diagnostics
- Treatment
The clinical picture does not have specific symptoms, since superficial gastropathy is a consequence of other gastroenterological diseases. A thorough diagnosis is required to make an accurate diagnosis.
Treatment is determined on an individual basis. At the initial stages, it is possible to eliminate the disease through conservative measures. Regardless of the chosen treatment tactics, a diet must be prescribed.
There is no definite prognosis, since everything will depend on the underlying factor, the timeliness of starting therapy and general health indicators. The disease has no clear restrictions on gender and age, but is more often diagnosed in women, which may be due to hormonal characteristics.
Classification
According to some authors, the disease is divided into degrees. The classification is based on the endoscopic sign of mucosal damage. It is customary to distinguish grades 1, 2 and 3 of erythematous gastropathy.
But in recent years, scientists have come to the conclusion that this classification is not entirely correct. The first degree is characterized by local redness.
But the second and third degrees, according to endoscopic signs, are already manifestations of a more severe pathology - gastritis, only in its different forms - superficial and erosive.
Prognosis for atrophic hyperplastic gastritis
Without timely detection and treatment, late diagnosis and non-compliance with doctor’s recommendations, the prognosis of the disease is unfavorable.
The transformation of this type of gastritis into stomach cancer plays a great role (transformation into oncopathology occurs in 20% of cases of the disease), the growth of polyps with their further malignancy.
It is impossible to completely recover from this pathology, but it is quite possible to stop its development and control the manifestations of atrophy and hyperplasia with drug treatment, diet and timely examination.
Important:
Follow the doctor’s recommendations, eat responsibly, do not eat coarse, fatty, spicy and salty foods, avoid alcohol and smoking.
You should not self-medicate or adjust doctor’s prescriptions. If all recommendations are followed, annual examinations are performed and the pathology does not progress, the prognosis is relatively favorable.
All persons with identified pathology are registered with a dispensary outpatient clinic and are required to undergo an annual FGDS with a biopsy in order to monitor the dynamics of their condition and the processes occurring in the stomach.
Causes of the disease
This disease is a polyetiological disease, that is, it can be caused by a variety of factors and causes. All these provoking conditions can be divided into two main groups.
1. Exogenous factors . This group includes all external influences that in one way or another can affect the development and course of the pathology. Most often these include:
- eating poorly prepared stale food. This group is formed by food toxic infections, such as: coli infections, salmonellosis, botulism, staphylococcal infections;
- Bingeing - constantly eating too much food at one time;
- systematic intake of foods that are too hot, spicy, high in fat, too hot or, conversely, cold;
- frequent inclusion of poorly digestible food ingredients in the diet;
- consumption of strong alcohol and tobacco;
- insufficient mechanical processing of food in the oral cavity - ineffective chewing. As doctors also call this phenomenon, fast food or a quick snack. The point is that thoroughly grinding a bolus of food in the mouth with teeth and wetting it with saliva has a beneficial effect on the digestive function of the stomach and stimulates the production of the required amount of digestive enzymes.
- This process of preparing food to enter the gastrointestinal tract is the most basic. If cooked foods are improperly consumed and quickly swallowed, the wall of the digestive organ can be damaged and injured, thereby causing gastropathy. Especially if this phenomenon occurs regularly.
- taking a number of pharmacological agents. Most often, this group includes those cases in which patients arbitrarily took certain types of medications without a doctor’s prescription, without taking into account their side effects and influences. Most often, the development of pathology is provoked by the intake of salicylates, non-steroidal anti-inflammatory drugs, quinine, antibacterial agents, hormonal drugs and insulin.
2. Endogenous factors . This group is formed by causes that are in the body and themselves contribute to the occurrence of the disease:
- Psycho-emotional health disorders. This group includes prolonged regular stress, panic attacks, and prolonged depression.
- Infectious processes with constant sources of infection in the body. These include pyelonephritis, tonsillitis, otitis, adnexitis, colitis and others in different organs and systems.
- Metabolic shifts. Diseases that develop in the process of hormonal changes: dyslepidemic syndrome, obesity, diabetes mellitus, gouty lesions, hyperhypothyroidism, adrenal insufficiency.
- Kidney pathology that accompanies uremic syndrome: all forms of renal failure, urolithiasis, glomerulonephritis.
- Global in area, numerous burns of various etiologies, frostbite.
- Exposure to radiation is radiation sickness.
- Traumatization of the stomach by various chemicals, especially among children.
A special type of gastropathy is erythematous gastropathy against the background of atrophy of the gastric mucosa. The thing is that these two diseases often accompany each other.
With atrophic phenomena, the protective forces of the organ are greatly weakened, so any negative effect on the wall of the organ can cause the phenomenon of gastropathy.
In the process of exposure to a pathogenic factor, the surface layer of the epithelium and the glandular component of the organ are damaged. All this entails the development of dystrophic-necrobiotic changes. If this process continues for a certain time, then the trigger for the development of the inflammatory reaction will work.
Clinical manifestation
Patients with Ménétrier's disease may present with a variety of clinical symptoms, including epigastric pain, significant weight loss, nausea, vomiting, gastrointestinal bleeding, diarrhea, and protein-losing gastroenteropathy [4,5,19,20]. In one study of 40 patients without morphological confirmation of Ménétrier's disease, the main complaints were:
- Epigastric pain - 65%
- Asthenia - 60%
- Anorexia - 45%
- Weight loss - 45%
- Edema - 38%
- Vomiting - 38%
In addition, approximately 80% of patients had hypoalbuminemia and increased intestinal protein loss. In other studies, hypoalbuminemia was present in 20-100% of patients, but its presence does not distinguish Ménétrier's disease from other causes of enlarged gastric folds other than Zollinger-Ellison syndrome [4,5,19,21,22]. Basal and stimulated gastric secretion of hydrochloric acid in Ménétrier's disease is usually reduced or normal, but varies depending on the stage of the disease [4,19,22,23]. A slight to moderate increase in serum gastrin concentrations may be present [24]. Additional clinical and laboratory findings are similar to those of other forms of protein-losing gastroenteropathies.
General symptoms of the disease
Among the symptom complexes of the described pathology, the most pronounced are the following:
- Loss of appetite. Occurs frequently, but not in all patients. It all depends on the shape and size of the lesion. Doctors say that this phenomenon occurs due to disturbances in the peristaltic function of the damaged organ.
- Stomach disorders, diarrhea syndrome. It manifests itself during changes in the processes of the secretory ability of the stomach. At the same time, the movement of chyme into the subsequent lower parts of the digestive canal is accelerated.
- Heartburn. Appears due to an increase in the secretory function of the stomach, in which insufficiency of the cardiac sphincter may develop, which leads to reverse reflux (reflux) into the esophagus of acidic stomach contents, which causes irritation of the nerve endings mainly in the distal esophagus;
- Belching. This disease is rare, most often if the provoking factor of the disease is stress. Appears when the muscle function of the esophageal sphincter is impaired.
- Nausea. It can appear due to food poisoning, exposure to poisons, damage to poorly processed and chewed food. Often precedes vomiting.
- Vomit. A common symptom of this pathology. With the help of vomiting, the stomach tries to independently remove pathological substances from the body. It is a reflex defense mechanism.
- Painful sensations in the upper floors of the abdominal cavity. Appear when overeating. As a result of overstretching of the stomach wall with food, the organ's pain receptors begin to fire. Impulses from these receptors enter the center of the brain, and the person begins to feel pain.
- Dyspnea. Feeling short of air or having trouble breathing.
- Bitter taste in the mouth;
- Feeling and sensation of excess coating on the tongue.
In addition to gastrointestinal disorders, erythematous gastropathy occurs with symptoms of changes in general condition, such as:
- weakness,
- rapid onset of fatigue, lethargy,
- periodic pain in the head together with intestinal manifestations,
- pale skin,
- pressure surges,
- decreased immune reactivity,
- sophistication of taste preferences and appetite.
Definition
The term "Ménétrier's disease" is often applied to any condition in which the size of the gastric folds is increased [3-6]. This imprecise definition leads to confusion in the literature and does not distinguish between hyperplasia (an increase in the number of cells, as occurs in Ménétrier's disease and Zollinger-Ellison syndrome) and hypertrophy (an increase in the mass of a cell or organ, as also occurs in some conditions). [7]. The best way to classify conditions associated with enlarged stomach folds is to divide them into two broad categories:
- Hyperplastic gastropathy
- Enlarged stomach folds due to other reasons
How to diagnose and detect the disease
The very first thing a doctor does with a patient is a general examination. May appear:
- paleness of the skin, visible mucous membranes (oral cavity, sclera),
- coating of the tongue from white to grayish shades;
- There may be an unpleasant odor from the oral cavity;
- the patient himself may notice increased dry mouth and constant thirst.
Then the doctor must evaluate the secretory function of the stomach using pH-metry manipulation. The secretory function at the beginning of the disease is a quantitative increase in gastric secretion and acidity (pH), then hypersecretion is replaced by inhibition of the functions of the gastric glands.
If necessary, an x-ray examination is prescribed. There are no characteristic radiological signs; a slowdown in motor and evacuation functions is detected due to hypotension, atony or spasm of the pylorus.
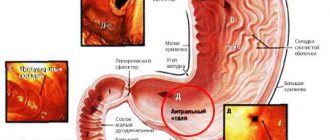
An important diagnostic method is gastroscopy. However, this method is not indicated for everyone for this pathology. If there is a suspicion that the disease is caused by mechanical damage or chemical exposure, then the procedure may further aggravate the course. Therefore, gastroscopy is performed only in the remission stage.
During the procedure, signs such as:
- redness and swelling of the mucous membrane;
- infiltration by the body’s protective cells – leukocytes;
- full-blooded vessels.
Diagnostics
A comprehensive diagnosis is required, since there is no specific clinical picture. A gastroenterologist, after a visual examination and history taking, may prescribe the following:
- general clinical and biochemical blood test;
- general urine analysis;
- general analysis of stool;
- pH-metry;
- PCR testing;
- endoscopic examination of the gastrointestinal tract;
- esophagogastroduodenoscopy;
- X-ray of the stomach with a contrast agent;
- ELISA.
At the discretion of the doctor, the diagnostic program can be supplemented with other laboratory or instrumental research methods.
Treatment of the disease
Due to the fact that erythematous gastropathy is a traumatic disease, you should follow a fasting diet for the first two days. Then a gentle diet is included in the diet: pureed and mushy food, not spicy, little salty, without excess acidity. As this happens, etiological factors are eliminated.
All manipulations and medications must be under the strict supervision of a doctor!
Once the diagnosis is made, the following procedures are necessary:
- With exogenous etiology, an important therapeutic measure is gastric lavage. This must be done in order to stop the negative impact of the damaging factor on the organ and the removal of toxic compounds. Gastric lavage is done so many times that the contents of the organ become clean without food residues or other impurities.
- If the previous medical manipulation cannot be carried out for one reason or another, then they resort to the method of artificial vomiting. This can only be done when the patient is conscious and there are no disturbances in the central nervous system. For example, in case of poisoning with toxic poisons, this should not be done under any circumstances.
- Drink plenty of fluids, replenish body fluids through infusion therapy in the form of droppers.
- If difficulties arise with washing the organ and inducing artificial vomiting, then only under the strict supervision of a doctor and according to indications, the emetic apomorphine is administered. Its independent use poses a threat to life and health.
- Adsorbents are widely used. These are medicinal active substances that remove toxic agents from the body and block their further absorption into the bloodstream. Activated carbon, polysorb.
- Laxatives are used to accelerate the removal of damaging factors from the body.
- For the first two days after diagnosis, bed rest and complete rest should be observed.
- You can drink warm, not strong tea.
Treatment of erythematous gastropathy with folk remedies
To treat this pathology, herbal remedies that have anti-inflammatory and wound-healing effects are most often used.
One of these traditional medicines is honey. It must be taken especially - one teaspoon of candied honey is placed in the mouth and dissolved until completely dissolved, gradually swallowing it. This manipulation is carried out 3 times a day.
Especially famous for the treatment of this pathology is a decoction of three herbs: oak bark - has astringent properties, chamomile flowers - anti-inflammatory effects, nettle leaves - wound healing properties.
All three dried components are mixed in equal proportions - 1 tablespoon each, pour 250 ml of boiling water, leave for 2-3 hours, strain and drink cooled after each meal.
Helicobacter pylori
Acute HP-associated gastritis can cause severe inflammation and enlargement of the folds of the stomach, which may even have an appearance similar to that of malignant diseases. In chronic HP associated gastritis, an increase in the folds of the stomach may also be observed, simulating Ménétrier's disease [30,31]. Several reports indicate the presence of enlarged gastric fundus and body folds with glandular hyperplasia, hypersecretion, and the presence or absence of hypoalbuminemia in patients without Zollinger-Ellison syndrome [19,32–34]. In the past, these cases were classified as gastritis with glandular hypertrophy [35], hypertrophic hypersecretory gastropathy [34,36], and Schindler's disease [37]. However, there are two observations indicating the role played by Helicobacter pylori in the development of this pathology:
- An examination of published micrographs of these patients showed that virtually all of them had gastritis consistent with HP infection [34].
- In one study, 18 of 32 patients with thickened gastric folds were infected with Hp [38]. Anti-Hp therapy led to normalization of the size of the gastric folds. Similar findings have been described in other reports [39,40]. It is noteworthy that in two of these reports [38,39], the term “Ménétrier's disease” was inappropriately used to refer to a condition associated with enlarged gastric folds.
Symptoms
The symptoms of atrophic hyperplastic gastritis are not specific and fit into the syndrome of gastric dyspepsia:
- decreased appetite;
- feeling of fullness in the stomach and early satiety;
- aching pain that occurs after eating and increases over time;
- belching;
- emaciation, symptoms of anemia (brittle and dry nails and hair, general weakness and decreased performance, tingling and burning sensation in the tongue);
- coating on the tongue is yellowish or whitish;
- With significant progression of the disease, constipation appears, alternating with diarrhea.