Diseases of the intestinal tract are considered one of the most common and dangerous. In the arsenal of today's medicine, there are many methods for studying the rectum and identifying its pathologies. Many examinations can help specialists detect diseases at the earliest stages. One such effective method is colonoscopy. But like some other GI studies, this is a rather unpleasant study. Therefore, doctors use sedation during intestinal colonoscopy. Read more about this in our article.
Sedation for colonoscopy
Types of colonoscopy
In medicine, there are two types of colonoscopy:
- virtual;
- using an endoscope.
A virtual colonoscopy is a test based on data that the doctor receives from a computed tomogram or nuclear magnetic resonance imaging. Read more in this article.
With this method, images of the intestine are projected in 2D or 3D form.
Experts say that colonoscopy cannot provide as much information as a full endoscopic examination. But the positive side of virtual colonoscopy is that it is painless.
The duration of the procedure is 10 – 15 minutes.
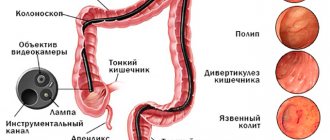
Colonoscopy using an endoscope performs a couple of functions. At the tip of the device there is a miniature camera, with the help of which the image is projected onto the monitor. This gives the doctor the opportunity to understand the condition of the internal surfaces of the intestines.
One of the main causes of constipation and diarrhea is the use of various medications.
.
To improve bowel function after taking medications, you need to drink a simple remedy
.
Is a colonoscopy done under general anesthesia?
Colonoscopy is usually performed without anesthesia. In patients who have severe pain, local anesthesia is administered (xylocaine gel, dicaine ointment). Many patients are afraid to have a colonoscopy. They are interested in whether it is possible to do a colonoscopy under anesthesia.
Doctors say that for most people this procedure does not cause pain. Due to a number of reasons, anesthesia is prohibited during intestinal colonoscopy, also in case of heart failure, severe stenosis of the aortic or mitral valves.
But there are cases when anesthesia is necessary for colonoscopy, and there are indications.
The choice is given to sedation - a method of pain relief with special medications, with the help of which the patient is put into a state of sleep.
One of the main causes of constipation or diarrhea is poor diet.
.
Therefore, to improve bowel function, you need to drink a simple drink
.
Carrying out the procedure
Colonoscopy of the intestine under anesthesia can be performed both on an outpatient basis and in an inpatient setting in a specially designated room or operating room.
Scheme for performing colonoscopy under anesthesia:
- The patient undresses from the waist down and lies on his left side with his legs pulled up to his stomach.
- Anesthesia is administered.
- An endoscope is inserted into the anus and the intestines are examined.
- If necessary, the polyp is removed or a biopsy is taken.
- At the end of the procedure, the doctor carefully removes the probe and wakes the person.
If local anesthesia was used, the patient can go home immediately after the procedure. The general condition is satisfactory, but malaise is possible.
If sedation and general anesthesia are used, the patient is under medical supervision until he fully awakens.
Preparing for the procedure with sedation
The effectiveness of the study depends on proper preparation. Preparation for the procedure should begin a couple of days before the appointment.
We also wrote about what preparation for intestinal colonoscopy includes.
Diet
The essence of the diet is to prepare the colon for the procedure. The patient needs to eat light, refined foods. Before the procedure you need to drink water.
Colon lavage
To reduce discomfort during colonoscopy, doctors prescribe an intestinal antispasmodic. In private clinics in Moscow, St. Petersburg, Yekaterinburg, Novosibirsk, Yaroslavl, they offer computed tomography of the intestine for colonoscopy.
This procedure shows all pathologies and changes in the intestines.
Compared to colonoscopy, computed tomography differs in that:
- can detect malignant tumors in the early stages of development;
- there are no complications;
- The procedure is painless.
But there are cases when you need to do a colonoscopy, because computed tomography also has disadvantages:
- the color of the mucous membrane cannot be assessed;
- small formations are not visible;
- You can't take a biopsy.
Contraindications to colonoscopy
When FCS is prescribed, you should consult your doctor about contraindications and possible complications after the procedure.
Although the method is considered completely safe, it is necessary to consider whether the process can be carried out if the patient has certain ailments.
Colonoscopy: contraindications for the procedure are shown in the table:
| Contraindications | |
| Absolute – analysis excluded | Relative – possible, but not advisable |
| Peritonitis - severe form, surgery required | Bleeding from the anus |
| Severe degrees of pulmonary and heart failure, with circulatory disorders | The general condition of the patient is bed rest, severe, impossibility of administering anesthesia |
| Myocardial infarction - acute, possibly fatal | Insufficient blood clotting - any mechanical damage can cause bleeding |
| Perforation of the walls - activates severe bleeding | Poor preparation for the procedure – failure to follow recommendations |
| Ischemic or ulcerative colitis - likelihood of perforation | Recent abdominal surgery |
| Pregnancy - possible premature birth | Hernias (inguinal, umbilical) - after removal surgery |
Also, a separate type of contraindication is the patient’s state of shock.
A person should calm down and take medications to neutralize anxiety. Otherwise, muscle spasm occurs and the examination process is not possible.
How to do a colonoscopy under general anesthesia
Regardless of whether the doctor said that anesthesia is needed or not, the procedure is the same.
During the procedure, the patient lies on his side, with his legs pulled up to his chin. The colonoscope is inserted into the intestines into the anus. If the procedure is done without anesthesia, the colonoscope must be treated with a special agent, which reduces pain.
Thus, the doctor examines all parts of the intestine.
Before starting a colonoscopy, the intestine needs to be slightly inflated by pumping air inside. This is necessary to straighten the walls of the organ and facilitate the process.
To examine each wall of the intestine, the doctor gradually moves the colonoscope deeper into the intestine. If polyps are found, the doctor can remove them immediately using a snare that is inserted through the colonoscope.
If any neoplasms are fried during the procedure, the doctor performs a biopsy - that is, taking part of the material for analysis to determine how dangerous they are for the patient.
This must also be done using a special instrument that can be seen through a colonoscope.
Video
Polyp removal
Doctors carefully examine the entire intestinal area, then carefully pull the colonoscope out of the anus.
How long a colonoscopy will take depends on how many polyps and other growths are found. On average, the procedure will take no more than 30 minutes.
If the procedure was performed under anesthesia, then at the end the patient will feel a little weakness and possibly a headache.
In some situations, the patient feels a feeling of abdominal distension. This is a situation where the air has not been completely removed from the organ. If polyps were removed, the patient will feel pain in the abdomen, but it can be easily neutralized with the help of analgesics.
In rare cases, gastroscopy can be performed on the same day as colonoscopy. This type of research is carried out very quickly, although there are unpleasant sensations. In total, gastroscopy lasts 5–7 minutes. Read how to prepare for gastroscopy here.
Possible complications
Despite the fact that anesthesia during a colonoscopy helps the patient to endure the procedure much easier, there are still a number of risks.
Complications may occur:
- nausea;
- increased body temperature;
- bloody discharge from the anus;
- abdominal pain;
- allergic reaction;
- difficulty breathing or stopping during general anesthesia;
- intestinal perforation is a pathological condition that develops against the background of an aggressive effect on the intestinal wall;
- infectious processes;
- splenic rupture;
- Sepsis is a serious infectious disease characterized by high mortality.
Some of the complications occur extremely rarely and directly depend on the experience and length of service of the doctors who conduct the study.
In any case, if any undesirable symptoms occur, you must definitely contact your doctor with complaints.
Is it dangerous
Many patients are interested in whether general anesthesia is dangerous and whether anesthesia has consequences. General anesthesia carries certain risks for the patient, but modern medicine and an experienced doctor can significantly reduce them. Especially if the preparation of the procedure is under the guidance of a doctor.
There are no very dangerous consequences of anesthesia. The rumor that “anesthesia affects memory and psyche” is associated with the history of anesthesiology, when a dangerous anesthetic was used. Modern medicine does not have these side effects.
| Ukraine | Price, UAH. | Russia | price, rub. |
| Kyiv | 1020 | Moscow | 9843 |
| Kharkiv | 800 | Saint Petersburg | 4294 |
| Odessa | 900 | Kaliningrad | 6547 |
Reviews
Lack of fluid in the diet is one of the main causes of constipation. To get rid of it in 3 days, you need to drink a simple remedy every day.
I did this procedure a year ago. 4 polyps were removed. I came out of anesthesia after half an hour. There was a slight headache.
It took me a long time to get ready for a colonoscopy. I read a lot of forums, but still decided. I did it without anesthesia. Yes, it was an unpleasant procedure, but I didn’t feel any pain. I recommend it.
Practicing gastroenterologist. Work experience: 9 years in a private clinic. If you haven't found the answer to your question, ask the author!
✓ Article checked by doctor
Diseases of the intestinal tract are considered one of the most common and dangerous. In the arsenal of today's medicine, there are many methods for studying the rectum and identifying its pathologies. Many examinations can help specialists detect diseases at the earliest stages. One such effective method is colonoscopy. But like some other GI studies, this is a rather unpleasant study. Therefore, doctors use sedation during intestinal colonoscopy. Read more about this in our article.
Sedation for colonoscopy
What is a colonoscopy?
This is an endoscopic method for diagnosing the condition of the internal walls and surface of the colon using a special device - a colonoscope.
Colonoscope (endoscope) is a probe that easily moves through the rectum without injuring it due to its bendable design.
A tiny video camera is installed at the end of the device, with which the diagnostician can see the condition of the intestines on a special screen. The length of the colonoscope does not exceed 2 meters, this is quite enough to examine the cecum, sigmoid, colon and rectum. In this case, the small intestine is not affected. The procedure is carried out by a proctologist and an assisting nurse.
Note! Colonoscopy is needed not only to detect pathologies, but also to take tissue samples for biopsy, stop intestinal bleeding (thermocoagulation), restore intestinal patency (if narrowing occurs), eliminate polyps or remove foreign objects.
What is a colonoscopy?
During the examination, the endoscopist uses a flexible colonoscope hose, which is equipped with lighting and optical systems. Modern devices have cameras with which the doctor takes pictures of the most “suspicious” areas of the mucous membrane of the digestive tract. These images can be saved on digital media and, if necessary, used for a more detailed study or analysis of the dynamics of the disease. The patient is placed on his left side, legs bent at the knees, and a colonoscope is carefully inserted into the anus. Gradually, the doctor uses the device to pump air into the intestinal cavity, straightening the folds of the mucous membrane. This helps to move forward and examine areas of the intestine more carefully (see video). Colonoscopy has been used for a long time as the most informative diagnostic method, however, there was no previous experience of using it under anesthesia. For this reason, colonoscopy left behind an unpleasant sensation, since when air was pumped in, the patient experienced quite noticeable pain.
Today it has become possible to carry out the procedure against the background of pain relief in different ways:
- local anesthesia;
- sedation;
- general anesthesia.
Local anesthesia is performed by applying an anesthetic substance to the tip of the colonoscope. It does not completely eliminate unpleasant sensations. The pain decreases, but sensitivity remains.
The best option for the patient is general anesthesia. The patient falls asleep, does not feel anything, and there are no bad memories of the procedure, since his consciousness is completely turned off. The examination under general anesthesia guarantees complete comfort for both the patient and the doctor. Unfortunately, the method of such anesthesia has some adverse consequences, sometimes complications, so the procedure is carried out in the operating room, under the supervision of doctors, including an anesthesiologist, so that safety is maximized.
Another method to ensure patient comfort is sedation. It causes a state similar to sleep, when all sensations are dulled, the patient does not experience anxiety and fear. The drugs used are propofol and midazolam. Both methods have both disadvantages and advantages. Thus, midazolam completely eliminates the appearance of unpleasant sensations in the patient, but the period of awakening after its use is longer. Propofol has completely opposite effects: the subject may retain memories, but awakening will be faster.
Who needs the procedure?
People over 50 years of age who have no family history of colon cancer are recommended to undergo this procedure every 5-7 years. Those who have a bad hereditary history of oncology need to have a colonoscopy once a year. This is necessary in order to identify the possible occurrence of the disease in time.
As a rule, specialists can prescribe this examination to a patient if:
- intestinal bleeding;
- polyps;
- already identified colon cancer (for biopsy);
- the presence of a constant temperature (37-37.5 °C) for a long time without signs of a cold;
- sudden weight loss for no apparent reason;
- frequent diarrhea or chronic constipation;
- low hemoglobin;
- presence of Crohn's disease;
- nonspecific ulcerative colitis.
The study helps to find out the location and degree of formation of the pathology
Important! Colonoscopy is contraindicated in pregnancy, allergies, ulcerative colitis, pulmonary and heart failure, peritonitis, blood clotting pathologies and infectious diseases!
Carrying out colonoscopy of the intestines
Colonoscopy is considered the main instrumental diagnostic measure for female and male patients. The procedure is carried out using the classical and capsule method. A classic examination involves inserting a flexible fibercolonoscope instrument into the anorectal canal.
The procedure is prescribed for:
- taking a biopsy;
- removing a foreign object;
- restoration of intestinal patency;
- elimination of neoplasms;
- preventing blood loss.
Most often, colonoscopy is performed while you sleep, in other words, under general anesthesia. How long does a diagnostic colonoscopy take? On average, the procedure takes from 25 to 50 minutes. To conduct a research event, high-quality preparation is necessary. To do this, proctologists recommend thoroughly cleansing the intestines with enemas or laxatives. If a person often experiences constipation, he is additionally prescribed to drink castor oil; enemas are necessary for rare bowel movements. A special Esmarch circle device is used as an enema.
A slag-free diet is prescribed three days before a diagnostic colonoscopy. You cannot eat raw vegetables or fruits, herbs, smoked, salted, pickled foods, or black bread. Chocolate, sunflower seeds, coffee, milk, flour, sweets, and nuts are excluded. In the evening before the appointment of the session, proctologists recommend cleansing yourself of toxins and fecal accumulations with the medications Lavacol, Fortrans or Endofalk.
Organ testing begins with the insertion of a bendable probe with a microcamera through the anorectal canal, which causes some inconvenience and discomfort for the patient. To relieve psychological stress, patients are recommended to buy special panties for colonoscopy. The examination begins with the rectum, moving step by step through all areas and parts of the organ. To improve visibility, air is pumped into the patient’s intestines through special equipment (straightening folds and pockets).
If the diagnosis is carried out correctly, people do not experience complications, however, in some cases, patients came with complaints after the session about:
- blood loss;
- intestinal perforation;
- bloating;
- fever;
- pain.
If after examination the condition worsens, urgent medical attention is needed. When there are no diseases in the organ, the mucous tissues have a pinkish color with a shine, without ulcers, tumors, or protrusions. The pattern of blood vessels is smooth, there are no compactions, polyps, pus, fibrin deposits or necrotic masses. In case of peritonitis, severe respiratory and heart diseases, heart attack, ischemic stroke, the study is not carried out.
Preparation before the procedure
Any serious medical examination requires mandatory preparation for it. The patient will need to prepare for a colonoscopy in advance - two to four days before the scheduled examination. Initially, strict adherence to the diet will be required. The following should be excluded from the diet:
- milk (cow), carbonated drinks, coffee, alcohol and strong tea;
- pasta, wheat porridge, bakery products;
- vegetables, fruits, berries, herbs;
- nuts, beans, peas;
- products containing dyes, flavor enhancers;
- fatty meat products, smoked meats, sausages.
Thus, these days you need to eat boiled turkey meat, steamed fish, low-fat broths, homemade yogurt, and kefir.
People suffering from constipation are recommended to give themselves enemas during this period to better cleanse their intestines.
Important! The last meal is allowed no later than 12 hours before the colonoscopy.
For the remaining time, you will have to limit yourself to clean water or green tea. On the day the procedure is to be performed, the patient must not take any food or liquid as the stomach must remain empty (2 hours before the procedure).
The remaining preparatory activities will be carried out by doctors at the medical institution. As a rule, this is an enema or bowel cleansing with the help of medications that stimulate the process of defecation (Fortrans, Lavacol). Their dosage should be prescribed by the attending physician, since it is calculated based on the weight and condition of each individual patient.
Video - Recommendations from a specialist in preparing for a colonoscopy
How to prepare for the procedure?
The key to highly accurate, fast and effective fibrocolonoscopy is a clean, empty intestine.
Preparation takes place in three stages:
- Preliminary preparation.
- Slag-free diet.
- Purgation.
Preliminary preparation
Several days (at least 5) before the procedure, patients should not use antidiarrheal drugs, dietary supplements with fiber, or supplements with iron.
Diet
Before fibrocolonoscopy, you need to adhere to a slag-free diet. 2-3 days before the procedure, you should not eat foods rich in fiber (vegetables, fruits, greens).
It is necessary to exclude foods that are poorly digested (cereals, nuts, pasta).
Purgation
The day before the colonoscopy, it is necessary to thoroughly cleanse the intestines.
Laxatives and cleansing enemas are taken, which are prescribed by the attending physician.
Before the procedure, you should not eat for 17 hours. You can only drink a little tea.
Preparation for fibrocolonoscopy is very important. If you do not follow and adhere to the doctor's recommendations, this may result in distorted results and the procedure will need to be repeated.
How is a colonoscopy performed?
Many people are afraid of the upcoming procedure precisely because they have no idea what exactly will happen to them in the diagnostic room. To get ready to undergo an examination of the rectum using an endoscope, it is best to have an idea of how it is carried out.
So, the step-by-step progress of the examination can be described as follows:
- The patient lies on his left side on the couch, with his knees drawn up.
- The specialist gives the patient anesthesia (general anesthesia, sedation, anesthetic gel, depending on the patient’s condition and wishes).
- Once the anesthesia has taken effect, the doctor inserts a probe into the rectum.
- Depending on the purpose of the study, a colonoscopy can last about 15 minutes until the doctor completes all manipulations.
- The diagnostician carefully moves the probe out.
After the procedure, a person may feel severe bloating and distension of the abdomen. Activated carbon is used to eliminate it.
Attention! Examinations using anesthesia should only be carried out in the presence of an anesthesiologist!
Anesthesia options
The endoscope examination itself is quite unpleasant and can sometimes cause pain to the patient. Therefore, in some cases, specialists choose one of the options for pain relief or anesthesia.
Table 1. Types of anesthesia for colonoscopy
| Name | Description |
| General anesthesia | The patient is put into deep medicated sleep, which continues throughout the entire procedure. After the completion of the colonoscopy and the cessation of the effects of the drugs, the person gradually comes to his senses, but he will not remember the procedure itself, nor will he feel the consequences. |
| Local anesthesia | The anesthetic is applied directly to the device. Often this is not enough: the patient’s pain threshold increases, but the discomfort from moving the colonoscope will not disappear anywhere |
| Sedation | A variant of superficial medicinal sleep, in which a person is conscious, but under the influence of sedatives does not feel the diagnostician’s manipulations (borderline state) |
Advancing the endoscope (especially in the presence of tumors) can be quite painful, which is why doctors recommend putting a person into medicated sleep
Types of pain relief
The use of a specific method of pain relief during intestinal colonoscopy is determined by the person’s medical history and the expected pathology.
The doctor decides which anesthesia to choose.
There are three main types of anesthesia for colonoscopy:
- local anesthesia;
- sedation;
- general anesthesia.
Local anesthesia
In order to reduce the sensitivity of the nerve endings, a local anesthetic is applied to the device. But this type of anesthesia cannot completely relieve pain; moreover, a feeling of fear and anxiety remains.
To increase the comfort of the procedure, antispasmodics and sedatives are prescribed at the preparation stage.
Sedation
Sedation during colonoscopy is carried out by using medications that induce drug-induced sleep in a person (Propofol, Metazolam).
The sleep is shallow, the person does not feel anything, but hears everything and responds to the doctor’s requests (for example, to change position). Under sedation, a person breathes on their own.
Related articles:
Preparing for sigmoidoscopy and how to go through the procedure CT scan of the intestines or colonoscopy, which is better - comparison Stool analysis for dysbacteriosis: preparation and delivery, interpretation Colonoscopy of the intestine: preparation and conduct, contraindications Sigmoidoscopy and colonoscopy, what is the difference: pros and cons
When using Propofol, the patient remembers everything and awakens quickly.
Metazolam is a stronger drug that “erases” all information about the procedure from a person’s memory. The recovery from half-sleep takes longer.
Colonoscopy with sedation has its drawbacks - allergic reactions of varying severity may occur (from urticaria to anaphylactic shock).
Side effects - vomiting, nausea. In order to provide timely assistance in the event of any adverse reactions, an anesthesiologist is located next to the patient.
For children under 12 years of age, the best option is a colonoscopy while sleeping.
General anesthesia
Under general anesthesia, a person is in a deep sleep stage, does not hear or feel anything.
Contraindications:
- purulent skin lesions;
- rickets;
- acute respiratory tract diseases;
- elevated body temperature of unknown origin;
- light weight.
The disadvantage of general anesthesia is that this type of anesthesia is more likely to cause complications than others.
Sedation for colonoscopy: pros and cons
So, during general anesthesia, a person’s consciousness is completely switched off; accordingly, this requires a longer recovery of the body after its effect ends. Based on the obvious differences, we can talk about the advantage of the sedation method over local anesthesia and putting the patient into a state of medicated deep sleep.
Attention! According to doctors, in the absence of special indications, preference is given to the sedation method, as it is more gentle and less risky.
Why is it so important that the patient is not only pain-free, but also comfortable? The thing is that quite often the doctor has to waste time on persuasion and requests to relax instead of carefully and efficiently conducting the examination. This is especially true for children: young patients are not only afraid, but may also refuse the procedure altogether. In this case, sedation is the best solution to the problem.
What drugs are used for sedation?
There are various sedatives, but, as a rule, specialists during colonoscopy prefer to use drugs such as Propofol and Midazolam.
Sedative "Propofol"
- "Propofol." It relaxes, has a quick and short-term effect, so awakening in this case is easier. Does not affect memory; the patient retains some memories of the procedure. It is highly tolerable and has a slight antiemetic effect. Disadvantages: lacks antiallergic effect, rather high cost.
- "Midazolam." Promotes short-term memory loss: the patient will not remember what happened during the study. Among specialists, it is considered the most controlled drug and has an anticonvulsant effect. Disadvantage: for the patient, waking up after Midazolam is more difficult due to the specific nature of the drug’s action.
Which method is preferable? The issue is controversial among doctors, and the choice in favor of one drug or another is made based on the characteristics of the patient’s condition and the personal experience of the anesthesiologist himself.
In what cases is sedation acceptable?
The decision about whether gastroscopy can be done during medicinal sleep or not is made by the doctor. As a rule, an emergency procedure is not done with sedation, since there is no time to select and administer the drug. Also, the doctor does not have a diagnosis or additional examinations that are necessary to understand whether sedation is dangerous for the patient.
In normal cases it is necessary:
- a person’s desire to undergo gastroscopy during medicated sleep;
- availability of appropriate equipment and anesthesiologist;
- availability of results of a general blood test, fluorography and other specific examinations.
If we talk about the medical indications of gastroscopy under anesthesia or sedation, it is necessary to mention such as: a strong gag reflex in patients, which complicates the doctor’s task to conduct an examination, as well as some inflammatory processes of the gastrointestinal tract, which cause problems with swallowing.
Disadvantages of Traditional Surveys
Classical FGDS is carried out on an outpatient basis. And after them, the patient can leave the walls of the clinic in the near future. Surprisingly, for most, gastroendoscopy is the most uncomfortable.
This is explained by the fact that when a special device is inserted - an endoscope - a person develops a very strong gag reflex. Saliva accumulates in the mouth, which he cannot swallow, so the senses send signals to the brain that the foreign object must be urgently removed.
Often, for this reason, many people experience difficulty breathing (due to panic). If the procedure affects adults in this way, it is difficult to imagine how it affects children. In some cases, informative research has led to mental disorders in young patients. That is why gastroscopy and colonoscopy during sleep are primarily recommended for children. The main thing is that the child must be at least 7 years old.
Endoscopy with sedation is performed for children over 7 years of age if gastrointestinal diseases are suspected. A competent specialist will determine the age-appropriate dose of the drug and will monitor the condition of the little patient throughout the procedure.
Alternative colonoscopy methods
The upcoming colonoscopy procedure is always scary for patients. It must be said, not in vain, because although this is not surgical, it is still an invasion of the human body. Also, some patients are afraid of being put into a state of medicated sleep. In this regard, the question often arises: is there an alternative to this type of examination, which includes a lesser degree of drug and surgical intervention?
In the arsenal of modern medicine there are studies that are not inferior in information content to colonoscopy. These are magnetic resonance imaging (MRI) of the intestine and capsule endoscopy.
- MRI. Such an examination does not cause any particular harm to the body. A special device (tomograph) records all changes in the rectum and takes three-dimensional pictures, as if recreating a model of the human intestinal tract. Doctors call MRI virtual colonoscopy. In this model of the intestine, all pathologies are clearly visible, and the patient is freed from feelings of discomfort and fear. However, MRI has a significant drawback: this method does not allow specialists to see tumors whose size is less than 10 mm. That is why magnetic resonance imaging can only be used as a means of obtaining a preliminary diagnosis.
- Capsule endoscopy. A new and high-quality method, an excellent alternative to colonoscopy. For this examination, a special capsule with a camera is used. It has many advantages: painlessness, safety, comfort, information content. The capsule is eliminated from the body naturally after 3-4 hours, after which the diagnostician deciphers the information recorded on it. However, capsule endoscopy is a rather expensive study. In addition, it is not carried out in every clinic.
Despite all the pros and cons, these two methods have a significant drawback: unlike colonoscopy, they are only informative, depriving specialists of the opportunity to carry out therapeutic manipulations.
Methods for diagnosing parts of the gastrointestinal tract
So, colonoscopy is an effective method for diagnosing pathologies of the intestinal tract, allowing you to accurately determine its condition, as well as remove polyps and obstructions without surgical intervention. Using an endoscope, the doctor can easily take material for histological examination. In order for the examination to be successful and as painless as possible, specialists resort to anesthesia, the preferred type of which is sedation.
Types of anesthesia for endoscopic colonoscopy
The anesthesiologist-resuscitator decides what type of anesthesia is necessary and suitable for a particular patient. To do this, he conducts an interview and gets acquainted with the patient’s chart. Based on this, one of the following types of anesthesia used for colonoscopy is selected.
Sedation
The drugs are administered intravenously. The patient falls into a state of superficial sleep. The resulting mental relaxation allows the procedure to be carried out without traumatic consequences and without pain. Sedation is the best and most often prescribed type of anesthesia for colonoscopy, since the patient is in a state that allows him to respond to the commands of the diagnostician. If during the examination such anesthesia is not enough, the anesthesiologist can increase the dose of the drug and transfer the subject to general anesthesia.
For sedation, the patient is administered a drug that has a hypnotic effect.
Intravenous anesthesia
The subject is immediately put into a state of deep sleep with the help of an intravenous injection, for example, propofol or diprivan. But, nevertheless, general anesthesia for colonoscopy is not recommended - the risk of complications is higher than the benefits of its use.
Inhalation anesthesia
Mask anesthesia using inhalation of volatile liquids or gas is the best choice for putting children, older patients, as well as patients with certain types of pathologies of the respiratory and cardiovascular systems into sleep. An important factor in choosing this type of anesthesia is that modern inhalational anesthetics have almost no harmful effects and are quickly eliminated from the body by the lungs and liver.
Use of gaseous general anesthetics
Absolutely everyone who is scheduled to undergo a colonoscopy should take a sleeping pill or a regular sedative the night before.
For patients awaiting any type of anesthesia, Seduxen or Relanium is prescribed. You should start taking the pills 36-24 hours before the examination.
If the patient has a low pain threshold, or there is an indication from the proctologist for individual indications, then 40 minutes before the colonoscopy the anesthesiologist will give an anesthetic injection of 0.5 ml of atropine (0.1%).
Reviews about the procedure
Patients who have had to undergo a colonoscopy under sedation note that the use of anesthesia during this examination is a justified measure. If you have a history of any pathologies, you cannot do without anesthesia, because neoplasms make the procedure very painful. The subjects say that sedation made the procedure comfortable and unnoticeable. The state under the influence of sedatives was such that they felt almost nothing, while some even characterized their feelings as “a state of happiness and peace.”
Anesthesia for colonoscopy
Despite the small size of the apparatus with which the procedure is performed, colonoscopy does not provide a pleasant sensation. In order to reduce pain symptoms and calm the patient, colonoscopy is performed under general anesthesia. The use of anesthesia is mandatory in the following cases:
- childhood - even mild pain and the presence of doctors in white coats can affect the psychological state of the child,
- adhesions on the intestines,
- low pain thresholds – even the sensation of mild pain can cause shock or fainting,
- patients who experience destructive processes in the intestines,
- Crohn's disease.
Painkillers are selected taking into account the patient's sensitivity to anesthetics. Many may be contraindicated for health reasons. Doctors recommend using anesthesia. Since discomfort and pain can be accompanied both during the procedure and after it. It is also difficult to predict the body’s response to the procedure and whether the colonoscopy will be painless.
What are the benefits of colonoscopy under sedation?
Before we talk about the features of this method, let's understand what sedation is during colonoscopy, as well as during other medical procedures. Sedation is a method that allows the patient to relax and calm down while being conscious. Why is it important? If a doctor performs any unpleasant procedure, he is often, willy-nilly, faced with a situation where he has to persuade the patient to relax and listen to instructions. This takes a fairly large amount of time, which could have been spent on high-quality and scrupulous implementation of the study. If it comes to children, then, in addition to tears and persuasion, there may be a complete refusal to perform the necessary procedure, and it also happens that the little person begins to have the so-called “fear of the white coat,” which means that problems may arise in the future at absolutely any visit to the doctor. This is where sedation comes to the rescue.
When a minimum dose of the drug is administered, a state of absolute calm and relaxation is achieved. In some cases, when using intravenous sedation, a colonoscopy, or any other unpleasant examination, is completely erased from the patient’s memory, and the effect of amenesia is achieved. In other cases, with the use of inhalational sedation, relaxation simply sets in. By the way, this is the method that is usually used in children.
Indications and contraindications
Indications
- The indication for sedation during colonoscopy is the patient's childhood.
- The presence of adhesions in the intestines. This makes it difficult to conduct research and aggravates discomfort.
- Strictures of the rectum and anus
- Those cases when you need to relax the abdominal cavity
- Low pain threshold
As a rule, the reasons for a colonoscopy examination are diseases and formations in the large intestine, which can cause additional discomfort during the procedure. Will, for example, sedation during a colonoscopy help with dolichosigma? Undoubtedly. Moreover, if necessary, the tube used for the examination is treated with a local anesthetic.
Contraindications
Contraindications to sedation during colonoscopy are:
- Severe form of somatic diseases
- Consumption of alcohol and drugs the day before
- Risk of developing an allergic reaction to medications used
- Any cold that results in nasal congestion
- Epilepsy
Contraindications
Like any other procedure, colonoscopy has some contraindications:
- severe heart or pulmonary failure;
- third stage hypertension - the most severe stage of hypertension, in which constantly elevated blood pressure is observed (above 180/110);
- ulcerative colitis in severe form - a pathology that affects the mucous membrane of the colon;
- peritonitis - bacterial or aseptic inflammatory process of the abdominal cavity;
- adhesive intestinal disease in the acute stage is a pathological condition that is caused by the proliferation of adhesions in the abdominal cavity;
- stroke is an acute cerebrovascular accident in which the blood supply to a certain area of the brain is disrupted or completely stopped;
- pregnancy.
There are conditions in which the doctor evaluates the benefit-harm ratio, such as: various diseases of the anal area, the early period after colon surgery, internal hernias.
Reviews about colonoscopy under sedation
Anna , 42 years old
“The gastroenterologist sent me for a colonoscopy with suspected colitis. I can’t express how afraid I was; on the day of the study I was simply shaking. But everything went very smoothly, they let me breathe into the mask, maybe because of this, or maybe because the specialist was good, I didn’t feel anything at all. I just didn’t think about anything, I felt as if I was about to fall asleep, even somehow cozy. I advise you to undergo this study with pain medication; I had sedation.”
Nikolay , 38 years old
“Colonoscopy is generally an unpleasant procedure, and with a history of the disease it’s generally a hell of a pain. I know firsthand, I somehow went through this study without pain relief or anesthesia. I didn’t want to repeat the experience, so I chose a clinic in advance where it was possible to undergo a colonoscopy with sedation. Heaven and earth, of course. They do something to you, but you don’t care at all.”
Svetlana , 56 years old
“I was very afraid of the upcoming study. I’m generally afraid of medical procedures, I’m shaking all over in the doctor’s office, but here it is... I discussed everything with the doctor in advance, he suggested deep sedation. As a result, before the procedure, they injected me with medicine into a vein, and the condition was almost like during anesthesia, I don’t remember anything, so, one might say, my colonoscopy took place without my participation!”
.If you have experience with such a procedure, you can share it on our website. In addition, you can ask a question online to a qualified anesthesiologist.
I created this project to tell you in simple language about anesthesia and anesthesia. If you received an answer to your question and the site was useful to you, I will be glad to receive support; it will help further develop the project and compensate for the costs of its maintenance.