What is obstructive jaundice and its causes?
The hepatobiliary tract is a system that includes several organs: liver, bile ducts, gallbladder. Inside the liver, pigments and acids are secreted, which mix with water to form bile. This substance subsequently enters the bladder through the ducts, and from there into the intestines, where it takes part in digestion.
With obstructive jaundice, bile is not removed from the liver. This is caused by pathologies in which the patency of the biliary tract is impaired. As a result, the substance stagnates in the liver.
One of the functions of bile is to remove excess bilirubin from the liver. As part of this substance, bilirubin passes through the intestines and subsequently leaves it with feces. If the outflow is impaired, cholestasis develops - stagnation of bile in the liver. This inevitably leads to an increase in the level of bilirubin, which, penetrating into the blood, causes jaundice.
Provoking factors:
- Cholecystitis
- Pancreatitis
- Hepatitis
- Cirrhosis
- Tumor neoplasms (oncology, cysts, polyps)
- Parasitic infestation
- Inflammation of the lymph nodes in the area of the bile ducts
The mechanism of development of pathology is complex. In most cases, it is associated with an ongoing inflammatory disease. Due to inflammation, edema develops, affecting the patency of the bile ducts. As a result, stagnation occurs.
This is interesting: Pathological jaundice in newborns: causes, symptoms, treatment and consequences
How is the drainage procedure carried out?
Drainage of the common bile duct has its own indications and contraindications. So, start draining if necessary:
- Remove infected and stagnant fluid from the liver and passages.
- Eliminate narrowing of the lumen of the common bile duct and restore the passage of bile to other organs.
- Rinse the gallbladder and its passages with antiseptics or antibiotics.
- To avoid scar formation at the surgical site in the gastrointestinal tract.
- To prevent the formation of fistulas after surgery on the duct.
- To drain fluid from the liver to clean the bladder cavity.
The primary indications for surgical intervention are such pathologies and diseases of the gallbladder as:
- Gallstone disease - surgical intervention allows you to expand the lumen of the duct, which facilitates the passage of the stone. It is important to understand that after surgery to remove the gallbladder, drainage is not installed, but deep suturing of the ducts is performed.
- Cholecystitis in the acute stage - here intervention is indicated when the inflammatory process interferes with the drainage of fluid and its stagnation and infection occur.
- Obstructive jaundice - intervention is necessary to remove excess bilirubin and the outflow of enzymes from the liver.
- Tumors are the main cause of blocked passages.
- Pancreatitis - dilation of the ducts is indicated when swelling of the head of the pancreas occurs, which interferes with the flow of bile into the duodenum.
- Cholangitis and cysts on the ducts.
- An anomaly in the development of the gallbladder, which leads to congenital blockage of the ducts.
Also, expansion of the bile ducts can be carried out if it is necessary to introduce medications into the bile ducts, including antibacterial and antiseptics, and flush organs in order to improve the condition of the bile ducts.
So, installing drainage is possible if a person does not have:
- Blood clotting disorders.
- Accumulation of fluid in the peritoneum and severe stage of liver failure.
- Oncological process in the stage of metastasis.
- The presence of tumor-like formations along the path of drainage installation.
- Pregnancy in late gestation.
- Obesity.
- Cardiac and respiratory disorders.
These contraindications must be observed, since performing the procedure in their presence can lead to the development of complications such as infections, bleeding and insufficient effectiveness of the procedure.
Obstructive jaundice does not always require drainage. Depending on how much fluid is excreted by the patient’s organ and the person’s condition, specialists may resort to conservative treatment of the pathology. If complications develop or the situation worsens, doctors decide whether surgery is necessary.
The main indications for drainage in obstructive jaundice are:
- Damage to the common duct.
- Pancreatitis and cholecystitis in the acute stage.
- Purulent processes in the gallbladder.
- Tumors.
- Stone formation.
Drainage of the bile ducts in obstructive jaundice is indicated when there is a violation of the outflow of fluid from the organ, with the accumulation of a large amount of bilirubin in the human blood.
During the procedure, it is important to monitor the patient’s condition to prevent the catheter from becoming dislodged or damaged - this can lead to serious complications, leading to irreversible consequences and death of the patient.
Surgery does not affect the process of bile formation. Even if the gallbladder is removed, it continues to be produced by liver cells. Only now the secretion is not retained in the gallbladder, but goes directly into the duodenum. In the first time after cholecystectomy, until the liver adapts and it begins to synthesize a limited volume of bile, the person will experience symptoms of digestive disorders (loose stools, flatulence, nausea).
If the bladder is cut out, the anatomy and physiology of the entire digestive tract changes:
- changes in the structure of the pancreas - detected on ultrasound as increased echogenicity;
- the pancreas produces more trypsin enzyme and less lipase;
- pressure inside the stomach and duodenal space increases;
- the outflow of pancreatic juice is disrupted;
- the number of Helicobacter pylori on the gastric mucosa increases;
- dilation of the hepatic and bile ducts (up to 10 mm according to ultrasound);
- the concentration of bile acids changes;
- the tone of the sphincter of Oddi is impaired.
The uncontrolled outflow of bile into the duodenum and an imbalance of its components leads to impaired digestion and absorption of fatty compounds. That is why the antimicrobial properties of the secretion deteriorate, which entails an increase in the numerical value of bacteria on the mucous membrane of the duodenum, disruption of the intestinal microflora, and a deterioration in the cyclic circulation of bile acids in the digestive tract.
Despite the fact that the gallbladder is not a vital organ, its absence leads to serious changes in the physiology of all components of the digestive tract. Experts from foreign and domestic medicine came to these conclusions, based on the results of many years of research, which are regularly published in articles on a reputable medical website.
If the gallbladder is removed, the most common consequence is dysfunction of the sphincter of Oddi (this is the second name for postcholecystectomy syndrome). It occurs in 40% of patients and can develop:
- according to hypertonicity - the closing muscle is always in tension;
- by hypotonicity - when the sphincter is constantly relaxed.
The problems are caused by the absence of the gallbladder, which simulated the work of the sphincter of the bile ducts by transmitting a signal in the form of nerve impulses and stimulating the production of cholecystokinin. Lack of communication with the gallbladder causes incoordination of the sphincter of Oddi, which can lead to the following symptoms:
- pain in the area of the removed bladder;
- heaviness and discomfort in the stomach;
- nausea, vomiting;
- heartburn, flatulence;
- belching, diarrhea.
Correction of any consequences after removal consists of drug treatment, compliance with the doctor’s recommendations regarding diet, diet, and lifestyle. In case of serious violations, sphincter function is restored through surgery.
Choledocholithiasis
Metabolic disorders and lithogenicity of bile persist after gallbladderectomy, so even after a few years, stones can form again. But this time their localization is the common bile duct (common bile duct). Stones obstruct the flow of bile and lead to the appearance of typical signs of stone formation:
- cholangitis - inflammatory damage to the walls of the ducts;
- obstructive jaundice – due to an increase in the concentration of bilirubin in the blood;
- hepatic colic - paroxysmal acute pain under the right rib.
With the development of inflammatory processes, the pain syndrome is accompanied by nausea, vomiting, fever with a sharp rise in body temperature to 39 degrees, and increased sweating. If the stone blocks the duct, signs of jaundice appear - yellowness of the skin and sclera. In this case, dissolution or removal of stones is indicated to normalize the condition.
Life after surgery, namely gallbladderectomy, is clouded by problems with the pancreas. Violation of the mechanism of enzyme production, retention of pancreatic juice leads to inflammation of the organ. The disease can progress for many years and manifests itself:
- attacks of pain in the right and left half of the abdomen;
- sometimes the pain syndrome can be girdling in nature;
- an attack is provoked by eating fatty, spicy, fried foods;
- in some patients, pain may appear at night;
- During an exacerbation, there is a slight increase in body temperature.
During periods of severe exacerbation, men and women are prescribed a 3-day therapeutic fast and drinking mineral water without gas. In the future, recommendations are given on following diet No. 5 with a strict restriction of fats. The consequences after removal of the gallbladder directly depend on nutrition, so it is important to follow a diet.
After removal of the gallbladder, due to a disruption in the functioning of the sphincter of Oddi, contents from the duodenum are refluxed into the stomach. The pathological phenomenon is accompanied by the following symptoms:
- pain spreading throughout the abdomen;
- the tongue is covered with a yellow coating;
- belching, heartburn.
Reflux is confirmed by ultrasound examination of the abdominal organs, treated with medication, and in severe cases with surgery. A long course of duodenogastric reflux leads to the development of gastric and duodenal ulcers due to the aggressive effect of bile on the gastrointestinal mucosa.
Gastritis and esophagitis
Inflammation of the stomach and esophagus is a common occurrence after removal of the gallbladder. Regular reflux of caustic bile irritates the walls of the upper gastrointestinal tract, destroys the protective layer of mucus and causes an inflammatory reaction. When the esophagus is damaged, a person develops:
- feeling of a lump in the throat;
- pain while swallowing;
- burning, heartburn.
In complicated cases, the voice becomes hoarse, ulcers form in the mouth, bad breath, pain spreads beyond the sternum and radiates to the back. Usually, if the gallbladder has been removed, a consequence such as esopharyngitis is combined with gastritis. This is fraught with the appearance of:
- dull aching pain in the epigastric region;
- heaviness in the upper abdomen;
- heartburn, belching;
- vomiting with bile and mucus;
- gray coating on the tongue;
- loss of appetite.
The pathological process also extends to the intestinal region, causing rumbling in the abdomen, flatulence, upset stool - alternating constipation and diarrhea. To improve the condition after removal of the gallbladder, a person is recommended to adhere to a diet. An important piece of advice is the need to lead a healthy lifestyle, avoiding alcohol and other bad habits.
Indications for drainage of the bile ducts and gallbladder
Drainage is a surgical operation, the purpose of which is to improve the outflow of substances and eliminate the causes of mechanical obstruction. Any surgical intervention is considered complex and is carried out strictly according to indications after preliminary preparation.
In patients with obstructive jaundice, gallbladder drainage is performed if conservative methods of therapy do not provide a significant result. Often, competent drug therapy leads to improved patency. Thanks to this, the outflow of substances is normalized, and the level of bilirubin is stabilized. For some diseases, conservative methods of therapy are not effective, which is why drainage is used.
Indications:
- Gallstone disease in late stages
- Malignant and benign tumors
- Acute cholecystitis
- Congenital malformations
Drainage is also prescribed as a preparatory procedure before major operations. Often drainage is placed before using antiseptic drugs or antibiotics to treat bacterial lesions.
What examination is carried out for obstructive jaundice in cancer patients?
Blocking of the bile ducts - common bile duct, right and left hepatic, as well as intrahepatic ducts in cancer patients occurs due to compression of them by the tumor in the following cases:
- for cancer of the head of the pancreas;
- for cancer of the common bile duct (common bile duct);
- for duodenal cancer;
- for gallbladder cancer;
- for cancer of the papilla of Vater (the place where the common bile duct enters the duodenum);
- with primary liver cancer, when the tumor is located near large ducts;
- with liver metastases from cancer of other organs;
- for lymphomas.
Most often, obstructive jaundice is diagnosed during cancer treatment abroad and it is believed that this is associated specifically with metastases to the liver, and here’s why. The fact is that the main function of the liver is to cleanse the entire body of toxins, and venous blood flows to it through the portal vein, collecting from all organs and parts of the body.
If there is a malignant tumor in any organ or part of the body, its cells can be washed out and enter the tissue fluid, from there into the lymph and blood, and then into the liver. Settling there, they multiply and form a metastatic node - a secondary cancerous tumor. This happens in advanced cases of cancer, when it grows and becomes more friable. Metastases in the liver always indicate stage 4 cancer.
They can come from literally any organ when:
- lung cancer;
- breast cancer;
- stomach cancer;
- bowel cancer;
- uterine cancer;
- prostate cancer;
- ovarian cancer;
- breast sarcomas.
Obstructive jaundice in the treatment of non-Hodgkin lymphomas abroad is associated with damage and enlargement of the lymph nodes at the porta hepatis, which compress the bile ducts.
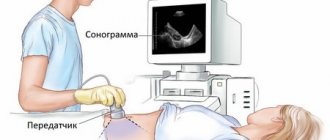
When examining a cancer patient with obstructive jaundice, liver ultrasound and Doppler sonography are performed, which make it possible to determine the presence and location of the tumor, the condition of the bile ducts - their narrowing, expansion, deformation. Additionally, MRI and PET are prescribed to accurately determine the spread of the tumor in the abdominal cavity; cholangiography is mandatory - an X-ray examination of the bile ducts with contrast. Such studies are carried out in all clinics in Israel and other countries with developed healthcare systems.
It can be done in two ways:
- endoscopic retrograde - through a probe inserted into the duodenum, contrast is injected into the lumen of the common bile duct and photographs are taken.
- percutaneous puncture, in which a liver puncture is made in the intercostal space on the right under ultrasound control, a large bile duct is penetrated and contrast is injected, then pictures are taken.
Such a study allows you to accurately determine the level of compression of the duct, which is very important for choosing a treatment method.
In addition to these studies, the patient undergoes:
- scanning of all organs;
- full laboratory examination;
- determination of the amount and fractions of bilirubin;
- research on tumor markers;
- molecular genetic tests.
Types of drainage
Various drainage installation methods are used. They differ in the method of administration, indications, and other features. The optimal way to reduce bilirubin concentration is prescribed taking into account the characteristics of the patient and the clinical picture.
External drainage of the bile ducts
Guide tubes are inserted into the area of obstruction. They remove bile from the organ into a container fixed outside.
Drainage is carried out in preparation for operations or after undergoing interventions. The advantage of the external method is the ability to control the volume of secretion produced, the presence of blood and pus in it, indicating complications. Medications can be administered through an installed catheter with a string.
Patients with external drainage need to take enzyme preparations. To maintain digestive functions, bile is injected directly into the intestines.
This is interesting: How long is jaundice treated in newborns: causes and consequences
External-internal drainage
The drainage is installed in such a way that most of the bile enters the intestines. Excess secretion is discharged outside into the receiving container.
The procedure is carried out using the puncture method. If performed incorrectly, complications may occur. Most often this happens when the drainage tube is damaged.
Percutaneous transhepatic drainage (PTD)
Provides for the introduction of a device that prevents the development of stagnant processes. It is installed for a long time. Thanks to this method, re-development of obstruction is excluded. The volume of bile entering the intestines is controlled.
This version of the procedure is used mainly as a palliative therapy measure for terminally ill patients. Often prescribed to patients with cancer, cirrhosis, and congenital anomalies.
Reviews about the treatment of obstructive jaundice abroad
Obstructive jaundice is dangerous for the body, causing severe intoxication and dysfunction of all organs.
In oncology, it is more often diagnosed during the treatment of metastatic cancer abroad, and such patients are often given up as not promising for treatment. This formulation of the question is typical for medical institutions, the level of which leaves much to be desired, where there are no new technologies for examining and eliminating this complication.
However, in modern clinics and centers, both foreign and domestic, methods are used that allow:
- pinpoint the causes;
- jaundice level;
- take measures to restore normal bile circulation.
Next, we will look at the clinical nature of the development of this condition, and also find out how long obstructive jaundice lasts.
Consultation with a leading doctor
Treatment of obstructive jaundice is carried out in parallel with complex treatment of the underlying disease (cancer, sarcoma, lymphoma). This treatment does not eliminate the tumor, but only eliminates the blockage of the bile ducts, creates conditions for the outflow of bile into the intestines, thereby saving the patient from death, increasing life expectancy with obstructive jaundice. In some cases, droppers are prescribed for obstructive jaundice.
Of course, it is possible to eliminate the block of bile and restore the patency of the bile ducts only through surgical intervention. In modern clinics, so-called drainage operations on the bile ducts are used, which are performed after cholangiography and determining the level of blockage of the duct.
The following drainage methods are used:
- external drainage - a probe is installed that removes bile outside. At the same time, its stagnation and obstructive jaundice are eliminated. The disadvantage of this method is the lack of flow of bile into the intestines and associated digestive disorders - indigestion of fats and fat-soluble vitamins. However, the advantages are that the probe can be used to introduce chemotherapy drugs into the liver, for selective radiotherapy of cancer (injection of a solution with radioisotopes).
- internal drainage - restores the passage of bile into the intestines, eliminating jaundice and normalizing digestion. Such operations are called biliodigestive anastomoses, when the common bile duct is cut off from the place of its compression and sutured into a loop of the small intestine. However, these operations on the abdominal cavity are more complicated, and not every patient can perform them, taking into account the general state of health.
- combined (external-internal) drainage - bile partially enters the intestines and is partially excreted. The drainage method is selected individually, depending on the location of the bile blockage, the nature and location of the tumor, anatomical features and the general condition of the patient. Most often, these operations are performed using minimally invasive methods - endoscopic, laparoscopic, so as not to cause additional trauma to the patient.
Among the new methods of treating bile duct obstruction used in the treatment of cancer in Israel, stenting is becoming very popular - dilating the duct with a special probe and introducing a tubular metal or plastic frame (stent) into its lumen, which does not allow the duct to narrow.
Such operations are performed when the duct is surrounded by a tumor, and there is no way to remove it; they expand its lumen from the inside, using a stent.
In modern clinics, stenting is performed using endoscopic video systems (Olympus, etc.) and a tomographic digital stenoscope (General Electric). The procedure is precise, low-traumatic and takes little time.
New types of intraductal stents are also being developed. The fact is that the service life of a conventional stent is 2-3 years; it gradually becomes clogged with a putty-like mass formed from bile and ceases to perform its function.
Today it is possible to use self-expanding nitinol wire stents, which respond to changes in the lumen of the duct and the degree of its compression, and the period of their installation is not limited.
Get a treatment program
Many patients are interested in the question: how long do people with obstructive jaundice live? Drainage operations for obstructive jaundice and stenting of the biliary tract are very effective; they actually save the patient’s life, or rather, eliminate the threat of death from developing obstructive jaundice. Of course, this prolongs his life by years, even in cases of inoperable cancer, and improves his quality of life.
According to statistics provided by different clinics, drainage operations and stenting for oncological obstructive jaundice within 2-3 weeks allow:
- eliminate liver failure;
- normalize digestion;
- prepare the patient for a course of chemotherapy and radiotherapy, which are highly undesirable during jaundice.
When talking about visiting leading oncology clinics, we cannot ignore the issue of the cost of cancer treatment abroad. It must be taken into account that the cost of services is affected by the patient’s condition and the stage of his disease. Despite the fact that obstructive jaundice in cancer patients is an indicator of an advanced metastatic stage of cancer, one should not give up.
Those who have had obstructive jaundice can best describe the results of therapy for this diagnosis.
“After I was treated for a gallbladder tumor at the regional oncology center, I developed jaundice. And since I still had to undergo chemotherapy, my husband insisted that I continue treatment abroad. I ended up in a Turkish clinic, where they quickly gave me drainage and later I was able to finish chemotherapy. It’s very good that I ended up here, because Russian doctors would not have been able to cope.”
Olga, Perm
“Jaundice appeared due to liver cancer. I had to urgently look for a hospital abroad, as I understood that I simply might not be saved at home. I went to the Ichilov clinic in Israel. Here I was examined within 2 days, an operation was prescribed and I felt better. Now I am undergoing further treatment here.”
Anna, St. Petersburg
The life expectancy of a patient with a malignant tumor may be longer than with obstructive jaundice syndrome. There's no time to waste!
According to WHO, liver cysts are diagnosed in 0.8–2% of people on the planet. This is a benign formation in the parenchyma in the form of a cavity filled with a liquid or jelly-like transparent substance. The size of cysts can reach up to 25 cm in diameter. As a rule, the diagnosis is made in people aged 40–50 years (three times more often in women), since liver cysts usually progress asymptomatically.
Causes
All cystic formations in the liver parenchyma are divided into parasitic and non-parasitic. In the first case, it is clear that the disease is acquired and develops against the background of a parasitic invasion - usually echinococcosis or alveococcosis. In the second case, the issues of etiology have not been fully studied, so doctors now offer several hypotheses for the origin of the cysts:
- defect in fetal development in the womb, when intrahepatic blood circulation in the portal vein is disrupted; as a result, closed areas covered with epithelium appear, which over time, as the liver processes incoming elements (food, drugs, chemicals), are filled with inflamed fluid and various biological “garbage”;
- hormonal imbalance and long-term use of hormonal drugs - according to research results, women who have given birth repeatedly have an increased tendency to develop cystic processes;
- rapidly progressive inflammation in the liver, in particular fibrosis and cirrhosis due to hepatitis or alcoholic illness;
- surgical and traumatic injuries of the liver, as a result of which a large residual cavity is formed (where bile and blood accumulated), which does not allow the edges of the parenchyma to close.
Classification
Liver cysts can change its morphological structure in different ways - located in different lobes, occupy a specific segment, or spread only on the surface of the parenchyma. In rare cases, a cyst forms “on its own,” connecting to the liver only with a thin bridge.
The color of the cystic substance is determined by the elements it contains - epithelial cells, fibrin, cholesterol, mucin and bilirubin. So, with the accumulation of cholesterol, the liquid has a white or slightly yellow color, and with a high bilirubin content, it has a bright light brown tint. In rare cases, when the liver becomes infected with a purulent process and hemorrhages, the contents of the cyst become dark brown or blue.
Conservative treatment for obstructive jaundice of tumor origin is ineffective, since it does not eliminate its main cause. Moreover, jaundice can progress, as over time the patency of the biliary tract becomes worse. Infusion therapy can reduce the level of bilirubin in the blood, but the primary goal in the treatment of liver tumors is to restore the outflow of bile.
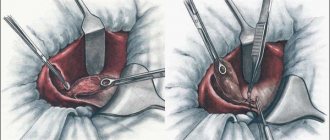
Since patients with already formed obstructive jaundice are admitted for treatment quite late, treatment is divided into 2 stages - temporary bile diversion followed by radical surgery. This approach reduces mortality and the number of postoperative complications.
Surgical techniques allow not only to get rid of obstructive jaundice, but also to prepare for radical surgery to remove the tumor. Several approaches have been developed - endoscopic, percutaneous, intraoperative (during another operation). Before any intervention, careful visualization of the lesion is carried out using ultrasound and x-ray techniques.
Contraindications to drainage
The procedure may not be prescribed to all categories of patients. This is due to the potential risk of complications. Before the operation, it is imperative to ensure that there are no restrictions.
Contraindications:
- Diseases characterized by bleeding disorders
- Liver failure accompanied by ascites
- Late stages of cancer
- Pathological neoplasms at the site of intended drainage fixation
- Late pregnancy
- Obesity
- Serious illnesses, heart defects
The operation is not performed for obstructive jaundice in patients who have recently undergone surgery. It is prohibited to intervene if the patient is in serious condition. In the vast majority of cases, the procedure is carried out as planned. Drainage is rarely performed as an emergency therapeutic measure.
The essence of drainage
Drainage of the bile duct is a type of process of invasive creation of an anastomosis on the path from the bile duct to the intestine. At the first stage, using an infusion drip, the patient is administered sedatives and analgesics. Sometimes general anesthesia is used. During the operation, indicators of the cardiovascular system and pressure should be under constant monitoring by the nurse.
The possibility of carrying out such operations is ensured by the availability of special X-ray equipment for ultrasound. Thanks to this surgical intervention for serious diseases, for example, inoperable cancer, the patient’s life can be extended from 6 months to 1.5 years.
Possible complications
Obstructive jaundice is a rather dangerous disorder. In the absence of timely treatment, severe pathological phenomena develop. Therefore, it is necessary to restore the patency of the bile ducts, improve the outflow of substances, and reduce the load on the organs.
Installing drainage is the most effective method of treatment. Unlike conservative methods, it allows you to quickly eliminate obstruction and restore normal outflow. External and external internal drainage is installed without complications. Such options are considered safe and in rare cases cause side effects. Most often, complications arise with the percutaneous transhepatic method.
This is interesting: Is jaundice dangerous in newborns: types and consequences
Negative consequences of the procedure:
- Hemorrhagic disorders
- Peritonitis due to leakage of bile into the abdominal cavity
- Pain syndrome
- Development of cholangitis
- Displacement of drainage catheter, tube, prosthesis
- Suppuration in the area of implementation
Thanks to the use of modern medical instruments and equipment, the risk of complications is minimal.
Types of operations
Nutrition starts on the second day. Eat simple food for the postoperative period. On this day you will have to limit yourself to low-fat light broth, fruits, light cottage cheese, yogurt.
It is recommended to take food in small quantities, with great frequency: 5-7 meals.
After three days, you can start eating everyday foods. Rough foods, fatty, fried foods, spices, and sauces are excluded. It is not recommended to consume products made from rye flour, or anything that promotes the secretion of bile or gas formation.
It is recommended to switch to nutrition according to therapeutic diet No. 5.
Completely postoperative pain disappears after 24-96 hours. If during this period the pain does not go away, but on the contrary, intensifies, a doctor’s consultation is necessary. Underwear should be soft, should not press or rub the puncture site.
Drainage
In most cases, drainage is required. Its main purpose is to ensure reliable outflow of bile and fluid. Drainage prevents stagnation. If the formation of fluid has decreased and restoration processes have begun, the drainage can be removed.
The sutures, unlike abdominal surgery, are small and compact. They do not exceed 1.5-2 cm in diameter. The sutures are removed as the incisions heal. If healing is good, the sutures are removed on the second day; if the speed of recovery processes is low, removal is carried out approximately on the 7-10th day. It all depends on the individual characteristics of the patient.
The scars after laparoscopy are insignificant, not exceeding 2 cm in size. Four scars remain after the operation. They heal quickly.
How long do you have to lie down after gallbladder removal surgery?
The patient should lie down for a 4-6 hour period. Then you can rise and make slow movements. Quite often they are discharged from the hospital even on the day of surgery.
After a routine uncomplicated laparoscopic cholecystectomy, the patient is transferred from the operating room to the intensive care unit, where he spends the next 2 hours of the postoperative period to monitor adequate recovery from the state of anesthesia.
In the presence of concomitant pathology or characteristics of the disease and surgical intervention, the duration of stay in the intensive care unit may be increased. The patient is then transferred to a ward where he receives the prescribed postoperative treatment.
During the first 4-6 hours after surgery, the patient should not drink or get out of bed. Until the morning of the next day after the operation, you can drink plain water without gas, in portions of 1-2 sips every 10-20 minutes with a total volume of up to 500 ml.
The patient can get up 4-6 hours after surgery. You should get out of bed gradually, first sit for a while, and, in the absence of weakness and dizziness, you can get up and walk around the bed.
It is recommended to get up for the first time in the presence of medical personnel (after a long stay in a horizontal position and after the action of medications, orthostatic collapse - fainting) is possible.
The next day after the operation, the patient can move freely around the hospital, begin to take liquid food: kefir, oatmeal, diet soup and switch to the usual regime of drinking liquids. In the first 7 days after surgery, the consumption of any alcoholic beverages, coffee, strong tea, drinks with sugar, chocolate, sweets, fatty and fried foods is strictly prohibited.
The patient's diet in the first days after laparoscopic cholecystectomy may include fermented milk products: low-fat cottage cheese, kefir, yogurt; porridge with water (oatmeal, buckwheat); bananas, baked apples; mashed potatoes, vegetable soups; boiled meat: lean beef or chicken breast.
In the normal course of the postoperative period, the drainage from the abdominal cavity is removed the next day after surgery. Removing the drainage is a painless procedure; it is performed during dressing and takes a few seconds.
In the first month after surgery, the functions and general condition of the body are restored. Careful adherence to medical recommendations is the key to full recovery of health. The main areas of rehabilitation are adherence to physical activity, diet, drug treatment, and wound care.
In the hospital, special stickers will be applied to postoperative wounds located at the places where instruments are inserted. It is possible to take a shower with Tegaderm stickers (they look like a transparent film), while Medipore stickers (a white patch) must be removed before showering.
You can shower starting 48 hours after surgery. Getting water on the seams is not contraindicated, but you should not wash the wounds with gels or soaps or rub them with a washcloth.
After taking a shower, you should lubricate the wounds with a 5% iodine solution (or Betadine solution, or brilliant green, or 70% ethyl alcohol). Wounds can be treated using the open method, without dressings.
Taking baths or swimming in pools and ponds is prohibited before the sutures are removed and for 5 days after the sutures are removed.
Sutures after laparoscopic cholecystectomy are removed 7-8 days after surgery. This is an outpatient procedure, the sutures are removed by a doctor or a dressing nurse, and the procedure is painless.
As soon as the patient has learned that surgery is indicated as the only effective treatment, and the date is already known, it is worth starting preparations. First, the doctor must explain how long the rehabilitation period after cholecystectomy will take. The length of your stay in a hospital bed may vary depending on the size of the incision.
Typically, the patient is provided with a list of things to prepare upon admission to the surgical department.
Diet after gallbladder laparoscopy is a major aspect of recovery. A well-structured diet helps prevent gastrointestinal upset, which is a common manifestation after cholecystectomy.
Up to 4 months you should stick to the following diet:
- lean meat, boiled or steamed;
- boiled white fish meat;
- vegetables, preferably potatoes, carrots and zucchini;
- fresh berries and fruits;
- weak tea, vegetable juices and fruit drinks.
You should forget about baking, fried foods, and fatty dairy products. It is better to eat “yesterday’s” bread. As a dessert, you can prepare yourself a baked apple with cottage cheese, compotes, and jelly. You need to eat in small portions, at least 5-6 times a day.
It is necessary to reduce the consumption of foods high in cholesterol. The daily portion of butter should not exceed 20 grams. You need to buy low-fat dairy products.
It is important to chew food slowly, this will awaken the enzymes necessary for digestion. All these recommendations are designed to help the liver.
However, many patients ignore these rules and begin to eat whatever they want. This attitude towards your body will not lead to anything good. In medical practice, there are cases when a patient after cholecystectomy was again admitted to the hospital for rehabilitation several months later. A return to a normal diet should take more than a year.
And, of course, you should forget about alcohol forever. Recovery after surgery is a long journey towards your health. Of course, this requires patience and endurance, however, in order to prevent serious complications, you need to try.
Physical activity plays an important role in restoring the body. Immediately after surgery, loads should be limited to subjective sensations, then you can include warm-up and walks in the fresh air. The core muscles should not be strained earlier than after a year. Pleasant emotions are the best medicine for a person undergoing surgery.
Currently, laparoscopic removal of gallstones is very rarely used. This phenomenon is due to the fact that the chronic course of cholelithiasis is associated with disorders in cholesterol metabolism and surgery does not make much sense, since a relapse will occur after a certain period of time.
Cholecystectomy is used to treat diseases such as:
- chronic calculous inflammation of the gallbladder;
- cholesterosis;
- gallbladder polyposis;
- acute inflammation of the gallbladder;
- asymptomatic stone carriers.
General contraindications to laparoscopy are diseases such as malignant tumors, cardiac and pulmonary decompensation, and general peritonitis. The minimally invasive method is not used in people who are overweight and in pregnant women in late gestation.
Also, laparoscopic cholecystectomy is not performed for people who have an abscess (purulent inflammation with the formation of a limited infiltrate) of the gallbladder, with severe scars in the area of the organ, or with acute pancreatitis (inflammation of the pancreas. The operation is not indicated for people with a pacemaker and obstructive jaundice.
Laparoscopy, despite the considerable trauma, is a serious surgical intervention, therefore, before the operation, preparations must be made for the removal of the gallbladder. It includes a full diagnostic examination of the body’s condition. The patient must donate blood for a general and biochemical analysis, which evaluates the functioning of the liver, kidneys, pancreas and the presence of inflammatory reactions.
The patient also needs to submit a urine sample for a general analysis, which helps analyze kidney function. Before the operation, the surgeon needs to know whether the patient has blood-borne infections: AIDS and HIV, syphilis, hepatitis. The patient must also donate blood for a coagulogram - a test characterizing the state of the blood coagulation system.
Among the instrumental examination methods, the obligatory ones are an electrocardiogram (assessment of heart function), fluorography (assessment of the condition of the lungs), FGS or EGDS (assessment of digestive function). The patient is carefully examined by a surgeon, therapist, and anesthesiologist. If he has chronic diseases, it is mandatory to see a doctor who treats the affected organ.
The day before surgery, eating after six o'clock in the evening is prohibited. The patient should not drink 8 hours before the upcoming laparoscopy. During a planned admission, the patient is given two enemas: in the evening the day before the intervention and in the morning before the operation. 7 days before the proposed laparoscopy, you should stop taking blood thinners and non-steroidal anti-inflammatory drugs, which will help avoid bleeding.
Typically, cholecystectomy is performed under general anesthesia using a special mask. This type of anesthesia helps to achieve a complete absence of unpleasant sensations and prevents unwanted movements of the patient during the operation.
After removal of the gallbladder, the patient is transported to the ward, where he recovers from anesthesia. At this time, he may be bothered by nausea, headaches, poor health, and a feeling of “overwhelm.” Bed rest is recommended for 8 hours, then the patient can sit down and perform simple manipulations in a lying position. Doctors advise not to get out of bed for the rest of the day. You can drink water 4-5 hours after laparoscopy.
The first few days the patient is often bothered by pain in the area of the surgical wounds; they usually go away after 3-5 days. Any physical activity after removal of the gallbladder is allowed only after a week; until this point the patient is prohibited from lifting weights.
In the absence of complications, the temperature after removal of the gallbladder remains normal, or rises on the first day to 37.5 degrees, and then drops to 36.6.
To prevent postoperative infectious complications, the patient is prescribed broad-spectrum antibiotics. Analgesic non-narcotic drugs are used to relieve pain. According to indications, doctors may prescribe intravenous infusions. The time for removing sutures depends on the type of material; most often this manipulation is performed after 1-2 weeks.
| Advantages | Laparoscopy of the gallbladder | Operation through an incision |
| Less traumatic intervention | 4 punctures of 1 cm each. | The incision is 20 cm long. |
| Lower blood loss | During laparoscopy of the gallbladder, the patient loses on average 30-40 ml of blood. | Blood loss is significantly greater. |
| Shorter rehabilitation times | The patient is discharged from the hospital after 1-3 days. | The patient is discharged from the hospital after 1-2 weeks |
| Faster recovery | Performance is fully restored within a week. | Recovery takes 3-6 weeks. |
| Less pain after surgery. | As a rule, ordinary painkillers are sufficient to relieve pain. | Sometimes the pain is so severe that the patient has to be prescribed narcotics. |
| Lower incidence of postoperative complications. | Adhesions and hernias form much less frequently after laparoscopy. |
Currently, the following types of surgical interventions are performed for diseases of the gallbladder:
- Laparoscopic cholecystectomy – removal of the gallbladder laparoscopically. This is one of the most common interventions in endoscopic surgery.
- Choledochotomy is a dissection of the common bile duct.
- Anastomosis is the creation of communications between the bile ducts and other organs of the digestive system to improve the outflow of bile.
Indications for laparoscopic cholecystectomy
Indications for making an incision and performing an open operation:
- On the day of surgery, the patient is usually allowed to stand up, walk and eat liquid food.
- The next day you can eat normal food.
- Approximately 90% of patients can be discharged within 24 hours after surgery.
- Within a week, performance is restored.
- Small bandages or special stickers are applied to postoperative wounds. The stitches are removed on the 7th day.
- After surgery, you may experience pain for some time. To relieve them, regular painkillers are used.
Complications are possible with any operation, and laparoscopy of the gallbladder is no exception. Compared to open surgery through an incision, interventions using endoscopy have a very low risk of complications - only 0.5%, that is, in 5 out of 1000 operated on.
Regardless of the type of planned intervention, be it laparoscopy or abdominal removal of the gallbladder, the indications for surgical treatment are:
- Cholelithiasis.
- Acute and chronic inflammation of the bladder.
- Cholesterosis with impaired bile excretion function.
- Polyposis.
- Some functional disorders.
Gallstone disease is usually the main reason for most cholecystectomies. This is due to the fact that the presence of stones in the gall bladder often causes attacks of biliary colic, which recurs in more than 70% of patients. In addition, stones contribute to the development of other dangerous complications (perforation, peritonitis).
In some cases, the disease occurs without acute symptoms, but with heaviness in the hypochondrium and dyspeptic disorders. These patients also require surgery, which is performed as planned, and its main purpose is to prevent complications.
Gallstones can also be found in the ducts (choledocholithiasis), which poses a danger due to possible obstructive jaundice, inflammation of the ducts, and pancreatitis. The operation is always complemented by drainage of the ducts.
The asymptomatic course of gallstone disease does not exclude the possibility of surgery, which becomes necessary with the development of hemolytic anemia, when the size of the stones exceeds 2.5-3 cm due to the possibility of bedsores, with a high risk of complications in young patients.
Cholecystitis is an inflammation of the gallbladder wall, occurring acutely or chronically, with relapses and improvements replacing each other. Acute cholecystitis with the presence of stones is a reason for urgent surgery. The chronic course of the disease allows it to be carried out plannedly, possibly laparoscopically.
Cholesterosis is asymptomatic for a long time and can be detected by chance, and it becomes an indication for cholecystectomy when it causes symptoms of gallbladder damage and disruption of its function (pain, jaundice, dyspepsia). In the presence of stones, even asymptomatic cholesterosis serves as a reason to remove the organ. If calcification occurs in the gallbladder, when calcium salts are deposited in the wall, then surgery is mandatory.
The presence of polyps is fraught with malignancy, so removal of the gallbladder with polyps is necessary if they exceed 10 mm, have a thin stalk, or are combined with cholelithiasis.
Open surgery
For the best treatment outcome, it is important to conduct adequate preoperative preparation and examination of the patient.
For this purpose, the following is carried out:
- General and biochemical blood and urine tests, tests for syphilis, hepatitis B and C;
- Coagulogram;
- Clarification of blood type and Rh factor;
- Ultrasound of the gallbladder, biliary tract, abdominal organs;
- ECG;
- X-ray (fluorography) of the lungs;
- According to indications – fibrogastroscopy, colonoscopy.
Some patients need consultation with specialized specialists (gastroenterologist, cardiologist, endocrinologist), all – with a therapist. To clarify the condition of the biliary tract, additional studies are carried out using ultrasound and radiopaque techniques. Severe pathology of internal organs should be compensated as much as possible, blood pressure should be brought back to normal, and blood sugar levels should be monitored in diabetics.
Preparation for surgery from the moment of hospitalization includes eating a light meal the day before, completely refusing food and water from 6-7 pm before the operation, and in the evening and morning before the intervention the patient is given a cleansing enema. In the morning you should take a shower and change into clean clothes.
If it is necessary to perform an urgent operation, the time for examinations and preparation is much less, so the doctor is forced to limit himself to general clinical examinations and ultrasound, allocating no more than two hours for all procedures.
The essence of the procedure
Drainage of the gallbladder refers to routine surgical interventions, the purpose of which is to restore the bile flow, reduce the concentration of bilirubin in the blood, and evacuate bile from the liver tissue. If suturing the ducts is not indicated, such as after radical removal of the gallbladder (cholecystectomy), surgeons immediately begin to drain the organs of the hepatobiliary system. Installation of a drainage structure is often carried out laparoscopically, but if necessary, alternative methods that differ in surgical access are prescribed.
When the ducts are blocked, drainage is installed at the site of narrowing, which restores the patency of the lumens, improves the passage of bile, and relieves symptomatic manifestations such as acute pancreatitis. Endoscopic or laparoscopic operations are performed under the control of X-ray equipment or ultrasound, which ensures precision of manipulation and minimizes the risk of damage to healthy tissue.
What signs indicate diseases of the liver and gallbladder?
- dull pain in the abdomen, liver, which can radiate to the shoulder blade, arm, solar plexus, lower back, pancreas, and the pain increases and may intensify with inhalation;
- darkening of urine, abnormal stool – diarrhea;
- the skin and sclera of the eyes become yellow;
- skin itching appears;
- a person experiences nausea, and constantly, vomiting appears;
- appetite decreases, anorexia develops, even if you follow a diet;
- For many, the body temperature rises, signs of general intoxication of the body appear - sweating, drowsiness, weakness and fatigue;
- the liver increases in size, sometimes to such an extent that the right side becomes asymmetrical in relation to the left hypochondrium.
Many people are concerned about the question of whether obstructive jaundice is contagious. You can definitely say “no”. It is contagious only in one case - if it is caused by hepatitis.
Touching this area is unpleasant and painful. Moreover, palpation often causes involuntary holding of breath.
If the cause of the blockage is malignant and benign neoplasms, then the pain is dull, radiating to the back area. Palpation reveals nodes in the liver, but the spleen cannot be felt. The following symptoms are also observed: loss of appetite, belching with a bitter taste and darkening of the urine.
With pancreatitis, pain develops not only in the liver area, but also in the pancreas area.
Itching often develops before the main symptoms appear, especially in the presence of tumorigenesis. The itching is very severe and cannot be relieved with medications and ointments.
At the same time, constant scratching leads to small hematomas and wounds. Diet does not help in this case either.
Another pathogenesis is sudden weight loss. Such a symptom in 85% indicates a cancerous neoplasm (Klatskin tumor), cancer of the head of the pancreas.
Subhepatic jaundice may be accompanied by fever. This is explained by the fact that an inflammatory process develops and is sometimes a sign of the genesis of tumor disintegration. But sometimes there is no temperature.
The duration of pathology in adults may vary depending on the causes. Obstructive jaundice can persist for several days and be observed for several months.
Symptoms such as jaundice and pain are quite serious and indicate a malignant neoplasm - Klatskin tumor, cancer of the head of the pancreas, especially if the person loses weight.
Speaking about forecasts, we can say the following - it all depends on the reason why the skin turned yellow. If it is associated with blockage of the canal, caused by a stone, then after appropriate treatment, the person’s condition will return to normal. For pancreatitis, medications that reduce bilirubin levels should be taken.
For malignant neoplasms in adults (Klatskin tumor, cancer of the head of the pancreas), the prognosis is, unfortunately, disappointing, so at the first manifestations you should not hesitate to consult a doctor for detailed diagnostics and medical care.
Common symptoms of obstructive jaundice are:
- Pain in the hypochondrium and epigastric areas, which is dull in nature and tends to gradually increase.
- Darkening of the color of urine and discoloration of stool, as well as diarrhea.
- The color of the skin is yellowish, gradually turning into an earthy color. In obstructive jaundice, bilirubin is significantly increased.
- Itching on the skin.
- Nausea and vomiting.
- Abnormal weight loss.
- Lack of appetite.
- Increased body temperature.
- Cholesterol deposits in the eyelid area in the form of formations with clear edges.
- Enlarged liver.
Medications after gallbladder laparoscopy
Sometimes a course of antibiotic therapy may be necessary (if there is an increased risk of infection, during inflammatory processes). Fluoroquinolones, common antibiotics, are often used. When microflora is disturbed, probiotics and prebiotics are used. Such drugs as Linex, Bifidum, Bifidobacterin have proven themselves well.
A multivitamin may be needed. Further therapy is purely individual and depends on existing disorders and risks. For pain, painkillers (ketanal, ketanov) are used, and for spasms, antispasmodics (no-spa, duspatalin, mebeverine) are used.
In the presence of concomitant diseases or complications, etiological or symptomatic therapy is used. So, for pancreatitis, enzyme preparations are used, such as Creon, Pancreatin, Micrazim.
For increased gas formation, drugs such as meteospasmil and espumizan may be useful.
To normalize the functioning of the sphincter and duodenum, motilium, debridate, and cerucal are used.
When using medications, you must always consult your doctor, as self-medication can be dangerous.
How to take Ursosan after laparoscopy of the gallbladder?
Ursosan is a hepatoprotector that protects the liver from adverse effects. They are taken for a long time, from 1 to 6 months.
The active ingredient of this drug is ursodeoxycholic acid, which protects the mucous membranes from the toxic effects of bile acids. Use the drug 300-500 mg at night.
The drug becomes vitally necessary, since the liver requires even greater protection from bile, which is released directly into the intestine.
Shilajit is a fairly effective remedy that is used for various diseases. This is an ancient folk medicine that stimulates the digestive organs well.
Mumiyo is harmless to the body. After surgery, the dosage of the drug is reduced by 3 times compared to the standard dosage.
You should drink mumiyo for 21 days. A repeat course can be taken after 60 days.
The course includes 20 g of mumiyo, which is dissolved in 600 ml of water. Apply three times a day.
The first week is used for 1 hour. l
, second - 2 tsp each
, third week - 3 tsp.
Treatment
Conservative treatment of obstructive jaundice - following a diet, taking medications. Surgical treatment in surgery depends on the disease that caused the syndrome.
Stenting and drainage using endoscopic or percutaneous methods are used. The latter include: percutaneous transhepatic cholangiostomy (PTCHS) or percutaneous transhepatic cholecystostomy under ultrasound and CT control.
Among the types of endoscopic drainage are: papillosphincterotomy (EPST), duodenobiliary drainage.
Obstructive jaundice - treatment with medications
The choice of treatment for obstructive jaundice with medications depends on the pathogenesis of the disease. Antispasmodics are used to reduce pain and increase the lumen of the ducts.
For cholelithiasis, cholangitis, and chronic cholecystitis, ursodeoxycholic acid is indicated. To protect the liver parenchyma, hepatoprotectors are needed, and for Klatskin tumor, gastric and pancreatic carcinoma, chemotherapy is needed.
Along with these medications, your doctor may prescribe:
- B vitamins;
- lipocaine;
- Vikasol;
- methionine;
- Trental;
- administration of glucose.
Drainage of the gallbladder for obstructive jaundice
Transhepatic percutaneous drainage (TPD) promotes the flow of bile. External drainage directs the discharge of bile through a catheter into the digestive system so that losses do not lead to stomach upsets.
Drainage of the gallbladder with obstructive jaundice (external-internal) requires the installation of a catheter from the outside. When the swelling in the area of narrowing decreases, it is carried out into the duodenum, and bile is sent to the gastrointestinal tract.
Percutaneous arthroplasty: Doctors insert a plastic prosthesis that replaces part of the wall.
Diet for obstructive jaundice
Nutrition eliminates excess stress on liver parenchyma cells. The diet for obstructive jaundice should include: plenty of fluids, carbohydrate-rich foods, low-fat dairy products, day-old or dried bread, fruits, vegetables, cooked meats and steamed fish.
All products and food should be at room temperature, boiled and pureed. To obtain fat, you can consume a small amount of butter and vegetable oil.
Treatment of obstructive jaundice should be carried out in the surgery department and always includes two stages.
The first stage includes decompression (unloading) of the biliary system in order to reduce the symptoms of the disease. There are open (performed during abdominal surgery) and closed (performed without major surgery) decompression. Currently, methods of closed unloading of the biliary tract are more popular. These include:
- Retrograde methods (bile diversion is carried out in the direction opposite to the normal flow of bile). These include a common intervention - percutaneous transhepatic cholangiostomy (PTCH). The method involves passing a tube through the skin of the anterior abdominal wall and liver tissue into the bile duct. The bile that does not enter the duodenum will flow through this tube.
- Antegrade methods (bile diversion is carried out in a direction coinciding with the normal flow of bile). These include nasobiliary drainage (NBD), biliary tract stenting and lithoextraction. NBD involves passing a tube through the nose, esophagus and stomach into the duodenum. Next, this tube, through which bile should subsequently flow, is inserted into the major duodenal papilla (MDP). Biliary stenting involves inserting a small, dense tube (stent) using an endoscopy into the narrowed bile ducts. The stent prevents them from collapsing, and normal bile drainage is restored. Lithoextraction (from the Latin “lito” - stone, “extraction” - removal) consists of removing the stone that is in the bile duct through the bile duct.
At the second stage, after the patient’s general condition has normalized, treatment is aimed directly at the cause of the disease. For example, if there is a tumor compressing the bile ducts, the surgeon decides to remove the tumor.
Thus, obstructive jaundice is not a homogeneous syndrome, but has many causes and requires different treatment methods. That is why the patient should not independently try to diagnose himself and prescribe treatment, even if he has certain symptoms and results of laboratory and instrumental studies.
In this case, you must definitely consult a doctor.
Treatment of obstructive jaundice consists primarily of eliminating the root cause of the appearance of such symptoms. For this purpose, a special diet is followed, and conservative drug treatment is also carried out. It consists of intravenous administration of a solution of glucose, various B vitamins, as well as drugs such as:
- "Essentiale". Stimulates the process of blood circulation in the liver.
- "Vikasol". Prevents bleeding.
- "Trental." Contains glutamic acid.
- Antibiotic drugs.
In addition, plasmapheresis is used, which cleanses the blood and enterosorption, aimed at ridding the body of toxins. Obstructive jaundice is also treated in surgery.
Obstructive jaundice is treated in various ways, depending on the cause of the disease. However, in most cases, the treatment is surgical - removal of stones blocking the duct, removal of scars or strictures, or removal of a tumor that interferes with the flow of bile.
Of course, the mandatory treatment of obstructive jaundice will include following a strict diet with a high content of protein foods and taking certain medications, such as:
- antibiotics and anti-inflammatory drugs (as indicated);
- vitamins;
- hepatoprotectors.
If the pathology is caused by oncological causes (tumor or metastases), surgical removal of the formation is required, followed by radiation therapy or chemotherapy.
Unfortunately, surgeons do not always have the opportunity to completely remove a tumor or, in general, perform an operation - in such cases the prognosis becomes extremely unfavorable and, despite the patient being prescribed chemotherapy and radiation therapy, his life expectancy does not exceed six months.
As for the diet, a person will have to adhere to it all his life with this disease, since after surgical removal of the cause that caused the blockage, the organ will no longer function in the same way as before the disease, and the person will have to spare it by eating only approved foods.