A bend in the gallbladder in a child is a pathology or a normal variant
The mechanism of development of gallbladder inflection in children
All VVP are associated with disruption of the autonomic nervous system (ANS), which has two divisions: sympathetic and parasympathetic (SNS and PSNS). Depending on which branch’s influence predominates, the following types of JVP are distinguished:
- if the influence of the SNS predominates, a hypokinetic type of GIB develops, the gallbladder loses its tone, stretches, and stagnation of bile appears in it, which contributes to the development of inflammatory processes and the formation of stones; this type of dyskinesia is more common in adolescence and is manifested by constant aching pain in the hypochondrium; if the influence of PSNS predominates, a hyperkinetic type of GIVP develops, which manifests itself in the form of spasms of the smooth muscles of the gallbladder and is accompanied by short-term attacks of severe spastic pain; this type of dyskinesia is more common in preschool children.
With any type of bile duct, a bend in the child’s gallbladder can develop. Most often these are functional excesses associated with sudden movement, lifting weights, severe fear, and so on. When examining a child with an ultrasound, it is not always possible to detect an inflection, since it is labile (changeable) in nature.
In the future, bile ducts and kinks in the gallbladder can lead to the development of an inflammatory process in the gallbladder and biliary tract (cholecystitis and cholangitis), as well as to diseases of the gastrointestinal tract due to constant digestive disorders associated with impaired secretion of bile into the intestines.
But it also happens that a bend in the gallbladder in children develops against the background of existing cholecystitis. This contributes to even greater stagnation of bile and supports the inflammatory process.
Symptoms of gallbladder bending in children
In young children, a bend in the gallbladder usually manifests itself in the form of sharp paroxysmal pain in the right hypochondrium, radiating to the right scapula and collarbone. The appearance of pain is usually associated with errors in diet, stress, sudden movement or heavy lifting. Nausea and one-time vomiting often appear along with pain. The attack usually passes quickly, but under similar circumstances it may appear again.
Older children can also have such attacks, but they are more characterized by constant aching pain in the right hypochondrium, which intensifies with stress, dietary errors and heavy physical activity. Nausea, vomiting, and sometimes diarrhea may occur periodically.
What to do if your child has abdominal pain
You should consult a doctor and undergo an examination. The sooner the gallbladder is identified and the gallbladder is bent, the easier it will be to help the child.
A bend in the gallbladder in a child is not such a rare occurrence. The main thing is its timely detection and treatment.
AGENESIS, APLASIA AND HYPOPLASIA OF THE GALL BLADDER AND BIL DUCT are malformations of embryonic development, manifested in the complete absence or underdevelopment of the gallbladder and bile ducts.
Agenesis and aplasia of the gallbladder are an extremely rare developmental anomaly (occurs 1 time in 500,000 births) and is a pathology incompatible with life (although the literature describes a case of the formation of a gallbladder in a newborn child in the case of normal development of the bile ducts). Much more common is hypoplasia of the gallbladder with complete or partial absence of bile ducts - atresia or their aplasia. The development of this defect is due to the characteristics of embryonic development. Violation of the fusion and process of recanalization of the ducts leads to the development of aplasia and atresia of the biliary system. Intrauterine pathological processes in the liver (congenital hepatitis, etc.) may have a certain significance.
Manifestations of gallbladder hypoplasia and bile duct atresia are typical. A child is born with jaundice, or it develops in the first 2-3 days after birth. Characterized by a gradual increase in jaundice. The stool has been discolored since birth. The urine is the color of dark beer. After 2-3 weeks from birth, an enlargement of the liver and then the spleen is noted. Noteworthy is the increase in the size of the abdomen, the expansion of the network of saphenous veins of the abdominal wall, later hemorrhagic manifestations occur, and ascites develops. children die from biliary cirrhosis 6-9 months after birth.
Diagnosis of congenital anomalies of the biliary system presents significant difficulties due to the identity of the clinical manifestations of a number of diseases accompanied by prolonged jaundice. Differential diagnosis is carried out with prolonged physiological jaundice of the newborn, conflict hemolytic jaundice, generalized cytomegaly, toxoplasmosis. syphilis. blockage of the bile ducts by mucus plugs, congenital giant cell hepatitis. With prolonged physiological jaundice of a newborn, the stool is usually excessively colored, the urine is dark, the jaundice tends to decrease, the free fraction of bilirubin predominates in the blood (with atresia, jaundice increases, the bound direct fraction of bilirubin predominates).
In conflict hemolytic jaundice, as in physiological jaundice, free bilirubin predominates; as a rule, there is a Rh conflict or a conflict in the ABO system.
The diagnosis of congenital syphilis, toxoplasmosis and cytomegaly is rejected or confirmed using serological reactions and special tests. If blockage of the bile ducts is suspected, antispasmodics are prescribed; under their influence, the bile ducts expand, the plugs come out, the jaundice quickly passes, and the child recovers.
Differential diagnosis with congenital giant cell hepatitis is possible only by using special research methods - laparoscopy and liver puncture biopsy.
An important role for making a correct diagnosis is played by: biochemical blood testing (total direct and indirect bilirubin is determined) and ultrasound examination.
An operation aimed at restoring the patency of the bile ducts is indicated. In case of total atresia and hypoplasia of the gallbladder, in order to partially divert bile into the intestines and prolong the life of the child, the thoracic lymphatic duct is transplanted into the esophagus.
The results of the operation are directly dependent on the form and degree of the developmental anomaly and the timing of the intervention. The best results can be obtained in the first 2 months of a child’s life.
Modifications of the usual form
An anomaly in the shape of the gallbladder is one of the most common and diverse types of modifications.
It can be acquired and congenital, dangerous and absolutely neutral. Some of them are characteristic of childhood and are corrected as they increase with age during the development and growth of the child:
- the Phrygian cap, named by analogy with the headdress, is never acquired, and extremely rarely causes any complications;
- septa in the bladder (usually multiple, arising for various reasons, interfere with the physiological outflow of bile secretions and cause stagnation, cholelithiasis and other pathological processes);
- diverticula or protrusions of the walls of the gallbladder, can be congenital or acquired as a result of the appearance of adhesions, are difficult to diagnose, but can act as factors in the development of inflammation;
- kinks (true and functional), sometimes called kinks and kinks, appear as a result of congenital problems or the influence of external factors, such as increased physical activity, errors in diet and weight (the degree of danger can be different and depend on the cause and nature of the kinks);
- cylindrical, spherical, boomerang-shaped and s-shaped - features of an individual complex of causes, sometimes causing controversy in pathological etiology, due to the variability of the forms inherent in the gallbladder.
An anomaly in the shape of the gallbladder is a common type of deformation of the gallbladder, caused by a variety of reasons.
It takes on the character of modifications from the most dangerous to those that pose virtually no risk.
Each specific case is considered separately, taking into account the possible development of a pathological scenario.
Often the condition of the organ is simply monitored, and medical measures are taken when dangerous signs appear.
In childhood, many of them go away as the child grows or can be corrected with diet and exercise.
Symptoms and treatment of bile duct in children
A bent gallbladder in a child can often pose a health threat. Gallbladder #8211; an organ that occupies a special position in the lower region of the liver. Its shape can be pear-shaped or conical. Often, a newborn may develop a bend in the pancreas.
Functions of the gallbladder
The main function of the gallbladder in children #8211; accumulation and concentration of bile, which will be used by the body itself to digest food, in particular fat. At the next stage, bile begins to be transported into the duodenum and bile duct.
In addition to the described properties, the gallbladder can have a contractile and enzymatic effect. Every year, the bending of the gallbladder in a child is becoming an increasingly common disease. The pathology begins to progress if the bladder rotates incorrectly, resulting in impaired outflow of bile. A similar phenomenon in science is called discension.
Some cases are characterized by the absence of symptoms, but in most cases the bend has a pronounced pain syndrome. In this case, it is not recommended to postpone visiting a doctor. The physician must diagnose the current clinical picture and establish an appropriate treatment regimen.
Symptoms and treatment
Severe pain in the abdominal area, decreased appetite, frequent vomiting, and increased body temperature may indicate a bend. Congenital bending causes a constant discharge of bile, causing vomiting.
In some cases, irritability, decreased activity and anxiety appear, sometimes #8211; sleep disturbance.
A bend in the gallbladder should be treated promptly, and treatment should be trusted #8211; only to specialists.
The pediatrician prescribes a diet for a bent gallbladder. All fatty, smoked, and sweet foods should be excluded from the children's diet. In addition, carbonated drinks and dishes made from fatty meat and fish will not be beneficial.
The best medicine #8211; a diet based on self-cooked food. It does not contain harmful preservatives, dyes and various kinds of food additives that are harmful to the child’s body. Meals should include fresh fruits and vegetables. The diet should include products of plant origin containing large amounts of natural fiber.
In providing proper treatment for the gallbladder in a child, treatment should be based on multiple meals. Steamed dishes or light oatmeal are a good alternative to fried foods. Porridges can absorb excess bile. For sweets you can eat: marshmallows, soufflé, marshmallows and crackers (not the sweet kind).
If a bend in the gallbladder is detected, you can supplement the diet with cottage cheese. If the child cannot tolerate sour taste, cottage cheese can be mixed with fruit.
Drinking plenty of fluids is recommended. The liquid will improve bile flow. To improve the clinical effect, you can use herbal decoctions of mint, chamomile, rose hips, etc.
Before starting use, you should consult your doctor, as herbs can cause allergic reactions.
Choleretic drugs can be used only after an ultrasound has been performed, which has established the absence of stones and sand. In some children, the bend disappeared as other organs grew.
If the bend does not disappear, then there is no need to panic. This disease #8211; not a sentence, you can lead a full life with it. Main condition #8211; proper diet without fried and spicy foods. The daily regimen should be supplemented with active physical activity. Courses of choleretic drugs can only be prescribed by doctors.
Self-prescribing medications and self-diagnosis can harm the child’s health. The first symptoms of bending #8211; a reason to immediately seek help from a doctor.
Treatment
When selecting therapeutic methods, the main role is played by the diagnostic results and the reasons due to which gallbladder anomalies formed.
If doctors reject the need for surgery to eliminate the anomaly, then treatment uses diet therapy, medications, physiotherapy and, with the doctor’s permission, traditional medicine.
- normalization of the contractile function of the bladder;
- improvement of bile outflow;
- elimination of symptoms, as well as the underlying disease that caused the abnormal phenomena of the gastrointestinal tract;
- preventing complications, such as organ inflammation or stone formation.
Be sure to prescribe treatment table No. 5 or 5-a according to Pevzner. “Heavy” foods are excluded from the diet: fried, smoked, fatty, pickled, spicy foods and similar foods. You should also not drink alcohol-containing drinks. Among traditional medicines, herbal choleretic infusions are allowed.
For symptomatic therapy, the patient is prescribed No-Shpu or other antispasmodics to eliminate pain. If the gallbladder is inflamed, you need to take antibacterial medications. Doctors can also prescribe choleretic drugs, for example, Hotifol or Holiver.
A person with an abnormal form of gastrointestinal tract is recommended to normalize body weight, balance nutrition and do gymnastics daily. This helps improve the flow of bile from the bladder and prevent the formation of stones or inflammation of the organ.
What is gallbladder hypoplasia
AGENESIS, APLASIA AND HYPOPLASIA OF THE GALL BLADDER AND BIL DUCT are malformations of embryonic development, manifested in the complete absence or underdevelopment of the gallbladder and bile ducts.
Agenesis and aplasia of the gallbladder are an extremely rare developmental anomaly (occurs 1 time in 500,000 births) and is a pathology incompatible with life (although the literature describes a case of the formation of a gallbladder in a newborn child in the case of normal development of the bile ducts). Much more common is hypoplasia of the gallbladder with complete or partial absence of bile ducts - atresia or their aplasia. The development of this defect is due to the characteristics of embryonic development. Violation of the fusion and process of recanalization of the ducts leads to the development of aplasia and atresia of the biliary system. Intrauterine pathological processes in the liver (congenital hepatitis, etc.) may have a certain significance.
Manifestations of gallbladder hypoplasia and bile duct atresia are typical. A child is born with jaundice, or it develops in the first 2-3 days after birth. Characterized by a gradual increase in jaundice. The stool has been discolored since birth. The urine is the color of dark beer. After 2-3 weeks from birth, an enlargement of the liver and then the spleen is noted. Noteworthy is the increase in the size of the abdomen, the expansion of the network of saphenous veins of the abdominal wall, later hemorrhagic manifestations occur, and ascites develops. children die from biliary cirrhosis 6-9 months after birth.
Diagnosis of congenital anomalies of the biliary system presents significant difficulties due to the identity of the clinical manifestations of a number of diseases accompanied by prolonged jaundice. Differential diagnosis is carried out with prolonged physiological jaundice of the newborn, conflict hemolytic jaundice, generalized cytomegaly, toxoplasmosis. syphilis. blockage of the bile ducts by mucus plugs, congenital giant cell hepatitis. With prolonged physiological jaundice of a newborn, the stool is usually excessively colored, the urine is dark, the jaundice tends to decrease, the free fraction of bilirubin predominates in the blood (with atresia, jaundice increases, the bound direct fraction of bilirubin predominates).
In conflict hemolytic jaundice, as in physiological jaundice, free bilirubin predominates; as a rule, there is a Rh conflict or a conflict in the ABO system.
The diagnosis of congenital syphilis, toxoplasmosis and cytomegaly is rejected or confirmed using serological reactions and special tests. If blockage of the bile ducts is suspected, antispasmodics are prescribed; under their influence, the bile ducts expand, the plugs come out, the jaundice quickly passes, and the child recovers.
Differential diagnosis with congenital giant cell hepatitis is possible only by using special research methods - laparoscopy and liver puncture biopsy.
An important role for making a correct diagnosis is played by: biochemical blood testing (total direct and indirect bilirubin is determined) and ultrasound examination.
An operation aimed at restoring the patency of the bile ducts is indicated. In case of total atresia and hypoplasia of the gallbladder, in order to partially divert bile into the intestines and prolong the life of the child, the thoracic lymphatic duct is transplanted into the esophagus.
The results of the operation are directly dependent on the form and degree of the developmental anomaly and the timing of the intervention. The best results can be obtained in the first 2 months of a child’s life.
Size anomalies
Hypoplasia is underdevelopment and can affect the entire saccular organ or its individual segments.
With careful monitoring and the correct diet, it is not a particular problem and is sometimes detected in adulthood.
A giant bladder is detected with any type of modern hardware diagnostics and is characterized by a uniform enlargement of the bladder, but normal dimensions of the biliary tract.
Dwarf - simply reduced in size, maintaining functionality and patency, can lead to the development of dyskinesia, due to the insufficient volume of the reservoir for storing a specific secretion.
Anomalies of gallbladder development
The gallbladder is a reservoir of bile. In newborns it has a spindle-shaped or cylindrical shape. Its bottom does not protrude from under the edge of the liver. In an adult, the length of the bladder is 8-12 cm. The capacity is equal in adults - 30-65 ml, on average 45 ml. The gallbladder is adjacent to the abdominal wall in the place where the angle formed by the costal arch and the outer edge of the rectus abdominis muscle (Ker's point) is located.
Bile is secreted by the liver continuously, but on its way to the duodenum it meets the sphincter, so it is sent to the gallbladder, where the mucous membrane absorbs water and the bile is concentrated 5 times. From 3 to 4.5 liters of provisional bile is secreted per day; it thickens in the gallbladder. If 40 cm 3 of bile accumulates in the gallbladder, its nerve elements are irritated, the muscles are reflexively excited, and the spiral fold relaxes, as a result of which a portion of bile is released into the duodenum. In the same way, bile is released reflexively if food enters the duodenum.
The right and left hepatic ducts unite at the porta hepatis to form the common hepatic duct. The latter merges with the cystic duct, forming the common bile duct. Various options for the relationship between the cystic and common bile ducts are observed. The cystic duct may cross the common bile duct or be located next to it. Sometimes both ducts flow separately into the duodenum.
The common bile duct in half of the cases connects with the pancreatic duct, forming the hepatopancreatic ampulla, which is located in the major duodenal papilla. Here, a special device is formed that regulates the flow of bile and pancreatic juice into the intestines - the sphincter of the hepatopancreatic ampulla, which continues into the sphincter of the common bile duct and the sphincter of the pancreas. The sphincter of the ampulla consists of interwoven bundles of smooth muscle cells running in a circular, longitudinal and oblique direction, covering the ampulla and the terminal sections of the common bile and pancreatic ducts. In newborns and in the thoracic period, the sphincter of the ampulla is poorly developed and is represented mainly by circular muscles. By 2-4 years, the number of muscle cells in it increases, and it acquires a characteristic structure.
1. Agenesis of the gallbladder - it is based on damage to the caudal part of the hepatic diverticulum during the 4th week of embryonic development. There are 2 forms:
A) complete – absence of gall bladder and extrahepatic ducts;
B) while maintaining the biliary tract.
2. Hypoplasia of the gallbladder - manifests itself in the form of a very small bladder.
3. Dystopia of the gallbladder – change in the position of the gallbladder. There are several position options:
B) intraperitoneal (syn. vagus gallbladder) - insufficient fixation of the gallbladder to the liver, when it lies completely outside it, is covered on all sides by the peritoneum and has a mesentery, which can cause volvulus of the gallbladder.
D) under the left lobe of the liver,
D) left-sided with the reverse arrangement of organs.
4. Duplication of the gallbladder - there are several forms:
A) The gallbladder is bilobed - there is a common neck for 2 separate chambers. Drainage can be through a single or double cystic duct.
B) “ductular” gallbladder – true duplication of the gallbladder. At the same time, there are 2 fully formed organs; the cystic ducts independently open into the common bile duct or hepatic ducts.
C) Triplication of the gallbladder - all three organs are located in a common fossa and have a common serous cover.
Studopedia. ru He is not the author of the materials posted. But it provides free use. Is there a copyright violation? Write to us
Laboratory signs of cholestasis:
• increased concentration of conjugated bilirubin in blood serum;
• increased activity of alkaline phosphatase in the blood serum (especially the hepatic isoenzyme);
• increased activity of γ-glutamyl transpeptidase (γ-GTP) in blood serum;
• increased leucine aminopeptidase (LAP) activity in blood serum;
• increased activity of 5#8242;-nucleosidase in blood serum;
• increased concentration of cholesterol in blood serum;
• increased concentration of bile acids in blood serum;
• increased concentration of copper in blood serum;
• increased concentration of urobilinogen in urine. The severity of symptoms can vary significantly across different diseases, from minimal to extremely severe. An additional sign of cholestasis is the presence of thick bile (biliary sludge) in the lumen of the gallbladder. The presence of cholestasis can be reliably confirmed using hepatobiliary scintigraphy: a slowdown in the entry of the radiopharmaceutical into the duodenum is recorded.
In everyday practice, pediatricians most often encounter kinks and constrictions of the gallbladder, which may not have any clinical significance or cause disturbances in the passage of bile. Of particular importance are combinations of kinks that form the so-called S-shaped gallbladder and lead to its dysfunction. Functions of the gallbladder:
• cumulative - accumulation of bile during the interdigestive period;
• concentration - absorption of water;
• reabsorption - reabsorption of amino acids, albumin, inorganic substances;
• contractile - movement of bile along the biliary tract;
• secretory - secretion of mucus, enzymes, electrolytes and
• enzymatic – acceleration of the action of pancreatic lipase;
• hormonal - release of anticholecystokinin;
• regulatory - maintaining a sufficient level of bile components during digestion.
Dysfunctional disorders of the gallbladder and biliary tract in children are a common cause of the development of inflammatory diseases of the biliary system.
Methods for diagnosing anomalies of this organ
It is impossible to detect all such anomalies based on external symptoms, so the use of instrumental diagnostic techniques is required, such as:
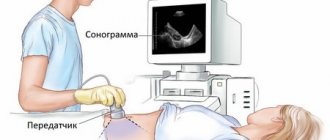
- Ultrasound is the most common technique for detecting deviations from the normal shape of this organ; if such a study does not provide a clear picture, other instrumental studies are used;
- MRI (magnetic resonance imaging) or CT (computed tomography) of the abdominal cavity is the most modern and accurate methods for identifying deviations of this organ from the norm;
- oral cholecystography – involves the use of a contrast agent followed by x-ray examination;
- retrograde endoscopic cholecystopancreatography is also performed using contrast and x-rays, but involves the introduction of a contrast agent through an endoscope from the intestine.
Ultrasound of gallbladder pathologies
In some cases, such anomalies are discovered only during surgery performed on the gallbladder in the treatment of cholelithiasis or cholecystitis.
Associated abnormalities
The most common accompanying deviation is the structure of the bile ducts, which does not correspond to the usual anatomical concept.
It develops in different variants, which can affect the common bile duct connecting the hollow organ with the liver, the bile ducts directed to the intestines and liver.
The appearance of additional segments is also not uncommon:
- atresia - when there is congenital obstruction of the biliary tract and there is an inability to perform functions, it is eliminated by surgery;
- false ducts (2-3, no more), do not give symptoms and often do not serve any purpose, they are simply there;
- stenosis (partial obstruction of the ducts), requires shunting or artificial dilation, but usually develops with existing pathologies of the liver and gallbladder.
There is also biliary sludge, but it is difficult to classify it as an anomaly, although some schools adhere to this view of this phenomenon.
This is most likely a consequence of a diverticulum or constriction. It can be diagnosed when the appearance of sediment at the bottom of the bladder consistently leads to depletion of the walls of the saccular organ, intended for the concentration of bile, inflammation and the appearance of cholelithiasis.
An abnormality of the gallbladder, contrary to popular belief, does not always lead to the need for surgical intervention.
Often, the prescription is made to eliminate the consequences that result from poor nutrition, bad habits and lack of control, which provoke the development of all kinds of complications.
If you follow medical prescriptions and eat the right way (little and small), avoid fatty and sweet foods, and give up bad habits, you can avoid many troubles.