Rehabilitation after laparoscopy of the gallbladder in the postoperative period
Nutrition starts on the second day. Eat simple food for the postoperative period. On this day you will have to limit yourself to low-fat light broth, fruits, light cottage cheese, yogurt.
It is recommended to take food in small quantities, with great frequency: 5-7 meals.
After three days, you can start eating everyday foods. Rough foods, fatty, fried foods, spices, and sauces are excluded. It is not recommended to consume products made from rye flour, or anything that promotes the secretion of bile or gas formation.
It is recommended to switch to nutrition according to therapeutic diet No. 5.
Completely postoperative pain disappears after 24-96 hours. If during this period the pain does not go away, but on the contrary, intensifies, a doctor’s consultation is necessary. Underwear should be soft, should not press or rub the puncture site.
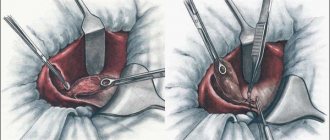
Drainage
In most cases, drainage is required. Its main purpose is to ensure reliable outflow of bile and fluid. Drainage prevents stagnation. If the formation of fluid has decreased and restoration processes have begun, the drainage can be removed.
[37], [38], [39], [40], [41], [42], [43]
Seams
The sutures, unlike abdominal surgery, are small and compact. They do not exceed 1.5-2 cm in diameter. The sutures are removed as the incisions heal. If healing is good, the sutures are removed on the second day; if the speed of recovery processes is low, removal is carried out approximately on the 7-10th day. It all depends on the individual characteristics of the patient.
Scars
The scars after laparoscopy are insignificant, not exceeding 2 cm in size. Four scars remain after the operation. They heal quickly.
How long do you have to lie down after gallbladder removal surgery?
The patient should lie down for a 4-6 hour period. Then you can rise and make slow movements. Quite often they are discharged from the hospital even on the day of surgery.
Consequences and complications after gallbladder removal
A person who is about to undergo surgery to remove the gallbladder must know in advance what consequences are possible in later life and how to avoid them.
It cannot be assumed that after the operation there is a risk of disability - the gallbladder is a fairly important element of the digestive system, but not vital. The body is designed in such a way that, if for some reason it loses such an organ, it compensates for its functions. But it is necessary to take precautions to avoid complications.
Early consequences
Pain after removal of the gallbladder is typical for the first postoperative days. If an open cholecystectomy was performed, the main trouble in the early recovery period is pain from the wound.
Regardless of the type of operation, the patient is bothered by severe physical discomfort - surgical intervention, even at a high professional level, disturbs the internal organs, affecting their functioning. The effects of anesthesia make themselves felt. Dizziness, confusion, weakness, and vomiting are possible.
In addition, after surgery, patients suffering from acute complicated cholecystitis are haunted by phantom pain - it seems that the gallbladder is hurting when it is not there.
Possible complications
During the first days, the patient is under the supervision of a doctor; after discharge home, you need to monitor your well-being independently.
Signs such as low-grade fever (about 37°C) that does not go away for several days, severe cramping pain in the abdomen on the right, reminiscent of colic, vomiting, loose stools, and yellowing of the skin indicate a possible complication. In such cases, you should consult a doctor immediately.
- A poorly performed operation or its performance for emergency reasons without prior preparation can cause the development of biliary peritonitis. Bile enters the abdominal cavity from ligated ducts or with the development of obstructive jaundice.
- Undesirable consequences of the operation include adhesions. The formation of adhesions occurs due to a violation of the integrity of the tissues of internal organs during surgery due to the proliferation of connective tissue. The main symptoms of adhesions: a feeling of tightness inside, stabbing pain. Severe adhesions may require repeat surgery.
- A common complication after gallbladder removal surgery is a cicatricial hernia. The strangulated area of the intestine or omentum protrudes under the skin in the form of a swelling or sac. For some time, a hernia may not cause inconvenience and be painless, but prolonged tissue infringement leads to poor circulation, inflammation, and in advanced cases, the development of necrosis or peritonitis. At the first sign of a hernia, hernioplasty should be performed. A special mesh is placed under the skin directly on the area of the pinched organ to prevent relapse. There is no other treatment other than surgery for this disease. The risk of hernia formation is high in people who are overweight, have flabby, saggy abdominal muscles, or neglect the requirements to prohibit heavy loads. For prevention, they are advised to wear a bandage for several months after surgery.
- Disorders of intestinal motility, which are inevitable in the absence of a gallbladder in the body, often cause persistent constipation, especially if you do not adhere to a healthy diet and regularly snack on fast food, sandwiches or baked goods. If a lack of movement is added to this, the situation may well be complicated by hemorrhoids. The veins of the rectum will be constantly overflowing with blood, will lose tone and will constantly remind themselves of a burning sensation, bleeding, and prolapsed nodes.
The absence of a gallbladder does not affect the amount of bile produced. The only thing that changes is its circulation.
If previously the bile produced by the liver was stored in a bladder, the walls of which absorbed excess moisture, and dosed into the intestines during the digestion of food, now this liquid fills the ducts and can be in the intestines outside of normal hours. Bile acids, passing through the intestines, are not used again and are excreted.
In addition, excessively liquid, immature bile protects the intestines less well from pathogenic microbes. Such disorder provokes the development of a number of digestive tract disorders: dysbiosis, bloating, flatulence, diarrhea, changes in intestinal microflora.
Heartburn after gallbladder removal is not uncommon. Under the influence of aggressive bile acids, the structure and integrity of the mucous membranes of the stomach and intestines can change. Biochemical and physiological changes in bile secretion provoke the development of colitis, gastritis, enteritis, pancreatitis. An exacerbation of pathologies is likely if there is a history of them.
Already in the first days after surgery, most patients experience an expansion of the common bile duct due to increased flow of bile and the absence of a place for its reserve.
Cholecystectomy is a forced measure that relieves a person from the threat of becoming disabled or dying.
If the operation was performed due to cholelithiasis, it should be remembered that the main cause of stone formation is the lithogenicity of bile, which persists even after the operation. This means that stones can form and deposit in the intrahepatic ducts, the common bile duct, which threatens the development of choledocholithiasis.
In order to prevent stone formation and reduce the lithogenicity of bile, Ursosan or Hepatosan are prescribed - drugs based on ursodeoxycholic acid. A lipotropic diet is required - consumption of foods that reduce cholesterol levels in the body. These include egg whites, olive oil, lean fish, green vegetables, and fermented milk drinks.
Lifestyle after surgery
Diet after surgery is not a temporary phenomenon, but a way of life. In the first two months she is strict. Food is taken at the appointed time, in small portions, ideally every 2.5 hours. You’ll have to say goodbye to gastronomic delights and switch to pureed boiled meat and fish, soups with vegetable broths, jelly, and porridge. Eliminate animal fats and sugar, alcohol.
The preferred drinks are still mineral water - table water and medicinal water, herbal teas. In case of insufficient pancreatic function, it is allowed to take enzymes. Any violation of the regimen can cause exacerbation of pancreatitis or peptic ulcer. Over time, you can expand the list of products by gradually introducing salads from raw vegetables and fruits.
You will have to adhere to food restrictions for the rest of your life.
You also need to say goodbye to a sedentary lifestyle. To avoid the formation of adhesions, hernias, constipation, hemorrhoids, it is necessary to move to improve digestive processes. Physical activity should not be strength, but aerobic, that is, stimulate blood circulation and maintain the tone of the cardiac system. It is useful to walk a lot, ski, ride a bike, swim.
Over time, healthy habits will help the body recover properly.
Source: https://ProPechen.com/gallbladder/posledstviya-i-oslozhneniya-posle-udaleniya-zhelchnogo-puzyrya.html
Medications after gallbladder laparoscopy
Sometimes a course of antibiotic therapy may be necessary (if there is an increased risk of infection, during inflammatory processes). Fluoroquinolones, common antibiotics, are often used. When microflora is disturbed, probiotics and prebiotics are used. Such drugs as Linex, Bifidum, Bifidobacterin have proven themselves well.
A multivitamin may be needed. Further therapy is purely individual and depends on existing disorders and risks. For pain, painkillers (ketanal, ketanov) are used, and for spasms, antispasmodics (no-spa, duspatalin, mebeverine) are used.
In the presence of concomitant diseases or complications, etiological or symptomatic therapy is used. So, for pancreatitis, enzyme preparations are used, such as Creon, Pancreatin, Micrazim.
For increased gas formation, drugs such as meteospasmil and espumizan may be useful.
To normalize the functioning of the sphincter and duodenum, motilium, debridate, and cerucal are used.
When using medications, you must always consult your doctor, as self-medication can be dangerous.
How to take Ursosan after laparoscopy of the gallbladder?
Ursosan is a hepatoprotector that protects the liver from adverse effects. They are taken for a long time, from 1 to 6 months. The active ingredient of this drug is ursodeoxycholic acid, which protects the mucous membranes from the toxic effects of bile acids. Use the drug 300-500 mg at night. The drug becomes vitally necessary, since the liver requires even greater protection from bile, which is released directly into the intestine.
Mumiyo
Shilajit is a fairly effective remedy that is used for various diseases. This is an ancient folk medicine that stimulates the digestive organs well. Mumiyo is harmless to the body. After surgery, the dosage of the drug is reduced by 3 times compared to the standard dosage. You should drink mumiyo for 21 days. A repeat course can be taken after 60 days. The course includes 20 g of mumiyo, which is dissolved in 600 ml of water. Apply three times a day. The first week use 1 tsp, the second - 2 tsp, the third week - 3 tsp.
Postoperative complications
Laparoscopy is used to remove the gallbladder.
More often, laparoscopic techniques are used to remove the gallbladder. Despite the minimally invasive nature, tissue injury is possible, so the body’s reaction in the form of slight inflammation is normal. That is why pain under the ribs and throughout the abdomen is not a deviation. A bad sign is increased pain under the ribs. This happens for many reasons, but mostly due to non-compliance with medical recommendations regarding the rules and diet, physical activity.
Often the removed organ continues to be bothered by pain of the same intensity as previously in different parts of the abdomen, under the ribs or shoulder blades. This happens due to the following factors:
- occurrence of complications;
- making mistakes during the intervention;
- exacerbation of existing diseases of the digestive system in a chronic form;
- development of postcholecystectomy syndrome.
Return to contents
What is postcholecystectomy syndrome?
Despite the fact that surgeons call cholecystectomy one of the simplest operations in medical practice, it is associated with the loss of one of the human organs - the gallbladder. And although such an operation allows patients to forget about problems associated with the gallbladder, after it is performed in the human body, there is a violation of the outflow of bile, a malfunction of the digestive system and liver. As a result of such changes, the patient may experience the so-called postcholecystectomy syndrome, which is usually accompanied by pain in the right hypochondrium and abdomen.
Depending on the location of pain after surgery to remove the gallbladder, it can be divided into the following types:
- pancreatic - predominantly localized in the left hypochondrium and back;
- biliary – most often occur in the upper abdomen (in the stomach area) and spread to the right shoulder blade;
- bile-pancreatic - have a girdling character.
Other symptoms of postcholecystectomy syndrome are:
- diarrhea;
- flatulence;
- bitterness in the mouth;
- nausea and vomiting;
- weakness;
- jaundice;
- belching;
- decreased performance.
Lifestyle during rehabilitation
You can return to a normal lifestyle within 3–4 weeks after surgery, but full recovery occurs within 3–6 months, depending on the patient’s condition. At this time, you must adhere to the following rules:
- abstain from intimacy for 2–4 weeks after surgery;
- reduce physical activity to a minimum during the first month;
- do not lift more than 1 kg of weight during the first month, more than 3 kg for three months and more than 5 kg for six months;
- adhere to a rehabilitation diet for the first week after surgery and diet No. 5 according to Pevzner for the next 3–4 months;
- take vitamins and minerals (the choice of a specific drug must be agreed with your doctor).
You should not strain your body for the first month after surgery. Therefore, people suffering from constipation need to take a laxative to soften their stools.
Sometimes, to speed up the patient’s recovery and prevent secondary stone formation already in the bile ducts, doctors prescribe ursodeoxycholic acid.
Why does pain occur after cholecystectomy?
Disorders of the sphincter of Oddi
Answering the question why, after removal of the gallbladder, the right side, stomach, intestines or back hurts, experts in this field note that most often this occurs due to disruption of the sphincter of Oddi - a special muscle formation that controls the flow of bile and gastric juice into the stomach. duodenum. As a result of a decrease in the tone of the sphincter of Oddi, not only bile, but also pathogens enter the intestines and bile ducts. This leads to inflammatory processes.
Damage to the extrahepatic bile ducts
According to many studies, after removal of the diseased organ, there is an increase in the volume of the common bile duct and inflammation of the bile ducts. Most often, this situation occurs due to injury to the bile ducts during surgery or disruption of the drainage process in the postoperative period.
Also, alarming symptoms may occur against the background of the formation of a common bile duct cyst or as a result of a long stump of the bile duct.
However, the most dangerous cause of pain that appears after cholecystectomy is inflammation of the bile ducts (cholangitis), which develops as a result of impaired outflow of bile, its stagnation and the spread of infection along the bile ducts.
Liver diseases
Patients often ask why their liver hurts after gallbladder removal. Typically, pain in the area where the liver is located is associated with a violation of its basic functions. If an inflammatory process occurs in the liver, along with unpleasant and painful sensations in the right hypochondrium, the patient has back pain, lower back pain, and also feels discomfort in the spine. One of the most common causes of such ailments can be fatty hepatosis, which in the postoperative period develops in 42% of patients after cholecystectomy.
Another cause of pain in the liver can be cholelithiasis. Even if the diseased organ is removed, stones may remain in the liver and bile ducts. Small stones can easily pass out of the body along with feces, but large stones can cause blockage of the bile ducts, intestinal obstruction, sepsis, biliary pancreatitis and liver abscess.
Typically, a painful attack lasts 10-20 minutes, occurs after eating or at night, and is accompanied by nausea and vomiting.
Diseases of the gastrointestinal tract
If a person has a stomach ache after removal of the gallbladder, this may be due to the development or exacerbation of concomitant diseases such as ulcers, gastritis or inflammation of the pancreas.
Signs of postcholecystectomy syndrome can also occur against the background of impaired bile passage. After removal of the gallbladder, the main reservoir for bile, it begins to flow uncontrollably into the intestines. As a result of changes in the composition of bile, the body's ability to dissolve bacteria is reduced, intestinal microflora and the metabolism of bile acids are disrupted.
Other causes of pain that occurs after cholecystectomy in the back, abdomen or side may include:
- damage to the intestinal mucosa, small and large intestine;
- an increase in the amount of liver enzymes in the blood;
- damage to neighboring organs during surgery;
- violation of the prescribed regime.
Severe pain may occur due to surgical complications. First of all, we are talking about the formation of postoperative adhesions and scars on the bile ducts.
Also, people who have had a cholecystectomy may experience pain due to inflammation of the scar that is left after the laparotomy. Due to the inflammatory process, pain can radiate to the navel and spread throughout the abdomen. However, with proper care, the surgical suture at the site of the removed organ heals quickly and the pain goes away.
Recovery diet
A restorative diet involves eating only warm cereals and purees, as well as chopped lean meat. For drinks, it is recommended to drink water, herbal teas and chicory. A week after the operation, you can switch to diet No. 5, which provides the following rules:
- you need to eat in small portions (5–6 times a day);
- food cannot be fried;
- meat must be dietary (chicken, turkey, rabbit, beef);
- the consumption of legumes, mushrooms, yeast and various products that cause increased flatulence is prohibited;
- Canned food, alcohol, spicy dressings, sauces and spices, baked goods, cakes, pastries, chocolate, smoked meats, marinades, cocoa, black tea and coffee are excluded;
- sugar should be limited to 25 g per day, and salt to 5 g;
- bread can only be eaten dried (up to 200 g per day);
- It is recommended to drink a glass of low-fat kefir before bed;
- For sweets, honey, marshmallows, jam, jelly, mousses, dry biscuits and oatmeal cookies are allowed;
- You should not eat sour vegetables and fruits.
This diet must be followed to avoid increased secretion, which causes belching and heartburn. The main emphasis should be on vegetables, fruits, cereals and low-fat dairy products. Doctors recommend eating on a schedule. However, after the gallbladder is removed, bile has nowhere to accumulate, so it immediately goes into the duodenum. Because of this, if you experience unpleasant sensations in the pit of your stomach, you need to take a snack in the form of kefir, an apple, or tea with cookies, even if this is not provided for by the established regime.
Doctors advise constantly adhering to diet No. 5, since it is based on the main principles of healthy eating. This is the best preventative against diseases of the liver, stomach and pancreas.
Diagnostic methods
Before treating pain after cholecystectomy, it is necessary to find out the main cause of its occurrence.
The main diagnostic methods are:
- a chemical blood test that allows you to determine the level of liver enzymes and bilirubin, a special bile pigment;
- ultrasound examination, which can be used to assess the condition of the liver, stomach and intestines;
- radionuclide scanning of the hepatic and bile ducts;
- endoscopic retrograde cholangiopancreatography, which allows you to identify abnormalities in the hepatic and bile ducts;
- sphincter of Oddi manometry, which is necessary to measure the pressure in the sphincter;
- CT scan.
Complications of laparoscopic cholecystectomy
This is a minimally invasive method and is preferred due to its high accuracy, small area of damage and quick recovery. However, the risk of complications after laparoscopic removal cannot be excluded. Possible:
- mechanical damage to tissues, organs and blood vessels;
- thermal injuries that occur due to excessive electrocoagulation lead to impaired circulation of the biliary system;
- leakage of bile as a result of damage to the ducts or gallbladder - provokes peritonitis;
- loss of stones from the gallbladder - occurs during resection of the bed or removal of the organ from the abdominal cavity.
The consequences of removal by laparoscopy are associated with insufficient visibility. The doctor sees only a certain area and cannot assess the condition as a whole.
Methods of treatment and prevention
Depending on the cause of pain after removal of the diseased organ, the patient is prescribed drug therapy. In most cases, conservative treatment methods help eliminate pain after cholecystectomy.
To eliminate severe pain in the abdomen and lower back, the doctor prescribes painkillers and antispasmodics (Drotaverine, Bencyclane, Mebeverine). Nitroglycerin will help quickly relieve spasms. However, this drug must be used very carefully, since long-term use of nitroglycerin can negatively affect the cardiovascular system.
Patients may also be recommended special medications aimed at improving the outflow of bile, restoring the functions of the liver, intestines and digestive system organs. First of all, we are talking about choleretic drugs (Panzinorm forte, Allochol) and enzyme preparations (Creon, Pancitrate).
In case of inflammatory processes and the growth of pathogenic bacteria, it may be advisable to use antibiotics (Doxycycline, Intetrix, Furazolidone, Metronidazole). To restore the natural intestinal microflora, along with antibiotics, it is recommended to take probiotics and prebiotics (Hilak-Forte, Linex, etc.).
If the above medications are ineffective, patients are prescribed endoscopic papillosphincterotomy - a small operation that normalizes the outflow of bile and the flow of gastric juice into the duodenum, removes remaining stones in the ducts and thereby eliminates pain. Unlike conventional abdominal surgery, endoscopic papillosphincterotomy is performed using a papillotome, which the surgeon inserts into the major duodenal papilla and makes a bloodless tissue incision.
Exacerbation of diseases
A person who has had their gallbladder removed is likely to develop diseases of the liver, intestines, and pancreas.
The most difficult period of life with a removed gallbladder is considered to be half of the first year after surgery. During this time, old gastrointestinal pathologies may worsen or new ones may develop. Without gall, the first to suffer are:
- liver;
- pancreas;
- duodenum of the intestine.
The following pathologies can cause severe pain under the ribs:
- inflammation of the pancreas (pancreatitis);
- ulcerative lesion of the duodenum;
- adhesions in the bile ducts;
- hepatitis;
- untreated cholelithiasis (remnants of stone in the main bile duct);
- duodenitis;
- biliary dyskinesia.
You can determine which specific disease has worsened by the accompanying symptoms and the nature of the pain, for example:
- if pain occurs in the right side, the stomach, back and collarbone hurt, inflammation of the bile ducts of the liver occurs;
- if pain occurs in the peri-umbilical region and in the left hypochondrium, then the pancreas is inflamed;
- if the pain radiates to the left side and back, then the inflammation affects the spleen or other organs.
Additional symptoms are:
- constant nausea;
- flatulence;
- instability of stool consistency, frequency and color.
If the discomfort does not disappear after 2 days while following a diet, and pain medication does not help, you should immediately consult a doctor.
Return to contents
When should you see a doctor?
Many patients are convinced that if their back hurts after removal of a diseased organ, as well as liver colic and slight pain in the abdomen, this is not a reason for concern. However, in some cases, the patient may urgently need medical attention.
Urgent hospitalization is necessary if:
- pain that is localized in the abdomen, side or back does not go away for a long time;
- a person’s body temperature rapidly rises;
- a painful attack lasts more than 20 minutes;
- pain is accompanied by vomiting.
If people who have had cholecystectomy experience back, abdominal or side pain, it is important to remember that self-medication can be dangerous.
To avoid problems with the biliary tract and reduce the risk of pain, patients who have had their gallbladder removed will benefit from additional preventive measures, in particular, a special diet and split meals. In the postoperative period, which, depending on the complexity of the operation, can last from several months to a year, doctors recommend refraining from eating fatty, spicy and fried foods, and also eliminating spices, seasonings, coffee, alcohol and foods rich in essential oils (garlic) from the diet. , radish and onion).
The main food products in the next few years after cholecystectomy should be soups, boiled meat and fish, baked dishes, vegetables and fruits. If the pancreas is functioning normally, the diet can be supplemented with carbohydrates.
Only timely diagnosis and thorough examination of patients who have had their gallbladder removed will make it possible to quickly and accurately determine the true causes of pain and prescribe effective treatment to completely eliminate the pain syndrome.
Source: albur.ru
Indications for laparoscopy and time after surgery
When this organ becomes diseased, hard compounds called stones form in it. In this case, the gallbladder is removed. Less traumatic is the method of excision of the gallbladder using punctures in the abdominal cavity - laparoscopy.
This method reduces the likelihood of a postoperative hernia. If pain appears in the right hypochondrium, you should consult a doctor, do an ultrasound and rule out gallbladder disease.
In what cases is such an operation prescribed to patients?
- The first day of an attack of acute cholecystitis.
- Calculous cholecystitis.
- Presence of stones in the bile ducts.
- There are stones in the gall bladder, but pain and complications do not appear.
The first week is the postoperative period. After emerging from anesthesia, you should remain in a state of absolute rest for 5-6 hours.
Then you can rise, roll over, and do simple movements. On the first day you cannot eat; you can drink still water or rosehip infusion without sugar. On the second day, you can consume 1-1.5 liters of low-fat kefir or fruit jelly. One serving should not exceed half a glass. The frequency of administration is 1.5-2 hours.
On the third day, you can eat cottage cheese, chopped lean meat, broth, fruits, and dairy products in small portions. You should drink a lot between meals. In the following days, food is normal, with the exception of spicy and salty foods and black bread. The injection sites will hurt for some time until the injured tissues heal.
You cannot give your body physical activity. Linen should be soft and made from natural fabrics.
The postoperative period ends with the removal of stitches from the punctures on the abdomen. After discharge from the hospital, the patient remains on sick leave for some time (10-12 days) until the external and internal wounds are completely healed.
Sometimes complications appear in the form of compactions, redness or discharge from the puncture sites, then the treatment is prolonged. A postoperative complication can be expressed as a hernia in the scar area. A hernia is painful if strangulated, accompanied by vomiting and lack of stool. It can occur if a gentle regime of physical activity is not observed. The puncture sites are treated with iodine. They can be wetted after 5 days.
Pain in the first period is successfully relieved by taking analgesics. If everything is normal, then the need for them disappears. During the operation, a hollow space is created in the abdomen by pumping carbon dioxide. This can cause pain in the supraclavicular area.
During the postoperative period, you can offer the patient the following dishes:
- Vegetable puree soup with lean broth.
- Steamed omelette.
- Mashed potatoes with the addition of carrots, beets or pumpkin.
- Ground boiled rabbit or turkey meat.
- Dishes made from low-fat cottage cheese.
- Low-fat boiled fish.
- Jelly or mousse from non-acidic fruits.
- Tea.
Bread is introduced into the diet gradually in the form of wheat crackers soaked in broth or tea. Among porridges, preference should be given to buckwheat and oatmeal porridge with water.
Postoperative period
Immediately after the operation, the surgical patient is transferred to intensive care or a regular therapeutic ward. The duration of the recovery period depends on the volume and method of surgical intervention, as well as on the general health of the patient. Typically, the rehabilitation period after laparoscopic cholecystectomy is 1-2 days, after laparotomy - a week. The patient can be discharged from the hospital after he is able to eat on his own.
Postoperative period
After the surgical removal procedures are completed, the postoperative period begins. It involves staying in the intensive care unit for 3-4 hours. Intensive care staff closely monitor the condition of the admitted patient, in particular, how he recovers from anesthesia. After reaching a satisfactory condition, the doctors in the intensive care unit transfer the operated person to the ward. Here he will spend the next few days.
For the first 4-5 hours, the patient should lie in absolute peace, preferably without moving. Drinking, eating and trying to get up is prohibited. After about 6 hours, the patient is allowed to drink plain water without gas or additives. The liquid should enter the body in small portions, that is, you can drink in small sips. The interval between drinks is 7-10 minutes. You are allowed to start eating only one day after surgery.
On the second day after the procedure, the patient is allowed to stand up. This should only be done under the supervision of hospital medical personnel. After 2 days, you are allowed to take liquid food and walk on your own.
Complications and medical errors
Laparoscopic surgery to remove the gallbladder is simple and safe, but there are risks. Common medical mistakes that lead to complications include:
- placing bad stitches;
- insufficient sanitation of the peritoneum at the site of the removed bladder;
- affecting nearby tissues and organs with their damage.
After surgery, the patient may experience constant pain.
Complications arise mainly in the presence of anatomical features of the biliary tract. Often, laparoscopy reveals severe damage to blood vessels or nearby organs, which requires open surgery. Pain due to complications and medical errors is as follows:
- constant severe pain under the ribs due to leaking stitches on the bile ducts;
- diffuse, aching (dull) pain throughout the abdomen due to infection of the wound, which is caused by insufficient sanitation of the peritoneum;
- pain under the shoulder blade due to cardiac dysfunction.
- pain in the navel and right side;
- inflammation of the stitches with redness and swelling;
- severe increase in body temperature;
- chills, fever and other signs of poisoning.
When the gallstone is removed, the suture heals quickly. Persistent pain in the hypochondrium and right side indicates a narrowing or spasm of the bile duct, its irritation by the remains of stones, and the aggressive effect of bile on the intestines. It is possible to form a fistula from the remnant of the bile duct. Urgent hospitalization is required if:
- severe malaise with progressive deterioration;
- heat, chills, fever;
- purulent discharge, bleeding from a sutured incision;
- sealing the edges of the sutured wound;
- pain that cannot be controlled by medication.
Return to contents
Poor nutrition
Table No. 5 is most suitable for diet therapy
The digestive organs react especially acutely to the quality and quantity of food after surgery. Regular food is the main reason for the deterioration of the condition and slowdown of the rehabilitation process. Important nuances to consider during diet therapy:
- Do not eat or drink cold food with liquid. This can provoke a gastric spasm, which will reflexively affect the bile ducts and sphincters.
- You can't overeat. Excessive amounts of food consumed at one time make it difficult to digest and evacuate the food bolus from the stomach. As a result, bile does not enter the intestines.
- Fatty, spicy, fried and other unhealthy foods should be excluded from the diet. This applies to lard, margarine, concentrated broths, beer, wines, syrups, vinegar, and sweets. Such foods are especially difficult for the stomach in the postoperative period. After consuming even a small amount, a spasm of the bile ducts may occur, which will manifest itself as pain on the right under the ribs or in the pit of the stomach.
- The most suitable diet is table No. 5. The goal of diet therapy is to restore the function of the liver and pancreas and relieve inflammation in the biliary tract.
- It is important to maintain a fractional diet - up to 7 times in small portions.
Return to contents