Characteristics of colon adenomas
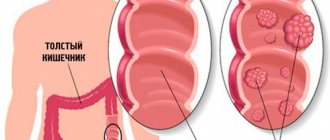
A polyp is a fleshy formation on a thin or thick stalk. The growth develops from the epithelium and protrudes above the mucous membrane in the intestinal lumen. It is often injured during the passage of feces, which is why blood or dark mucus can be found in the feces.
Tubular adenoma of the colon in appearance resembles a loose red tube (Latin Tubulus - tubulo), sphere, oval, mushroom. It consists of connective tissue and has glandular branches. The adenoma is sharply limited and, as it grows, acquires a crimson color. The tumor grows slowly, reaching a diameter of 1 cm. Then such a tumor can become larger and mutate into a malignant form.
Villous adenomas occur in 5 cases out of every 100 visits. They can be dense or thin fleshy finger-like projections located close to each other. Polyps grow along the lower intestine (rectum or colon), occupying an area of more than 1 square meter. cm, tend to transform into a malignant form. A group of tumors in appearance resembles a fuzzy carpet or seaweed.
With tubular villous adenoma, the neoplasm combines two previous types of polyps . That is, it includes round tubular and thread-like forms, grows up to 3 cm, and over time turns into a malignant neoplasm.
Doctors recommend removing all types of polyps to reduce the risk of cancer. If the adenoma is small, then specialists may prescribe its excision. The procedure is performed directly during a diagnostic colonoscopy during the initial examination. If the glandular epithelium is pathologically modified, that is, dysplasia of glandulocytes (secretory cells) has occurred, which means that the neoplasm could begin to transform into a cancerous tumor. In this case, additional studies are carried out and the patient is recommended to undergo surgery.
Symptoms of the disease
At an early stage, the disease practically does not manifest itself at all. A villous polyp makes itself felt only when its size approaches one centimeter. The first symptom is bleeding. The blood may be light or bright red.
The functionality of the digestive tract is not impaired, since the formation does not lead to the development of additional diseases.
If the fleecy polyp has become more than one centimeter in diameter, then the patient experiences constipation. If the tumor appears in the area of the rectum, sigmoid or colon, the patient complains of discomfort in the anal area and bloating.
The most dangerous types of the disease include tubular villous and serrated adenoma of the colon. They are the ones who transform into cancerous tumors. Characterized by three degrees of dysplasia. In appearance they resemble raspberries with a fuzzy surface. They grow up to 3 centimeters. The cancer process begins after 2-3 years. The tumor can only be removed surgically.
Causes of pathology
Mixed, villous or tubular adenomas develop more often in people who are genetically predisposed to its formation. In this case, we are talking about heredity, when this pathology, familial polyposis or similar diseases have already been recorded in a person’s family.
Indirect causes of intestinal tumor development:
- congestion in the pelvic organs, physical inactivity;
- smoking and other bad habits;
- chronic diseases of the stomach or gastrointestinal tract;
- metabolic disorders, intracellular metabolism, etc.;
- working and/or living in a poor ecological area;
- work in hazardous industries;
- chemical poisoning;
- eating poor quality food, unhealthy diet.
The listed factors can provoke dysfunction of the organs of the digestive system, worsen peristalsis, and clog the mucous membrane of the gastrointestinal tract with decay products (“slags”). They are considered the main lever capable of triggering cell transformation and tumor formation. As for the direct reasons due to which intestinal adenoma is formed, WHO specialists and evidence-based medicine have not identified them.
Causes of adenomas in the intestines
- Bodily diseases;
- Consumption of foods with a large amount of calories and carcinogens, which impair intestinal function and contribute to the appearance of adenomas;
- Polluted environment;
- Abuse of alcoholic beverages, smoking;
- Chronic and acute gastrointestinal diseases;
- Toxin poisoning;
- Activities in hazardous industries;
- Physical inactivity;
- Heredity.
When polyps increase in size, characteristic signs of neoplasms appear:
- The process of defecation is accompanied by pain;
- There is discomfort and sharp pain in the lower abdomen;
- Flatulence;
- The stool is full of mucus and blood clots;
- Alternating constipation with diarrhea.
Scientists have not yet figured out the exact etiological factor contributing to the development of intestinal adenomas. There are several theories about the occurrence of benign neoplasms. Most doctors believe that a combination of several factors plays a leading role in the occurrence of this disease. Based on this, there are several reasons for the appearance of tubular adenoma:
- Genetic predisposition. Heredity is of great importance in the occurrence of intestinal polyps. In some cases, tubular adenomas are detected in several family members.
- Nature of nutrition. It is believed that people whose diet contains a large amount of animal fats are prone to the appearance of both benign neoplasms and gastrointestinal cancer. In turn, the risk of developing these pathologies is reduced by consuming vegetables, herbs, and foods rich in fiber.
- Bad habits.
- Exposure to the body of various chemical agents and ionizing radiation.
- Stressful situations.
Most often, tubular adenoma occurs in elderly people. Due to the fact that this group of people has an increased risk of developing intestinal cancer, polyps are subject to mandatory removal.
Symptoms of pathology
Typically, tubular villous adenomas are asymptomatic. When the intestinal tumor reaches about 2 cm, a person may feel discomfort during bowel movements. In this case, the main symptom of the disease is the appearance of blood in the stool when the tumor is injured by moving feces.
Other signs of adenoma:
- pain in the lower abdomen, especially during bowel movements;
- itching of the anus;
- feeling as if there is a foreign body inside the intestine;
- an abundance of clear or white mucus in the stool;
- stool disorders (constipation and diarrhea alternate for no reason).
Since the formation of a tumor is asymptomatic, in most cases it is discovered during a routine or comprehensive examination, when other diseases are being looked for.
For colon adenoma, doctors analyze the degree of dysplasia:
- In stage 1, epithelial cells begin to steadily divide. There are no other symptoms of tumor development.
- At grade 2, there is a moderate increase in dysplasia. Cells divide quickly, the boundaries of the layers are hardly noticeable.
- Doctors equate stage 3 to the precancerous stage of the disease. Cells multiply intensively, their structure changes, and the transformation process becomes irreversible.
If the pathology is not treated, the adenoma continues to grow until it blocks the intestinal lumen. Then the symptoms inherent in complications of the neoplasm are added.
Complications
One of the most dangerous consequences is the process of malignancy, when benign cells begin to transform into malignant ones.
After surgery, complications may occur in the form of bleeding from the anus.
Perforation of the intestinal walls cannot be ruled out, which can occur against the background of a burn during electrocoagulation.
In addition, if the disease is not treated in time, the cellular structures continue to grow, which leads to blockage of the intestinal lumen. As a result, intestinal obstruction develops.
Treatment of pathology
During diagnosis, doctors need to differentiate an adenomatous polyp from adenoma and other similar neoplasms. This is necessary for the correct selection of methods for removing the growth(s).
Types of surgery:
- transanal excision (the stalk of the polyp is cut off with a laser or surgical instrument);
- electrocoagulation (throw a loop under the growth and cauterize it with an electric current);
- colotomy (abdominal surgery to remove adenoma);
- resection (a piece of intestine with a tumor is cut out and the remaining 2 parts are sewn together);
- extirpation (complete removal) of the rectum with a neoplasm.
At an early stage of the disease, treatment with medications is possible. Often, suppositories are prescribed for adenoma, for example, “Chistobolin”. They are administered using a sigmoidoscope after a cleansing enema. If epithelial dysplasia or other contraindications are absent, the doctor may allow the additional use of traditional medicine . A good result is obtained by using an enema with a decoction of celandine. The procedure is carried out every other day for a month.
Types of colon adenomas
- Tubular adenoma or polyp is a benign formation that grows slowly and has clear boundaries. Reaches a size of up to 1 cm. A detailed examination reveals a red tumor. As the adenoma grows, it can become crimson and rise above the level of the colon on a thin stalk. Tubular adenoma has glandular branches and loose connective tissue. It is necessary to treat such a polyp, as it tends to transform into cancer. It can also provoke abnormal development of epithelial cells;
- villous adenoma - similar in appearance to seaweed, where papillae in the form of a pile are located in the upper part. It grows along the rectum or colon, reaching quite large sizes. May degenerate into cancer;
Location of the rectum
The main difference between a villous adenoma and a tubular one is that a villous tumor never develops on a thin stalk, bleeds easily under mechanical influence, and has a lobular structure. It is also worth noting that tubular adenoma eventually turns into villous adenoma.
The structure of villous adenoma
Villous adenoma is covered with villi of varying lengths, which have a tree-like structure. They also have dense columnar epithelium with specific goblet cells. Villous adenoma has an elongated round shape with a velvety surface of a red-pink color. The tumor villi are lighter in color. The consistency of the formation is pliable and quite soft, which moves easily during palpation.
Classification of adenoma by the nature of formation:
- nodular adenoma is the most commonly diagnosed case. It looks like a tumor growing on a broad base;
- creeping adenoma - grows on the surface of the colon mucosa, affecting its individual areas.
The mucous membrane around the formation always remains the same color as healthy tissue. However, in some cases, between the tumor and the colon itself, the cells become paler. As a rule, this concerns creeping adenoma.
Types of villous tumors:
- adenoma - is the result of hyperplastic transformations of villous polyps, which have a slow growth rate and remain without any significant changes for a long time;
Villous adenoma of the rectum
It is quite difficult to establish the exact cause that provokes the development of villous adenoma, but doctors have identified a certain pattern.
In the first stages, benign tumors occur without any special symptoms and are discovered randomly during a routine endoscopic examination. When villous adenoma grows to 2-3 cm, pathological changes begin to occur in the human body:
- During defecation, mucus appears, which is released from the papillae of the tumor. It is a rather dangerous sign;
- bleeding may indicate both benign tumors and other proctological problems, so this sign cannot be called unambiguous;
- constipation as a result of intestinal obstruction. Appear when the tumor increases significantly;
- pain in the abdominal area usually appears after damage to the formation of the colon.
Treatment of serrated adenoma of the colon
Colon adenoma is extremely dangerous, as there is an increased risk of developing into cancer.
Symptoms appear even in the early stages and interfere with the patient’s usual lifestyle. Most often, a patient turns to a proctologist only when the pathology has reached advanced stages and affects internal organs. Feces collect in the large intestine. This internal organ consists of a sigmoid, transverse and blind section. A polyp can form in any of the departments, but most often it is found in the sigmoid. In advanced cases, colon carcinoma develops.
There are 3 histological types of colon adenomas:
- Tubular;
- Tubular villous;
- Villous.
The separation criterion is the ratio of villous and tubular structures. Tubular adenoma of the colon - what is it? Microscopically, tubular adenoma is represented by proliferating adenomatous epithelium. The tumor consists of branching and significantly convoluted glandular tubes, longer than in the normal intestinal mucosa.
In tubular adenoma, no more than 25% villous tissue is present. Tubular adenoma of the colon has a mucous membrane-covered base. It is represented by connective tissue, smooth muscle cells and blood vessels. Tubular adenomas have a stalk and a smooth lobulated surface. Less often they are located on a wide base. Creeping tubular adenomas, which protrude slightly above the surface of the mucous membrane, are very rare.
In tubular-villous adenomas, the number of villi increases, which can be detected both on the surface of the polyp and inside large glands. The glands lengthen, acquire an irregular shape, and fit tightly to each other. The degree of epithelial dysplasia increases. In tubular-villous adenoma, the percentage of villous tissue varies from 25 to 75%. The tumor consists of pronounced lobules and has small areas with villi or very small lobules.
Villous adenoma consists of thin finger-like outgrowths of the connective tissue of the lamina propria, which are covered with epithelium. In villous adenomas, a small number of glands and 75% of the villous component can be found. Macroscopically, villous adenomas have a wide base and a “shaggy” surface.
Adenomatous epithelium belongs to the category of neoplastic. For this reason, each adenoma has signs of dysplasia of varying severity. Histologists distinguish 3 degrees of dysplasia of tubular adenoma of the colon:
- 1st degree – weak;
- 2 degrees – moderate;
- Grade 3 – severe.
Tubular adenoma of the colon with low grade dysplasia is a poorly differentiated tumor. It can transform into adenocarcinoma.
Histologists distinguish the following types of malignant neoplasms of the large intestine:
- Well-differentiated colon adenocarcinoma;
- Moderately differentiated colon adenocarcinoma g2;
- Poorly differentiated adenoma.
Glandular cancer can generally be represented by the following types of colon carcinomas: tubular, mucinous, signet ring cell, squamous cell. Tubular adenocarcinomas consist of tubular structures. Tumors of this type occur in more than 50% of patients with glandular cancer. They have blurred contours and small sizes.
Mucinous adenocarcinoma consists of mucous components and epithelial structures and has no defined boundaries. Metastasis occurs through the lymphogenous route. The high risk of recurrence is due to insensitivity to radiotherapy.
Signet ring cell adenocarcinomas are characterized by a highly aggressive clinical course. Most patients with tumors of this type, who seek medical help at the Yusupov Hospital for the first time, already have metastases in the lymph nodes and liver. Oncological disease is most often observed in young patients.
Squamous cell adenocarcinomas form in the area of the anal canal. The tumor consists of flat epithelial cells. The clinical course of squamous cell adenocarcinomas is characterized by a high level of malignancy. They often recur, growing into the tissue of the vagina, ureters, bladder, and prostate gland. The five-year survival rate for squamous cell adenocarcinomas does not exceed 30%.
The development of tubular adenoma of the colon is promoted by nutritional factors: high fat content and low dietary fiber. Changes in diet affect the likelihood of developing adenoma and adenocarcinoma. Refined fats can disrupt the proliferation of epithelial cells.
The individual risk of developing colon adenoma increases in first-degree relatives of patients with colorectal cancer. The likelihood of developing colorectal carcinomas increases if a person has first-degree relatives diagnosed with colon cancer before the age of 50 years.
An increase in the size of the polyp, the number of villi and severe dysplasia increase the risk of malignancy of colon adenoma. According to statistics, 4.8% of tubular, 22.5% of tubular villous and 40.7% of villous adenomas are converted into adenocarcinoma. The risk of transformation of benign neoplasms into malignant tumors increases with the degree of dysplasia.
Villous, tubulovillous adenomas, and adenomas larger than 1 cm increase the risk of subsequent development of colon adenocarcinoma. This risk is higher in patients with multiple polyps.
Most colon adenomas do not manifest themselves clinically. They are discovered incidentally during screening tests or examinations for complaints that are not related to them. Sometimes adenomas cause significant bleeding or lead to chronic anemia due to prolonged hidden blood loss.
Doctors at the Yusupov Hospital identify colon adenomas using sigmoidoscopy and colonoscopy. Adenoma of the large intestine most often takes the form of a polyp located on a broad base or connected to the intestinal wall with a pedicle. Its stalk length depends on the growth rate of the polyp localization. Rapidly growing adenomas have a wide base. Slowly growing ones are located on a stalk, which is formed as a result of peristalsis and stretching of the polyp by a peristaltic wave.
Some colon adenomas have a deepened or flat appearance. They do not rise above the surface of the mucous membrane. They can be visually identified by changes in color, structure of the mucous membrane, and the absence of a capillary network. The Yusupov Hospital uses a simple and effective method for their identification - chromoscopy with indigo carmine.
In general, an adenoma is a benign neoplasm that develops from glandular epithelial cells. The latter are found in all glands of the body (salivary, mammary, pituitary gland and others) and also line the mucous membranes.
Adenoma of the large intestine is a growth of glandular tissue over the mucosa, which can be attached to the membrane with a thin stalk (have a “pedicle”), or look like a “tubercle” (polyp with a wide base).
In addition to adenomatous ones (accounting for 10% of all polyps), hyperplastic, inflammatory and hamartomatous polyps can occur in the colon, the difference between which is the low likelihood of transformation into oncological pathology.
Reference! According to statistics, approximately 50% of people over 60 years of age have at least one adenoma of 1 cm in diameter. Moreover, in 90% of cases these are small tumors with a low risk of malignant transformation, and only in 10% are tumors larger than 1 cm with a risk of developing colon cancer (which also occurs in only 10% of cases, even with bulky tumors).
Differentiation of all identified colon adenomas by location gives the following picture:
- rectal adenoma – 25%;
- colon adenoma – 67%, of which in the sigmoid colon – 25%, descending colon – 18%, ascending colon – 13%, transverse colon – 11%;
- adenoma of the cecum – 7%.
The likelihood of developing oncological pathology is directly related to the type of adenomatous polyp detected.
Tubular adenoma
The most common variety (can also be called tubular) is characterized by the following features:
- the neoplasm is soft, with a smooth red surface, with clear boundaries and a wide base. Consists of glandular and loose connective tissue;
- size – most often 10-12 mm, rarely – up to 30 mm.
- the likelihood of cancerous degeneration is low.
Having reached 3 cm, the adenoma can split into lobes, acquire a crimson hue and the appearance of a “leg”. The appearance of villous character and malignant potential is also possible.
Villous adenoma
Neoplasms of this type are most often found on the surface of the rectum, their characteristics will be as follows:
- the tumor is soft, with a “velveteen” surface, may externally resemble cauliflower, and is formed from villi of fibrous tissue, epithelium and mucosa. In most cases, the adenoma “spreads” over the surface of the intestine, slightly rising above it, less often it has a thick or thin stalk;
- dimensions - up to 2 cm, sometimes reaches 3 and rarely - 10 cm;
- the probability of degeneration is higher than that of all other types.
Attention! A third of patients with this type of adenoma were found to have fragments of non-invasive intraepithelial cancer, and the other third had invasive malignant changes.
Diagnostics
Diagnosis of villous adenoma of the rectum is made using colonoscopy, as well as x-rays. In some cases, x-ray examination may not be informative, since small tumors may not be visualized. Only in the case of the presence of glassy mucus secretions, the X-ray diagnosis is repeated after 1-2 months.
An adenoma that begins to degenerate into cancer significantly changes its appearance: shape, structure, color. Tumors also appear, forming necrotic and fibrous deposits. Deformation of the rectum is possible, which causes unusual bends and narrowing of the lumen.
Also, to diagnose a villous tumor, a histological examination is performed. Sometimes this is quite difficult to do, since at the slightest touch the adenomas begin to bleed.
The most common method for removing villous adenomas is endoscopic. At first, treatment is carried out without excision of part of the colon, but if the slightest signs of malignancy are detected, resection is required.
If the tumor begins to block the lumen of the rectum and it is not possible to get to the site of the lesion endoscopically, surgical intervention is performed.
Gastritis is one of the most common gastrointestinal diseases. People who prefer snacks and abuse spicy and fatty foods are at risk. For those patients who suffer from stomach diseases, diet number 1a has been developed. It is tougher than others and does not allow the digestive tract to be restored. General principles of the diet There are two main...
Biliary reflux gastritis is a pathological condition during which the remains of undigested food in the intestine are thrown back into the epigastric cavity, provoking the process of inflammation in the gastric mucosa. Inflammatory changes in the coolant are called “esophagitis.” General features of the disease There are two types of reflux: biliary - from the bile ducts duodenal - from the intestines Bile acids that enter...
Gastritis is an inflammatory, often infectious disease of the gastric mucosa. The reasons for its development are varied, ranging from poor nutrition to central nervous system disorders. Considering the duration and main symptoms, the disease is divided into the following forms: acute and chronic. The chronic form of the disease can lead to disruption of the gastric mucosa (GMT), and can also become the main…
Adenomas of the gastrointestinal tract are commonly called polyps. A polyp forms on the mucous epithelium of the stomach and intestines. Among the patients, the most common are patients with tubular adenoma, with and without dysplasia, villous adenoma, and tubulovillous adenoma. Most polyps that form on the mucous membranes of the digestive tract have the ability to develop into malignant formations. Therefore, it is so important to provide timely diagnosis and treatment of the patient.
This article provides brief information about tubular adenoma, villous adenoma, and tubular villous adenoma. The features of these polyps and methods of their treatment are presented.
Types of disease
The type of polyps depends on a number of signs:
- Size.
- Architecture.
- External features.
- Quantity.
Tubular adenoma of the intestine in section
- Tubular type of adenoma with dysplasia. The most common variety. Localization is possible in the colon or sigmoid colon, also in the stomach. Characterized by the appearance of small tumors. Most often does not exceed a centimeter. The surface of the tumor is smooth with clearly defined boundaries.
- Villous. It is called so because the tumor is formed from the villi covering the mucous membrane of the gastrointestinal tract. A dangerous type of disease. This is due to the rapid progression of the disease, which activates oncological processes in the body. The new growths are soft in structure and have a velvety surface. Can form in the cecum.
- Tubular-villous. In medical practice it is observed quite rarely. The size of the tumor in the detailed type of adenoma reaches 2.5 cm.
The papillary type of adenoma can develop in organs with glandular epithelium. Characterized by papillary growths.
It is important to establish the type of disease during diagnosis. This will prevent possible complications.
Tubular adenoma
A tubular polyp, like most benign tumors, grows slowly. When small in size (up to 1 cm), tubular adenoma is clearly defined and red in color. Growing, the adenoma acquires a rich crimson color and rises with the help of a stalk. Among patients with this type of polit, the most common is tubular adenoma of the colon, less commonly tubular adenoma of the sigmoid gland and tubular adenoma of the stomach. The structure of such an adenoma consists of glandular branches bounded by loose connective tissues (80% of the total composition of tubular adenoma of the colon). Treatment of this polit is strictly necessary, since it has malignancy (precancerous condition).
What treatment methods are suitable for tubular adenoma of the colon? Treatment is exclusively surgical. Since the use of medications will only delay the symptoms for some time. However, there are several options among surgical methods. Tubular adenoma of the colon, treatment:
- Transanal method of microsurgical removal of a tubular polyp using an endoscope.
- If there are many pedunculated polyps, it is recommended to remove them using electrocoagulation. In this way, the polyps are removed, and their legs can be docked.
- If the polyps reach large sizes and affect the intestinal tissue, then in this case the tubular adenoma of the colon (surgical treatment) undergoes resection of the polyp and the part of the intestine that was damaged.
Tubular adenoma of the sigmoid colon causes acute lesions of the human digestive tract. The development of tubular adenoma of the sigmoid colon is facilitated by dysplasia of tumor cells.
Tubular adenoma of the sigmoid colon requires only surgical intervention. Tubular adenoma of the stomach can cause obstruction of the digestive process, tubular (tubular) structures contribute to this pathology. The papillary structure of gastric tubular adenoma grows slowly. Only surgical intervention is required for tubular adenoma of the stomach, since other methods do not achieve the desired treatment result.
Villous adenoma
Villous adenoma looks similar to seaweed; on the surface there are papillae resembling pile. Has a soft consistency. It grows along the mucous membrane of the colon and can reach large sizes. Often does not have a clearly defined form. Villous adenoma is usually manifested by copious mucus discharge, which can be found in the stool.
Villous adenomas of the rectum are common. Their occurrence is the result of inflammatory processes not only in the rectum, but in the intestine as a whole. Villous adenoma of the rectum is removed using endoscopy. The operation is relatively simple if the villous adenoma of the rectum has not become malignant and is small in size. Large polyps are removed surgically. If after examination it is discovered that the villous adenoma of the rectum has managed to acquire malignant components, then the affected part of the large intestine is removed.
Tubular villous adenoma
Tubular villous adenoma is similar in structure to both adenomas mentioned above. The histological structure of such a polyp resembles both a villous and a tubular polyp. Tubulovillous adenoma has three degrees of dysplasia: mild, moderate, severe.
The most common polyps are 2-3 cm in size. Tubular villous adenoma is found in the large intestine, sigmoid colon. They can transform from benign to malignant tumors. Tubulovillous adenoma requires surgical intervention: endoscopic for small sizes, classical surgical for large sizes.
Tubular adenoma of the colon has another name: polypoid adenoma. Initially, this is a benign process, which, in the absence of proper treatment, degenerates into oncology. The tumor reaches 1 cm in diameter and develops against the background of adenomatous polyps.
The exact cause of the appearance of polyps in the large intestine has not been established. Doctors suggest that a hereditary factor plays an important role. Another argument from doctors is somatic diseases that can provoke the appearance of tubular adenoma.
The following disturbances in human behavior serve as secondary factors influencing the development of the disease:
- Errors in nutrition that disrupt the functioning of the entire digestive tract. Consumption of carcinogens, fatty foods, and low amounts of fiber reduce intestinal motility. As a result, its microflora suffers, which provokes the appearance of adenomas.
- Bad ecology.
- Having bad habits.
- Human activities associated with contact with toxic substances.
- Other gastrointestinal diseases.
- Lack of physical activity.
Polyposis at the very beginning with small adenomas occurs without visible symptoms. The disease may be discovered by chance when diagnosis is being made for other reasons. As tubular adenoma develops, a person may notice scarlet blood streaks in the stool. But disruptions in the functioning of the gastrointestinal tract have not yet been observed.
When polyps begin to grow, the following signs of disease appear:
- During defecation, mucous blood is found in the stool.
- There is discomfort in the anal area.
- During defecation, pain is felt in the rectal area.
- Itching is felt in the anus area.
- The appearance of constipation or loose stools.
- Abdominal pain.
- Due to the fact that gases pass through the intestines with difficulty, bloating is felt.
Such symptoms can occur individually or be present in combination. If you find yourself with at least one of the listed signs, then consult a doctor.
Causes of serrated adenoma
The exact cause of the development of the disease is still unknown to science, despite numerous studies. Scientists were able to identify the main factors in the development of the disease. The main reason is infection in the intestines and the occurrence of further inflammatory processes.
Factors causing serrated adenoma also include:
- Stress. Constant nervousness contributes to the development of many diseases.
- Poor nutrition. Harmful foods, like an unbalanced diet, lead to improper functioning of internal organs. Gastrointestinal diseases activate the process of tumor formation.
- Bad habits. Alcohol and smoking have a negative effect on all internal organs.
- Lack of physical activity. A sedentary lifestyle leads to disruptions in the gastrointestinal tract.
- Working conditions. Contact with toxic materials and toxic substances disrupts the amount of essential microelements. This changes the structure of cells, which ultimately triggers the development of serrated tumors in the intestines.
- Obesity. People who are overweight are more susceptible to tumors and cancer processes. The reason is insufficient intake of vitamins and microelements into the body, as well as their poor absorption.
- Bad ecology. Due to environmental degradation, the environment has a destructive effect on the body. Human immunity decreases. This causes serious negative changes in the cells of the body, causing the development of the disease.
- Heredity. Scientists have found that genetics also influences the development of precancerous pathologies. If parents are diagnosed with this disease, over time, children become prone to developing it.
We invite you to familiarize yourself with the Bicycle and the Prostate - 5 Basic Prevention Recommendations
Diagnostics
Despite the complexity of the diagnosis, tubular adenoma of the rectum is not so rare. To identify the disease, you need to consult a proctologist. He initially examines the patient and performs a digital examination of the rectum.
If there is a suspicion of the presence of a tubular adenoma, the patient is referred for an instrumental examination.
Many will ask the question, why don’t they take blood and stool tests? For this disease, this type of research is uninformative. It is only possible to identify the presence of a somatic disease, due to which an adenoma appeared in the colon.
If the adenoma is located in the duodenum or in the intestine, then the ultrasound method is used. It provides complete information about the location of the tumor. For tubular adenoma of the sigmoid colon, an effective method for detecting the disease is sigmoidoscopy. A mini camera is inserted into the anus, which can examine the internal organs, while all their contents are displayed on the computer monitor screen. Using irrigoscopy, all parts of the large intestine are assessed. This is the rectum, cecum, descending colon, etc.
It happens that the above methods are prohibited for health reasons. In this case, magnetic resonance imaging is used.
Treatment is surgical. Serrated adenoma of the colon is also removed surgically. Drug treatment in this case is powerless. When the polyps have already been removed, they are sent for diagnostics in order to identify their malignant nature. It is not always possible to detect cancer before surgery, since cancer cells can be located inside the polyps themselves. When the tumor has already been removed, conservative treatment is carried out.
As a complication of any operation, it is possible that bleeding may begin, which may occur even after several weeks.
Traditional medicine is also powerless for tubular adenoma of the colon; it not only cannot save you from the disease, but can also aggravate the situation, delaying time and leading to the growth of cancer cells. If the growths in the large intestine are small, doctors do not decide to remove them immediately. In this case, an observation tactic is chosen when the patient is constantly monitored for the growth of adenomas. And only if they begin to actively grow, surgery is performed.
Recently, the method of electrocoagulation has become popular. The procedure is much more effective and safer than conventional surgery. But after the procedure, a histological examination of the removed tissue will be required.
Resection of part of the intestine is necessary if the formation is malignant. But first, partial excision of the affected tissue is carried out and an analysis is carried out for the presence of malignancy. Large polyps are removed in parts.
If polyps are detected in the anus, it is prohibited to remove them using electrocoagulation. Since healing in this place will be long and a complication may develop.
The prognosis of the disease will be favorable if it was possible to detect an adenoma at the initial stage of its development. It is known that such a neoplasm becomes malignant over time. Therefore, you should regularly undergo preventive examinations from doctors of all specialties.
If you notice problems with your intestines, do not self-medicate, but once again consult your doctor on this issue.
After surgery to remove a polyp larger than 2 cm, a control colonoscopy is performed to identify residual tissue. After this, the patient will need to be examined every 6 months, since the possibility of relapses cannot be ruled out. But with high-quality resection or electrocoagulation, they occur only in 10% of cases.
Remember that tubular adenoma of the colon will eventually develop into cancer. If your doctor offers you surgery, do not refuse and do not hope for miracle medications. They do not exist; only surgery can rid a person of adenomatous polyps in the large intestine.
Adenomatous changes in the epithelium can be both a precancerous condition of adenocarcinoma and an indicator of an increased risk of its development. In the absence of therapy, up to 25% of polyposis undergoes slow malignancy.
According to the WHO classification, there are several forms of mucosal lesions:
- tubular;
- papillary (villous);
- tubulopapillary.
Tubular adenoma of the stomach has clearly defined edges and a glandular structure. Tubular branches and vessels located in the upper layer of the mucosa are surrounded by atypical epithelium. The underlying tissue may remain normal or, more commonly, undergo a cystic change.
This type of polyp is the most dangerous and often turns into cancer. The most unfavorable in terms of malignancy are adenomas larger than 1–2 cm in circumference.
The papillary polyp has a velvety surface and is rarely found in its pure form. The formation can be pedunculated or have a wide base; it rarely degenerates into a malignant form.
Tubular villous adenoma is a combination of tubular and papillary structures, each of which occupies at least 30% of the total tumor volume. Further growth of the epithelium leads to an increase in the number of villi, which can be located both on the surface of the formation and inside the glandular cavities.
Introduction
The possibility of endoscopic treatment of early colon cancer has been discussed for a long time. It is a generally accepted fact that tumor removal within healthy tissue is sufficient for cancer limited to the mucous membrane. Opinions on the endoscopic treatment of early invasive colorectal cancer (CRC) range from complete denial of this possibility [2] to assessment of endoscopic removal as radical in all cases where the tumor is removed within healthy tissue [8].
When, during sigmoidoscopy, proctologists at the Yusupov Hospital discover a small polyp, the size of which does not exceed 1 cm, they perform a biopsy. If an adenoma is morphologically verified, colonoscopy is performed to identify possible synchronous lesions in the proximal colon.
If during sigmoidoscopy doctors detect a polyp measuring 1 cm or more, there is no need to perform a biopsy. The tumor is removed during a colonoscopy, which is performed to identify synchronous tumor lesions in the upper parts of the colon. If a non-tumor polyp (hyperplastic, inflammatory) is detected, there is no need for further observation.
After a total colonoscopy and removal of all polyps, a subsequent colonoscopy is performed after 3 years. In case of incomplete removal of the polyp, removal of large broad-based adenomas, multiple polyps, subsequent colonoscopies are performed at an earlier date. If no new adenomas are detected during a control colonoscopy, the observation interval is increased to five years.
In the presence of large wide-based polyps, the risk of complications during endoscopic removal of which is high, surgical intervention is performed using a laparotomic approach. After complete endoscopic removal of adenomatous polyps with severe dysplasia), there is no need for additional examination or treatment of patients. Follow-up colonoscopy is performed within three years. If no new adenomas are detected, the observation interval is increased to 5 years.
After endoscopic removal of an adenomatous polyp with signs of a malignant tumor, further tactics are determined based on prognostic criteria. If the endoscopist is convinced that the polyp was completely removed, a morphological examination revealed a well-differentiated or moderately differentiated adenocarcinoma, there was no invasion of the blood or lymphatic vessels, and no malignant cells were found at the resection margins, endoscopic polypectomy is considered radical.
When there is no confidence in the complete removal of the adenoma, a morphological examination reveals low-grade adenocarcinoma, there is invasion of the lymphatic or blood vessels, malignant cells are found at the resection margins, the patient undergoes surgical intervention due to the high risk of residual adenocarcinoma and metastases to regional lymph nodes.
If there are signs of intestinal discomfort, the cause of which may be tubular or tubular villous adenoma of the colon, well-differentiated or poorly differentiated adenocarcinoma, carcinoid of the appendix, contact the oncologists of the clinic. You will be given an appointment with a doctor at the Yusupov Hospital.
Localization
The favorite place for adenoma is the antrum and vestibule of the stomach, located near the transition to the duodenum. Somewhat less often, polyps are located in the body of the stomach or cardiac segment.
Most of the formations are single structures on a stalk or tightly seated on the mucosa, sometimes indented.
Atrophic gastritis is recognized as one of the main causes of gastric adenoma, especially if it is complicated by unfavorable conditions. Another, no less common culprit of polyposis is hereditary predisposition.
The following factors can provoke pathological proliferation of the epithelium:
- unhealthy diet (irregular meals, inclusion of “aggressive” foods in the diet);
- poor environmental conditions;
- decreased immunity;
- uncontrolled use of medications;
- the presence of the bacterium Helicobacter pylori in the gastrointestinal tract;
- age after 40 years.
A viral infection of the gastric mucosa, drinking alcohol and smoking, and frequent stress can serve as an impetus for the development of adenoma.
At an early stage of the disease, the polyp does not manifest itself in any way. Only as it progresses, when the adenoma begins to grow and compress neighboring structures or clog the inlet, do the first symptoms of illness, reminiscent of gastritis, appear:
- sharp or dull pain in the epigastric area;
- lack of appetite;
- belching;
- nausea;
- deterioration of health.
Often the patient’s tastes change or become distorted - the person cannot eat meat and other familiar foods, and a craving for inedible things appears. With advanced adenoma, gastric bleeding, anemia, and pale skin occur.
Diagnostics
Today, the diagnosis of gastric adenoma has made significant progress and makes it possible to identify polyps up to 0.5 cm in size, determine their type and exact quantity.
Although a reliable diagnosis can only be made with the help of a biopsy and endoscopy, the patient is prescribed a number of additional studies that help determine the patient’s general condition and the degree of damage to the mucosa:
- clinical blood test with test for Helicobacter pylori;
- Ultrasound;
- CT;
- contrast radiography.
During the diagnostic process, adenomatous polyposis must be differentiated from carcinoma, gastritis and various types of hyperplasia.
Adenoma in all cases is subject to surgical removal. Drug therapy is not only ineffective, but can also waste valuable time. The use of medications is justified only if the pathology has developed against the background of gastritis - with their help, the symptoms of inflammation of the mucous membrane are eliminated.
To remove the adenoma, endoscopic polypectomy or gastrectomy is used. The first method is the most gentle and less traumatic. It is prescribed for single small polyps. After 1.5–2 months, the operated tissues are completely restored, and after 11–12 weeks the patient undergoes a repeat endoscopy to ensure that there is no adenoma.
Sometimes the oncologist takes a wait-and-see approach, taking the patient under observation. The patient is prescribed a strict diet, adherence to a lifestyle and nutritional regimen, perhaps a change of job and medical observation. When gastric adenoma becomes active, the question of surgery arises.
Prevention
Specific prevention designed to protect a person from the appearance of a tumor has not been developed. Prevention of pathology is usually based on measures to prevent and treat gastritis, as well as other inflammatory diseases of the gastric mucosa.
The main ways to prevent gastrointestinal adenomas:
- adherence to diet;
- refusal of excessively hot, spicy and irritating foods, preservatives;
- taking medications only as prescribed by a doctor;
- eliminating stress and fatigue.
To maintain immunity, it is very important to lead an active lifestyle, wisely alternate between exercise and rest, and not get carried away with alcohol. All these measures taken together will help to avoid the appearance of a tumor or, if trouble has already happened, to slow down its growth.
Gastric adenoma is a conditionally benign tumor, that is, with timely and competent surgical therapy, it is completely curable. Therefore, at the slightest suspicion of pathology, it is necessary to consult a specialist, and not engage in amateur activities.