Many patients are concerned about the question of how to live after removal of the gallbladder. Will their lives be as fulfilling, or are they doomed to disability? Is full recovery possible after gallbladder removal? There are no unnecessary organs in our body, but they are all conditionally divided into those without which further existence is simply impossible and those in the absence of which the body can function
The process in which the gallbladder is removed is a forced procedure; it is a consequence of the formation of stones and a malfunction in the body, after which the gallbladder ceases to function normally. Stones that appear in the gall bladder begin to form as a result of chronic cholecystitis.
Diet after gallbladder removal will prevent the occurrence of postcholecystectomy syndrome.
Recommendations for patients after gallbladder removal
| Can: | It is forbidden: | |
| wheat and rye bread (yesterday's); | bread and bakery products | butter dough; |
| any porridge, especially oatmeal and buckwheat; pasta, vermicelli; | cereals and pasta | |
| lean meat (beef, chicken, turkey, rabbit) boiled, baked or steamed: meatballs, dumplings, steam cutlets; | meat | fatty meats (pork, lamb) and poultry (goose, duck); |
| boiled lean fish; | fish | fried fish; |
| cereal, fruit, milk soups; weak broths (meat and fish); borscht, vegetarian cabbage soup; | soups | fish and mushroom broths; |
| cottage cheese, kefir, lactic acid products; mild cheese (including processed cheese); | Dairy | |
| butter in limited quantities; vegetable oil (sunflower, corn, olive) - 20-30 g per day; | fats | animal fats; |
| any vegetables, boiled, baked or raw; fruits and berries (except sour ones) raw and boiled; | vegetables and fruits | spinach, onion, radish, radish, cranberry; |
| cracker; | confectionery | cakes, cream, ice cream; carbonated drinks; chocolate; |
| Snacks, canned foods | ||
| vegetable and fruit juices; compotes, jelly, rosehip decoction | beverages | alcoholic drinks; strong tea; strong coffee |
| Essentuki No. 4, No. 17, Smirnovskaya, Slavyanovskaya, sulfate Narzan 100-200 ml warm (40-45°) 3 times a day 30-60 minutes before meals | Mineral water |
The postoperative period is a stay in the hospital.
After a routine uncomplicated laparoscopic cholecystectomy, the patient is transferred from the operating room to the intensive care unit, where he spends the next 2 hours of the postoperative period to monitor adequate recovery from the state of anesthesia. In the presence of concomitant pathology or characteristics of the disease and surgical intervention, the duration of stay in the intensive care unit may be increased. The patient is then transferred to a ward where he receives the prescribed postoperative treatment. During the first 4-6 hours after surgery, the patient should not drink or get out of bed. Until the morning of the next day after the operation, you can drink plain water without gas, in portions of 1-2 sips every 10-20 minutes with a total volume of up to 500 ml. The patient can get up 4-6 hours after surgery. You should get out of bed gradually, first sit for a while, and, in the absence of weakness and dizziness, you can get up and walk around the bed. It is recommended to get up for the first time in the presence of medical personnel (after a long stay in a horizontal position and after the action of medications, orthostatic collapse - fainting) is possible.
The next day after the operation, the patient can move freely around the hospital, begin to take liquid food: kefir, oatmeal, diet soup and switch to the usual regime of drinking liquids. In the first 7 days after surgery, the consumption of any alcoholic beverages, coffee, strong tea, drinks with sugar, chocolate, sweets, fatty and fried foods is strictly prohibited. The patient's diet in the first days after laparoscopic cholecystectomy may include fermented milk products: low-fat cottage cheese, kefir, yogurt; porridge with water (oatmeal, buckwheat); bananas, baked apples; mashed potatoes, vegetable soups; boiled meat: lean beef or chicken breast.
In the normal course of the postoperative period, the drainage from the abdominal cavity is removed the next day after surgery. Removing the drainage is a painless procedure; it is performed during dressing and takes a few seconds.
Young patients after surgery for chronic calculous cholecystitis can be sent home the next day after surgery; other patients are usually in the hospital for 2 days. Upon discharge, you will be given a sick leave certificate (if you need one) and an extract from the inpatient card, which will outline your diagnosis and features of the operation, as well as recommendations on diet, exercise and medication. A sick leave certificate is issued for the duration of the patient’s stay in the hospital and for 3 days after discharge, after which it must be extended by the clinic surgeon.
Benefits and complications
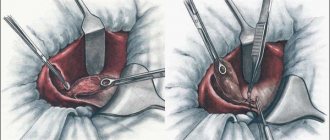
During laparoscopy of the gallbladder, 4 punctures are made in the abdomen, into which surgical tubes (trocars) are inserted, and the gallbladder is removed through an opening in the navel.
A laparoscope (video camera with a lighting device) allows you to monitor the progress of the operation. The main indication for laparoscopic cholecystectomy is cholelithiasis (cholelithiasis). At the initial stage of calculous cholecystitis (stones in the gallbladder), conservative methods are used: diet, drug treatment, destruction of stones by ultrasound. In later stages, surgery is necessary.
Removal of the gallbladder is performed in the following cases:
- Acute inflammation of the gallbladder, which is accompanied by a high temperature that does not subside for a long time.
- The presence of large stones in the biliary system.
- Signs of inflammation of the peritoneum.
- Fibrous or purulent exudate is present in the abdominal space.
Reference. The gallbladder is removed through an open incision or laparoscopically. The latter method is considered more modern and safer.
Advantages of laparoscopic cholecystectomy:
- After surgery, the patient regains activity faster. After only 5-6 hours he is allowed to get out of bed under the supervision of medical staff.
- The wounds are small and heal quickly.
- The patient needs intensive care for no more than 2 hours.
- After surgery, the patient does not have to stay in bed for a long time.
- Laparoscopy of the gallbladder is less likely to cause complications than standard abdominal surgery.
- There are no large scars on the skin.
- The patient is discharged home earlier.
However, even laparoscopy can cause complications:
- Injury to nearby organs and vessels.
- Puncture of the gallbladder, stomach, colon, duodenum, inflammation of the skin around the navel.
- There is a risk of umbilical hernia in overweight patients with congenital muscle abnormalities.
After laparoscopy, the risk of hernia formation is lower than after standard surgery, so the patient does not have to wear a bandage. However, for the first 6 months he is prohibited from lifting weights or straining the muscles of the anterior abdominal wall. The patient should play sports, but about the set of exercises you need to consult a doctor.
Compliance with physical activity regimen.
Any surgical intervention is accompanied by tissue trauma and anesthesia, which requires restoration of the body. The usual rehabilitation period after laparoscopic cholecystectomy ranges from 7 to 28 days (depending on the nature of the patient's activity). Despite the fact that 2-3 days after the operation the patient feels satisfactory and can walk freely, walk on the street, even drive a car, we recommend staying at home and not going to work for at least 7 days after the operation, which is required for the body to recover. . At this time, the patient may feel weakness and increased fatigue.
After surgery, it is recommended to limit physical activity for a period of 1 month (do not carry weights of more than 3-4 kilograms, exclude physical exercises that require tension in the abdominal muscles). This recommendation is due to the peculiarities of the formation of the scar of the muscular aponeurotic layer of the abdominal wall, which reaches sufficient strength within 28 days from the moment of surgery. 1 month after surgery there are no restrictions on physical activity.
What methods are used to remove an organ?
The following methods are used to carry out the operation:
- laparotomy;
- laparoscopy;
- mini access.
Each of these methods is used by doctors in specific cases. The first is performed using a 15-centimeter incision in the wall of the abdominal cavity, through which the gallbladder is removed. This method is used for emergency surgery, if laparoscopy is contraindicated, there is an acute inflammatory process or the ducts are severely damaged.
Since the operation is abdominal, recovery after removal of the gallbladder will require a long period. The patient's sutures are removed after about 10 days. The patient receives inpatient treatment for 2 weeks. Gradually, the person returns to normal life, but will have to adhere to a special diet, not lift weights and not swim in ponds for six months.
The second method (laparoscopy) is considered less traumatic. It is carried out using punctures in the abdominal wall in 4 places. Equipment is inserted into these incisions to allow the organ to be removed. The postoperative period after removal of the gallbladder during laparoscopy is much faster. Three days later the patient is discharged from the hospital.
In the case of a mini-access, the incision is from 3 to 7 cm: thus, the tissue is injured less than in the first case. This method is used if adhesions have formed or there is an inflammatory process in the tissues.
Drug treatment.
Minimal medical treatment is usually required after laparoscopic cholecystectomy. Pain syndrome after surgery is usually mild, but some patients require the use of analgesics for 2-3 days. Usually these are ketanov, paracetamol, ethol fort.
In some patients, it is possible to use antispasmodics (no-spa or drotaverine, buscopan) for 7-10 days.
Taking ursodeoxycholic acid (Ursofalk) can improve the lithogenicity of bile and eliminate possible microcholelithiasis.
Taking medications should be carried out strictly as directed by the attending physician in an individual dosage.
Normalization of digestion
The postoperative period is often complicated by constipation. To avoid this, you need to replenish your diet with vegetables, maintain moderate physical activity, and consume kefir, natural yogurt, and cottage cheese (with a low fat content) every day. Constipation can be eliminated with medications with a laxative effect that do not inhibit intestinal motility. Enemas do not need to be given frequently, as this can lead to colon distension and dysbacteriosis.
Medicines are used to relieve digestive disorders
For diarrhea, it is recommended to eat vegetables and fruits after heat treatment, and porridge with water. To normalize the natural bacterial flora of the intestines, special supplements are prescribed.
The following symptoms may be present for some time after laparoscopic cholecystectomy: burning behind the sternum, belching, nausea, bitter taste in the mouth. If there are no concomitant diseases and the patient follows a diet, then these symptoms disappear on their own after some time.
Many patients are interested in the question of what pills to take after removal of the gallbladder. Drug treatment is carried out only as prescribed by a doctor, who decides on the choice of medications.
For duodenogastric reflux (reflux of the contents of the duodenum into the stomach), anti-reflux medications are used, for example, Motilium. Treatment of heartburn and pain is carried out with the help of antacid drugs: Rennie, Maalox, Almagel. For stomach ulcers, medications are used that suppress the secretion of bile (Omeprazole).
If necessary, magnetotherapy and ultrasound irradiation are prescribed.
Care of postoperative wounds.
In the hospital, special stickers will be applied to postoperative wounds located at the places where instruments are inserted. It is possible to take a shower with Tegaderm stickers (they look like a transparent film), while Medipore stickers (a white patch) must be removed before showering. You can shower starting 48 hours after surgery. Getting water on the seams is not contraindicated, but you should not wash the wounds with gels or soaps or rub them with a washcloth. After taking a shower, you should lubricate the wounds with a 5% iodine solution (or betadine solution, or brilliant green, or 70% ethyl alcohol). Wounds can be treated using the open method, without dressings. Taking baths or swimming in pools and ponds is prohibited before the sutures are removed and for 5 days after the sutures are removed.
Sutures after laparoscopic cholecystectomy are removed 7-8 days after surgery. This is an outpatient procedure, the sutures are removed by a doctor or a dressing nurse, and the procedure is painless.
Complications from wounds.
These may be subcutaneous hemorrhages (bruises) that go away on their own within 7-10 days. No special treatment is required.
There may be redness of the skin around the wound and the appearance of painful lumps in the wound area. Most often this is due to wound infection. Despite the ongoing prevention of such complications, the incidence of wound infection is 1-2%. If such symptoms appear, you should consult a doctor as soon as possible. Late treatment can lead to suppuration of the wounds, which usually requires surgical intervention under local anesthesia (debridement of the festering wound) followed by dressings and possible antibiotic therapy.
Despite the fact that our clinic uses modern high-quality and high-tech instruments and modern suture material, in which wounds are sutured with cosmetic sutures, in 5-7% of patients hypertrophic or keloid scars may form. This complication is associated with the individual characteristics of the patient’s tissue reaction and, if the patient is dissatisfied with the cosmetic result, may require special treatment.
In 0.1-0.3% of patients, hernias may develop at the sites of trocar wounds. This complication is most often associated with the characteristics of the patient’s connective tissue and may require surgical correction in the long term.
Residual choledocholithiasis.
According to statistics, from 5 to 20% of patients with cholelithiasis also have concomitant stones in the bile ducts (choledocholithiasis). A set of examinations carried out in the preoperative period is aimed at identifying such a complication and using adequate treatment methods (this can be retrograde papillosphincterotomy - dissection of the mouth of the common bile duct endoscopically before surgery, or intraoperative revision of the bile ducts with removal of stones). Unfortunately, none of the methods of preoperative diagnosis and intraoperative assessment is 100% effective in identifying stones. In 0.3-0.5% of patients, stones in the bile ducts may not be detected before and during surgery and cause complications in the postoperative period (the most common of which is obstructive jaundice). The occurrence of such a complication requires endoscopic (using a gastroduodenoscope inserted through the mouth into the stomach and duodenum) intervention - retrograde papilosphinctoromy and transpapillary sanitation of the bile ducts. In exceptional cases, repeated laparoscopic or open surgery is possible.
Intraoperative period
Preoperative diagnosis of anomalies in the development and location of the gallbladder helps to develop tactics for surgical intervention, but does not always provide comprehensive information. In some cases, adjustments to the actions of the medical team occur after opening the peritoneum. Most often, this does not affect the result in any way, but with an urgent operation, without sufficient diagnostic, medicinal and sanitary preparation, both treatment options and complications are possible.
Complications during surgery include not only and not so much undesirable consequences resulting from surgical manipulations, but concomitant lesions of the abdominal organs that have become obvious.
Complications include:
- inflammation of the liver, stomach, pancreas is a common concomitant phenomenon detected during the intervention, developing simultaneously with the pathology of the gallbladder or as a result of the disease;
- abscesses - local purulent formations on neighboring organs that arose before surgery due to infection from the gallbladder, but require the intervention of surgeons, which increases the time and complexity of the operation;
- injuries to neighboring organs and vessels due to tumor spread, fusion of adjacent areas - if possible, sutured during surgery;
- rupture of the gallbladder with the entry of particles of contents into the retroperitoneal cavity - a serious complication that occurs when seeking medical help late, when surgical care is provided as an emergency for health reasons - requires careful sanitation of all internal surfaces to avoid peritonitis;
- bleeding - occurs when an abnormally located hepatic or portal vein is injured, dangerously massive loss of blood in a short time, requiring immediate stop and transfusion.
Whatever the intraoperative complications when removing the gallbladder, the operation ends sooner or later and the patient is transferred to intensive care.
Damage to the bile ducts.
Damage to the bile ducts is one of the most severe complications in all types of cholecystectomy, including laparoscopic. In traditional open surgery, the incidence of severe bile duct injury was 1 in 1500 operations. In the first years of mastering laparoscopic technology, the frequency of this complication increased 3 times - up to 1:500 operations, however, with the growing experience of surgeons and the development of technology, it stabilized at the level of 1 in 1000 operations. A well-known Russian specialist on this problem, Eduard Izrailevich Galperin, wrote in 2004: “... Neither the duration of the disease, nor the nature of the operation (emergency or planned), nor the diameter of the duct and even the professional experience of the surgeon affect the possibility of damage to the ducts...”. The occurrence of such a complication may require repeated surgery and a long period of rehabilitation.
Remote period
When the gallbladder is removed due to the presence of stones in it, the cause of poor health - obstruction of the bile ducts - is eliminated, but not the cause of this condition - the composition of the bile remains unchanged. Therefore, in late periods after surgery, complications from the hepatic bile duct are possible.
Allergic reactions to medications.
The trend in the modern world is an ever-increasing allergization of the population, therefore allergic reactions to medications (both relatively mild - urticaria, allergic dermatitis) and more severe (Quincke's edema, anaphylactic shock). Despite the fact that in our clinic allergological tests are carried out before prescribing medications, allergic reactions are possible, and additional drug treatment is required. Please, if you know about your personal intolerance to any medications, be sure to tell your doctor about it.
Exacerbation of peptic ulcer of the stomach and duodenum.
Any, even minimally invasive, operation is stressful for the body and can provoke an exacerbation of gastric and duodenal ulcers. Therefore, in patients at risk of such a complication, prophylaxis with antiulcer drugs in the postoperative period is possible.
Despite the fact that any surgical intervention carries a certain risk of complications, refusing or delaying the operation also carries a risk of developing severe illness or complications. Despite the fact that the clinic’s doctors pay great attention to the prevention of possible complications, the patient plays a significant role in this. Performing cholecystectomy in a planned manner, with non-advanced forms of the disease, carries a much lower risk of unwanted deviations from the normal course of the operation and the postoperative period. The patient’s responsibility for strict adherence to the regimen and doctors’ recommendations is also of great importance.
Types of cholecystectomies
Laparotomy cholecystectomy
The classic method consists of making a large incision in the abdominal wall, isolating and removing the gallbladder. Laparotomy is used when emergency intervention is necessary and a laparoscopic procedure cannot be performed.
Like any other abdominal surgery, it is relatively difficult to tolerate. For this reason, a long recovery period is necessary.
Laparoscopic cholecystectomy
Laparoscopic interventions are less traumatic for the patient.
It has a number of advantages over classical cholecystectomy. During laparoscopy, several small incisions are made in the abdominal wall, which minimizes trauma to organs and tissues. The patient's rehabilitation period is much shorter.
Long-term rehabilitation after cholecystectomy.
Most patients after cholecystectomy are completely cured of the symptoms that bothered them and return to normal life 1-6 months after the operation. If cholecystectomy is performed on time, before the occurrence of concomitant pathology from other organs of the digestive system, the patient can eat without restrictions (which does not negate the need for proper healthy nutrition), not limit himself in physical activity, and not take special medications.
If the patient has already developed concomitant pathology of the digestive system (gastritis, chronic pancreatitis, dyskinesia), he should be under the supervision of a gastroenterologist in order to correct this pathology. A gastroenterologist will give you recommendations on lifestyle, diet, dietary habits and, if necessary, drug treatment.
Save on social networks:
The recovery period and its features
If your health is dear to you, and you do not want even more serious problems with the gastrointestinal tract, you will have to come to terms with a new lifestyle. First of all, you will need to adjust the proportions of nutrients entering the body with food.
The daily diet is structured as follows:
- Proteins – their share is 25 percent. They are necessary in order to normalize the functioning of the liver and activate the process of renewal of its cells. This means that the diet must include poultry, dairy products and fish.
- Fats – the share of these substances is 25 percent. Their consumption must be reduced because stones in the gallbladder ducts are formed from cholesterol. But it is important to give up cholesterol-containing foods and leave those containing unsaturated fats. We are talking about vegetable oils. They help reduce the risk of stone formation and speed up the dilution of bile.
- Carbohydrates are the remaining 50 percent. You need to choose them as carefully as possible. For example, cereals and baked goods can cause bile acidification. This leads to the formation of stones. And “light” carbohydrates give impetus to metabolic processes in the body and can contribute to weight gain. With the help of a nutritionist, you can find the optimal balance between one and the other group of carbohydrates.
In addition , patients after such an operation are always prescribed vitamins K and B, ascorbic acid. This is necessary to maintain normal liver function.
Let's consider what dietary habits need to be introduced at each stage of the recovery period after laparoscopy.