Esophageal varices occur as a result of portal hypertension in liver diseases. Bleeding from esophageal varices is a life-threatening disease that can only be treated in a hospital setting. Detection of bleeding too late in most cases leads to death.
Symptoms of varicose veins of the esophagus
Causes
The main reason is the appearance of portal hypertension, which causes high blood pressure. Next, the blood flow is blocked.
There are acquired and congenital forms of the disease.
Congenital is quite rare. Acquired occurs as a result of liver dysfunction.
It develops against the background of several factors:
- Budd-Chiari disease;
- the presence of gallstones, cysts, neoplasms;
- sclerosis;
- hypertension, in which it is very difficult to reduce blood pressure;
- cirrhosis, hepatitis, tuberculosis, other liver pathologies;
- thrombosis of internal organs.
Treatment methods
The main goal in treating varicose veins is to prevent bleeding, which can be life-threatening. If bleeding occurs, all efforts are aimed at stopping it.
Prevention of bleeding
Treatment aimed at reducing pressure in v. portae may reduce the risk of bleeding from varicose veins. It may include the following methods:
The drug Anaprilin with the active ingredient propranolol
Stopping bleeding from VRVP
Bleeding from esophageal varices is a life-threatening condition that requires immediate medical attention. Methods used to stop bleeding and eliminate the effects of blood loss:
- Ligation of bleeding esophageal varices using elastic rings.
- Tamponade using a Blackmore probe. This method is used as a temporary rescue measure for uncontrolled bleeding from the esophageal urinary tract. The Blackmore probe has two balloons. It is inserted into the stomach through the mouth, after which the doctor inflates the first (gastric) balloon. The probe is then gently pulled up until the inflated balloon rests against the gastroesophageal junction. Doctors inflate the second balloon (esophageal). The inflated balloons of the Blackmore probe press against esophageal varices, thereby stopping bleeding.
- Medicines that slow blood flow in the portal vein. To reduce the flow of blood from internal organs into the portal vein system, doctors often prescribe the drug Octreotide. Drug therapy complements endoscopic vascular ligation and lasts approximately 5 days.
- Redirection of blood flow from the v. system. portae. Doctors may recommend that a patient with varicose veins undergo a transjugular intrahepatic portosystemic shunt, which involves placing a small tube (shunt) connecting the v. portae and hepatic vein. This shunt reduces the pressure in v. portae and helps stop bleeding. However, such surgery can cause serious complications, including liver failure and brain problems, which can occur because toxins normally cleared by the liver enter the systemic bloodstream directly through the shunt. This method is most often used when other methods of reducing pressure in v are ineffective. portae, and also as a temporary measure in people awaiting liver transplantation.
- Restoration of circulating blood volume. To replace lost blood and eliminate clotting factors, patients are often given transfusions of blood components.
- Prevention of infections. As bleeding develops, the risk of infectious complications increases, so patients are often prescribed antibiotics.
- Liver transplantation is a treatment option for patients with severe liver damage who develop recurrent bleeding episodes.
Blackmore probe
Classification
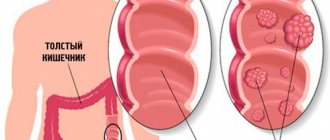
Defects of blood vessels in the esophagus are classified by several indicators. The main thing is the severity of the disease.
Degrees of phlebectasia:
- 1st degree - symptoms are mild or completely absent. When conducting an examination at this level, the canals are expanded to 3-5 mm. In this case, single ectasia or its absence can be detected. Clear lumen, diagnosed by endoscopy;
- 2 - the first symptoms are observed. Diagnosed using radiography. The veins at this stage expand to 10 mm. The results of the study are tortuous, dilated channels in the lower esophagus. The blood supply system is greatly expanded and can occupy 1/3 of the cavity of the entire esophagus;
- 3 - capillaries dilated more than 10 mm and occupied 2/3 of the esophagus cavity. The veins swell, the nodes are visible visually. Gastroesophageal reflux begins to develop, as the mucous membrane has become very thin;
- 4 - advanced stage, at which bleeding begins. The nodes form clusters, severe damage to the mucosa is observed, and there is practically no lumen.
Of all the degrees, 4 is the most dangerous for human life.
Diagnostics
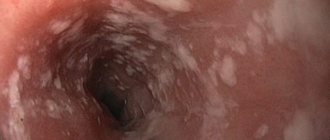
The diagnosis can be suspected, but cannot be confirmed without esophagogastroduodenoscopy. This is practically the only way to establish a connection between bleeding and esophageal varices; gastric varices are often simultaneously detected.
The procedure allows you to determine the degree of deformation of the veins, the stage of the disease, visually determine the condition of the vascular walls, and predict rupture. It is almost impossible to conduct research during bleeding.
Contrast radiography of the esophagus is routinely prescribed; before the image, the patient is given a barium mixture to drink. A series of radiographs are used to monitor the movement of the contrast and its spreading in the lumen of the esophagus.
Laboratory way:
- it is necessary to determine the presence of anemia by the content of red blood cells, platelets, and color indicator;
- in case of acute bleeding, the hematocrit is calculated;
- be sure to do an analysis of clotting indicators;
- determine liver function by enzyme tests, protein, glucose, bilirubin levels; deviations in the results make it possible to suspect the influence of liver pathology on changes in the venous system of the esophagus;
- if there are signs of bleeding, the blood type and Rh factor are determined in case of a necessary blood transfusion.
Development mechanism
With phlebectasia, the blood outflow from the liver vessels is disrupted. However, it is significantly reduced in the portal vein during hypertension. This can further lead to thinning and deformation of the bloodstream.
Blood begins to accumulate on the walls of the vessels, which forms characteristic thickenings in this place. When blood pressure rises, the load on the capillary wall increases and it bursts.
In case of cardiac pathologies, it develops slightly. Localization occurs over the entire surface of the esophageal tube.
If the disease is caused by liver pathology, dilation of the vessels located in the lower cavity occurs.
Bleeding directly depends on the condition of the vascular tissue, the size of the node and the pressure surge.
Causes of development of esophageal varicose veins
If blood cannot flow through the portal vein or liver tissue, it accumulates under pressure in the portal system and tries to find alternative routes. This path is represented by the systemic esophageal veins, which connect the portal system with the vena cava. In portal hypertension, blood flows through this esophageal artery, causing it to become enlarged, called varicose veins.
Of course, the most common cause affecting the development of esophageal varicose veins is cirrhosis of the liver, due to chronic alcohol consumption.
Partner advertising
Symptoms
In the initial stages, the disease proceeds unnoticed. In some cases, the symptoms are similar to those of gastrointestinal diseases.
Over time, progressive pathology makes the venous channels brittle and fragile, partial or complete rupture occurs, which entails bleeding. This condition becomes life-threatening.
The onset of varicose veins may be accompanied by the following symptoms:
- swallowing dry food becomes difficult;
- pain is felt in the sternum;
- the occurrence of frequent belching;
- the presence of constant heartburn.
At the stage of hemorrhage you can observe:
- dizziness;
- general malaise;
- due to loss of blood, the skin becomes pale;
- the patient is constantly bothered by diarrhea, black in color;
- constant nausea, attacks of vomiting with blood clots in the vomit.
At the first symptoms, you should immediately call an emergency ambulance team. Medical intervention in this case is necessary.
Symptoms of the disease
At the first stage of the disease there is no pronounced discomfort; it is usually attributed to a violation of the diet and its errors, or to the symptoms of a gastrointestinal disease.
Heartburn appears, a mild indigestion, for which people often do not consult a doctor. When the disease progresses to the second stage, symptoms appear : belching, heartburn. Difficulty swallowing. Enlarged abdomen - ascites, accumulation of fluid in the abdominal cavity. Heaviness and burning in the chest
Complications of the disease are accompanied by: impaired swallowing reflex, bleeding, vomiting with blood, dark feces. In this case, urgent assistance is needed. Symptoms are different for everyone; diagnostics, a thorough medical history, and collection of all necessary tests are required.
Survey
Pathanatomy offers the study of micropreparations, tissue sections, and their laboratory study to identify the pathogen. The macroscopic specimen shows how the vessels are damaged and the esophageal mucosa is changed; specialists need this data to perform operations.
If a disease is suspected, the patient is prescribed tests and medical procedures. In differential diagnosis, other diseases that give similar symptoms are excluded. Qualitative research contributes to successful diagnosis. They include:
- General blood analysis . Shows the number of leukocytes and platelets in the blood
- Blood chemistry . Cholesterol content, liver enzymes, bilirubin level, protein amount, blood type and Rh.
- Endoscopy . The most detailed and reliable diagnosis is fibroesophagoscopy. Internal examination of the walls of the esophagus using an endoscope. The procedure allows you to find out the condition of the veins, the esophageal mucosa, the cause of bleeding, and identifies signs of other diseases with similar symptoms: cancer, ulcers.
- X-ray . Contrast radiography is used. To do this, the patient uses a radiopaque agent barium sulfate internally. When filling the esophagus, barium has a white light in the image and clearly highlights all the structures of the esophagus. Damaged vessels are clearly visible, in the form of oval filling defects.
- Duplex scanning of blood vessels . This is a dual ultrasound examination consisting of B-mode and Doppler. In modern medicine, the method of color Doppler mapping has appeared. The color determines the direction and intensity of blood flow. The use of these two methods allows you to examine the anatomy of blood vessels and veins, find out the degree of their expansion, see the presence of nodes and ectasia
Why is it dangerous?
Diagnosing the disease in a timely manner and prescribing adequate effective treatment does not exclude the possibility of relapse. It can occur within 3 years from the onset of the disease. This is the danger of the disease.
As a result of hemorrhage, the patient loses a lot of blood. If not treated promptly, blood loss can be fatal.
The most dangerous condition is observed:
- after vomiting;
- when ulcerative formations occur;
- after straining or overeating;
- with fever and high blood pressure;
- with sudden lifting of weights.
If you monitor your condition all the time, bleeding can be predicted.
Blood loss is promoted by:
- sudden darkening of the eyes, complete loss of consciousness;
- sudden bleeding with the consistency of coffee grounds. At the same time, the blood can be either brown or scarlet;
- there is a constant tickling sensation in the larynx;
- There is a salty taste in the oral cavity.
After bleeding, treatment is suggested with surgery. Rarely, hemorrhage may occur during sleep. Its complications can be caused by decreased blood clotting and cardiac failure.
How do esophageal varices manifest?
Symptoms of the disease depend on the pathology that caused esophageal varicose veins. The initial period proceeds without clinical manifestations, patients are unaware of the development of pathology. But there are frequent cases of a progressive course with sudden bleeding.
The condition worsens within 4–5 days. Patients feel increasing heaviness behind the sternum, compression. This sign is considered a harbinger of massive bleeding and requires urgent measures, since surgeons' observations associate it with death.
All symptoms of varicose veins are determined by threatened manifestations of blood loss. In a chronic course with a small amount of excreted blood, the body gradually weakens. Hypochromic anemia develops. The patient is pale, losing weight, has difficulty moving, and is troubled by shortness of breath. Sometimes there is liquid black feces.
Harbingers of bleeding and initial signs of varicose veins can be:
- vague pain in the chest;
- severe heartburn;
- belching after eating;
- difficulty swallowing dry food.
Heartburn and belching are explained by dysfunction of the esophageal sphincters, reverse (reflux) reflux from the stomach. Some patients experience a tickling in the throat, soreness, and a salty taste in the mouth before bleeding begins.
In acute bleeding, the following appears:
- increasing pallor of the skin;
- vomiting blood (“coffee grounds”);
- constant dizziness;
- loose, tarry stools;
- darkening of the eyes;
- severe weakness.
Bleeding is provoked by lifting weights, physical work, elevated body temperature, taking anticoagulants, and the fibrogastroscopy procedure. But sometimes it occurs spontaneously against the background of general health. It is necessary to differentiate bleeding from a disintegrating tumor of the esophagus and stomach, tumor germination into a large vessel and its breakthrough, and injury to blood vessels by a foreign body.
Which doctor should I contact?
If the diagnosis is known, you need to contact a phlebologist. If you have problems with the digestive system, you will need to consult a gastroenterologist.
If the clinic does not have a phlebologist, you can contact an angiologist. This specialist has a broader specialization. An angiologist deals not only with veins, but also with all capillaries, arteries, and any vessels.
If you are not sure about varicose veins, you should first contact your local physician. When the diagnosis is confirmed by the therapist, he gives a referral to a gastroenterologist, phlebologist or angiologist.
The surgery is performed by a vascular surgeon and gastroenterologist.
FAQ
My husband has been diagnosed with cirrhosis of the liver, with slight bleeding from the veins of the esophagus. A blood test revealed a decrease in platelets. What is the prognosis for this diagnosis?
Liver cirrhosis is an irreversible disease, and bleeding indicates a severe stage of varicose veins. A decrease in platelet levels is a signal of constant, even invisible to the patient, bleeding. At this stage, the most correct tactic is to prevent the progression of the disease.
Is it possible to play sports and drink alcohol at the initial stage of esophageal varicose veins?
If you do not want the disease to progress to the next, more severe stage, you will have to give up physical activity and alcohol.
How to quickly stop bleeding from the esophagus?
This can only be done surgically (by one of the above methods); you yourself need to quickly deliver the patient to the hospital.
Therapy methods
Therapy directly depends on the degree of damage to the esophageal veins. In cases where the disease is diagnosed due to hemorrhage, treatment is aimed at preventing blood loss.
Therapeutic measures:
- fixation of affected vessels with a probe;
- electrocoagulation of affected channels;
- prescribing drugs that constrict blood vessels and restore blood circulation;
- blood transfusion is performed.
If hemorrhage occurs due to cirrhosis of the liver, treatment is directed towards the treatment of the underlying disease.
In this case, treatment is aimed at restoring liver tissue. Also, measures are being taken to prevent relapse.
Therapeutic treatment:
- antacids and astringents are prescribed;
- Vitamin therapy is prescribed.
Surgery may also be prescribed:
- devascularization - removal of the affected arteries;
- sclerotization - injection of a hemostatic solution into the affected area. The procedure is carried out 4 times a year;
- bandage - installation of rubber discs at expansion points;
- portosystemic shunting - connection of the portal and hepatic beds to normalize pressure.
For patients suffering from cirrhosis, surgery is contraindicated, so they undergo endoscopic ligation of the affected vessels.
The principle of the procedure is ligation of blood vessels with elastic rings or nylon threads.
In addition, for varicose veins of the esophagus and stomach, a diet is prescribed.
At this stage, it is very important to follow certain nutritional rules. The food consumed must include fiber, vitamins B and C.
Treatment
A person who has been diagnosed is wondering how to cure varicose veins . The treatment is complex and long. Unfortunately, it does not always bring results. If esophageal varicose veins are diagnosed as a result of a concomitant disease, the chance of complete recovery is low.
Specialists can only maintain the vital function of the body. Prevention is better than cure. Physical activity, combating obesity, proper nutrition , timely treatment of concomitant diseases will give a chance to avoid varicose veins. Treatment of varicose veins of the esophagus includes various measures:
- Therapeutic diet . Most often, varicose veins are a consequence of liver disease. It is very important to follow a proper diet so as not to aggravate the condition of the body. The doctor will select a therapeutic diet, taking into account individual characteristics. Dieting should become a way of life to maintain quality of life.
- Taking medications. Antacids, vitamins, hemostatic and vasoconstrictor drugs. Diuretics, drugs to reduce portal pressure.
- Blood transfusion. In case of bleeding, blood or plasma transfusion occurs in cases that threaten the patient's life. This procedure is carried out after surgery.
- Sclerotherapy Injection of a special solution into a vein. The substance is a sclerosant, causing the destruction of the vein. Using an esophagoscope, a probe is inserted and an injection is made into the vein on both sides.
- Intrahepatic shunt. A catheter is inserted into the neck through a vein, with which a stent is installed. A metal cylindrical device that connects the hepatic and portal veins. The operation reduces the pressure in the liver.
- Splenorenal shunt. A surgical operation during which the splenic vein is connected to the kidney vein, reducing blood pressure in the liver.
- Surgery (cessation of blood supply). In case of acute disease, bleeding, varicose veins are surgically removed.
- Liver transplantation. Prescribed against the background of advanced liver diseases.
Surgical intervention
During pregnancy, only elimination of symptoms and diet are possible. The operation will take place only after childbirth. A modern medical clinic offers many treatment methods, but surgical treatment is not always effective. The operation only eliminates the consequences of the disease - high blood pressure, damaged blood vessels. Treatment of diseased organs brings results.
For liver cirrhosis and fibrosis, stem cell treatment has proven itself to be effective . This method takes into account the ability of stem cells to replace destroyed cells.
Cells are taken from the bone marrow and grown to the required number. Injected into the affected parts of the liver. Liver function and blood quality are restored.
This treatment is considered safe and can be combined with other forms of treatment. With treatment using advanced technologies, a good prognosis for recovery is possible.
Many people are interested in treatment with folk remedies. Unfortunately, varicose veins of the esophagus cannot be treated, especially with folk remedies. But with their help you can significantly improve the condition of the body and prolong life.
Before undergoing procedures or following a certain diet, you should consult your doctor. If there are no contraindications, treatment with herbs is effective: Japanese sophora, yarrow, rose hips and rowan, choleretic herbs are useful. Surgery for varicose veins of the esophagus (video)
Therapy with folk remedies
In combination with traditional therapy, traditional therapy methods can be used. In this case, consult your doctor before using them. In the treatment of folk methods, it is recommended to use medicinal compositions from rose hips and red rowan.
For the composition you need to take 1 tbsp. l. rowan berries and 1 tbsp. l. rose hips, add 500 mg of boiling water and simmer over low heat for 5 minutes. Next, the drink is filtered and cooled.
Take the composition ½ cup 4 times a day.
Patient examination plan
If you have symptoms of varicose veins of the esophagus or stomach, consultation with a phlebologist and gastroenterologist is required. The following studies need to be carried out:
- magnetic resonance imaging;
- Ultrasound of the esophagus;
- radiography;
- FGDS;
- blood tests.
An ultrasound can determine the condition of the liver and determine the cause of varicose veins. Using X-ray examination, the shape, relief and diameter of the esophagus are assessed. With varicose veins, narrowing and deformation are observed. The image reveals the convoluted folds of the organ and changes in contours. FGDS has the greatest diagnostic value.
This is an endoscopic examination in which a thin probe with a camera at the end is inserted into the esophagus and stomach through the mouth. The procedure is performed slowly so as not to injure the veins. During the examination, tuberosity of the esophageal mucosa and the presence of nodes are revealed. Laboratory tests are of little value. A blood test can reveal signs of inflammation and anemia.