Pancreatic necrosis is one of the most severe diseases of the abdominal organs and in 1% of situations causes an acute abdomen. Pancreatic necrosis is more often (in 70% of cases) diagnosed in young people and can be either a separate nosological entity or act as a complication of acute pancreatitis.
The chances of surviving after destruction (destruction) of the pancreas are small and amount to 30–60% even with adequate and timely treatment, and in the case of total pancreatic necrosis they are zero. In recent years, there has been an increase in the incidence of the disease, which is 6–9%. Pancreatic necrosis is equally often diagnosed in both men and women.
Pancreatic necrosis and its types
Pancreatic necrosis is a disease of the pancreas in which its cells die due to the development of an inflammatory process in the organ. As a result, the gland is subjected to destructive (destructive) processes and multiple organ failure develops. Pancreatic necrosis is not a complication of acute pancreatitis, but its stage, and is characterized by a severe course and rapid progression.
Kinds
The disease is classified according to the following parameters:
- Depending on the prevalence of the destructive process:
- limited necrosis (small-, medium- and large-focal);
- widespread necrosis (subtotal - almost the entire gland is affected, and total - the gland is damaged throughout its entire volume).
- Whether or not there is an infection in the pancreas:
- infected;
- sterile.
- Depending on the course of the disease:
- abortive;
- progressive.
In turn, sterile necrosis of the pancreas is divided into three clinical and anatomical forms:
- fatty (develops slowly, over a 4-5 day period and has a better prognosis);
- hemorrhagic pancreatic necrosis (rapidly progressing, accompanied by internal bleeding);
- mixed necrosis of the pancreas (more common than other forms).
Causes
The development of the disease is promoted by 3 main factors:
Nutritional
The most common cause of pancreatic necrosis. The destructive process is triggered by episodic consumption of significant doses of alcohol or large amounts of fatty foods (as a rule, 2 reasons act simultaneously, for example, after feasts).
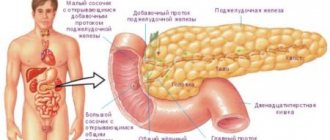
Obstructive
In this case, a blockage of the gland duct occurs, which leads to an increase in intraductal pressure, the permeability of the vascular walls and the activation of gland enzymes, which begin to melt its own organ. The main cause is cholelithiasis and diseases of the bile ducts.
Reflux
As a result of this factor, bile is refluxed from the duodenum into the pancreas, which activates proenzymes and triggers enzymopathic reactions. In this case, with pancreatic necrosis, the causes are postoperative complications on the abdominal organs, blunt trauma to the abdomen, endoscopic manipulations, vasculitis/thrombophlebitis of the pancreatic vessels, disorders of the sphincter of Oddi located in the duodenum, abnormal development of the gland, food poisoning.
Risk group for the development of pancreatic necrosis
The disease can occur in any person, but there is a risk group that increases the chances of necrotization of the pancreas:
- chronic alcoholics;
- people suffering from cholelithiasis;
- patients with liver pathology and pancreatic pathology;
- diseases of the digestive tract;
- drug addicts;
- patients with congenital malformations of the digestive tract.
What is pancreatic necrosis
Necrosis refers to the death of tissue, which was provoked by various types of pancreatic pathologies, which are based on inflammation of the gland.
Own enzymes are activated prematurely, thereby corroding the vascular walls and connective tissue. Among the causes of necrosis are alcohol abuse, fatty foods, diseases of the biliary tract and bladder. Often, responsibility for the occurrence of pancreatic necrosis lies with medications that were taken or dosed incorrectly.
The mechanism of pathology development
The basis for the development of this disease is a disorder of the local protective forces of the gland. The development of pancreatic necrosis occurs in 3 stages:
- Toxemia phase
Pancreas affected by pancreatic necrosis
As a result of the action of the etiological factor, the external secretion of the pancreas is significantly increased, its ducts are overstretched, and the outflow of pancreatic juices is disrupted. Increased intraductal pressure causes swelling of the organ parenchyma, destruction of small areas of the gland (acini) and increased action of proteolytic enzymes, which causes massive damage (necrosis) of the gland. That is, the organ begins to digest itself. If lipase is activated, fat cells become necrotic, and if elastase is activated, the vascular wall is destroyed. Toxins (tissue breakdown products) and activated enzymes enter the bloodstream due to the destruction of vessel walls and have a toxic effect on all organs. The first to be affected are the liver and kidneys, heart and brain (multiple organ failure develops).
The development of one or another clinical and anatomical form of the disease depends on the predominance of lipase and elastase activity. If lipase activity is exceeded to a greater extent, the adipose tissue of the gland is destroyed, and then areas of the greater and lesser omentum, peritoneum, mesentery and internal organs become necrotic. This form of gland necrosis is called fatty.
If microcirculatory disorders predominate, spasm of the organ’s blood vessels occurs, which causes rapid swelling. Within a few hours, toxemia causes paresis of the walls of blood vessels, their dilation and slowing down the movement of blood in the tissues of the organ. These processes increase thrombus formation and then lead to the development of ischemic necrosis. Increased action of elastase contributes to the destruction of the walls of blood vessels in the thickness of the gland, and later in other organs. As a result, the gland becomes saturated with blood, hemorrhages develop in the internal organs and retroperitoneal tissue, and effusion with blood appears in the abdominal cavity. This form of the disease is called hemorrhagic necrosis of the gland.
With the same level of lipase and elastase activity, they speak of a mixed form of necrosis.
- Second phase
An abscess forms in the pancreas and internal organs.
- Third phase
Purulent changes develop in the pancreas and retroperitoneal tissue.
Treatment of pancreatic necrosis
Without any doubt, pancreatic necrosis is an absolute and undeniable indication for immediate hospitalization of the patient. Already in the hospital, doctors decide on the optimal treatment strategy. She may be:
- conservative;
- surgical (in all cases of infected pancreatic necrosis).
Unfortunately, with fulminant pancreatic necrosis, which develops in just a few hours, sometimes the pathological destructive process becomes uncontrollable. Both intensive therapeutic measures and surgical interventions are powerless against this form of pancreatic necrosis. This dramatic variant is more specific for alcoholic pancreatitis. In the pre-infectious phase of the development of pancreatic necrosis, on the contrary, timely treatment is quite effective and can save the patient.
Symptoms of pancreatic necrosis
Pancreatic necrosis of the pancreas has such an obvious clinical picture that it is difficult to confuse the symptoms of the disease with any other pathology.
Pain
The cardinal sign of pancreatic necrosis is pain. Pain sensations occur in the left half of the abdomen, radiating to the shoulder, back, groin or chest. Often the patient cannot describe the exact location of the pain and calls the pain girdling. The intensity of the pain syndrome can be different and directly depends on the severity of gland necrosis. The further the destructive process in the organ progresses, the less pronounced the pain becomes, which is associated with the death of nerve endings in the gland. Relief of pain and persisting symptoms of intoxication are a “bad” prognostic sign.
Painful sensations are somewhat weakened in a position on the side with the knees bent and legs brought to the stomach, so the patient with this disease takes the described forced position.
Nausea and vomiting
Almost immediately after the onset of pain, uncontrollable vomiting begins. Vomiting is not associated with food intake and does not bring relief. The vomit contains only bile and blood clots (destruction of blood vessels by elastase).
Signs of dehydration
Constant vomiting leads to dehydration (dehydration) of the body. The skin and mucous membranes are dry, the tongue is coated, diuresis decreases, up to the development of anuria (no urination). The patient experiences thirst and constant dry mouth.
Flatulence and bloating
Since the pancreas is “switched off” from the digestive tract, fermentation/putrefaction processes intensify in the intestines, which leads to increased gas formation, bloating, weakened peristalsis, constipation and gas retention.
Signs of intoxication
Bacterial toxins (bacteria themselves may not be present in the blood) circulating in the bloodstream cause intoxication of the body. The temperature rises (up to 38 and above), general weakness occurs, the heartbeat and breathing become more frequent, shortness of breath appears, and blood pressure decreases. The effect of toxins on the brain leads to encephalopathy. The patient's consciousness is confused, the patient is excited or inhibited, disoriented. With severe toxemia, coma may develop.
Hyperemia or pale skin
During the toxemia phase, the pancreas releases vasoactive substances into the blood (dilate blood vessels), which is manifested by redness of the skin. Later, as intoxication develops, the skin turns pale, becomes sallow, marbled or icteric and becomes cold to the touch. Blue-violet spots appear on the sides of the abdomen, on the back, buttocks and in the navel area as a result of internal hematomas and hemorrhages into the soft tissues. Subcutaneous hemorrhages are not observed in all cases of pancreatic necrosis.
Internal bleeding
An increase in the level of elastase contributes to the destruction of blood vessels and the formation of hemorrhagic effusion in the abdominal, pleural and pericardial cavities.
Symptoms of peritoneal irritation
The toxemia stage lasts 5–9 days and is characterized by an increase in symptoms regardless of intensive treatment. The next stage is the formation of purulent and post-necrotic complications. Due to inflammation, the pancreas increases significantly in size, and a purulent infiltrate begins to form in the abdomen. In the pancreas area, the skin becomes too sensitive (hyperparesthesia). Multiple organ failure develops (toxic hepatitis and nephritis, carditis and respiratory disorders).
What complications may arise
The danger of pancreatitis, regardless of the timing of its onset and the correctness of its treatment, lies in its complications. Local complications are:
- Parapancreatic infiltrate (swelling around the pancreas).
- Omentobursitis (enzymes are released from the inflamed pancreas, which accumulate in the omental bursa).
- Pseudocyst (capsule with liquid).
- Streaks and accumulations of inflammatory fluid in various areas of the abdominal cavity (retroperitoneal tissue, pericardium, pleural sinus).
- An abscess (formation of a closed cavity with pus) in the pancreas or its tissue.
- Enzymatic peritonitis (inflammation of the peritoneum due to damage by accumulated enzymes).
- Biliary jaundice (obstructive jaundice due to spasm of the bile duct).
- Arrosive bleeding.
- Bleeding into the lumen of the alimentary canal.
- Enzymatic cholecystitis (inflammation of the gallbladder due to the entry of pancreatic enzymes into the bile duct.
Common complications of pancreatitis are: delirious syndrome (hallucinations, delirium, impaired consciousness), enzymatic shock (drop in blood pressure, multiple organ failure) and sepsis (a large amount of infection entering the blood).
Acute pancreatitis is manifested by three main symptoms: pain in the epigastric region (above the navel) and left hypochondrium (usually burning and girdling), nausea and vomiting (60% of patients), flatulence (“stopping” the intestine). In blood tests, alpha-amylase or lipase levels are 2-3 times higher than normal, and white blood cells are significantly elevated. With pancreatic necrosis, rapid breathing, shortness of breath, and cyanosis (blue discoloration of the skin of the face and limbs) occur. Acceleration followed by deceleration of the heart, a drop in blood pressure, the development of shock and collapse (pressure is not determined). The abdomen is swollen, purple spots may appear on it, and bluish skin on the sides of the body. When tapping, pain occurs in the left costovertebral angle. Body temperature is above 38C, the amount of urine per day is less than 500 ml. (norm 1.5-2 l.)
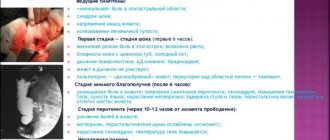
Pancreatic necrosis has a phase course. Each phase is manifested by certain symptoms.
1. Enzymatic phase. Occurs within the first 5 days. Pancreatic necrosis occurs.
2. Reactive phase. Starts at 2 weeks. It manifests itself as the onset of aseptic inflammation of the pancreas in areas of necrosis, near the pancreas. Looks like lumps in the pancreatic area, fever. Blood tests show an increase in leukocytes, an increase in ESR, and C-reactive protein. This phase can end with the resorption of inflammation, the formation of individual areas of necrosis, or the formation of necrosis with the addition of an infection or abscess.
3. Melting phase and more complete formation of areas of necrosis. Occurs after 3 weeks of illness. It may also fester.
Diagnostics
The diagnosis of acute pancreatic necrosis of the pancreas is established on the basis of anamnesis and characteristic complaints, examination of the patient and additional examination.
Laboratory diagnostics:
- general blood test (leukocytosis, granularity of neutrophils, increased ESR, increased hematocrit due to dehydration);
- amylase, elastase, trypsin in urine and blood (increase significantly);
- blood sugar (increases);
- calcitonin in the blood (its level increases with severe inflammation and infection, in particular with infected necrosis of the gland);
- increase in C-reactive protein (a sign of inflammation);
- increase in liver enzymes (AST, ALT).
Instrumental diagnostics:
- Ultrasound of the pancreas and biliary tract (presence of stones in the biliary tract, enlarged gland size, heterogeneous structure and uneven contours of the organ, fluid in the abdominal cavity and retroperitoneal space, foci of necrosis, cysts and abscesses and their localization)
- computed tomography (enlarged gland, dilated pancreatic duct, foci of necrosis, inflammation of the tissue around the pancreas, effusion in the abdominal cavity);
- radiography of the abdominal organs;
- Magnetic resonance imaging;
- puncture of fluid formations of the pancreas followed by a tank. inoculation of material, identification of microorganisms and their sensitivity to antibiotics);
- angiography of gland vessels;
- retrograde cholangiopancreatography (state of the pancreas ducts);
- diagnostic laparoscopy.
Accompanying pathologies and prognosis
The likelihood of a complete cure and a mild course of the pathology is significantly lower if pancreatic necrosis develops against the background of diabetes. Typically, patients require 24-hour insulin infusion through a pump. If hyperglycemia has developed, it is difficult to correct with medications.
Pancreatic necrosis can cause intestinal obstruction, which also worsens the patient's prognosis. The patient suffers from bloating, flatulence, pain in the stomach, muscles are tense, auscultation and palpation bring pain. The sounds of the intestinal tract either weaken or disappear completely. The organ cannot contract normally, feces accumulate in the intestinal lumens. All this significantly increases the risk of death. Pressure in the abdominal cavity increases, which affects the lungs and leads to a malfunction of the respiratory system. The patient has pulmonary insufficiency.
Treatment
When diagnosing pancreatic necrosis, treatment must begin immediately. The patient must be hospitalized in the surgical department in the intensive care ward. The hospital carries out complex therapy aimed at suppressing processes in the pancreas and its self-digestion, eliminating the symptoms of toxemia, and preventing the development of purulent-septic complications. The earlier and more actively treatment for gland necrosis is started, the greater the patient’s chances of recovery. Treatment is carried out using conservative and surgical methods.
Conservative therapy
Conservative therapy includes:
- Ensuring complete rest (bed rest) and therapeutic fasting
The patient is prohibited from any physical activity or eating. Nutrition is provided parenterally with nutrients for 5 to 7 days. Drinking is allowed without restrictions, preferably alkaline mineral waters.
- Pain suppression
Relief of pain and relaxation of the sphincter of Oddi is achieved by parenteral administration of antispasmodic drugs (no-spa, platifillin), non-narcotic analgesics (paracetamol, baralgin, analgin), regional novocaine blockade, intravenous infusions of 1000 - 2000 ml of glucose-novocaine mixture. The administration of narcotic drugs (promedol with atropine, diphenhydramine and novocaine) is allowed, with the exception of morphine, which spasms the sphincter of Oddi. See Medicines for the pancreas.
- Blocking the secretion of the pancreas, stomach and duodenum
To reduce the secretory activity of the pancreas and inactivate proteases, antienzyme agents (Gordox, Contrical, Trasylol) are administered intravenously. Suppression of gastric secretion is ensured by the administration of anticholinergics (atropine) and gastric lavage with cold solutions. Omeprazole and pantoprazole, proton pump inhibitors, also reduce gastric secretion. If there is no concomitant cholelithiasis, choleretic drugs are prescribed to unload the pancreatic and bile ducts. Local hypothermia (cold application to the abdomen) is also provided, which not only reduces the secretion of the pancreas and other organs, but also relieves pain.
- Antibiotics
Antibacterial drugs for destruction of the pancreas are prescribed for prophylactic purposes in aseptic necrosis of the pancreas and to suppress pathogenic microflora in infected necrosis of the pancreas. Antibiotics include cephalosporins (cefipime) with fluoroquinolones (ciprofloxacin) in combination with metronidazole.
- Infusion therapy
To cleanse the bloodstream of toxins and aggressive pancreatic enzymes, massive infusion therapy (glucose with insulin, Ringer's solution, saline) is prescribed. To replenish fluid volume and improve the rheological properties of blood, colloids (reopolyglucin, albumin) are injected intravenously. Suppression of vomiting is ensured by intramuscular administration of cerucal. Infusion therapy is prescribed in combination with diuretics (furosemide), which provides forced diuresis and reduces swelling of the pancreas.
- Detoxification
Extracorporeal detoxification methods are used: therapeutic plasmapheresis, hemosorption, peritoneal dialysis, hemofiltration.
- Somatostatin
The hypothalamic hormone somatostatin is injected intravenously, which suppresses the secretion of gastric juice and the exocrine and endocrine function of the pancreas. The drug also reduces blood flow in internal organs and prevents internal bleeding.
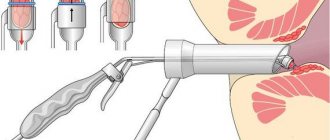
Surgery
With the development of pancreatic necrosis, surgery is indicated in many cases. The purpose of surgical intervention is to restore the outflow of pancreatic juices, remove necrotic foci and inflammatory hemorrhagic exudate, drainage of the abdominal cavity and retroperitoneal space, and stop intra-abdominal bleeding. Surgical treatment is postponed for several days (4–5 days), until the acute process subsides, hemodynamics are restored and the patient’s condition is stabilized. Immediate surgical treatment is indicated in the case of subtotal and total necrosis of the pancreas, purulent peritonitis, and pancreatogenic abscess. In case of infected destructive lesion of the gland, preference is given to laparotomy operations, which provide wide access to the abdominal cavity. In addition, during surgery it is often necessary to remove neighboring organs (gallbladder in destructive cholecystitis, spleen). Repeated surgery is often required due to ongoing self-destruction of the pancreas. Radical surgical treatment includes sequestrectomy (removal of necrotic masses), pancreatectomy (removal of part of an organ) and pancreatectomy (removal of the entire organ).
In case of sterile necrosis of the pancreas, minimally invasive surgical interventions (laparoscopic sanitation and drainage of the abdominal cavity, percutaneous puncture) are preferable.
Treatment and prognosis
If necrosis is diagnosed in the initial stages, when the lesions are single, the affected area has not yet become widespread, there is a chance to save the patient. It is no longer possible to completely restore the functioning of the pancreas to normal, but with constant maintenance of it with appropriate medications, it is still possible to save a person’s life.
Treatment involves combining conservative therapy with surgical therapy.
Surgery for necrosis is inevitable, since this is the only way to preserve healthy tissue. The technique for performing such manipulations and the general treatment regimen are selected individually for each patient.
The basis is the clinical picture, age, stages of development of necrosis, the causes of the pathology, concomitant pathologies and a number of other data obtained during the diagnostic process. Even after surgery, there is a risk of a lack of positive dynamics, so specialists are especially careful when choosing surgical and treatment tactics in general.
The approximate course of treatment for pancreatic necrosis can be presented as follows:
- Drug therapy. It is selected taking into account the pathogenesis, root cause of the condition, concomitant pathologies, as well as other specific factors. This may be a course of antibacterial drugs that limit the spread of pathogenic cells and infections to other tissues. Antibacterial therapy is recommended both before surgical procedures and during the rehabilitation period. If necessary, antiviral and other medications are prescribed.
- Activities that support the functioning of the pancreas. These are specially selected enzymes, which are important to take to facilitate the functioning of the gastrointestinal tract, better digestion and absorption of food.
- Diet. A prerequisite for effective treatment is diet. While the patient is in the hospital, preparing for further treatment, the operation is quite strict. In the future, you will also need to maintain the correct diet, since the pancreas, after necrotic changes, will not be able to perform its functions.
Surgery is almost always used. It can be performed in a minimally invasive way, involving the formation of special punctures or through abdominal surgery.
Care and rehabilitation
Temporary disability of the patient after surgery persists for a long time (up to 3 - 4 months or more). In the postoperative period, the patient's rapid recovery depends on care and rehabilitation measures. For the first two days, the operated patient is in the intensive care ward, where he is monitored for blood pressure, levels of electrolytes and blood sugar, hematocrit, and urine parameters. If the condition and hemodynamic parameters are stable, the patient is transferred to the general surgical ward. The first 2 days after surgery, therapeutic fasting is indicated. From the third day a gentle diet is allowed:
- not sweet tea with crackers;
- liquid pureed soups with vegetable broth;
- rice and buckwheat porridge (milk/water ratio is 1/1);
- protein omelet (half an egg per day);
- dried bread is included in the diet on day 6;
- cottage cheese;
- butter (15 gr.).
At night, a glass of yogurt or warm water with honey is allowed.
All dishes in the first week after surgery are steamed; after 7–10 days, small amounts of boiled lean meat and fish are introduced into the diet.
Discharge from the hospital occurs after 1.5 – 2 months.
Home treatment
In the first days after discharge, the patient is recommended to undergo complete physical rest (bed rest). Diet and afternoon naps are mandatory. After 10–14 days, short walks in the fresh air are allowed, the duration of which increases over time. During the rehabilitation period, avoid overwork. Reading, watching TV, walking and light household chores should not last long and should be stopped if the patient feels unwell.
Rehabilitation measures include:
- diet;
- taking insulin tablets (blood glucose regulation);
- multienzyme preparations (promote the absorption of food);
- physical therapy;
- physiotherapy.
Diet food
Diet recommendations for pancreatic necrosis:
- fractional meals up to 6 times a day, in small portions;
- eating at the same time;
- completely eliminate alcohol and smoking;
- food temperature should be at room temperature (excessively hot and cold dishes are prohibited);
- food must be crushed (mashed or finely chopped);
- dishes are steamed, boiled and stewed.
Prohibited products:
- fresh bread and pastries;
- corn, millet, pearl barley;
- beans, peas, beans, lentils;
- fatty meats, poultry and fish;
- chocolate, cocoa, strong tea and coffee;
- canned food and sausages, smoked meats;
- pickles and marinades;
- fast food;
- mushrooms and mushroom broth;
- meat and fish broths;
- spices;
- white cabbage (in any form);
- hot and sour vegetables (sorrel, green onions, radishes, spinach, radish, garlic);
- margarine and animal fats, lard;
- whole milk and fatty fermented milk products;
- eggs in any form and yolk;
- grapes, figs, dates.
Authorized products:
- dried bread;
- low fat cottage cheese;
- vegetable soups;
- porridge with a milk-water mixture (1/1);
- boiled pasta;
- kefir, low-fat yogurt;
- egg white omelette;
- lean fish, meat and poultry (beef, chicken, pollock, flounder);
- boiled vegetables (beets, cauliflower, zucchini, pumpkin);
- diluted freshly squeezed juices;
- butter (no more than 15 grams per day);
- vegetable oil (no more than 30 g);
- unsweetened dry biscuits.
Forecast
With pancreatic necrosis, the prognosis is questionable and depends on many factors (how quickly and adequately treatment was started, the age of the patient, the form of the disease, the presence of concomitant pathology, compliance with medical recommendations and diet, the extent of surgical intervention).
25% of patients who have suffered a destructive form of pancreatitis develop diabetes mellitus. Pseudocysts also often form, chronic recurrent pancreatitis occurs, and pancreatic fistulas form. The mortality rate for this disease is quite high. With aseptic necrosis of the pancreas it is 15–40%, and with an infected pancreas it reaches 60%.