Read more about pancreatitis and methods of treatment
The first stage of the pathology can last up to 10 years, and is characterized by alternating phases of exacerbation and remission.
The patient's main concern is pain. At the second stage of development of pancreatitis, intestinal motor disorders, severe weight loss, and pain are reduced.
Complications can develop at any stage of the disease. Pancreatitis often worsens with the release of digestive enzymes into the blood, followed by severe intoxication.
Conservative therapy is considered the main method of treating pancreatitis. In some cases, according to indications, surgical intervention is performed in which the pancreas is removed - completely or partially. Drug therapy is prescribed depending on the phase of the pathology (exacerbation or remission).
Conservative therapy used for chronic pancreatitis is aimed at relieving inflammation, relieving symptoms, and increasing the duration of the remission period. In this case, there is a real possibility of remission of chronic pancreatitis, that is, you can forget about the symptoms of the disease forever.
What kind of disease is pancreatitis?
What is pancreatitis and how to treat it. Pancreatitis is an inflammatory process in the organ of internal and external secretion - the pancreas. A whole group of diseases and syndromes is defined by this name. When diagnosing pancreatitis, it is necessary to classify what kind of diseases are hidden under the inflammatory process. The World International Organization divides diseases of the pancreas:
- Acute process. It develops suddenly with a clear clinical picture and requires emergency hospitalization in the gastroenterology department.
- Chronic process, including alcoholic pancreatitis and other types. The development of chronic pancreatitis is often the result of an acute form.
- Pancreatic cyst. The emergence of a pathological cavity as a result of inflammatory and destructive processes.
- Pseudocyst. Consequence of an acute or chronic process. It is characterized by the accumulation of large amounts of pancreatic juice surrounded by fibrous tissue.
- Pancreatic steatorrhea. It develops against the background of chronic pancreatitis and is characterized by a violation of the regulatory function of the intestine associated with the digestion and absorption of fats.
Acute pancreatitis is divided into abscess and necrosis of the pancreas, as well as pancreatitis itself, which occurs in the following forms:
- acute;
- recurrent;
- hemorrhagic;
- subacute;
- purulent.
The types of pancreatitis are conditionally divided according to the symptoms that appear and the results of laboratory tests. Pain is the main symptom of inflammation of the pancreas.
Among the types of chronic pancreatitis, obstructive and non-obstructive processes are distinguished. The development of the first disease is characterized by the death of pancreatic cells, followed by the replacement of tissue with connective fibers and the formation of pseudocysts. All functions of external and internal secretion are lost even after treatment of pancreatitis and elimination of the causes that caused the disease. A separate option is calcific pancreatitis, which is the result of the formation of calcifications outside the organ, on the parenchyma and membranes.
Chronic non-obstructive pancreatitis is characterized by the formation of stones in the body of the pancreas, dilation of the ducts and fibrotization of organ tissue. Atrophy of cells that produce enzymes occurs.
Subsequent development of the disease leads to various pancreatic necrosis, which differ in the affected area. This destructive form of pancreatitis is conditional, as the conclusion of pancreatic necrosis is pathological and anatomical and is not used as a diagnosis.
People suffering from diseases of the digestive tract need to know everything about pancreatitis. Impaired functioning of the pancreas will lead to improper secretion and formation of enzymes necessary for the breakdown of useful substances and, as a result, to disruption of the body's metabolic processes. The production of important hormones - insulin and glucagon - will change during inflammation, which will cause the development of other pancreatic diseases, such as diabetes.
The first signs of pancreatitis indicate any changes in the tissues of the pancreas and dysfunction.
While studying pancreatitis, causes and symptoms, remember the important functions that the pancreas performs:
- Participation in metabolic processes during digestion.
- Production of hormones (insulin and glucagon) to participate in the body's carbohydrate metabolism.
The mechanism of the pancreas is quite complex. The organ is unique in its structure and there is no replacement for normal functioning. All destructive processes are irreversible.
Severe form
Before starting treatment for the pathology, the doctor will draw up a treatment regimen depending on the severity of pancreatitis and the patient’s well-being. It is necessary to understand that there are no classical measures when there is inflammation of the pancreas. Medicines for pancreatitis are selected individually.
treatment with tablets for pancreatitis
First of all, in the acute period of pancreatitis, bed rest is necessary. Therefore, if a severe form of the acute course of the disease is observed, then treatment of pancreatitis takes place only in a hospital setting. This is a prerequisite, since inflammatory changes in the gland can lead to disruption of important functions necessary for life.
For 3 days you only need to drink liquid to prevent dehydration and also remove toxic substances from the body.
To alleviate the condition of unbearable pain, medication treatment is prescribed. What medications are best to use to get rid of the problem will be prescribed by your attending physician. Everything will depend on the patient’s well-being, physiological characteristics and the degree of damage to internal organs.
drug treatment of pancreatitis
Drugs for acute pancreatitis include anti-enzyme agents, painkillers and anti-spasm drugs, and antibiotics. And enzyme medications, pills and injections that relieve spasms, anti-inflammatory drugs will help treat chronic pancreatitis. In addition, it is mandatory to use agents that have a choleretic, enveloping effect, and vitamin therapy will also be required.
Replacement therapy
Acute pancreatitis refers to an actively ongoing inflammatory process in the pancreas, which is manifested by pain in the abdomen (especially in the upper part), an increase in the level of pancreatic enzymes found in the urine and blood.
At the same time, with the elimination of the cause of the disease, the manifestations of the disease fade away. The treatment regimen for acute pancreatitis largely depends on what complications arose from the disease. Of the most severe combined pathologies, gland abscess, pseudocyst and necrosis of individual areas or the entire pancreas can be diagnosed. In some cases, the patient's condition may deteriorate sharply, as evidenced by a sharp decrease in systolic pressure (below 90), pulmonary and renal failure, and gastric bleeding (blood loss of more than 500 ml per day).
https://www.youtube.com/watch?v=Ybd5DPWPYJo
The main goal facing the doctor is to eliminate systemic complications of the disease, prevent the death of pancreatic tissue and the occurrence of infection if necrotic processes have already begun. Complications include a sharp decrease in blood pressure and renal and respiratory failure. To treat such complications, the drugs Calcitonin, Somatostatin, Glucagon and others are used.
As a result of the disease, low blood pressure and difficulty breathing are often observed, which require medication to eliminate.
In practice, it has been noted that the risk of systemic complications is greatly reduced if patients do not have stones in the common bile duct. Therefore, in the first days of hospital stay, stones are removed using a probe.
Infusion therapy in such patients is intended to prevent pancreatic necrosis. As for infection of dead areas of the gland, Escherichia coli (Escherichia coli) and Klebsiella are more often found here. Much less common are staphylococcus and streptococcus. Despite the fact that there is now debate about the effectiveness of antibiotics, they are still used in patients with pancreatic necrosis. The gland tissue is most susceptible to Ciprofloxacin and Ofloxacin.
In the absence of systemic complications, pancreatitis is classified as mild, uncomplicated. Treatment of the disease is carried out in the form of maintenance treatment. It is important that the patient replenishes the body fluids that he lost as a result of vomiting. If the patient experiences a decrease in the volume of blood circulating in the vessels, then the disease threatens to worsen and necrotize the gland. In this case, a blood transfusion is possible.
In some cases, pancreatitis may require a blood transfusion
To relieve pain symptoms, narcotic analgesics Meperidine or Hydromorphone are prescribed under strict medical supervision. If infectious complications occur, antibacterial treatment is carried out. After the pain subsides and peristalsis is restored, the patient can eat little by little.
If the secretion produced is insufficient, replacement therapy is carried out, which significantly relieves the load on the organ. The following requirements apply to drugs of this type:
- they must contain a high amount of lipase (from 20 to 40 thousand units);
- have a strong shell from digestion in the stomach;
The presented drugs alleviate the patient's condition with chronic pancreatitis
- small granule size;
- rapid evacuation of granules in the upper intestines;
- lack of bile acids.
Patients with chronic pancreatitis are recommended Mezim, Creon, Penzital, Festal, Panzinorm and other drugs, as well as a low-fat diet.
If enzyme replacement treatment does not bring positive results, then Paracetamol, Ibuprofen, Celecoxib, Lornoxicam, Meloxicam, Nimesulide, Naproxen are used to treat the pain syndrome of chronic pancreatitis. Octreotide (another name is Sandostatin) has a very good effect. With the help of the drug, pancreatic secretion is inhibited and the release of cholecystokinin and secretin is reduced. The positive effect of the drug has been proven in more than half of the patients.
In the presence of acute pain, these drugs are used
Before starting treatment for the pathology, the doctor will draw up a treatment regimen depending on the severity of pancreatitis and the patient’s well-being. It is necessary to understand that there are no classical measures when there is inflammation of the pancreas. Medicines for pancreatitis are selected individually.
treatment with tablets for pancreatitis
First of all, in the acute period of pancreatitis, bed rest is necessary. Therefore, if a severe form of the acute course of the disease is observed, then treatment of pancreatitis takes place only in a hospital setting. This is a prerequisite, since inflammatory changes in the gland can lead to disruption of important functions necessary for life.
For 3 days you only need to drink liquid to prevent dehydration and also remove toxic substances from the body.
To alleviate the condition of unbearable pain, medication treatment is prescribed. What medications are best to use to get rid of the problem will be prescribed by your attending physician. Everything will depend on the patient’s well-being, physiological characteristics and the degree of damage to internal organs.
drug treatment of pancreatitis
Drugs for acute pancreatitis include anti-enzyme agents, painkillers and anti-spasm drugs, and antibiotics. And enzyme medications, pills and injections that relieve spasms, anti-inflammatory drugs will help treat chronic pancreatitis. In addition, it is mandatory to use agents that have a choleretic, enveloping effect, and vitamin therapy will also be required.
In case of exacerbation of the disease, you should immediately consult a doctor for help in order to properly treat the exacerbation of chronic pancreatitis. By contacting a medical specialist, the patient can learn in detail about what medications are best to treat chronic pancreatitis; individual dosages of the recommended medications are also important.
In the process of treating a chronic form of the disease, several different methods of medical influence on the body are used. The range of treatment methods includes:
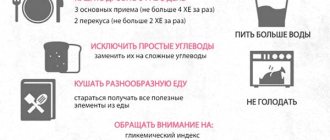
- diet;
- elimination of emerging pain symptoms;
- restoration of the normal state and functioning of the organs included in the digestive system;
- elimination of pancreatic enzyme deficiency;
- stopping processes of an inflammatory nature in organ tissues;
- restoration of normal functioning of organ tissues;
- prevention of complications.
This list of methods represents a certain standard approach to treating the disease; most attending physicians adhere to it. During the treatment process, the doctor takes into account the individual characteristics of the patient and decides how best to treat exacerbation of chronic pancreatitis in each specific case.
Often patients suffering from pancreatitis wonder where chronic pancreatitis in the acute stage is treated. Most often, doctors recommend treating chronic pancreatitis in the acute stage in a hospital setting. This allows you to more quickly respond to changes in the body’s condition and make timely adjustments to the process of carrying out medical procedures and taking medications.
The main objectives in the treatment of pancreatitis during an exacerbation are:
- relief of pain;
- correction of organ function.
To reduce pain during an exacerbation, you should adhere to a special strict diet recommended by your doctor.
If severe pain occurs, non-narcotic painkillers such as Aspirin or Diclofenac may be prescribed. These drugs help reduce the intensity of the inflammatory process, which in itself helps reduce pain.
Painkiller for pancreatitis
For very severe pain, doctors may prescribe Octreotide. This medication suppresses the synthesis of hormones that stimulate the functioning of the pancreas. The drug is used only if the patient is being treated in a hospital.
With the long-term development of the disease, the normal tissue of the organ is replaced by connective tissue, which provokes the occurrence of serious disturbances in the functioning and loss of functions characteristic of the pancreas.
In order to correct the activity of the organ, a course of special medications containing pancreatic enzymes is prescribed. Such drugs include Mezim, Pancreatin, Festal and some others. Taking pancreatic enzymes helps normalize the digestion process and reduce pain symptoms. Such properties of the drugs make it possible to relieve the pancreas to some extent and reduce the load placed on it.
Long-term progression of chronic pancreatitis leads to disturbances in the production of insulin by the gland, which is a hormone that controls glucose metabolism in the human body. An insufficient amount of this hormone provokes the development of diabetes.
When a period of remission occurs after an exacerbation, patients are interested in how chronic pancreatitis can be treated at home. As a rule, upon discharge from the hospital, doctors give the patient a whole list of recommendations on how to carry out medical procedures and take medications at home during the period of remission.
When treating chronic pancreatitis at home, you can use various folk remedies. Your doctor can tell you what to use and how to treat chronic pancreatitis with folk remedies. It is not recommended to use this treatment without consulting a doctor.
One of the folk remedies for treating pancreatitis is clove
Types of chronic pancreatitis
The concept of “chronic pancreatitis” includes a whole group of pathologies. Chronic pancreatitis has several classifications.
Classic classification:
- Toxic-metabolic. Formed under the influence of drugs or alcohol.
- Idiopathic. It is formed without obvious prerequisites.
- Hereditary. Occurs when there is a genetic malfunction in the body.
- Autoimmune. Appears subsequently due to the impact of the body’s immune system on the pancreas.
- Recurrent. It is characterized by long periods of remission, which alternate with periods of exacerbation.
- Obstructive. It develops as a result of compression or blockage of the gastric ducts.
- Primary. Forms without a primary disease.
- Secondary. Appears as a complication of another pathology.
Classification according to M.I. Cousin:
- Primary: alcoholic, unknown etiology, medicinal, metabolic or dietary disorders.
- Post-traumatic: against the background of pancreatic injury (after surgery).
- Secondary: provoked by other diseases.
Classification according to the international system M-ANNHEIM (2007):
- According to clinical stage.
- By origin (risk factor) (from A to M type).
- According to the severity of the disease (grading system is used).
Causes
The main causes of acute pancreatitis:
- Genetic predisposition.
- Alcoholism and alcohol abuse (70% of cases).
- Cholelithiasis.
- Autoimmune problems (when the immune system attacks its own cells)
- Parasites such as roundworms can also cause blockage in the pancreas.
- Blockage of the pancreatic duct or common bile duct, such as a gallstone.
- Damage to the ducts and pancreas during surgery.
- Complications of cystic fibrosis.
- Kawasaki disease.
- Reye's syndrome.
- Hemolytic uremic syndrome.
- Hyperparathyroidism.
- High content of fats in the blood - triglycerides (hypertriglyceridemia).
- Poor blood circulation of the pancreas.
- Trauma to the pancreas as a result of an accident.
- Viral infections, including mumps, mycoplasma, pneumonia, and campylobacter, hepatitis C.
- Diseases of the duodenum, small and large intestines, accompanied by constipation, such as peptic ulcer, enteritis, colitis, enterocolitis, diverticula.
- Use of certain medications (especially estrogens, corticosteroids, thiazide diuretics, and azathioprine).
Chronic pancreatitis often develops in people who are between 30 and 40 years of age and is most often caused by alcohol abuse over many years, with men predominating over women. Repeated episodes of acute pancreatitis can lead to chronic pancreatitis. In some cases, genetics may be a factor in its development. In 10-15 cases of chronic pancreatitis, the cause is unknown.
Other factors that are also associated with chronic pancreatitis:
- Autoimmune problems;
- Use of estrogens, corticosteroids, thiazide diuretics, and azathioprine;
- Blockage of the pancreatic duct or common bile duct;
- Hypercalcemia - high levels of calcium in the blood;
- Hyperlipidemia or hypertriglyceridemia - high levels of fats in the blood;
- Metabolic disorders, especially fats, associated with overeating;
- Complications of cystic fibrosis, the most common hereditary disorder, when the secretions secreted by various organs are too viscous and thick.
Due to chronic inflammation, scarring occurs on the pancreas, and the organ becomes unable to produce the required amount of digestive enzymes. As a result, the body may be unable to digest fat and other important food components. Damage to the part of the pancreas that produces insulin can lead to diabetes.
Enzymes and antienzyme drugs for pancreatitis
To normalize the acidity of gastric juice, the doctor prescribes medications containing substances that replace the digestive enzymes produced by the pancreas. This is amylase, which promotes the processing of starch into sugars, as well as protease and lipase (the first breaks down the compounds between amino acids in proteins, the second - fats).
For the treatment of pancreas, enzyme medications containing pancreatin are prescribed. It breaks down fats, proteins and carbohydrates, replacing amylase, lipase, protease:
- Festal. In addition to pancreatin, the composition contains hemicellulose and bovine bile extract. The medicine promotes not only the digestion and absorption of food, but also the breakdown of fiber, improves bile secretion, and activates lipase. Dose: 1 tablet per day after or during meals.
- Creon. Release form: capsules 150, 300, 400 mg of pancreatin. The dosage depends on the clinical picture of the disease; it is taken during or after a meal.
- Panzinorm 10000 and 20000. Available in capsules, drink 1 tablet with meals three times a day.
- Digestal. Release form: pills. Take 1-2 pcs after or during a meal. three times a day.
- Mezim 10000 and 20000. Available in tablets, capsules, dragees. Take 1-2 pcs before or after a meal. one to three times a day.
If the pancreas is swollen, its activity should be suppressed. To do this, the doctor prescribes intravenous administration of antienzyme drugs. Among them, Kontrikal or its analogue Aprotinin should be highlighted. They inactivate proteinase and have an inhibitory effect on the kallikrein-kinin system, a group of proteins that are actively involved in inflammatory processes, blood clotting, and pain.
When symptoms of the disease appear, treatment in adults is initially carried out by a therapist and a series of tests are prescribed. Before using medicine for pancreatitis, visit a gastroenterologist who will prescribe a course of treatment that is suitable for the sick patient in all respects. Medicinal treatment with drugs will help improve your well-being, but you will not be able to get rid of the disease using drugs. Thanks to a nutritionist, a diet will be determined and a diet will be prescribed.
structure of the pancreas
- Medicines in tablets and injections that relieve spasms and have an analgesic effect.
- Antacids.
- Enzyme and antienzyme agents.
- H2-blockers of histamine receptors.
- Groups of sedative drugs.
Specific medications, quantity and dose are regulated by the doctor. This is due to the fact that during the drug treatment of chronic pancreatitis, it is prohibited to take many medications.
If the damage to the gland involved the cells responsible for the production of the hormone insulin, the package of standard remedies includes insulin agents. The optimal medication is selected by an endocrinologist.
endocrinologist during illness
Such treatment causes the development of unpredictable consequences. When the gland becomes inflamed, drugs alone cannot cure it. Dietary nutrition and adherence to a proper lifestyle are required.
Be sure to follow your doctor’s recommendations, because if the acute form of pancreatitis is not treated correctly, it will become chronic.
Enzymes
To change the acidity level in the stomach and improve the functioning of the gland, you can use enzyme and anti-enzyme drugs. Medicines and their dosage are selected exclusively by a doctor.
In this case, it is important to alternately take means of different effects.
pancreatic enzymes for pancreatitis
- helps break down proteins, fats and carbohydrates;
- flatulence, bloating and stomach cramps decrease;
- stimulates the absorption and digestibility of beneficial elements from consumed foods;
- releases the gland, improving the patient's condition.
Enzymes are effective if therapy for pancreatitis is long-term. The doctor monitors the effectiveness of the drug taken, leaving it for subsequent use or replacing it with a similar one.
It is important to take enzyme medications for pancreatitis during meals or immediately after. If you take the pills on an empty stomach, even greater inflammation of the organ is possible.
attending physician during illness
High-quality, good enzymatic preparations contain an extract from the gland of cattle, which is identical to the substance produced by the human gland - pancreatin. It helps break down foods into molecules that the intestines and stomach will absorb and assimilate into the body.
If you receive pancreatin in sufficient quantities, the body will compensate for the lack of pancreas. All elements that come with food are well digestible, and the patient does not face the problem of exhaustion and vitamin deficiency.
tablets for pancreatitis
- Festal.
- Mezim.
- Creon.
- Pancreatin.
- Panzinorm.
- Digestal.
These drugs are enzymatic. They have different mechanisms of influence and composition, so the specialist will indicate which one is best to take for the treatment of pancreatitis in a particular situation:
- degree of inflammation of the gland;
- changes in the activity of other organs - gall bladder, intestines, liver.
When using antienzyme agents for treatment:
- intoxication of the body is reduced;
- pain syndrome decreases;
- the patient’s well-being improves;
- the threat of death is reduced;
- the development of edema and tissue necrosis is blocked.
anti-enzyme drugs after an attack
The following drugs in this group are distinguished:
- Gordoks.
- Contrikal.
- Trasylol.
- Trascolan.
- Ingitril.
Antienzyme drugs are administered in a hospital into a muscle or into a vein on the first day after an attack of the disease. Such medications are necessary to stop further tissue inflammation as a result of the release of pancreatic secretions.
Often, patients use traditional methods to treat diseases, since they are natural and do not have side effects and solve the problem. However, admission is also impossible without the approval of a doctor.
One of the folk remedies is chaga. It is allowed to be used in the treatment of diseases of the gastrointestinal tract and pancreas only after diagnosis and following the doctor’s recommendations.
chaga mushroom and its benefits for pancreatitis
Pancreatitis can be treated with chaga when the acute stage of the disease is over, since an exacerbation can increase the secretion of the gland.
Chaga for the glands is often prescribed as a tea. Thanks to this tool you can:
- eliminate signs of illness - nausea, dizziness;
- restore mucous tissue;
- remove toxins from the body;
- increase hemoglobin;
- prevent the growth of pathogenic bacteria.
Pharmacy chains sell preparations based on the fungus in the form of pills or a concentrated extract. Chaga is found in the composition of individual remedies for the treatment of pancreatitis of the homeopathic spectrum, Badakh. However, a natural infusion is more effective.
To make an infusion, the chaga is washed out and placed in boiling water. The mushroom stays like this for several hours. Then it is crushed, and the mushroom is poured with standing heated water again. Store this product for no more than 4 days. Treatment with the drink is carried out in 3 doses of 200 grams per day.
If you take the medicine during an exacerbation, complications arise. Chaga is not allowed to be taken for pancreatitis if there is an ulcer in the intestines or stomach.
When pancreatitis worsens, it is necessary to temporarily inhibit the production of gastric juice. This procedure is temporary, then it will need to be stimulated for the normal functioning of the digestive system.
Medicines for exacerbation of pancreatitis:
- Ranitidine.
- Cimetidine.
- Nizatidine.
drugs for exacerbation of pancreatitis
A group of anti-inflammatory drugs will be required in case of acute inflammation. But it is undesirable to take such pills for pancreatitis, since the true dynamics of the disease may be missed.
In addition, the drugs have side effects and are not prescribed for more than 10 days:
- Diclofenac.
- Nise.
- Ibuprofen.
- Nimesulide.
To absorb and remove harmful elements from the body, in the fight against pathogenic intestinal microflora, a drug with a wide spectrum of effects, Polyphepan, is prescribed. Natural medicine. Its analogue is Enterosgel. It is often used to treat pancreatitis. The medicine is taken together with other drugs in the treatment of illnesses that are associated with poisoning.
acipol
Acipol will help with intestinal damage, dysbacteriosis, and allergic manifestations. It will bring the intestines back to normal.
Iberogast
Iberogast is prescribed to improve digestion. The drug also tones and has a choleretic effect.
One of the herbal medicines that treats the biliary tract is Flamin. This remedy is cholekinetic, it relieves spasms and inflammation, helps to produce the required volume of bile. Similar drugs include:
- Hepasin;
- Hepel N.
Before starting treatment, you need to understand what pills to take for pancreatitis, why they help, and know about possible side effects and contraindications. Therefore, it is important to consult a doctor about this.
Useful decoction
To support the functioning of the gland during the chronic development of pancreatitis, folk remedies are used, including in this case herbs and decoctions from them. Drink a decoction of immortelle and wormwood. Parsley and its root part have a beneficial effect on the function of gastric juice secretion.
Decoctions can be complex and include several types of herbs. The main thing during treatment is to follow the dose and recipe.
decoction for pancreatitis
During the recovery period, a decoction of green onions with parsley, St. John's wort and mint is prepared. For acute inflammation, mint with yarrow and cudweed are used.
Choleretic drugs for pancreatitis are replaced with herbs that have a milder effect. Herbs are selected individually.
traditional medicine cholagogues
- Burdock root, chicory.
- Dog-rose fruit.
- Turmeric.
- Corn silk.
- Aloe.
Folk remedies
The following traditional medicines are used to treat pancreatitis:
- Collection of herbs. To prepare the collection, take string, cudweed, horsetail, chamomile and calendula flowers, St. John's wort, wormwood and sage in equal quantities. The herbs are mixed and crushed. Then prepare an infusion (take a tablespoon of the collection per glass of boiling water, infuse for an hour, strain). The infusion is consumed three times a day, half a glass, half an hour before meals.
- Two leaves of golden mustache are poured into 0.5 liters of boiling water, placed on low heat and boiled for 15 minutes. Then cool the mixture for 8 hours. Before use, the infusion is heated to a warm state in a water bath and drunk before meals (half an hour before). You need to drink three tablespoons of infusion a day.
- Take burdock, elecampane and dandelion roots in equal quantities, chop and mix them. The resulting mixture is placed in boiling water (a dessert spoon of the mixture per glass of water), boiled for 15 minutes, then infused for an hour. After this, the infusion is filtered and drunk before meals, a tablespoon, three times a day.
- Carrot and potato juice. Take two carrots and two potatoes, squeeze the juice out of them and drink them on an empty stomach, in the morning, for a week.
- Infusion of motherwort, immortelle and calendula. Take one tablespoon of the above herbs, mix and pour a liter of boiling water. Cover the resulting mixture with a cloth, leave for an hour, then filter. You need to take the resulting decoction 6 times a day, half a glass.
- Barberry bark is taken and crushed. Then the crushed barberry bark is added to boiling water (a teaspoon of bark per glass of water), boiled for 15 minutes, after which the resulting decoction is cooled and consumed before meals, a tablespoon, three times a day.
- Take cumin seeds (2 teaspoons), pour a glass of hot water and leave for 2 hours. Then the mixture is filtered and taken three times a day, before meals, half a glass.
It should be remembered that folk remedies can be used in the treatment of pancreatitis only as additional therapy and only with the permission of a doctor.
Strict adherence to nutrition and diet, complete abstinence from drinking alcohol, strict adherence to recommendations for drug treatment significantly reduce the frequency of exacerbations, transforming the process into a rarely relapsing variant with slow progression. In some patients it is possible to achieve noticeable and lasting remission.
Chronic pancreatitis is characterized by a progressive course, however, cessation of exposure to causative factors and adequate therapy slow down the progression of the disease and significantly improve the quality of life of patients and the prognosis.
medsimptom.org
Symptoms of pancreatitis
With pancreatitis, patients suffer from acute pain in the abdomen, usually in the left region, the pain can radiate to the back. Intoxication is pronounced, expressed in the form of nausea, vomiting, general weakness, rising temperature, loss of appetite. The stool is mushy, oily, and contains undigested food particles.
In some cases, the disease may be asymptomatic, but digestive problems are still present; this can be expressed in heaviness present in the lower part of the stomach or slight numbness after eating food or alcohol.
The pancreas synthesizes digestive enzymes and hormones that regulate protein, fat, and carbohydrate metabolism - insulin, glucagon, somatostatin. The organ has an oblong shape and is located in the upper abdomen, behind the stomach, in close contact with the duodenum. Iron weighs about 70 g, length ranges from 14 to 22 cm, width - from 3 to 9 cm, thickness - 2-3 cm.
Inflammation of the pancreas can occur in acute and chronic forms, the clinical manifestations of which are different. Acute pancreatitis is deadly, since toxins can provoke necrosis of pancreatic tissue and other organs, infection, and purulent processes. Even with timely treatment with modern means, the mortality rate is 15%.
There is no clearly defined clinical picture for acute pancreatitis, so additional examinations are necessary for an accurate diagnosis. In the acute form of the disease, false cysts often form in the pancreas, which cause pain in other organs and disrupt the movement of food through the stomach and intestines. In addition, the pathology manifests itself with the following symptoms:
- acute pain in the upper abdomen, radiating to the left side, back;
- nausea;
- vomiting with bile, which does not bring relief;
- bloating;
- dehydration;
- Jaundice may develop, accompanied by yellowing of the skin, dark urine, and light-colored feces;
- in some cases, bluish spots appear near the navel or on the left side of the abdomen, sometimes with a yellow tint.
With chronic inflammation, irreversible changes occur in the pancreas. It shrinks, the ducts narrow, the cells are replaced by connective tissue, which is why the organ ceases to perform its functions, and the synthesis of digestive enzymes and hormones decreases. Chronic pancreatitis is characterized by a vague clinical picture; its symptoms can easily be confused with other diseases of the digestive system.
The disease develops gradually and does not make itself felt for a long time. The pathology manifests itself as constant or periodic pain in the abdomen, near the left hypochondrium, and can radiate to the lower back. The disease is accompanied by nausea, vomiting, belching, heartburn, and an unpleasant sour taste in the mouth. Diarrhea may alternate with constipation; particles of undigested food are released along with feces.
Causes and symptoms of the disease
Additional agents used include pancreatic enzyme inhibitors: Trasylol, Contrical, Gordox, Delargin. For example, trasylol, 10-15 thousand units in 5% glucose or 0.9% sodium chloride is administered intravenously (drip) until acute symptoms subside (approximately 7-10 infusions per course).
To stop steatorrhea, coated drugs with increased doses of lipase are added.
The main reasons leading to the development of the disease are considered to be the following:
- alcoholism in chronic form: frequent consumption of alcoholic beverages in large quantities significantly contributes to the development of a large number of various pathologies in the body, including chronic pancreatitis;
- diseases of the liver and ducts that provide bile excretion in a chronic form;
- diseases of the digestive tract;
- chronic eating disorder;
- long-term use of certain medications that provoke the development of an inflammatory process in the pancreas;
- hereditary predisposition;
- duodenal ulcer.
The main symptoms of CP are considered to be the following:
- pain in the abdomen that intensifies after eating;
- the occurrence of a feeling of nausea after eating foods rich in fat, a single urge to vomit;
- yellowness of the skin, sclera of the eyeballs and oral mucosa;
- the development of diabetes mellitus in the later stages of the disease.
The development of pancreatitis in chronic form occurs quite slowly - over several years. For this reason, when the first symptoms of the disease appear, a person most often does not pay attention to them, and without examining the body, he does not think about the question of how to treat chronic pancreatitis, and what drugs are best to use for this.
If two pathologies are detected simultaneously, you should resort to their comprehensive treatment. Therapy should be carried out under the supervision of a medical specialist and in accordance with his recommendations on how to treat chronic pancreatitis and cholecystitis.
To relieve pain, they resort to non-coated products with high doses of proteases
When the gland becomes inflamed, the patient experiences severe pain on the left side under the ribs, in the upper abdomen. The discomfort can be so unbearable that it is impossible to stand, sit, talk, or breathe. It happens that the pain syndrome affects the back, between the shoulder blades, and the lower back. These zones indicate which part of the organ is affected.
To eliminate pain, the following drugs are used for pancreatitis:
- non-steroidal group – Paracetamol, Ibuprofen;
- strong analgesics - Baralgin, Analgin.
To relieve pain when its manifestations are unbearable, narcotic analgesics are prescribed, which are administered intramuscularly:
- Buprenorphine.
- Tramadol.
Painkillers should not be used regularly, even if they do not contain narcotic substances and they do not cause habit.
painkillers for pancreatitis
- Drotaverine.
- Spasmalgon.
- No-shpa.
- Spasmol.
- Riabal.
These medications have the following effects on illness:
- alleviate the patient’s condition by eliminating pain;
- reduce the load on the organ, helping to improve the output of digestive effects.
Medicines that prevent or weaken the effect of acetylcholine and cholinomimetic drugs will help defeat the disease.
Medicines prevent pathological impulses in the nerve ganglia and brain.
The working course of the gastrointestinal tract returns to normal:
- Atropine.
- Chloroquine.
- Spasmolitin.
- Platyfillin.
If the combination of enzyme preparations and H2 histamine blockers is ineffective, the treatment regimen for pancreatitis may include drugs with analgesic and anti-inflammatory effects from the NSAID group (paracetamol, diclofenac, ibuprofen, piroxicam).
It is recommended to use analgin-containing mixtures (for example, from analgin, novocaine and no-shpa or ready-made baralgin, spasmalgon intramuscularly or intravenously).
In a hospital setting, octreotide is prescribed for severe pain. It is a strong inhibitor of neuroendocrine hormones acting on the digestive system. A dose of 200 mcg administered subcutaneously three times daily for a month contributed to a significant reduction in pain severity.
Surgical treatment of pancreatitis is indicated if pain relief cannot be relieved with conservative therapy.
Treatment with myotropic antispasmodics
Another option for the treatment of chronic pancreatitis, namely pain, is taking myotropic antispasmodics, which can reduce smooth muscle tone and motor activity. The most popular drugs in this group for the treatment of pancreatitis are drotaverine derivatives: No-shpa, Vero-drotaverine, Drotaverine hydrochloride, etc.
Dspatalin and Bencyclane are also used. They are presented under the pharmaceutical names Mebeverine and Halidor, respectively. The effect of hymecromone, which forms the basis of the drug Odeston, has also been proven. The main “merit” of the drug is a decrease in intraductal pressure, which significantly accelerates the flow of bile into the intestines in conditions of chronic pancreatitis.
If the pain does not stop, a diagnostic examination of the gland ducts with a probe is indicated in order to determine the nature of their damage. In the absence of positive effects from treatment, the regimen is supplemented with surgical intervention.
Features of taking medications for pancreatitis
In some cases, with chronic inflammation of the pancreas, doctors prescribe sedatives that have a calming effect on the nervous system and reduce emotional stress. These drugs not only reduce depression, but also enhance the effect of pain medications for pancreatitis. Among these drugs are:
- Doxepin;
- Amitriptyline;
- Glycine;
- Phenibut.
If the pancreas is inflamed, the doctor may prescribe hormonal therapy. To suppress the production of pancreatic and gastric juice, Octreotide is used, an analogue of the hormone somatostatin, which is used to treat tumors. Corticosteroids (eg, Prednisolone) are prescribed if chronic inflammation is caused by an autoimmune disease. Hormonal therapy for a certain period of time, since long-term treatment can cause many side effects.
In chronic pancreatitis, indigestion accompanied by diarrhea is often observed. Enzyme deficiency slows down the digestion of food, which is why food is retained in the gastrointestinal tract, and bacteria settle in it, causing rotting processes, causing diarrhea and flatulence. Sorbents can cope with this problem.
Antibiotics are used to destroy pathogenic bacteria that provoke infectious complications: rupture of the pancreatic duct, bile stagnation, inflammation of the bile ducts, the appearance of cysts, bacterial infections. Drugs for acute pancreatitis are prescribed by injection, since in case of exacerbations it is necessary to act quickly.
- Ceftriaxone, Cefotaxime from the group of cephalosporins;
- Amoxiclav from the penicillin group;
- Thienam from the thienamycin group;
- Ampiox is a combination medicine of the antibiotics Ampicillin and Oxacillin;
- Vancomycin is from the group of tricyclic glycopeptides.
To prevent swelling of the pancreas and remove excess enzymes and poisons from the body, doctors prescribe diuretics - diuretics. For pancreatitis, Furosemide and Diacarb are prescribed in combination with potassium supplements. You should take diuretics strictly as directed by your doctor, since improper use can destroy pancreatic cells, provoke an increase in creatinine and urea in the blood, a severe decrease in blood pressure and other reactions.
The doctor must prescribe a treatment regimen and explain which medications for the pancreas should be taken after and which ones during meals. For example, enzyme medications for pancreatitis are taken simultaneously with meals, while antibiotics are taken after, proton pump inhibitors are taken once a day. Painkillers can be taken if necessary at any time, strictly following the dosage indicated in the instructions.
All tablets for pancreatitis should be taken with plenty of clean drinking water. During illness, alcohol is strictly prohibited, the toxins of which have a destructive effect on all cells of the body, including the pancreas. The combination of drugs with ethanol will increase the load on the liver, kidneys, and other organs of the digestive tract, leading to serious complications.
Any medicine can cause side effects and has contraindications, so before use you must read the instructions and tell your doctor about any chronic diseases. If a medicine for pancreatitis provokes complications and serious side effects, it should be discontinued immediately, replacing it with another active ingredient.
The duration of treatment with each specific drug is prescribed by the doctor. For example, antibiotics should not be taken for more than two weeks, as bacteria become addicted and the medications become ineffective. It is impossible to interrupt the prescribed therapy, since this can not only reduce the effectiveness of treatment, but also provoke a relapse of the disease.
For treatment to be effective, you must adhere to a diet. In the acute form of the disease, a hunger strike is indicated in the first two days, after which you can begin to eat low-calorie foods. Fatty, spicy, salty, peppered, smoked foods and other dishes that stimulate the secretion of gastric juice and gas formation in the intestines are prohibited.
To restore liver cells, tablets for pancreatitis are used: Essentiale Forte. The drug is used in parallel with the prescription of antibiotic drugs.
Prescribe the medicine 1 capsule 3 times a day during meals. The product is used in courses, as prescribed by a doctor. Phospholipids, which are present in the composition, are aimed at restoring and protecting cells. It has a good effect on metabolism and has few side effects. An overdose does not pose a health risk.
Rezalut pro, Essliver Forte. for cell protection
Medicines for pancreatitis in adults have the following analogues:
- Rezalut about;
- Essliver Forte.
Treatment of pancreatitis depending on the severity of pain
Since the main cause of exacerbation is the activation of infection and inflammation of the pancreas, first of all, antibacterial and anti-inflammatory therapy is carried out: enteroseptol or intestopan penicillin, ampicillin in the form of 2-3 week courses.
Pancreatitis in remission
A positive effect is achieved by prescribing a strict diet. Meals are divided, food is taken every three hours. Sharply limit the proportion of fat to 60 grams per day. These measures help reduce pancreatic secretion, which helps reduce inflammation and reduce pain.
The main cause of pain in chronic pancreatitis lies in increased intraductal pressure. It is possible to influence it by prescribing medications that reduce pancreatic secretion.
Intake of pancreatic enzymes into the body in the form of tablets (mezim forte or pancreatin, which is better you can find out on our website in the drug treatment section)
Due to the inclusion of feedback, it will reduce the production of gastrointestinal hormones, and therefore reduce the excretory function of the pancreas. The pain will be relieved by reducing the pressure in the ducts and tissues of the organ.
To avoid neutralization of enzymes by gastric acid and pancreatic proteases, H2 histamine receptor blockers (famatidine, ranitidine and others) are added to the treatment regimen.
The drug of choice is Creon. This is a pancreatic enzyme preparation, which is a capsule that contains microspheres that are resistant to acidic environments. After taking the drug, complete release of enzymes occurs quickly within an hour when the acidity of gastric juice is 5.5 or higher. At higher acidity, it is advisable to prescribe H2 histamine receptor inhibitors.
In addition to relieving pain, taking enzymes stimulates peristalsis of the gastrointestinal tract. More efficient and complete breakdown and absorption of nutrients occurs. Digestion occurs in a more gentle manner.
Diagnostics
Various methods are used to determine chronic pancreatitis, but many of them cannot detect the disease in the early stages. Most diagnostic errors are explained by the multisymptom and phase nature of the manifestations of this disease. The correct diagnosis is determined only after a comprehensive examination, including:
- Fecal analysis.
- Urine analysis.
- General blood test - to determine signs of the inflammatory process by the number of leukocytes, the growth of ESR and other data.
- Biochemical blood test (to determine the level of pancreatic enzymes).
- Ultrasound of the abdominal cavity.
- Gastroscopy.
- Endoscopic retrograde cholangiopancreatography (ERCP).
- X-ray of the abdominal cavity.
The formation of chronic pancreatitis occurs very slowly, over several years.
When are antibiotics used?
For the treatment of pancreatitis, antibiotics are prescribed extremely rarely and only after the results of a complete examination are available.
In hospitals, antibacterial therapy is used in the form of injections if the doctor sees that the situation is critical and the patient needs urgent help. Antibiotics for acute pancreatitis are prescribed to relieve inflammation and relieve the organ as much as possible:
- Doxycycline.
- Cefuroxime.
Treatment of the chronic course of the disease is possible with oral antibiotics:
- Amoxiclav.
- Cefotaxime.
- Ampicillin.
- Abaktal.
- Vancomycin.
It is important to remember that medications are taken only after a doctor’s prescription.
Medicine to protect cells
To restore liver cells, tablets for pancreatitis are used: Essentiale Forte. The drug is used in parallel with the prescription of antibiotic drugs.
Prescribe the medicine 1 capsule 3 times a day during meals. The product is used in courses, as prescribed by a doctor. Phospholipids, which are present in the composition, are aimed at restoring and protecting cells. It has a good effect on metabolism and has few side effects. An overdose does not pose a health risk.
Rezalut pro, Essliver Forte. for cell protection
Medicines for pancreatitis in adults have the following analogues:
- Rezalut about;
- Essliver Forte.