Diagnostic examination
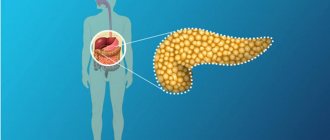
Diagnosis of pancreatitis (codes K85.0/86.0) consists of laboratory and instrumental research methods. The gold standard is ultrasound. The procedure is painless and accessible, allowing you to evaluate the structure and size of the pancreas. During an ultrasound scan, cysts, tumors, and also a picture corresponding to diffuse changes in the organ are detected. A type of ultrasound is elastography. The method allows a detailed assessment of the elasticity of the fabric. It is a non-invasive biopsy.
During a computed tomography scan, the diameter and shape of the organ are determined. CT visualizes not only pancreatic formations, but also possible regional metastases. Cholangiopancreatography is used for a detailed assessment of the gland ducts. Using a flexible endoscope, contrast is injected into the common bile duct and a scan of the organ is performed.
Laboratory diagnosis consists of blood, stool and urine tests. The level of sugar and amylase is determined in the blood, diastase in the urine, and the level of pancreatic elastase and undigested fats in the feces.
The function of the gland is determined to prescribe enzyme and hormonal therapy. Early diagnosis increases the patient's chances of a full recovery.
Signs of reactive changes in the pancreas in a child
Before talking about the signs, it doesn’t hurt to dwell on the reasons for the “explosive” reaction in the children’s pancreas.
Do you recognize an example? Nature, a dacha, a river bank, pork neck kebab, fried sausages, chicken wings, steaks - everything is “healthy” for a child. And, of course, with ketchup or mayonnaise - the child loves it. Then, for a sincere conversation, beer for the parents, and a colored drink with chips, fried peanuts, salted crackers, and dried fish sticks for the child. Pie for dessert. And at night, or even in the evening, parents dial “03” in a panic.
An unconvincing example? Then you can remember the fried chicken for grandma’s birthday or shawarma from a booth on the street, eaten right there, with the help of dirty children’s hands.
Unfortunately, there are more than enough examples of negligent and often criminal carelessness of parents.
Video from Dr. Komarovsky about digestive problems in children:
Now about the signs themselves. Reactive pancreatitis in children has characteristic symptoms that parents simply must know.
The most striking of them:
- bouts of vomiting that do not provide relief to the child;
- painful yellow color of the skin;
- dark colored urine;
- unnaturally light-colored stool;
- high temperature, chills, fever.
When helping a child, inexperienced mothers rely on someone else’s experience and their own know-it-all attitude. At the same time, pancreatitis begins to be uncontrollably suppressed with a horse dose of antibiotics.
As a result of this violence, the child’s fragile pancreas responds with vomiting and fever, and dysbiosis becomes the cause of uncontrollable diarrhea, dehydrating the body, which further aggravates the baby’s condition.
Important! Do not self-medicate - this is dangerous not only for the health, but also for the life of the child. Contact a doctor or call an ambulance immediately.
Definition and classification of acute pancreatitis according to ICD-10
There is a division of chronic pancreatitis into primary (primary inflammatory process of the unchanged pancreas) and secondary, developing against the background of cholecystitis, gastritis, enteritis and other diseases. Marseille-Roman classification of chronic pancreatitis: 1. Chronic calcific pancreatitis. 2.
Chronic obstructive pancreatitis. 3. Chronic fibrous indurative pancreatitis. 4. Chronic pseudocysts and pancreatic cysts. Classification of pancreatitis according to ICD-10: 1. Alcoholic chronic pancreatitis. 2. Other forms: a) infectious b) continuously recurrent c) recurrent. 3.
Stones in the pancreas are often the cause of chronic pancreatitis
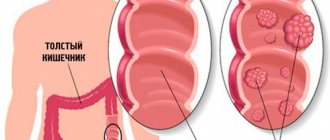
During the disease, the death of organ cells is noted due to a strong inflammatory process. During the development of the disease, defense mechanisms are disrupted. The pancreas begins to digest itself. With this disease, there is a high probability of disruption of the functioning of other organs or systems.
Photo of pancreatic necrosis of the pancreas
The disease code according to ICD-10 is K86.8.1. Pancreatic necrosis develops in three stages:
- At the first stage, bacterial toxins are formed. However, blood tests do not always show the presence of pathogenic microflora.
- In the second stage, an abscess appears. It affects neighboring organs. This stage occurs in the absence of treatment.
- The third stage - purulent processes are formed in the organ itself and in the retroperitoneal tissue. At this stage, there is a high probability of death.
If you do not want to develop pancreatitis in the future, then it is recommended to take preventive measures for those people who have a predisposition to this disease and like to treat themselves to smoked, spicy, fried and fatty foods. Prevention of pancreatitis includes:
- preventing organ inflammation;
- prolongation of the remission period;
- improving quality of life;
- reduction of risk factors;
- normalization of nutrition.
| Prevention measures | |
| You should not abuse alcoholic beverages. | Pancreatitis is a disease of adults and is often diagnosed in alcoholics. Constant consumption of alcohol causes significant damage to the pancreas, since ethyl alcohol destroys the cells of this organ and causes changes in its functioning. This leads to pancreatitis. Strict ban on drinking alcohol |
| Smoking has a negative effect. | The composition of the smoke of cigarettes or cigars is negative, affecting all human organs without exception, and in the combination of tobacco with alcoholic beverages the negative effect increases many times over. Smoke from cigars, penetrating the body, disrupts the functioning of gland cells, affects and provokes inflammation of the gastrointestinal tract, leading to increased stimulation of gastric secretion. If you have been diagnosed with pancreatitis, then it is better to quit smoking forever. |
| Ensuring proper nutrition. | Mostly, pathologies with the pancreas occur if a person likes spicy, fatty, fried and salty foods. These foods overload and deplete the gland. Therefore, one of the preventive measures is to review your diet. It is advisable to supplement the menu with vegetables, cereals, fruits, legumes, and cereals. |
Preventive measures also include:
- prevention of stressful situations;
- periodic walks in the fresh air;
- proper rest and sleep;
- active lifestyle.
If you follow these recommendations, you can improve your immunity, improve your health, and increase your body’s stamina. All this will help you significantly reduce the threat of developing this disease, which kills millions of people every year.
The most common cause of chronic pancreatitis (about 60% of cases). Due to the fact that less than 5-10% of patients suffering from alcoholism develop chronic pancreatitis, it has been assumed that there are associated risk factors. Thus, in 5.8% of patients with chronic alcoholic pancreatitis, the N34S mutation was detected; in patients with alcoholism without the development of chronic pancreatitis, this mutation was observed in only 1% of cases.
Cystic fibrosis (cystic fibrosis).
It is an autosomal recessive disease in which there is a mutation in the CFTR gene, which encodes a protein involved in the transport of chlorine across the cell membrane. Mutations in the CFTR gene can lead to severe chronic pancreatitis and respiratory damage. Cystic fibrosis, as an etiological cause, accounts for a small proportion of cases of chronic pancreatitis.
Hyperlipidemia (usually types 1 and 5).
It can cause the development of chronic pancreatitis, but usually manifests itself as repeated attacks of acute pancreatitis.
Taking medications.
Pancreatic-damaging agents include azathioprine, chlorothiazide derivatives, estrogens, furosemide, and tetracycline. Less commonly, the same effect is observed when using cimetidine, metronidazole, glucocorticoids, brufen, nitrofuran.
Idiopathic chronic pancreatitis (in approximately 30% of cases).
Idiopathic pancreatitis is divided into early and late onset forms. Some cases of "idiopathic" pancreatitis may have genetic mutations.
There is a division of chronic pancreatitis into primary (primary inflammatory process of the unchanged pancreas) and secondary, developing against the background of cholecystitis, gastritis, enteritis and other diseases. Marseille-Roman classification of chronic pancreatitis: 1. Chronic calcific pancreatitis. 2.
Chronic obstructive pancreatitis. 3. Chronic fibrous indurative pancreatitis. 4. Chronic pseudocysts and pancreatic cysts. Classification of pancreatitis according to ICD-10: 1. Alcoholic chronic pancreatitis. 2. Other forms: a) infectious b) continuously recurrent c) recurrent. 3.
Causes of pancreatitis
Chronic pancreatitis is more common in middle-aged and elderly people. Women are more susceptible to the disease. The disease can be primary or secondary in nature, and also develop against the background of diseases associated with the digestive system. The development of chronic pancreatitis can be provoked by:
- cholecystitis;
- enteritis;
- stomach ulcer;
- atherosclerosis of pancreatic vessels;
- viral hepatitis;
- typhoid fever;
- infectious mumps;
- gastritis.
Another article on this topic: What to do if an adult has severe diarrhea?
Acute pancreatitis often becomes chronic.
Pancreatitis can be drug-induced, alcohol-induced, purulent, hemorrhagic.
It is important to find out the cause of the disease so that the doctor prescribes quality treatment.
The following factors can provoke the disease:
- eating disorders;
- abuse of spicy and fatty foods;
- alcohol abuse;
- avitaminosis;
- intoxication of the body;
- fungal diseases;
- metabolic disorders;
- complications after surgery.
Pathogenesis
In alcoholic and hereditary chronic pancreatitis, a precipitation reaction of calcium and proteins inside the pancreatic ducts is observed. Normally, precipitation is prevented by PSP proteins, which are secreted by acinal cells. The level of this type of protein in patients with chronic pancreatitis is noticeably reduced, which contributes to an increase in calcium in pancreatic juice and its microcrystalization. Calcifications form in the lumen of the duct, clogging the ducts, and the pressure in them increases. Fibrosis eventually develops.
Ultrasound diagnosis of chronic pancreatitis
Symptoms and signs of the disease
According to the course of the disease, there are 2 main forms of chronic pancreatitis: in the form of relapses and in the form of constant abdominal pain. The clinical picture of chronic pancreatitis consists of a combination of pain, dyspeptic syndromes with malabsorption, weight loss, and various symptoms of functional insufficiency of the insular apparatus.
The pain is localized in the left hypochondrium or has a girdling nature, occurring or intensifying after eating (within half an hour). The duration of a painful attack is up to 2 hours. The pain may be diffuse or radiate to the back. As chronic pancreatitis progresses, the pain loses its connection with eating and becomes constant.
The development of malabsorption syndrome is associated with a violation of the exocrine function of the pancreas. The processes of cavity hydrolysis are disrupted, which leads to increased bowel movements up to 10 times a day. Later manifestations of malabsorption syndrome are weight loss, steatorrhea, creatorrhea. Often patients with chronic pancreatitis are bothered by pain in the bones, signs of osteoporosis are revealed, which is a consequence of a deficiency of vitamin B12 and fat-soluble microelements, primarily vitamin D.
Dyspepsia in chronic pancreatitis is manifested by belching, flatulence, nausea, and vomiting. In 80% of patients, an exacerbation begins with repeated vomiting, and then only pain occurs. 30% of patients with chronic pancreatitis have a concomitant diagnosis of diabetes mellitus or impaired glucose tolerance.
The development of the pseudotumor form of pancreatic lesions of the pancreas is accompanied by the appearance of the following symptomatic signs:
- the occurrence of pain that has a pronounced course,
- a sharp decrease in body weight over a short period of time,
- determination of uneven enlargement of the pancreas at the time of palpation examination of the abdominal cavity,
- pathological change in the exocrine functionality of the organ,
- dyspeptic system disorders,
- vomiting and nausea,
- paleness of the skin with the acquisition of a jaundiced tint,
- enlargement of the head of the gland.
Classification
By origin, CP can be primary (toxic, alcoholic), secondary, post-traumatic. The first develops as a result of damage to the pancreas, the second - due to pathology of other organs. The cause of post-traumatic is blunt or open injuries to the pancreas.
Classification of chronic pancreatitis according to clinical picture:
- Pseudotumorous.
- Painful.
- Combined.
The first occurs with partial duodenal obstruction, portal hypertension and cholestatic. The second is manifested by constant or recurrent pain. Combined is manifested by several clinical symptoms.
Chronic biliary-dependent pancreatitis occurs in 27% of patients. The provoking factor is cholelithiasis (GSD), which has become increasingly common in recent years. According to various authors, in patients with cholelithiasis, chronic biliary pancreatitis develops in 25-90% of cases. Unlike pancreatitis, another pathology, the etiological factor is not eliminated. Against the background of a developing pathological process in the pancreas, its effect continues.
Chronic parenchymal pancreatitis indicates inflammation of the parenchyma with a predominance of areas of fibrosis and mononuclear cells in the infiltrates. With this form of pathology, there is no damage to calcifications and ducts in the pancreas. There is no pain in the clinical picture; symptoms of endocrine and exocrine insufficiency appear.
Chronic calculous pancreatitis is diagnosed in 11% of cases of the total number of CP. It develops as a result of hypersecretion of glucagon, which stimulates the parathyroid glands. Among other reasons, doctors name a violation of the chemistry of pancreatic secretions due to congestion and inflammation in the pancreatic ducts. This in turn leads to damage to the tubules and ducts due to the formation of protein plugs and stones. With this form of CP, malignant degeneration is observed much more often than with other forms of the disease.
Chronic pancreatitis with exocrine insufficiency correlates with tobacco smoking and alcohol consumption, which contribute to the progression of the disease. The pathology is also associated with the development of diabetes mellitus and the formation of calcifications. Complex treatment includes enzyme therapy, antispasmodics and specially designed dietary nutrition.
According to the severity of the course, CP can be mild, moderate, or severe. Patients experience periods of remission and relapse.
Why do acquired cysts occur?
The most common reasons for the development of “bubbles” are:
- a sharp narrowing or stricture of the ducts that prevents the removal of digestive juices, their blockage, both scars and stones.
Such cysts are called retention cysts, or those that arise as a result of outflow disturbances. The formation mechanism will be passive accumulation of secretion with a gradual increase in the occupied space;
- degeneration and necrosis of the parenchyma. This process most often occurs with major trauma to the pancreas, such as a car accident, and blunt trauma to the abdomen. The second reason is extensive pancreatic necrosis, both hemorrhagic and fatty;
- finally, a proliferative process is possible, in which a tumor forms in the form of a cavity. Most often these are cystadenomas, which have a benign course, and cystadenocarcinomas, which are malignant neoplasms.
The process of formation of a post-acrotic cyst of the pancreas goes through 4 stages. At the first stage of the appearance of a cyst, a cavity is formed in the omental bursa, filled with exudate due to acute pancreatitis. This stage lasts 1.5-2 months. The second stage is the beginning of capsule formation.
The fourth stage is the isolation of the cyst. Only a year later, the processes of destruction of the adhesions between the wall of the pseudocyst and the surrounding tissues begin. This is facilitated by the constant peristaltic movement of organs that are fused with a fixed cyst, and the long-term effect of proteolytic enzymes on scar adhesions. The cyst becomes mobile and is easily separated from the surrounding tissue.
Any cystic formation is an accumulation of fluid that is located in a clearly demarcated cavity. They occur if the organ is formed by parenchyma, that is, tissue that may include glands or secreting cells. They do not exist in bone tissue.
Any cyst consists of at least two parts: the wall and its contents. In some cases, it can be multi-chambered and have a lobular structure. An example is a parasitic cyst in liver echinococcosis.
If they form in the pancreas, they can occur both in the tissues of the gland itself and in the tissues surrounding it, for example, in fiber. This formation occurs with equal frequency in both men and women, and does not depend on age.
Despite the fact that the modern international classification of diseases, tenth revision, or ICD-10, assigns a single designation, or code, to all pancreatic cysts, they are far from equivalent in origin and composition. Doctors distinguish the following types of fluid formations of the pancreas:
- a congenital cyst that occurs as a result of developmental defects.
These can be ectodermal or dermoid space-occupying formations. Fibrocystic formations, congenital benign tumors, or teratomas are also possible. Usually, congenital pathologies are accidental findings during ultrasound, if they are not related to the ductal system of the gland, do not suppurate and do not cause inflammation.
- acquired pancreatic cysts.
It is the acquired variants that are most often secondary, and they arise due to various diseases.
Complication of the disease
Complications of CP are divided into early and systemic. Pancreatitis provokes a violation of the outflow of bile, which can result in obstructive jaundice. Even in the early stages of development, the inflammatory process can cause internal bleeding, infectious complications, abscesses, damage to the biliary tract or phlegmon of the retroperitoneal tissue. These conditions are life-threatening and, in the absence of adequate treatment, pose a threat to life.
Disease progression
CP is a progressive disease. The inflammatory process disrupts the intrasecretory and exocrine functions of the pancreas. The course of the disease has a long-term relapsing nature. In severe cases, a change in the cellular structure of the gland occurs and its functional failure develops.
It is not recommended to self-medicate, because the sooner you visit a specialist, the sooner a serious problem with the pancreas can be identified. Systemic complications:
- encephalopathy;
- functional failure of the lungs, liver and kidneys;
- diabetes;
- malignant formations;
- esophageal bleeding;
- critical loss of body weight;
- death.
Diagnostics
When examining the patient, red spots the size of a millet grain are revealed, dryness and flaking of the skin, glossitis, and stomatitis are noted. Examination of status localis reveals abdominal bloating, pain in the epigastrium or left hypochondrium with possible irradiation. There is pain at the Desjardins point, which is determined on the line from the navel to the armpit at 5-7. The Desjardins point is the projection of the head of the pancreas onto the skin.
To the midline from the Desjardins point, the Shofar zone is determined (projection of the body of the pancreas). The tail of the pancreas projects to the Mayo-Robson point. Ultrasound determines the shape, size, features of the echostructure, contours, condition of the pancreatic ducts, cysts or tumors, and the condition of the intra- and extrahepatic ducts.
A significant advantage is the ability to conduct ultrasound diagnostics over time. CT examination provides even greater accuracy. Small calcifications and pseudocysts can be identified. Endoscopic retrograde cholecystocholangiopancreatoscopy is performed by inserting a cannula into the major duodenal nipple through a fibrogastroscope with retrograde X-ray filling and a series of images.
X-ray examination of the abdominal cavity reveals diffuse calcification. The study of elastase in the blood allows us to determine the severity of the disease. An elastase level of less than 100 indicates severe pathology of the exocrine function of the pancreas. Carrying out a caprogram makes it possible to detect steatorrhea. The presence of more than 10 grams of fat in the stool, when the patient is on a diet containing no more than 100 grams of fat in racina, indicates steatorrhea. For diagnostic purposes, the level of alpha-amylase and its isoenzymes in the blood is examined.
The clinical signs of a pancreatic cyst are determined by the underlying disease against which it arose, the presence of the cyst itself, and the complications that arise. A small cyst may be asymptomatic. In acute and chronic pancreatitis, during the next relapse of the disease, doctors at the Yusupov Hospital identify a slightly painful round formation in the projection area of the pancreas, which may suggest a gland cyst. The most often asymptomatic cysts are congenital cysts, retention cysts and small cystadenomas.
The pain, depending on the size of the cyst and the degree of pressure it exerts on neighboring organs and nerve formations, on the solar plexus and nerve nodes along large vessels, can be paroxysmal, in the form of colic, encircling or dull. With severe pain, the patient sometimes takes a forced knee-elbow position, lies on the right or left side, and stands leaning forward. pain caused by the cyst is assessed by patients as a feeling of heaviness or pressure in the epigastric region, which intensifies after eating.
More severe pains accompany the acute form of the cyst in the initial phase of its formation. They are a consequence of pancreatitis of traumatic or inflammatory origin and the progressive proteolytic breakdown of gland tissue. A tumor-like formation that can be felt in the epigastric region is the most reliable sign of a pancreatic cyst. Sometimes it appears and disappears again. This is due to periodic emptying of the cyst cavity into the pancreatic duct.
More rare signs of a pancreatic cyst are the following symptoms:
- Nausea;
- Belching;
- Diarrhea;
- Temperature increase;
- Weight loss;
- Weakness;
- Jaundice;
- Itchy skin;
- Ascites (accumulation of fluid in the abdomen).
Pancreatic cysts are well contoured during angiography of the branches of the celiac artery. Doctors at the Yusupov Hospital obtain valuable data for making a diagnosis with retropneumoperitoneum and pneumoperitoneum in combination with urography. Determining the level of pancreatic enzymes (amylase and lipase) in the blood and urine is of some importance for establishing an accurate diagnosis. Violations of the secretory function of the pancreas are very rare with cysts.
Why is a cyst located in the pancreas dangerous? Pancreatic cysts often lead to complications, which are manifested mainly by compression of various organs: the stomach, duodenum and other parts of the intestine, kidneys and ureter, portal vein, bile ducts. Rupture of a pancreatic cyst causes inflammation of the peritoneum (peritonitis).
The pain is localized in the left hypochondrium or has a girdling nature, occurring or intensifying after eating (within half an hour). The duration of a painful attack is up to 2 hours. The pain may be diffuse or radiate to the back. As chronic pancreatitis progresses, the pain loses its connection with eating and becomes constant.
Symptoms
Signs and manifestations are different for different forms of inflammation. In the acute form, patients complain of severe abdominal pain on the left, bloating, nausea and vomiting mixed with bile, and dehydration. Bluish-yellowish spots may appear on the left side or at the navel from burst small vessels and capillaries. The most dangerous complication of acute pancreatitis is intoxication of the body, which can cause cerebral edema, kidney failure and death of the patient.
Chronic disease reduces the ability of the pancreas to produce enzymes and hormones. As a result, the process of digesting food is disrupted. Sometimes in the pancreas, after acute inflammation, pseudocysts form in which fluid or pus accumulates. Over time, chronic inflammatory processes develop and these formations grow and are compressed by other organs, resulting in pain, heaviness after eating, nausea and a bitter taste in the mouth. Another symptom is obstructive jaundice, caused by narrowing and poor patency of the biliary tract.
Pathology has such symptoms not only with alcohol etiology, but also with other types of chronic disease, which are provided for by the tenth classifier of diseases. Digestive disorders, diarrhea, and intolerance to certain foods are also added to them.
Diagnosis of pseudotumor pancreatitis
The disease described cannot be determined solely by external signs. Pseudotumorous pancreatitis exhibits symptoms similar to a number of other diseases, pathologies of the liver and gallbladder. The described signs indicate both pseudotumorous pancreatitis and the possibility of oncology. Making an accurate diagnosis is only possible during a hospital stay and a group of medical tests.
At the appointment, the gastroenterologist asks questions to collect anamnesis, conducts a visual examination, and palpates the pancreas area. During the examination, an enlargement of the head of the organ is detected, the patient experiences pain upon palpation. Standard diagnostic methods are used (all or selected, at the discretion of the attending physician):
- blood tests;
- Analysis of urine;
- stool examination;
- ultrasound diagnostics of the abdominal organs;
- X-ray;
- MRI;
- CT;
- endoscopy of the pancreatic duct;
- gastroduodenoscopy;
- histology analysis.
Cancer is confirmed only by histological examination (puncture), other tests in the agreed plan are not indicative. To obtain the result, the doctor uses a special needle to pinch off a piece of the pancreas, which is examined in the laboratory for cancer cells. Sometimes such a study is carried out during the operation to confirm the diagnosis and determine the doctor’s further actions.
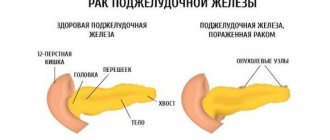
How quickly does cancer develop?
Pancreatic cancer has an extremely poor prognosis . If radical surgery is performed at the initial stage, the five-year survival rate is 50% of sick people, especially with cancer of the head of the pancreas.
At stage 2, the chances of cure are 30%. The rest cannot avoid relapse. Patients with the third stage can live for several years only in 5-9% of cases. With inoperable stage 4, the patient’s life is 6-8 months with the condition of palliative therapy, i.e. treatment that is aimed at alleviating the suffering of hopelessly ill patients.
From the case histories of cancer patients, it follows that without surgery and subsequent chemotherapy, no more than a year passes from the onset of the disease to death. Radiation and chemotherapy extend the period by 12-14 months .
For the well-known Steve Jobs, the fight against pancreatic cancer took 8 years (see photo).
Pancreatic tumors pose a serious threat to human health. Even if the formation is benign, it can cause diabetes, pancreatitis and other pathologies of the digestive system. In addition, there is a high risk of degeneration into cancer .
Malignant tumors are the worst in terms of prognosis, as they have an asymptomatic course. Cancer can be prevented by regularly undergoing preventive examinations and leading a healthy lifestyle.
Basic medical services according to treatment standards Select treatment using artificial intelligence
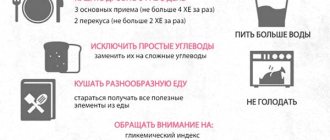
During the period of remission of chronic pancreatitis, diet and replacement therapy are indicated. Exacerbation of chronic pancreatitis requires the prescription of complex pathogenetic and symptomatic treatment, including parenteral nutrition, infusion therapy, antispasmodics, analgesics and antisecretory drugs.
In the first 2-3 days, complete fasting is prescribed. Then, with a mild pain syndrome, they switch to food according to table No. 5 with a decrease in fat, fried foods, smoked foods, alcohol, and carbonated water. You should eat 5-6 times a day. In order to reduce gastric secretion, it is enough to take ranitidine or famoditin at a dose of 40-60 mg/day.
The administration of somatostatin produces such effects as a decrease in the level of gastrin, HCl, inhibition of the exocrine and endocrine functions of the pancreas, a decrease in the volume of visceral blood flow, pressure in the portal system, without causing fluctuations in blood pressure in the systemic circulation. Plasma, rheopolyglucin, and 5% glucose solution are used as infusion therapy.
| Consultation with a surgeon any doctor – 607 clinic doctor Ph.D. – 207 clinics, doctor of medical sciences, professor – 115 clinics of the Russian Academy of Sciences – 2 clinics |
Surgery | |
| Endoscopic stenting of the common bile duct | |
| Thymectomy any sternotomy – 8 clinics Thoracoscopy – 5 clinics | |
| Sphincterotomy |
| Any resection of the small intestineSegmental resection of the small intestine – 82 clinicsDiverticulectomy of the small intestine – 36 clinicsLaparoscopic resection of the small intestine – 20 clinics |
| Resection of the sigmoid colon, any Sigmoidectomy – 58 clinics Hartmann operation – 31 clinics Proctosigmoidectomy – 13 clinics |
| Any colon resection Total colectomy – 56 clinics Left-sided hemicolectomy – 83 clinics Right-sided hemicolectomy – 90 clinics Transverse colon resection – 72 clinics Coloproctectomy – 11 clinics |
| Operations for cholelithiasis any Choledocholithotomy – 23 clinicsCholecystectomy from a mini-access – 29 clinicsOpen cholecystectomy – 116 clinicsLaparoscopic cholecystectomy – 146 clinicsCholecystotomy – 17 clinicsSILS-cholecystectomy – 16 clinics |
| Any surgery on the adrenal glands Laparoscopic removal of the adrenal gland – 59 clinics Removal of the adrenal gland (adrenalectomy) – 60 clinics Bilateral removal of the adrenal glands – 7 clinics |
Doctor consultations | |
| Consultation with an endocrinologist any doctor – 860 clinic doctor candidate of medical sciences – 281 clinics, medical sciences, professor – 165 clinics of the Russian Academy of Sciences – 2 clinics | |
Diet for chronic pancreatitis
It involves taking easy-to-digest foods that do not cause increased stomach acidity. Fatty foods and alcohol, which lead to the destruction of pancreatic cells, are prohibited. Sweets, jam, and sugar are excluded from the diet.
- Egg whites.
- Lean meats without skin.
- Beans, lentils.
- Low-fat dairy products.
- Tuna.
- Plant milk (rice, almond).
- Soy.
- Vegetable and fruit juices.
- Vegetables and fruits.
- Wholemeal bread.
- Light soups.
- Tea, honey
- Cyst of the head of the pancreas: symptoms and treatment
- Pancreatic tail cyst
- False pancreatic cyst
- True pancreatic cyst
| Codes without services: |
| Sphincterotomy |
| Codes without services: |
Treatment
Therapy for pancreatic abscess depends on many factors, in particular, the degree of progression of the disease and the development of possible consequences.
The following methods are mainly used:
- Surgical removal and drainage of the purulent capsule.
- Taking antibacterial agents.
- Restorative agents: digestive enzymes and restorative drugs.
During the period of treatment and rehabilitation, the patient must follow a diet. It eliminates increased stress on the digestive tract and possible difficulties in absorbing nutrients. The duration of therapy is determined individually and largely depends on the conscientiousness of the patient and the techniques used.