The essence of pathology
In childhood, pancreatitis most often manifests itself in a reactive form. Its difference from other pancreatic pathologies is that it is not an independent disease, but represents the body’s reaction to any infectious process or problems in the digestive system. Reactive pancreatitis in a child can be provoked even by such common infections as acute respiratory infections and acute respiratory viral infections, as well as poor diet and food poisoning. Moreover, it is poor-quality nutrition that most often causes this reaction in children due to the incomplete formation of digestive functions.
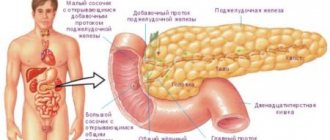
Like any pancreatitis, its reactive type is associated with inflammation in the pancreas. It becomes a consequence of premature activation of pancreatic juice, which is intended to be needed during the digestion process, but, lingering for a long time in the gland, begins to destroy parenchyma tissue, which becomes the cause of inflammation.
When reactive pancreatitis develops, symptoms and treatment in adults and children correspond to the acute form of the disease. The process develops rapidly, as befits an acute attack. Lack of treatment leads to the following: the reactive stage turns into chronic pancreatitis with alternating periods of exacerbation and remission.
Causes of pancreatitis in children
Several factors can cause the development of reactive pancreatitis in childhood. The most important of them is poor nutrition, in which the basic rules of eating are grossly violated. It happens that a child does not follow a daily routine and remains hungry for a long time, and then eats a large amount of food.
Or his diet includes a large number of products that should not be on the menu because they cannot be absorbed by the child’s body. On the contrary, insufficient attention is paid to necessary dishes. Particularly dangerous for the pancreas are:
- chips, crackers and instant foods with preservatives, dyes and flavor enhancers;
- store-bought juices;
- fast food;
- carbonated drinks;
- fried foods;
- smoked meats and so on.
The products listed above are most dangerous at school age, when the child already buys them himself. But even in infancy there is a risk of pancreatitis due to poor nutrition. This is due to the introduction of new foods into the diet that are not appropriate for the baby’s age, and leads to excessive stress on the pancreas, which it is not able to cope with.
As a result, it becomes inflamed, and since the organ is not yet sufficiently developed, any disturbances in its functioning can be catastrophic. If the patient is still a child, then pancreatitis is a deadly disease.
Therefore, the sooner the problem is detected, the better.
In addition, the following causes of reactive pancreatitis are identified:
- taking certain medications that affect an organ such as the pancreas (drug-induced pancreatitis);
- disturbances in the development of organs included in the digestive system, among which the most dangerous are deviations in the structure of the duodenal ducts;
- abdominal injuries;
- infections;
- regular stress and emotional overload;
- transmission of parasitic diseases;
- food allergies;
- inflammatory processes in organs close to the pancreas.
Etiological features
The mechanism of occurrence of the pathology can be based on 2 main circumstances: blocking of the ducts through which pancreatic juice produced in the pancreas enters the duodenum (blockage, spasms, etc.) and the reflux of food ingredients from the stomach into the gland, which causes juice activation.
The following main factors contributing to the development of the disease in a child are identified:
- Unbalanced diet. In babies, spasms of the ducts can be caused by excessively early and inappropriate complementary feeding. Children aged 5-7 years often suffer from excessive consumption of chips, nuts, crackers, sweets, and carbonated drinks.
- Worm infestation. Various types of worms and roundworms are capable of blocking the lumen of the canals.
- Gastrointestinal diseases of a congenital or acquired nature (gastritis, duodenitis, cholecystitis, etc.).
- Allergic reactions to certain foods.
- Untreated acute viral infections, including ARVI.
- Pathologies of a systemic nature – lupus erythematosus, cystic fibrosis.
- Thyroid diseases. The most common diagnosis is hypothyroidism.
- Congenital anomalies in the pancreas and its ducts.
- Traumatic impact. A strong blow to the abdominal area can trigger an inflammatory reaction.
- Stress and psychological overload.
- Medicines – antimicrobials (furosemide), antibiotics, corticosteroids, cytostatics (Nimustine, Cisplatin, etc.).
The child’s body has increased sensitivity, and therefore these factors provoke a sharp reaction of the body, including the pancreas.
Reference! Typically, the reactive form is caused by the consumption of aggressive foods and poor diet.
In particular, overeating in children threatens the emergence of this problem. The reaction appears almost immediately after eating low-quality food.
Forms of pathology in children, their causes and symptoms
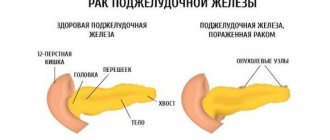
Diseases of the pancreas in children are classified according to severity, causes, and clinical picture of the disease. Any disorders of the pancreas are interconnected with the functioning of other organs and systems, so it is important to timely and accurately determine the type of pancreatitis so that treatment brings the most effective results.
Spicy
Acute pancreatitis occurs in children usually after ten years of age. It manifests itself as a sharp deterioration in well-being. Depending on the extent of damage to the pancreas, pancreatitis can be mild or severe. The disease is too serious to be ignored. If left untreated, complications may occur. It is necessary to immediately seek qualified medical help as soon as the first symptoms appear.
The acute form of the disease indicates significant errors in the child’s nutrition. The pancreas in children is much more delicate than in adults. Therefore, if a child, especially during the holidays, has eaten a lot of fatty, spicy foods, it is not surprising that his pancreas hurts.
Inflammation can also occur for other reasons: due to drug poisoning, an allergic reaction to drugs or products, or as a result of injury to the pancreas.
The main signs of acute pancreatitis:
- severe pain in the left side, which can radiate to the back;
- nausea, vomiting;
- temperature can rise to 37.5°C;
- bloating;
- dry mouth;
- bowel dysfunction;
- dizziness;
- cardiopalmus.
The child curls up in a ball on the bed in pain. You need to urgently call an ambulance.
Chronic
Chronic pancreatitis in children is rarely diagnosed. The cause of low-grade inflammation of the pancreas in children is most often, again, food. With regular poisoning by harmful foods, healthy organ tissue becomes inflamed and dies. It is replaced by connective tissue, after which problems with the pancreas appear, since it cannot fully perform its functions.
In children, the symptoms of chronic pancreatitis are mild. The child may get tired quickly, the temperature stays up to 37°C, and the tummy hurts after eating. Of course, such symptoms are not enough to establish a diagnosis, so additional examination and tests are needed.
Exacerbation of chronic pancreatitis has the same symptoms as acute pancreatitis and requires immediate hospitalization.
Reactive
The reactive form of the disease, as the name suggests, is a reaction or response of the pancreas to another disease. The provoking causes of pancreatitis in children are viral or bacterial infections, helminthic infestations. Individual intolerance to certain medications, including antibiotics, can also lead to inflammation and failure of the pancreas.
Reactive pancreatitis is accompanied by nausea, fever, and pain in the stomach area. Therapy is carried out with an emphasis on the underlying disease. At the same time, Pancreatin, which is prescribed to improve digestion, is contraindicated during an exacerbation.
Symptomatic features
The difficulty of identifying reactive pancreatitis in children is associated with the similarity of the signs of this pathology with other gastrointestinal diseases. It should be noted: the younger the baby, the less pronounced the specific symptoms (nausea, vomiting). Babies react to painful sensations by crying, refusing to eat, and restless behavior. Children aged 2-3 years become excessively whiny, nervous, and unsociable.
With age, the manifestations of the disease become more pronounced. The following symptoms are noted:
- Pain syndrome. It is felt as a sharp, piercing pain in the upper abdomen (slightly above the navel). In some cases, the syndrome does not have a clear localization, and the pain is distributed throughout the abdomen and sometimes radiates to the back. The pain subsides somewhat in a sitting position with the body moving forward.
- Nausea and vomiting. In older children, vomiting is profuse.
- Low-grade fever. Most often it rises no higher than 37.5 degrees.
- Diarrhea and increased frequency of bowel movements.
- Dryness in the mouth, and the drink improves the situation for a short time. The tongue becomes covered with a whitish coating.
- The appearance of yellowness on the skin.
Symptoms and treatment of reactive pancreatitis in children are under the jurisdiction of a pediatrician, who will definitely involve a gastroenterologist. If any symptomatic manifestations of the disease are detected, it is necessary to contact him as quickly as possible. Delay threatens serious complications.
The most characteristic continuation of the disease is transition to a chronic form. With this development of pathology, the child is doomed to constant dietary nutrition. A more serious complication is exocrine pancreatic insufficiency, leading to a deficiency of digestive enzymes. With age, pathologies such as diabetes mellitus, and then kidney and cardiovascular diseases can also be provoked.
Manifestations of reactive pancreatitis
Symptoms of reactive changes in the gland in children are not very specific.
1. Pain . It is localized in the upper abdomen. May have a shingling character.
2. Poor appetite . The child may refuse to eat at all.
3. Dyspeptic symptoms . Nausea, vomiting. And it doesn’t bring relief. Diarrhea for no apparent reason.
4. Children are whiny and irritable.
Often parents see the source of such symptoms in poisoning with some foods. Therefore, a visit to the doctor and full treatment is postponed. Which only worsens the child’s condition.
Chronic pancreatitis not only does not manifest itself clearly in a child, its symptoms are not specific at all. Therefore, it can progress for a long time, but remain undiagnosed. Only one day, suddenly, with a confluence of provoking factors, does it manifest itself in the form of acute reactive pancreatitis.
Diagnosis of pathology
The disease is diagnosed through laboratory and instrumental studies. First of all, anamnesis is analyzed to determine the prehistory of the disease. Then, a general blood test is performed to determine inflammatory mediators (leukocytosis, lymphopenia, increased ESR and decreased hemoglobin). A biochemical blood test helps to identify excess levels of specific enzymes - lipase, amylase, trypsin. Feces are tested for undigested food ingredients (especially protein fibers and starch) and for increased fat content.
Among the instrumental diagnostic techniques, ultrasound of the abdominal organs stands out first. Based on the results of the studies, it is possible to determine the foci of damage to the pancreatic tissue, as well as the degree of replacement of glandular tissues with connective tissues. Contrast radiography can detect changes in the ducts and gastrointestinal tract. If necessary, fibroesophagogastroduodenoscopy is performed using anesthesia.
Principles of treatment
Taking into account the fact that the pathology in question is only a reaction to certain processes in the body, treatment of reactive pancreatitis should be aimed, first of all, at eliminating the root causes that provoke the disease. Next, it is necessary to stop the inflammatory reaction and further destruction of glandular tissue, normalize the secretory functions of the organ and stabilize the functioning of the digestive system. An important place is given to symptomatic therapy, which allows eliminating all manifestations of the disease.
Acute pancreatitis, which includes its reactive form, requires mandatory hospitalization of the child for a period of 6 to 25 days, depending on the severity of the disease and the effectiveness of treatment. The baby should be under constant medical supervision to avoid complications. In the first days of an attack, a starvation diet is provided, up to complete fasting. Then a gradual transition to dietary nutrition is made with the exclusion of harmful foods.
Drug therapy
Conservative treatment of reactive pancreatitis in children is based on complex drug therapy. Medicines are prescribed by a doctor, taking into account age restrictions and the characteristics of the course of the disease. Self-medication is prohibited.
The treatment regimen includes taking the following groups of drugs:
- Pancreatic inhibitors or drugs that normalize the functioning of the pancreas and reduce the secretion of gastric juice; taking them gives time for the restoration of the affected tissues. The child can be prescribed Pirenzelin, Somatostatin, Contrical, Trasylol.
- Enzyme replacement therapy drugs. They contain enzymes that are lacking in a sick body, but which are urgently needed for normal digestion. There are such effective remedies as Festal, Mezim, Pancreatin.
- Antispasmodics. They are necessary to eliminate spasms in the ducts, that is, to ensure normal outflow of pancreatic juice from the gland. In addition, antispasmodics have an analgesic effect. The most commonly used are No-Shpa, Duspatalin, Platyfillin, Spazgon.
- Detoxification. General intoxication of the child's body is reduced by administering a glucose solution.
- Antihistamines in the presence of allergic reactions.
- Multivitamin complexes for general strengthening of the body.
If an acute attack is severe, then drugs are used that inhibit the premature activation of pancreatic juice. They are also used to prevent chronicity of the process. In this regard, proteolysis inhibitors are quite effective - Pantripin, Ingitril, Gordox.
Diet therapy
Most often, poor nutrition plays a decisive role in the development of this disease in children. That is why diet for reactive pancreatitis is the most important element of complex treatment.
Important! When an acute attack occurs, the child’s nutrition is provided in a special manner.
Fasting should be ensured for 20-40 hours under the supervision of a doctor and with bed rest. You can give children alkaline mineral water (for example, Borjomi). Volume - 5 ml per 1 kg of body weight. Water is given 5-6 times a day, warm, without gas.
Exit from the fasting process is carried out gradually over 10-12 days. Only 2 weeks after the attack, nutrition is established in accordance with diet No. 5p. Immediately after a complete fast, you can drink weak tea with crackers, as well as eat pureed porridge (buckwheat and oatmeal). On days 4-5, jelly, fermented milk products, vegetable purees, and day-old white bread are added to the diet. Only after 9-11 days can you offer boiled meat and fish, as well as steamed cutlets. Fresh vegetables and fruits can be consumed only after 13-14 days.
Diet
The diet and menu for the reactive type of disease must be monitored and prepared by a specialist, taking into account the individual characteristics of the child’s body and the presence of allergic reactions to certain products. In general, when drawing up a nutrition plan, the following principles are used:
- Children are fed frequently, but in small, fractional portions. It is recommended to provide food intake every 3 hours.
- Products must be pureed. The main cooking methods are boiling, steaming, stewing. The food temperature should be optimal.
- The protein content of food increases. For this, boiled meat and low-fat fish, and cottage cheese are recommended. The consumption of carbohydrates is reduced, including those contained in sugar and confectionery products. Fat consumption is sharply limited.
When creating a dietary menu, you should consider the following recommendations:
- The following products are subject to mandatory prohibition: rich broths (meat, cabbage, mushroom, vegetable with a juice effect), fried, pickled, salted, smoked, sweet, baked goods, preservatives of any type, sausages, spices and hot seasonings, lard and fatty meat, fatty fish. During an attack, you should not eat fresh fruits and vegetables.
- Recommended products: wholemeal bakery products and crackers; various soups with cereals and vegetables, cooked on the basis of chicken breast; dishes made from ground or pureed lean meat (cutlets, meatballs, rolls, etc.); fish prepared by boiling or steaming; steam omelettes; milk and fermented milk products (kefir, yogurt, cottage cheese, low-fat cheese); butter and vegetable (olive, sunflower) oil; vegetable purees; porridge and pasta; unsweetened fruits; jelly; jelly and compotes; tea, rosehip decoction.
Dietary food must be complete in energy value. The menu should contain a variety of dishes and appeal to the child. Fat consumption cannot be completely eliminated; it should only be significantly limited.
Treatment with folk remedies
The following folk remedies provide certain positive results in the treatment of pancreatitis:
- Blueberry. An infusion is prepared from its leaves. To do this, the crushed raw material (1 tablespoon) is poured with boiling water (250 ml) and left until it cools completely. Drink 500 ml of infusion during the day.
- Licorice. The root of the plant is ground to a powder state. Next, it is mixed with burdock and dandelion leaves (all 1 tablespoon each). The mixture is infused in boiling water (300 ml) until it cools completely. Use 20-25 ml 4-5 times a day.
- Calendula. The infusion is prepared from the flowers of the plant - 1 teaspoon per 200 ml of boiling water. This portion is drunk throughout the day, in 3 doses.
Alternative medicine cannot cure the disease, but folk remedies help increase the effectiveness of drug therapy. It is also important to understand the fact that even the use of medicinal plants must be agreed with a doctor.
The reactive type in childhood is the main form of manifestation of pancreatitis, which is justified by the imperfection of the digestive system. The main reason for its appearance is poor nutrition, and therefore the main preventive measure is the exclusion of indigestible, fatty and fried foods from the children's diet. The acute manifestation of this disease can become chronic in the absence of adequate treatment.
Diagnosis and treatment
Diagnosis and treatment of reactive pancreatitis in children is carried out by a gastroenterologist. After interviewing the patient and parents in order to collect the necessary information (nutrition, previous diseases, taking medications, severity of symptoms, time and order of appearance), the young patient is examined. Pale skin and mucous membranes, white coating on the tongue, tachycardia, low blood pressure, pain on palpation of the upper abdomen confirm the diagnosis of “reactive pancreatitis”.
After the examination, laboratory tests are prescribed:
- general blood and urine analysis;
- blood chemistry;
- stool analysis;
- Ultrasound of the abdominal organs.
Do not forget that reactive pancreatitis in children is a secondary disease; the first priority is to find the cause and eliminate the provoking factors. Children with a diagnosis are hospitalized for comprehensive monitoring of the course of the disease and tracking changes in the patient’s well-being.
The main tool for treating pancreatitis remains the diet prescribed by the attending physician depending on the stage and severity of the disease. For the first two to three days, it is recommended to avoid eating altogether. Then the damaged organ is provided with rest and stress relief. For this, enzymatic preparations are prescribed to facilitate the absorption of proteins and carbohydrates. It is important to know that prolonged use of this type of medication leads to a decrease in the production of pancreatic juice, and the pancreas ceases to function!
Antispasmodics and analgesics are used to relieve pain. The main sign of recovery is a weakening or complete absence of pain.
Principles of proper nutrition
- The main risk factor is poor nutrition – an abundance of fatty, salty and spicy foods (fast food) in the diet.
- The use of carbonated drinks has a negative impact on the functioning of the digestive system, which, in addition to increasing the acidity of the stomach, has a mechanical effect on the walls of the duodenum and provokes the reflux of contents into the pancreatic ducts. As a result of such actions, the activation of enzymes will occur before reaching their destination and will start the process of digesting the tissues of a healthy organ.
- It's also worth paying attention to portion sizes. Overeating is unacceptable. To avoid digestive problems, you should not force your child to eat if he refuses.
- Frequent snacking is a malicious enemy of the normal functioning of the digestive system.
- Food dyes, preservatives and flavor enhancers should be excluded from the child’s diet if possible.