Chronic pancreatitis is a fairly common disease, which is manifested by constant or periodic pain and signs of exocrine and endocrine insufficiency.
It is characterized by irreversible pathological changes in the pancreatic parenchyma - its wrinkling, sometimes the disappearance of acini, proliferative fibrosis, as well as stricture of the duct, the formation of stones in it or in the gland tissue.
It can occur with minimal clinical manifestations or under the guise of other diseases of the abdominal organs (chronic cholecystitis, biliary dyskinesia, peptic ulcer of the stomach and duodenum, hiatal hernia).
As a result, it is not possible to establish the true frequency of this disease.
Etiology
A common cause is alcohol abuse and the presence of gallstones or other gallbladder pathologies.
Other provoking factors that can cause inflammation of the pancreas include:
- parenchymal pancreatitis with a chronic course, observed in metabolic disorders;
- hormonal imbalance;
- vascular pathologies;
- injuries or other injuries in the abdominal area;
- diseases of the digestive system (for example, duodenitis or peptic ulcer);
- taking pharmacological agents (Furosemide, antibiotics, hormonal or sulfonamide drugs);
- surgical treatment in which surgery was performed on the stomach or biliary tract;
- infectious diseases (for example, mumps);
- viral hepatitis;
- ascariasis and other helminthic infestations;
- anatomical abnormalities.
It is worth noting that in some cases, hereditary predisposition plays a role. Sometimes the cause of chronic pancreatitis cannot be determined. At the same time, it is more difficult to determine how and with what to treat patients.
Disease prevention
Using preventive measures makes it possible to stay healthy. In order to avoid exacerbation of pancreatitis, you need to follow these rules:
- moderate physical activity;
- avoid visiting saunas and steam baths;
- stop drinking alcohol and cigarettes;
- timely treatment of gallbladder pathologies;
- eat right – choose a balanced diet;
- eat food in moderation;
- give up drinks such as coffee;
- do not include canned and smoked foods in the diet;
- follow the daily routine.
Compliance with these rules will help to avoid exacerbations of pancreatitis in the future and improve your well-being.
Forms of the disease
According to severity, chronic pancreatitis can be divided into 3 forms:
- Mild severity: exacerbation occurs infrequently (up to 2 times per year), short-lived, pain is insignificant, it is easy to stop, weight does not decrease, exocrine pancreatic function is not impaired, there are no pronounced signs of illness.
- Moderate severity: the attack occurs several times throughout the year, lasts for a long time with severe painful sensations, stool analysis shows a high content of fat, muscle fibers, protein, weight can decrease, exocrine pancreatic function tends to decrease.
- Severe: regular and prolonged attacks (more than 5 times during the year) with intense unpleasant sensations and pronounced symptoms. Weight drops significantly to the point of emaciation, a sign of which is diarrhea. Sometimes there may be additional adverse consequences - diabetes mellitus, duodenal stenosis, which occurs due to an increase in the size of the head of the pancreas.
Treatment of pancreatitis with herbs: recipes
Treatment of pancreatitis with herbs can be used as an additional or auxiliary remedy to the main treatment prescribed by a doctor. Treatment of pancreatitis with herbs is possible, but the herbs must have the following properties:
- antispasmodic,
- choleretic,
- increasing appetite,
- increasing the overall resistance of the body.
If the use of herbal preparations lasts more than two months, then they should be alternated, that is, changed every two months.
The most common recipes that give a good effect in the treatment of pancreatitis with herbs:
- a collection of yarrow, chamomile and calendula - herbs are mixed in 1 tbsp. and pour a large mug of boiling water over it. Leave for 30 minutes. Take 100 ml of decoction 30-40 minutes before meals, at least 4 times a day.
- 1 tbsp. pour boiling water (about 200 ml) of crushed barberry bark and let it brew for about 20-30 minutes. Cool. Should be taken 1 tbsp. every time before meals. Treatment of chronic pancreatitis will be especially effective with this decoction.
- Immortelle - 3 tbsp, wormwood - 1 tbsp, chamomile flowers - 2 tbsp. Pour 300 ml of boiling water over the herbal collection. Cool and consume 100 ml 6 times a day.
Classification
Chronic pancreatitis is classified
- by origin: primary (alcoholic, toxic, etc.) and secondary (biliary, etc.);
- according to clinical manifestations: pain (recurrent and constant), pseudotumorous (cholestatic, with portal hypertension, with partial duodenal obstruction), latent (clinical unexpressed) and combined (several clinical symptoms are expressed);
- according to the morphological picture (calcifying, obstructive, inflammatory (infiltrative-fibrous), indurative (fibro-sclerotic);
- according to the functional picture (hyperenzyme, hypoenzyme), according to the nature of functional disorders they can distinguish hypersecretory, hyposecretory, obstructive, ductular (secretory insufficiency is also divided according to the degree of severity into mild, moderate and severe), hyperinsulinism, hypoinsulinism (pancreatic diabetes mellitus);
Chronic pancreatitis is distinguished by the severity of the course and structural disorders (severe, moderate and mild). During the course of the disease, there are stages of exacerbation, remission and unstable remission.
Symptoms
In the initial stages of the disease, pathological processes proceed sluggishly, often without manifestations. The first clinically significant relapse of chronic pancreatitis occurs when degeneration and regressive processes in the pancreas are significant. Symptoms of chronic pancreatitis include not only severe inflammation, but also manifestations of intoxication due to the entry of enzymes into the general bloodstream.
Typical signs of chronic pancreatitis:
- intense pain (pain attacks) are cutting or dull in nature, lasting regularly or in the form of attacks; sometimes the pain can put the patient into shock; pain during chronic pancreatitis is localized depending on the affected part of the gland - if the pain is diffuse throughout the peritoneum and lower back, the entire organ is completely affected; if the tail or head is affected, irradiation is noted in the cardiac region, epigastrium or right side;
- a rise in temperature and surges in blood pressure are directly related to intoxication processes; a rise in temperature to 38–39 °C indicates intense damage with possible bacterial complications or the formation of abscesses; pressure changes occur in a short time interval and worsen the general condition;
- change in the patient’s appearance - the face takes on a suffering look, the eyes become sunken, facial features become sharpened; skin color changes to pale gray with an earthy tint; small red spots (“red drops”) may appear in the chest and abdomen area;
- development of obstructive jaundice (due to blockage of the bile duct) with yellowing of the skin and eye sclera;
- painful vomiting, and after an episode of vomiting there is no relief; vomit consists of undigested food mixed with bile;
- attacks of nausea and hiccups in combination with belching of air; in addition, dry mouth may appear;
- stool disorder can manifest itself in the form of constipation or diarrhea: repeated loose stools in the form of a foamy, foul-smelling mass with an abundance of mucus are typical for a relapse of the disease; constipation with flatulence and bloating are characteristic of the initial stages of chronic disease;
- lack of appetite and weight loss due to the inability to fully absorb nutrients.
Chronic pancreatitis in adults can occur with a clear dominance of one or more symptoms. For some, the course of the disease is completely asymptomatic - the person does not suspect the presence of inflammation for several years. In other categories of people, the chronic form of pancreatitis is manifested only by dyspepsia with frequent diarrhea and emaciation. Pain-type inflammation is associated with frequent attacks of severe pain after errors in diet and alcohol intake. Rarely, the symptoms have a picture of pseudotumor inflammation with signs of cancer and simultaneous yellowing of the skin and eye sclera.
Complications
If you do not carry out competent and complete treatment of chronic pancreatitis in a timely manner, then the following complications will begin to actively progress against its background:
- pancreatic ascites;
- diabetes mellitus of pancreatogenic type;
- abscess;
- formation of phlegmon in the retroperitoneal space;
- inflammatory process in the excretory ducts;
- chronic duodenal obstruction;
- B12 deficiency anemia;
- portal hypertension;
- gastrointestinal bleeding may occur due to rupture of the pseudocyst;
- formation of malignant tumors.
More about pancreatitis
Pancreatitis is an inflammation that modifies the pancreas and is accompanied by pain. Pathology can be divided into several stages, each of which should have an individual approach to treatment.
How to treat pancreatitis at home? Curing the disease at home is possible only after examination and an accurate diagnosis. The acute form of pancreatitis requires drug therapy to promptly stop the course of the disease and prevent it from becoming chronic.
The chronic form is first treated with medication, then you must stick to a diet and get rid of bad habits.
There are many home remedies that you can use to combat pancreatitis, but you should always consult your doctor before using them.
Diagnostics
Chronic pancreatitis can be successfully masked behind other pathologies over a long period of time. Symptoms indicating an exacerbation of chronic pancreatitis are quite similar to the symptoms of gastric ulcers, cholelithiasis, and others. Therefore, it is important to conduct a thorough diagnosis.
Standard diagnostic plan:
- inspection. What immediately catches your eye is that the patient is very thin. Severe pain forces the victim to take the fetal position on the bed. In the case of progression of the pseudotumor form, changes in the color of the skin are observed - it becomes icteric;
- palpation;
- clinical blood test;
- blood biochemistry;
- analysis to determine the activity of enzymes produced by the pancreas;
- coprogram (excess undigested fats can be detected in excrement);
- Ultrasound;
- CT;
- MRI.
How to treat chronic pancreatitis?
When describing a plan for upcoming treatment to a patient, the doctor sets very specific goals. Necessary:
- eliminate pain;
- provide rest to the pancreas;
- reduce its secretory activity;
- compensate for the deficiency of pancreatic enzymes;
- correct impaired carbohydrate metabolism (if necessary).
To achieve these goals, different techniques should be used in the non-surgical treatment of patients with all types of chronic pancreatitis. The complex effect of various therapeutic factors (diet therapy, medications, physiotherapeutic procedures, etc.) is more effective.
Drugs prescribed for treatment
Groups of drugs used in the treatment of chronic pancreatitis:
- Antispasmodics and analgesics (Nosh pa, Aspirin) are used for severe pain. Nosh pa 1 tablet 3 times a day.
- Anti-inflammatory drugs (Diclofenac) reduce pain by reducing inflammation in the pancreas.
- Replacement therapy is carried out with drugs containing pancreatic enzymes (Mezim, Creon, Pancreatin), in order to correct digestive processes (facilitate digestion), eliminate pain and bloating. These medications should be taken with meals. Take 1 tablet with meals.
- Antacid drugs (Phosphalugel, Almagel, Grastal) are prescribed to protect the duodenal mucosa from the acidic contents that are formed as a result of a lack of bicarbonates secreted by the pancreas. Almagel 1 tablespoon 3 times a day, 30 minutes before meals.
- Antisecretory drugs (Famotidine, Omeprazole) are prescribed to neutralize the acid. Omeprazole 1 tablet (20 mg) 2 times a day.
- Reducing the active secretion of the gland, drugs (Octreotide, Sandostatin) are used for exacerbation of chronic pancreatitis, with severe pain that is not relieved by antispasmodics. Sandostatin 100 mcg 3 times a day, subcutaneously.
- Prokinetics (Motilium, Cerucal) are used to suppress nausea and vomiting during exacerbation of chronic pancreatitis. Motilium 10 mg 3 times a day, 30 minutes before meals.
With long-term illness with chronic pancreatitis, endocrine disorders of the pancreas and the possible development of diabetes mellitus develop, so a mandatory consultation with an endocrinologist is necessary.
How to treat yourself at home?
Acute pancreatitis - symptoms and treatment at home can be stopped. But, if you do not know whether you are allergic to the drugs and traditional recipes listed below, then you should consult a doctor before use. Complex therapy includes several stages.
Also read: Which doctor treats the pancreas
The first stage is following a diet, doctors also recommend complete rest, all physical activity must be excluded.
The second stage is taking medications that will relieve the patient of painful symptoms.
The third stage is physiotherapy.
Drug therapy
As for medications, the first step is to take medications that will help support the functioning of the gastrointestinal tract.
Most often, doctors prescribe Almagel or enzymatic preparations. For example:
- Creon.
- Mezim.
Due to the fact that in this disease the intestinal microflora is disrupted, it needs to be restored. This can be done using Linkens or Lacidofil.
In severe cases of the disease, hormonal drugs, analgesics and antibiotics are prescribed: Ampiox, Kefzol.
Remember, before using any drug, read the instructions carefully; it is best to consult a doctor.
Diet therapy
It is necessary to understand that the disease occurs, as a rule, due to errors in nutrition. Therefore, as soon as the first signs appear, you need to refuse food for the first 24 hours. On the third day, a patient with pancreatitis is allowed to drink water.
But, since the treatment takes place at home, you can prepare dietary soups. After all, not every patient has the opportunity to administer intravenous nutrient solutions to prevent dehydration.
For this disease, follow diet No. 5 , which includes:
- Buckwheat, rice or semolina porridge.
- Chicken broth soup.
- Puree soup.
- The second courses are prepared from lean chicken or beef.
- You can steam the meatballs.
- Boiled vegetables.
Important! During an exacerbation, you should not eat legumes, fresh cabbage and radishes.
Oat drink
It is recommended to include an oat drink in your diet. A drink made from oats reduces the inflammatory process, because it contains antioxidants.
Chief gastroenterologist of the Russian Federation: “PANCREATITIS does not go away?! A simple treatment method has already healed hundreds of patients at home! To cure the pancreas forever you need...” Read more »
Rules for preparing oats: add water and leave for 24 hours. Then let it dry a little and then grind it. The result should be flour, dilute it with water and boil over low heat, leave and strain.
Also read: Chronic parenchymal pancreatitis
Application: drink fresh. Store the prepared oat drink at room temperature.
Dishes for normalizing pancreas
- Potato juice.
- Sauerkraut juice.
- Potato and carrot juice.
If you adhere to proper nutrition and take medications prescribed by your doctor, you can quickly get rid of the symptoms of the disease.
Herbal medicine at home
In order to carry out real herbal medicine at home, it is necessary to use herbs that not only have antispasmodic and choleretic effects, but also can increase the immune system and appetite.
For example:
- Immortelle.
- Dill.
- Iris.
- Yarrow.
- Chamomile and calendula.
Here are a few recipes for healing infusions.
First collection: mix 1 tablespoon each of chamomile, calendula and yarrow in a container. Pour 250-300 ml of water, boil over low heat. Strain before use.
Second collection: in a container, mix about 3 tablespoons of immortelle, 1 tablespoon of wormwood. spoon and chamomile. Prepare similarly to the above recipe.
Third collection: grind 1 tbsp in a container. spoon of barberry root, pour boiling water, approximately 200-250 ml. Leave for 30 minutes, strain before use.
Tincture of iris and wormwood
Attacks of acute pancreatitis can be treated with tincture of iris and wormwood.
Preparation: mix herbs in equal parts, pour a glass of boiling water. Leave for 20-30 minutes, before using, strain through sterile gauze or a clean cloth.
Application: it is recommended to drink 1 tablespoon half an hour before meals.
Dill decoction
Treatment of pancreatitis: you can use dill decoction at home. To prepare the recipe you will need 15 grams of chopped dill. Mix dill and 200 ml of boiling water in a container. Infuse the decoction for an hour.
At the moment of infusion, you will notice that there is less water in the container. Therefore, before using the recipe in treatment, add water to the original volume.
Also read: Modern classification of chronic pancreatitis
Potato
What else can you do to relieve the symptoms of pancreatitis? Currently, potatoes are actively used in treatment. The recipe is simple to prepare and can be used without prior consultation with a doctor.
Preparation. Take a small potato and run it through a juicer. The resulting juice should be consumed 2 times a day, drunk half an hour before meals. The course of treatment lasts for 7 days.
Propolis
An excellent beekeeping product is propolis; it can also be used in complex therapy with medications. Treatment should be carried out only with fresh propolis.
Preparation: infuse propolis in alcohol in a ratio of 2:1, leave for 5 days. If you don't have time to wait, you can use a different recipe. For example: dissolve 15 drops of pharmaceutical tincture in milk. In this case, the milk should be warm. Drink a glass before bed.
Diet and nutrition principles
If the exacerbation of chronic pancreatitis is quite serious and is accompanied by severe pain, persistent vomiting, and significant changes in laboratory tests, then patients need to starve.
It allows you to provide the inflamed organ with maximum rest and minimize the production of aggressive enzymes by the gland that destroy the organ. Its duration depends on the specific clinical case, but most often ranges from 1 to 3 days. Sometimes during the “hungry” phase it is allowed to drink rosehip decoction, alkaline mineral waters, and weak tea.
Then a special low-calorie diet (up to 2200 kcal) with a normal protein quota is prescribed. It is designed to spare the pancreas and other digestive organs as much as possible. The features of this diet are:
- exclusion of all products with a high content of extractives or essential oils (fish, meat broths, cocoa, coffee, etc.), fresh berries, vegetables, herbs, fruits, sour juices, carbonated drinks, marinades;
- ban on fatty foods (lamb, pork, cream, lard, etc.) and alcohol;
- fractional consumption of food (up to 6 times);
- chopping or mashing used products;
- salt restriction;
- dishes are served exclusively warm;
- widespread use of slimy cereal soups, vegetable puree soups with added boiled meat, soufflés, protein omelettes, fish and meat dumplings, steamed cutlets, meatballs, baked apples, vegetable purees, jellies, mousses, dried white bread, low-fat cottage cheese, jelly.
Subject to clinical and laboratory improvement, nutrition is expanded, increasing its calorie content and the amount of proteins needed for a speedy recovery. Although the set of acceptable foods is very similar to the already mentioned diet, the list of dishes on the menu increases (baking is allowed). If pancreatitis is accompanied by the development of diabetes, then white cereals, potatoes, honey, sweets, and baked goods are added to the forbidden food list.
What is an approximate menu for chronic pancreatitis?
The pancreas is a digestive organ that secretes special enzymes and hormones that help digest food and absorb nutrients.
The purpose of the diet for chronic pancreatitis:
- Reduce irritation of the pancreas;
- Eliminate symptoms of the disease (pain, bloating, nausea, loose stools, etc.);
- Provide the body with necessary nutrients.
With chronic inflammation of the pancreas, the ability to digest and absorb fats is primarily reduced, which is manifested by abdominal pain and loose stools. In this regard, the main principle when creating a menu is low fat content in the daily diet, no more than 50 grams of fat per day.
Eating low-fat foods with optimal protein and carbohydrate content reduces the load on the pancreas, reduces inflammation and prevents further damage.
When creating a menu, a number of basic principles must be observed:
| What's the point? | Principles |
| Reducing the load on the pancreas, the ability to process and absorb all fats. Eliminates pain, diarrhea, as well as impaired absorption of other substances. | Low fat content up to 50 grams per day. In this case, the total amount of fat should be evenly distributed across all meals. |
| The optimal amount of food allows the weakened pancreas to secrete a sufficient amount of enzymes to completely digest food. This reduces stagnation and fermentation of undigested food residues, which reduces bloating, pain, nausea and other unpleasant sensations. | A small amount of food up to 300-400 grams per meal. Other guidelines: The volume of food should not exceed the size of your fist or be guided by sensations; you need to eat so much food that you still want to eat at least the same amount. |
| Helps provide the body with all the necessary nutrients given the small amount of food consumed. Improves the protective properties of the mucous membranes of the digestive tract. | Frequent meals 5-7 times a day. |
| Eliminates spasms, improves the release of digestive enzymes, improves the processes of breakdown of nutrients. | Food and drinks should be warm. |
| Helps restore pancreatic function. Reduces the risk of exacerbations and complications. | Avoid substances that overly irritate the pancreas and mucous membrane of the digestive tract (alcohol, smoking, excessively fried, spicy, salty, smoked, etc.). |
Signs of exacerbation of pancreatitis
The most important symptom during an exacerbation of the disease is acute pain in the abdominal cavity. It is usually caused by previously eaten fatty, smoked, spicy foods. An exacerbation does not appear immediately, but about half an hour after eating food. For some people later. It all depends on the individual characteristics of the body.
Important! We wrote more about the symptoms and first signs of pancreatitis in our article.
Severe exacerbations are accompanied by nausea leading to vomiting. Diarrhea or constipation occurs, resulting in sudden weight loss.
Important to remember! At the first signs of exacerbation, you should seek help from a specialist!
What products are preferable for chronic pancreatitis?
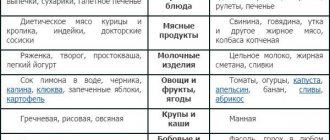
| Should be limited | Featured |
| Cream and cheese sauces, cream, fried cheese, high-fat dairy products, milkshakes. | Low-fat or low-fat dairy products such as milk, cheeses, yogurt, sour cream. |
| Fried, fatty meat, chicken with skin, animal organs (liver, etc.), duck, goose, fried eggs, bacon, canned tuna in oil, hot dogs, salami, sausages, smoked fish | Baked, boiled, stewed or steamed lean meat: veal, beef, rabbit, turkey, chicken (without skin), fish; canned tuna in its own juice, without oil, soft-boiled eggs, egg whites, steam omelet. |
| Coconut milk, nuts, nut butter, refried beans, fried tofu. | Almond/rice milk and products made from them, soy products, tofu. |
| Do not eat sour fruits and their varieties: lemon, cherry, red currant, etc. Avocados in limited quantities are high in fat. Melon, watermelon, small slices 1-2 per day. Avoid fried fruits. Limit grapes, especially those with seeds, gooseberries, plums, apricots. | Fresh, frozen, canned fruits. It is advisable to use heat-treated ones. Without peel, soft, sweetish, without coarse seeds.. For example: Sweet baked apples, bananas, blueberries. Tolerance to fruits in chronic pancreatitis is very individual. |
| Cookies, croissants, French fries, fried potatoes or corn, chips, fried rice, sweet rolls, muffins, fresh bread, baked goods. | Whole grains: bread (preferably yesterday's bread), couscous, low-fat crackers, noodles, pasta, rice, millet, barley, corn, oatmeal. |
| Fried vegetables, cabbage, raw onions, bell peppers, radishes, radishes, garlic, spinach, sorrel, daikon, tomatoes, cucumbers, white cabbage, eggplant, green peas, baby beans. | Fresh, frozen and cooked. It is advisable to use heat-treated ones. Remove peel and large seeds. Pumpkin, carrots, beets, zucchini, potatoes. |
| Lard, mayonnaise, olives, salad dressings, tahini paste. | Green cardamom, cinnamon, nutmeg, vegetable oil/butter in small quantities, maple syrup, low-fat mayonnaise, mustard, salt, sugar (in limited quantities). |
| Pastries, cakes, sweets, pies, custard, donuts. | Apple sauce, puddings, sherbet, marmalade, a small amount of chocolate, honey, jam. |
| Drinks with cream, carbonated drinks, alcohol, kvass. Juices from citrus fruits, grapes. | Compote of dried fruits, decoction of dates, sports drinks, weak tea, mineral water Borjomi, Essentuki No. 17. |
If you are low in weight, you can use special supplements containing a special type of fat such as MTC Oil, middle-chain triglycerides. Pancreatic enzymes are not required for the absorption of these fats. These fats can be purchased in sports nutrition stores in the form of separate mixtures, or they can be found in coconut and palm kernel oil (Palm Kernel Oil). Add MTS Oil to food, 1-3 teaspoons per day.
Treatment for exacerbation of chronic pancreatitis
Features of the treatment of a severe attack consist of strict adherence to bed rest, diet and taking appropriate medications only in a hospital setting, since there is a real threat not only to health, but also to human life. Before the ambulance arrives, the patient should be given first aid:
- Absolute hunger.
- Apply cold to the pancreas area.
- Complete rest and bed rest.
Many patients would like to clarify how long an exacerbation of chronic pancreatitis can last? Doctors emphasize that in most episodes, relapse of the disease does not exceed 7 days.
Auxiliary drugs for pain relief:
- enzymes (Creon or Pangrol);
- antispasmodics (drotaverine or papaverine);
- proton pump inhibitors (lansoprazole, rabeprazole).
To unload the pancreas, use:
- a diet with severe fat restriction or complete fasting for several days;
- complete exclusion of alcohol and smoking;
- Octreotide is a drug that is an analogue of the pancreatic hormone somatostatin.
Symptoms of exacerbation
Chronic and acute forms have completely different symptoms. The pain that occurs during an exacerbation is unbearable. This condition is called pancreatic colic. The person must be in bed.
The pain feels like a belt, covers the body, radiates to the hypochondrium and the left shoulder blade.
A symptom of exacerbation of chronic pancreatitis will be nausea and painful vomiting of bile, a bitter taste in the mouth, and fat impurities are visible in the loose stool. There is also a disturbance in the level of glucose in the blood: it increases significantly. This threatens secondary diabetes. The pain and vomiting do not go away even after taking medications.
Operation
To cure this disease, surgery is sometimes required. Indications for surgical treatment for chronic pancreatitis in adults include purulent complications, obstruction of the biliary and pancreatic tracts, stenosis, changes within the tissues of the gland, complex course, and other symptoms that are not amenable to conservative treatment.
The following types of surgical intervention are performed:
- sphincterotomy in the process of clogging the sphincter of Oddi;
- excision of stones in the ducts of the gland;
- opening and sanitation of purulent foci;
- pancrectomy;
- vasectomy, splanchectomy, partial excision of the stomach;
- removal of the gallbladder during complications in the large bile duct and gallbladder;
- a technique for creating circumferential bile outflows in order to reduce tension from the main pancreatic tracts.
Prevention
In order not to find out how to treat chronic pancreatitis, it is necessary to take timely measures to prevent the disease, which includes:
- to give up smoking;
- avoiding the consumption of alcoholic beverages;
- diet;
- Regular preventive examinations by specialists.
Chronic pancreatitis should be treated under the supervision of a gastroenterologist. When the first signs described in the article appear, be sure to undergo diagnostics to make an accurate diagnosis.
Why does an attack occur?
The chronic course of the disease can be replaced by an acute one for a number of reasons. This is often associated with the consumption of alcoholic beverages, which have a detrimental effect on the pancreas, but there are other circumstances:
- great physical activity;
- improper diet, replacing fractional 5-6 meals a day with uneven meals;
- non-compliance with diet instructions;
- unsystematic use of medications;
- violation of the drinking regime - you need to drink up to 2-2.5 liters per day.
Anyone who suffers from pancreatitis, no matter what form it occurs, needs to understand that alcohol affects the pancreas as a strong poison, destroying it and undermining a person’s already not very good health.
Forecast
When following recommendations for the prevention of exacerbations, chronic pancreatitis is mild and has a favorable survival prognosis. If the diet is violated, alcohol intake, smoking and inadequate treatment, degenerative processes in the gland tissue progress and severe complications develop, many of which require surgical intervention and can be fatal.
Pancreatitis Thyroid cyst: symptoms and treatment Cyst in the mammary gland Diabetes mellitus Cholecystitis Prostatitis in men: first signs and treatment
Causes of pancreatitis
The functioning of the pancreas is directly affected by the foods consumed. If the normal process of digesting food is disrupted, the person’s pancreas begins to become inflamed. As a result, acute pancreatitis occurs. There are a number of factors contributing to the development of the acute form of the disease against the background of chronic pancreatitis:
- Disruption of the gallbladder. The secreted bile becomes a source of a dangerous chemical reaction with gastric juice, which begins to destroy gland tissue.
- Gastritis and stomach ulcers.
- Intoxication of the body for various reasons. Alcohol poisoning and parasites lead to the development of the disease.
- Damage to the vascular system. Any circulatory disorders lead to improper functioning of the pancreas.
- Excessive eating. Regular metabolic disorders appear due to overeating, which increases the risk of inflammation of the gland.
- Allergic reactions.
- Genetic predisposition. The child may be born with an affected organ.
Important! Read our article for symptoms and treatment of reactive pancreatitis.
Exacerbation of pancreatitis may occur for the following reasons:
- alcohol abuse;
- excess weight;
- smoking;
- taking medications;
- regular stressful situations.
Important! Find out in our article about pancreatitis of the pancreas.
Important to remember! A healthy lifestyle can protect you from pancreatitis!