When acute hemorrhoids appear, treatment sometimes needs to be provided on an emergency basis to avoid serious consequences. Pinched nodes, severe pain, blood loss - this is not a complete list of problems that arise when this pathology worsens. Treatment should be aimed at overcoming painful and dangerous symptoms. It should be done as prescribed by a doctor, but it can be provided in a hospital setting or at home, depending on the severity of the manifestation.
Symptoms of hemorrhoids
In most cases, hemorrhoids begin unnoticed. For some time, people may feel a feeling of heaviness and mild discomfort in the anus. Since these symptoms do not affect general well-being and performance, the person does not consult a doctor. However, this stage is the most favorable for carrying out preventive measures. Subsequently, patients experience severe discomfort in the anus, pain of various types and bleeding associated with defecation.
The main symptom of hemorrhoids
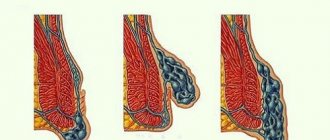
The disease is the presence of hemorrhoids in a person - dilated, sac-like and blood-filled veins of the rectum. They can be located in the lower parts of the rectum, and then only a doctor can detect them. But often they come out and become visible upon examination.
Hemorrhoids are round-shaped formations covered either with mucous membrane or thin skin. They are usually soft or elastic to the touch and, unless there are complications, painless. On average, hemorrhoids have a diameter of 0.5 to 2 cm. In case of inflammation or thrombosis, they increase significantly, become extremely sensitive and painful.
Hemorrhoids are characterized by bleeding. It almost always occurs at the time of bowel movement: when a person strains, thinned and enlarged hemorrhoids become overfilled with blood, after which they are injured by passing feces. Most often they are damaged during constipation, when the stool has a rather hard consistency.
Bleeding usually stops quickly, but may recur with the next bowel movement. With hemorrhoids, droplets of blood never mix with stool, but are usually visible on their surface or on toilet paper. Chronic blood loss due to hemorrhoids can lead to anemia (iron deficiency anemia).
Pain is the most severe and unpleasant symptom of hemorrhoids. It appears as a result of inflammation and trauma to the mucous membrane and skin with feces.
Pain is a characteristic feature of both the acute and chronic stages of the disease. With chronic hemorrhoids, pain is almost always clearly associated with stool and is felt as a burning or bloating in the anus. After bowel movement, the discomfort gradually subsides, but the burning sensation may remain for quite a long time.
During an exacerbation, the pain increases sharply, especially in the case of inflammation and thrombosis of hemorrhoids. It can be so severe and painful that people cannot sit up or sleep at night. The pain can be bursting, pulsating in nature and significantly intensify during bowel movements, coughing, sudden movements and touching the nodes.
If you discover similar symptoms in yourself, do not rush to diagnose yourself and treat yourself. Various intestinal diseases, including colon tumors, may have similar symptoms. Therefore, if there are signs of hemorrhoids, examination and treatment according to the algorithms proposed by the doctor is mandatory.
What to do for acute hemorrhoids1,2
The main thing to do if you have symptoms of acute hemorrhoids is to consult a doctor. After examining the complaints, examining and palpating, the doctor will most likely make a diagnosis. Instrumental studies will help exclude other diseases.
Treatment depends on the degree of thrombosis and the duration of symptoms of exacerbation of hemorrhoids. If 48–72 hours have not yet passed since the onset of thrombosis, the clot can be removed through surgery at the discretion of the proctologist. Sometimes you don’t even need to stay in the hospital for this.
If the disease lasts longer than 3 days, there is usually no point in surgical treatment - conservative therapy is used. Its goal is to relieve pain and inflammation. For this use:
- topical medications for relieving symptoms of hemorrhoids (ointment or cream for rectal and external use, as well as rectal suppositories);
- painkillers, both for external use in the form of ointments or suppositories, and in the form of tablets;
- anticoagulants that prevent the formation of blood clots;
- anti-inflammatory drugs;
- phlebotonics, which help improve vascular tone2.
Relief drugs are included in clinical guidelines for the treatment of hemorrhoids. Among them there are products with different principles of action. For example, “Relief” suppositories based on the vasoconstrictor phenylephrine, which helps relieve swelling, reduce inflammation and stop bleeding.
Relief Ultra contains hydrocortisone acetate, which fights inflammation, and zinc sulfate, which promotes wound healing. "Relief Advance" with benzocaine has an analgesic effect and helps relieve burning and itching from hemorrhoids.
It is important to understand that all medications have contraindications and side effects, so it is better to consult a doctor.
Causes of hemorrhoids
The risk of hemorrhoids depends on genetic predisposition. Weakness of the walls of venous vessels can be inherited by a person. Therefore, the likelihood of encountering hemorrhoids is higher among people whose relatives suffered from this disease or varicose veins.
Another predisposing factor to the onset of the disease is age. The older a person is, the less elastic his vessel walls are. This means that protrusions form in them more easily. Therefore, the disease often worries middle-aged and elderly people.
However, not all people with a genetic predisposition develop hemorrhoids. Its occurrence is also provoked by other reasons. Moreover, they can be influenced, and thereby reduce the risk of the disease. These include:
- a sedentary lifestyle and prolonged sitting, leading to stagnation of blood in the veins of the legs and rectum;
- constipation, which causes people to push;
- lifting weights, accompanied by an increase in intra-abdominal pressure and overload of the veins;
- poor nutrition: refusal of foods rich in fiber, insufficient water intake, abuse of spicy foods and alcohol.
In women, a factor that often provokes hemorrhoids is pregnancy and childbirth. The growing uterus puts pressure on the intestines, the walls of the pelvis and the veins located in it. This leads to constipation, blood stagnation and the appearance of hemorrhoids. During childbirth, problems are aggravated due to straining.
Etiology of the phenomenon
Exacerbation of hemorrhoids is associated with the influence of a number of factors. The most common triggers are the following:
- Poor nutrition. An acute attack is facilitated by the consumption of “aggressive” foods - hot seasonings, smoked foods, spices, marinades. Passion for alcoholic beverages is especially dangerous. Obvious signs of the disease appear intensely in the morning, with a hangover. It should be borne in mind that in the chronic form of the disease, even a shot of vodka can provoke an exacerbation.
- Abnormal bowel movements. Both constipation and prolonged diarrhea often cause prolapse and strangulation of hemorrhoids.
- Unfavorable posture. Prolonged sitting (especially on a hard surface) or prolonged standing on your feet leads to congestion in the pelvis, which causes the hemorrhoidal sacs to fill with blood. As a result, the risk of vein thrombosis increases, and the nodes fall out and become pinched.
- Physical exercise. An exacerbation of the disease is very often caused by heavy lifting, and this can be a one-time exposure to heavy weight or frequent unloading and loading work.
Exacerbation
The cause of the deterioration of the condition can be a variety of factors. The most common of them include:
- constipation,
- lifting weights,
- long sitting,
- diet disorders (especially alcohol abuse and spicy foods).
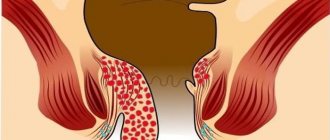
Exacerbation of hemorrhoids is always accompanied by pain: from quite pronounced to unbearable. Acute pain can appear due to blockage of veins with blood clots (thrombosis of internal or external hemorrhoids), as well as due to prolapse and pinching of nodes in the anus. The pain sharply intensifies when visiting the toilet, when touching nodes, sitting, walking and physical work.
In the acute course of the disease, hemorrhoids swell, increase in size, and acquire a bluish tint. They either adjust with difficulty or do not adjust at all. If a strangulated or thrombosed node ruptures, bleeding occurs. It can be quite strong, but the pain with this development of events decreases.
In severe cases, acute hemorrhoids are complicated by purulent inflammation of the perineal tissue. Due to poor circulation, ulcerations may appear on the surface of the nodes, which become a “gateway” for pathogenic bacteria. In such situations, in addition to local phenomena, the patient’s general well-being is also significantly disturbed: severe malaise appears, body temperature rises. It is even possible to develop such a serious complication as sepsis.
Therefore, exacerbation of hemorrhoids requires the earliest and most intensive treatment under the supervision of a proctologist.
Mechanism of attack development
Hemorrhoids are an inflammatory disease that develops in the venous plexus of the rectum in the area of the anus and is manifested by the formation of hemorrhoids, i.e. bag-like protrusions on the venous walls. Taking into account the localization of the lesion, external (external) and internal hemorrhoids are distinguished. In the first case, the hemorrhoid is located directly at the exit of the rectum in the anus or even on its surface, and therefore is detected visually. The internal location of the node hides it inside at some distance from the anus.
The disease can occur in acute and chronic form. An acute attack occurs as a result of an intense inflammatory process, vein thrombosis, or strangulated hemorrhoids. It can be an independent type of pathology or the result of an exacerbation of a chronic form. In any case, the acute type of the disease is characterized by a sharp onset, intense manifestation of the main symptoms, and sometimes a deterioration in the person’s general condition. In some cases, an attack can cause serious complications.
Prevention of hemorrhoids
To prevent the development of hemorrhoids or prevent its further progression, it is necessary to follow a number of recommendations.
- Make sure you have regular bowel movements and avoid constant constipation. Remember that this problem can be associated not only with poor nutrition, but also with insufficient physical activity and low water consumption. Drink at least 1.5 liters of plain water every day to soften your stool and make bowel movements easier.
- Limit in your diet foods that increase blood flow to the pelvis: spices, spicy, pickled and smoked foods, and especially alcohol. Give preference to vegetables and fruits that are rich in fiber and improve bowel function.
- Try to walk and swim more, especially if you have to stand or sit for a long time during the day. By the way, this will also prevent varicose veins in the legs, which often accompanies hemorrhoids. Active movements will prevent blood from stagnating in the legs and pelvis.
- Don't lift heavy objects.
- Try to wash the anus area with cool water after each bowel movement. This way you will not injure the mucous membrane and give your blood vessels a workout. If it is impossible to wash, use cold wet wipes.
- Perform special exercises to prevent hemorrhoids. The simplest of them is to squeeze the muscles of the perineum and anus, and then relax them. This exercise can be done several times a day in any environment. The main thing is regularity.
Symptoms
Symptoms occur suddenly and acutely. Due to the pinching of the node, the pain becomes unbearable. The sensations intensify even with sneezing and coughing, not to mention bowel movements.
The act of defecation is impossible without painkillers. The pain is sharp, twitching. A painful attack can last from several seconds to minutes. During this period, the patient cannot find a place for himself.
Holding back bowel movements causes constipation, which only worsens your health.
An acute attack of hemorrhoids can be recognized by the following external signs:
- A hemorrhoidal node is visible near the anus. It is blue, swollen and hard to the touch. When pressed, sharp pain occurs.
- There is blood in the stool. It can be in the form of drops or flow from the anus after a bowel movement.
- Swelling and redness of the skin around the anus.
- Discharge of mucus from the anus. The liquid causes irritation, itching and burning.
If hemorrhoids worsen, your body temperature may rise. The patient feels weak and tired. Bleeding is not always observed; it may be absent.
Hemorrhoids can get worse during pregnancy. This is due to physiological reasons. The symptoms are similar.
Treatment
INITIAL CONSULTATION
from 2,200 rub.
Treatment methods
Currently, different methods of treating hemorrhoids are used. They are divided into conservative (without surgery), minimally invasive and surgical.
In the early stages of the process, one is usually limited to the first two approaches. Surgical treatment of hemorrhoids is necessary in severe cases.
Treatment without surgery
Treatment of chronic hemorrhoids is usually used in the early stages and is aimed at preventing further development of the disease and preventing exacerbations. This can be achieved by:
- preventing constipation;
- strengthening the walls of blood vessels, increasing the tone of hemorrhoidal veins;
- prevention of bleeding from hemorrhoids.
To normalize stool, the first aid is diet and lifestyle changes: increased physical activity, abdominal massage. Only if these measures are ineffective, laxatives are prescribed.
To strengthen the walls of blood vessels, as prescribed by a doctor, drugs are used that increase the tone of the veins - venotonics. They can be used both in tablets and capsules for oral administration and for topical use.
To prevent and treat bleeding from hemorrhoids, topical preparations containing sodium alginate can be used. However, treatment without surgery is only possible for internal hemorrhoids without prolapse of nodes and frequent exacerbations. If periodic bleeding leads to the development of anemia (anemia) and interferes with general health, surgical treatment of hemorrhoids is necessary.
In case of acute hemorrhoids (exacerbation), treatment is aimed, first of all, at quickly eliminating inflammation and other symptoms, alleviating the patient’s condition and restoring the impaired quality of life.
It consists in:
- fast and effective pain relief;
- prevention of vascular thrombosis and resorption of existing blood clots;
- limiting inflammation.
For effective pain relief during exacerbation, local anesthetics, antispasmodics and analgesics are usually used. In order to resolve existing blood clots and prevent vascular thrombosis, heparin-based drugs are used. To limit inflammation, reduce swelling, itching and burning sensation, hormonal steroidal anti-inflammatory drugs are usually used as prescribed by a doctor.
Conservative methods of treating hemorrhoids also include treatment with leeches (hirudotherapy). The saliva of leeches contains the enzyme hirudin, which thins the blood, dissolves existing blood clots and prevents the formation of new ones. This technique is usually used in combination with other treatment methods.
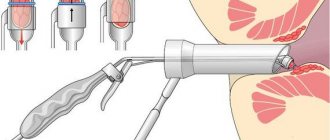
Minimally invasive treatment methods
Hemorrhoid treatment methods that allow the removal of hemorrhoids with minimal trauma to surrounding tissue are called minimally invasive. At their core, they are surgical procedures, but such interventions practically do not deprive the patient of his ability to work. These include infrared photocoagulation, cryotherapy, ligation of nodes with latex rings and some other methods. Sometimes hemorrhoids are treated with a laser.
With infrared photocoagulation, special thermal infrared rays are applied to the pedicle of the hemorrhoid. As a result, the vessels supplying the hemorrhoid are damaged. The blood supply to the node stops, and after some time it dies.
Cryotherapy
- This is the freezing of hemorrhoids using liquid nitrogen. As a result of short-term powerful cold exposure, the tissues of the node die and are rejected after some time. The moment of exposure does not cause serious pain to the patient, and after the nodes are rejected, no scars remain. This method gives the best effect in the second and third stages of the disease.
Another method of treating hemorrhoids called ligation with latex rings is also widely used. With this method of treatment, a dense latex ring is placed on the stem of the node. It compresses the vessels feeding the node. After some time, the tissues, deprived of blood supply and nutrition, die and, together with the ring, come out during bowel movements.
Minimally invasive procedures are usually performed on an outpatient basis. If pain occurs after the intervention, its duration ranges from several hours to two days. The pain is usually moderate and can be easily relieved with conventional painkillers. Patients do not require sick leave; they can start working in a few hours.
Surgical removal
Surgery to remove hemorrhoids is now resorted to only in the most difficult cases - for example, at the third or fourth stage of hemorrhoids, when other methods are ineffective. This operation is performed in a hospital using intravenous anesthesia, spinal or local anesthesia. Depending on the type of operation, the patient spends 2 to 7 days in the hospital.
Treatment methods for acute hemorrhoids
If signs of exacerbation of hemorrhoids appear, treatment should begin as quickly as possible. The list of therapeutic methods is determined based on the type of hemorrhoids, its stage, and existing complications (thrombosis or strangulation). In addition to conservative treatment (medicines, diet, folk remedies), surgical intervention is used.
The choice of treatment method is influenced by factors such as the presence of hemorrhoidal strangulation and the duration of this phenomenon, the presence of thrombosis, and much more.
Drug therapy
For acute hemorrhoids, local medications in the form of ointments, suppositories and gels are used. Oral agents are used when vascular walls are weakened and there is a high risk of blood clots, as well as in the presence of an inflammatory process. Medicines are selected based on the existing symptoms. These can be anti-inflammatory, painkillers, hemostatic agents. For greater effect, complex medications are prescribed for local use:
- Posterisan Forte;
- Proctosan;
- Procto-Glyvenol;
- Anuzol;
- Relief Ultra;
- Gepatrombin and others.
The listed suppositories for acute hemorrhoids are prescribed when the nodes are located inside the rectum.
If bleeding occurs, blood thinning drugs are not prescribed. In such situations, preference should be given to products with an antimicrobial effect in order to prevent infections from entering the wounds.
If there is an exacerbation of external hemorrhoids, proctologists give preference to medications in the form of ointments and gels:
- Heparin ointment;
- Troxevasin;
- Proctosedyl;
- Levomekol;
- Bezornil;
- Hepatrombin G;
- Aurobin and others.
They are applied directly to the external hemorrhoids and on a gauze pad and left overnight.
In case of an acute attack of hemorrhoids, oral medications are also prescribed: Phlebodia, Ginkor Forte, Movalis, Detralex and others. They fight the cause of the disease - varicose veins, strengthen the walls of blood vessels, and increase their tone. They can also be used to prevent exacerbations of hemorrhoids.
In extreme cases, when the pain becomes unbearable and the drugs mentioned above do not help eliminate the symptoms and relieve inflammation, suppositories with adrenaline and novocaine blockade are used.
Diet
The first thing to do in case of acute hemorrhoids is recommended by all proctologists without exception - to adjust your diet. The patient is recommended to follow a strict diet, the purpose of which is to normalize stool and eliminate constipation and diarrhea. The following products are excluded from the menu:
- fresh milk;
- legumes;
- mushrooms;
- pickles and marinades;
- smoked meats;
- baked goods;
- fatty fish and meats;
- spices;
- any fast food;
- alcohol, coffee, strong tea, carbonated drinks.
The basis of the diet is cereals, vegetables and fruits. They contain a lot of fiber, which helps normalize stool. Fermented milk products also help restore stool: kefir, fermented baked milk, natural yogurt without additives, cottage cheese. The diet also involves including eggs (no more than 2 per day) and lean meat (poultry breast, beef). It is useful to include laxative foods in the menu.
Meals should be regular: the number of meals reaches 5-6 per day, the portion size is average. It is advisable to drink plenty of water between meals. The minimum volume of liquid is 2-2.5 liters. These can be compotes, juices, herbal teas or plain water.
If, if you are prone to constipation, the diet does not help improve bowel movements, proctologists recommend using mild laxatives, for example, Regulax, Duphalac, Fitomucil or Mucofalk.
Video with a specialist’s opinion on nutrition for hemorrhoids:
Surgery
Surgical intervention for hemorrhoids is prescribed after overcoming the exacerbation, however, in case of severe bleeding, pinched nodes and thrombosis of hemorrhoidal veins, it can be performed urgently.
The choice of how to treat hemorrhoids with surgical methods depends on the stage of development of the disease:
- In the early stages, minimally invasive interventions are used - ligation with latex rings, photocoagulation or laser therapy, cryodestruction, disarterization and sclerosis.
- At stages 2, 3 and subsequent, when the nodes have reached a large size and began to fall out of the rectum, a Milligan-Morgan hemorrhoidectomy or Longo operation is performed.
- In the presence of thrombosis of hemorrhoids, thrombectomy is used.
Before surgery, it is necessary to undergo a course of conservative therapy. The use of topical and oral agents continues after surgery.
Folk remedies
In case of exacerbation of hemorrhoids, treatment at home is more preferable; only in case of pinched nodes and thrombosis, hospitalization is necessary. Left without the constant supervision of a specialist, most patients use additional means to eliminate the symptoms of hemorrhoids:
- sitz baths with herbal decoctions (chamomile, calendula);
- lotions and compresses with oils (sea buckthorn, butter, etc.) and garlic;
- microenemas with herbal decoctions (chamomile, oak bark, calendula);
- self-made rectal suppositories (from potatoes, ice, sea buckthorn oil, propolis);
- homemade ointments with sea buckthorn with oil and propolis, potato juice.
The effectiveness of most folk remedies used for treatment at home is questionable. They are recommended to be used only in combination with medications. Relying only on home remedies is dangerous, since they poorly relieve symptoms and have virtually no positive effect on blood vessels and do not prevent the further progression of hemorrhoids.
Important! Before using folk remedies, you should consult your doctor. Some home remedies have serious contraindications.
Internal and external hemorrhoids
There are several classifications of hemorrhoids. One of them is based on the location of the nodes. On this basis, internal and external (external) hemorrhoids are distinguished, as well as a combined form, when the nodes are located both in the lumen of the rectum and outside it.
Internal hemorrhoids
Course of the disease
Manifestations of internal hemorrhoids depend on the stage of the process, the size of the nodes, the presence of complications and concomitant diseases of the rectum. In the early stages, under the influence of provoking factors, a feeling of discomfort or a foreign body may appear in the anal area. But since the nodes do not come out, the patient rarely pays attention to these symptoms.
As the disease progresses, the feeling of discomfort increases, as the internal nodes increase in size and make the intestinal lumen narrower. When dense stool passes, pain and bleeding appear, and the mucous membrane around the internal nodes may become inflamed. Then a discharge appears from the rectum, which irritates the skin around the anus, causing itching and burning.
If internal hemorrhoids continue to grow, they increasingly interfere with the free passage of feces. Therefore, the stretched and thinned intestinal wall becomes very vulnerable. She bleeds every now and then, and bowel movements become very painful. The nodes can fall out and do not always correct themselves.
Complications of internal hemorrhoids
With internal hemorrhoids, complications may develop that require urgent medical attention. As a result of blood stagnation, a blood clot may appear inside the node, that is, thrombosis develops. A complication of internal hemorrhoids can also be strangulation of the hemorrhoid when it falls out.
The pain in such cases intensifies sharply and becomes unbearable. Thrombosis is often accompanied by inflammation, which, if left untreated, can spread to nearby areas. Therefore, medical assistance for complications should be provided as early as possible.
Diagnosis of internal hemorrhoids
Diagnosing internal hemorrhoids in the early stages is not easy, because the nodes are not visible from the outside. Therefore, to make a correct diagnosis, it is necessary to use additional examination methods. These include:
- digital examination of the rectum, when the doctor can find protruding nodules using the index finger;
- anoscopy, that is, examination of the lumen of the rectum and its mucous membrane with a special device that provides information about the condition of approximately 10 cm of the intestine;
- sigmoidoscopy is an examination using a special optical tube that allows you to see high-lying nodes and makes it possible to examine the rectum over a distance of 25 cm.
Treatment of internal hemorrhoids
Treatment for internal hemorrhoids is prescribed by a doctor. It depends on the size of the nodes and the stage of the disease. At the initial stage of the disease, you can limit yourself to the use of medications. For internal hemorrhoids, they are usually used in the form of suppositories. In parallel with local treatment, agents that increase venous tone are often recommended. They are taken orally over a long course.
If medications are ineffective and in later stages, minimally invasive surgical treatment methods are used that allow removal of already formed nodes.
External hemorrhoids
Course of the disease
With external hemorrhoids, the nodes are located outside around the anus. They are formed due to the expansion and protrusion of the walls of hemorrhoidal veins, which are normally located under the skin of the perineum near the anus.
The first symptoms of the disease with external hemorrhoids may appear even before the hemorrhoids become significantly enlarged. A person periodically experiences itching and discomfort in the anus, and may notice traces of blood on toilet paper. At the same time, the patient himself feels with his fingers the peculiar “bumps” around the anus.
With external hemorrhoids, the nodes are more easily injured and inflamed, so exacerbations occur more often than with internal hemorrhoids. However, in the “calm” stage, a person may not make any complaints.
Complications of external hemorrhoids
External hemorrhoids, like internal hemorrhoids, can be complicated by node thrombosis. In this case, acute and very intense pain occurs, intensifying with movement, coughing, and sneezing. The knot increases in size several times and dramatically impairs a person’s ability to work, as the pain intensifies from contact with clothing. When an inflammatory process occurs, redness and swelling appear around the node, and the body temperature may also increase. Treatment of complications of external hemorrhoids should be under strict medical supervision.
Diagnosis of external hemorrhoids
Diagnosing external hemorrhoids is usually not difficult. After all, the nodes are located outside. They can be seen during a routine examination of the anal area.
Treatment of external hemorrhoids
When treating exacerbations of external hemorrhoids, it is more convenient to use medications in the form of ointments. Various sitz baths are also used, as well as a variety of lotions.
External hemorrhoids often cause significant discomfort and exacerbations follow one after another. Therefore, in many cases, external manifestations require surgical intervention. It is usually minimally invasive and quite easily tolerated by the patient.
However, if factors that provoke the development of hemorrhoids remain in a person’s life, after surgery the nodes may reappear after some time. Therefore, the main condition that will help prevent the development of both internal and external hemorrhoids is a change in lifestyle.
Exacerbation of pathology
Symptoms and treatment prescribed to eliminate acute manifestations largely depend on the mechanism of development of the pathology. Acute external hemorrhoids (like the internal variety) develop rapidly, but the impetus for development is 2 reasons - strangulation of the hemorrhoid or thrombosis.
When the formation falls out as an exacerbation of a chronic disease, strangulated hemorrhoids always develop. As a rule, the cause of this phenomenon is physical activity or strained bowel movements. For a number of reasons, a sphincter spasm occurs, and the spasmed muscle blocks the knot from returning to its place after the load is removed. As a result of pinching the leg of the node, the blood outflow from the sac stops, swelling and intense pain appear. Prolonged stay in this position leads to the fact that the blood in the cavity of the node thickens, forming a blood clot. Next, a necrotic process is provoked, which necessitates surgical intervention.
According to the nature of the prolapse of nodes, hemorrhoids are divided into the following degrees of severity:
- Stage 1 - the formation falls out during defecation, but then returns to its original place on its own;
- Stage 2 - the hemorrhoid falls out and does not come back on its own, but it can be easily set back by hand;
- Stage 3 - the strangulated node cannot be set by hand, and the question of what to do can only be resolved with the assistance of emergency medical assistance.
The second mechanism for the development of the acute form of the disease is associated with thrombosis. Blood clots, i.e. blood clots are formed as a result of the appearance of stagnant zones in the veins. The blood mass begins to actively enter the cavity of the hemorrhoid, providing it with excess pressure and an increase in size. Severe pain occurs as a result of compression of nerve endings. Damage to the swollen sac during the passage of feces contributes to intense bleeding.
The thrombotic mechanism of development of acute hemorrhoids is divided into 3 stages:
- stage 1 - symptoms of the acute form are clearly expressed, but the process occurs without an inflammatory reaction;
- stage 2 - the inflammatory reaction does not extend beyond the boundaries of the hemorrhoid, which can cause slight redness and swelling in the immediate vicinity of the lesion;
- stage 3 - inflammation spreads to surrounding tissues, causing damage down to the subcutaneous tissue.
Stages
There are several stages of hemorrhoids depending on the size of the hemorrhoids and the degree of their prolapse.
- The first stage
is manifested by small nodes - up to 1 centimeter in diameter. They never fall out of the anus and can only be detected by digital examination of the rectum or examination using endoscopic techniques. Typically, patients at this stage do not present any complaints other than discomfort during bowel movements. - At the second stage
, hemorrhoids increase to 1-2 cm in diameter; during stool they can come out, causing discomfort, but quite quickly spontaneously return to the rectum. At this stage, characteristic signs of hemorrhoids appear: itching, burning, feeling of a foreign body in the rectum, minor bleeding. - The third stage
of hemorrhoids is characterized by prolapse of hemorrhoids, and they cannot be set back. However, the patient can return them back himself using his finger. Such nodes can become pinched in the anus, and thrombosis often develops in them. Itching, burning, bleeding, discomfort and pain can be either constant or intermittent. - In the fourth stage
of the disease, hemorrhoids fall out of the anus not only when visiting the toilet, but also during any physical stress that increases intra-abdominal pressure - lifting weights, coughing, laughing. The nodes at this stage are almost impossible to straighten on your own. All symptoms are very pronounced, bleeding can be quite heavy. Hemorrhoids at this stage are often accompanied by complications - thrombosis, weeping of the skin around the anus. Erosions, skin ulcers, infection through damaged areas and the development of a serious disease - paraproctitis - are possible. If the fourth stage of hemorrhoids is detected, surgery is indicated.
Acute hemorrhoids - what is it and how does it manifest?
Acute hemorrhoids are a condition in which a sudden exacerbation of the chronic form of the disease occurs. Proctologists consider this phenomenon dangerous and requiring urgent specialized help. The main symptoms by which an exacerbation of hemorrhoids can be identified are as follows:
- intense throbbing or twitching pain in the anus, which intensifies when sitting on a hard surface, coughing, during and after bowel movements;
- swelling of hemorrhoids - both internal and external hemorrhoids increase, the nodes fall out of the anus, become dense and become cyanotic;
- bleeding that occurs after a hemorrhoid ruptures and provides temporary relief from symptoms.
In most cases, the acute form of hemorrhoids is accompanied by inflammation of the nodes. The beginning of this process is indicated by redness of the mucous membrane of the rectum (if hemorrhoids are internal), anal folds and the skin over the external hemorrhoid.
In this case, additional symptoms appear in the form of swelling of the anus, a slight increase in temperature and fever (this occurs very rarely).
If treatment for the acute form of the disease is not started on time, the inflammatory process spreads to the surrounding tissues, including subcutaneous tissue. In this case, there is a high risk of purulent paraproctitis.
When inflammation spreads to the subcutaneous tissue, the pain spreads to the entire perineum. Exudate is released from the anus, which causes additional irritation.