Intestinal metaplasia of the stomach is the degeneration of the gastric glandular epithelium into the intestinal one. The parietal cells that produce hydrochloric acid cease to perform their functions. In this case, not only the digestive organ suffers, but also the metabolism as a whole. When gastric cells are replaced by the epithelium of the small intestine, the human condition is dangerous, but curable. If instead of stomach cells, colon cells begin to multiply in it, then the condition is characterized as precancerous. Treatment is possible, but advanced forms have a poor prognosis.
Development of pathology
Pathological disruption of the cellular activity of the digestive organ occurs mainly in older people. Constant renewal of cellular material is a natural process inherent in the genetic apparatus of gastric cells. The intense impact of negative factors on the mucous membrane causes an increase in the rate of their formation. When the proliferation rate of gastric cells exceeds the permissible rate, failures of the genetic program occur, resulting in the formation of intestinal cellular structures instead of gastric ones. The functionality of glandular tissue also changes, performing the role of intestinal absorption.
There are 2 types of intestinal pathology of the stomach.
- Small intestinal, also called mature. Found in most cases in patients suffering from gastritis. The stomach contains a full set of enterocytes: columnar enterocytes, goblet epithelial cells, exocrinocytes with acidophilic type granules, enterochromaffinocytes of various types: EC, ECL, I, S, D. Goblet epithelial cells fill the space of the stomach, being framed by bordered epithelial cells. The specificity of the histology of metaplasia is the presence of acidophilic exocrinocytes, especially in large numbers, accumulating in the recesses of the folded surface along with borderless epithelial cells.
- Intestinal metaplasia of the stomach of the immature type is characterized by the formation of goblet epithelial cells combined with prismatic epithelium, reminiscent of columnar cells of the large intestine. Endoenterocytes characteristic of the small intestine are not detected. A cytogenetic study reveals polyploidy of the nuclei and an increase in the intensity of the regulatory function of the nucleus on metabolic processes in the cytoplasm. When prismatic and endocrine epithelium are identified, mixed mucosal metaplasia is established. Immature (colic) metaplasia is diagnosed much less frequently. When cells characteristic of the small and large intestine are detected, a conclusion is drawn about a transitional form and the beginning of the development of a precancerous condition. A malignant neoplasm of the stomach is detected by histological examination in nineteen out of twenty patients with colonic metaplasia. Benign cell metamorphosis in the colonic form of metaplasia occurs in only one out of ten patients. In the absence of timely treatment, colonic metaplasia ends in death.
The degree of the disease is marked in Latin letters (A, B, C) and is described as minor, incomplete and complete.
Focal intestinal metaplasia, depending on the scale of the lesion, is divided into:
- weak - with the scale of damage to the surface of the mucous membrane up to 5%;
- medium – covering less than 1/5 of the entire surface of the stomach;
- strong – when spreading over more than 1/5 of the mucosal surface.
Based on the nature of the pathology, there are 3 types of metaplastic processes:
- With the pyloric type of disorder, focal and diffuse lesions are distinguished. The focal direction of the pathology reveals lesions of some glands of the fundic type. The renewal of glandular glandulocytes occurs with failures, the results of which are the formation of enterocytes. With a diffuse nature, the glandular cells of the stomach become smaller, since new glandular glandulocytes are involved in pathological processes, the process proceeds unidirectionally from the pyloric to the fundic. The antrum of the stomach is also subject to pathological renewal.
- Ciliary pathology often has an unfavorable prognosis, as it is detected during the development of malignant carcinoma. The appearance of ciliated epithelium in the gastric region is not considered normal, but a malignant neoplasm cannot be guaranteed. About a third of ciliary pathologies accompany benign gastric metaplasia.
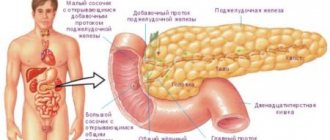
- In pancreatic pathology, the glandulocyte is stained unevenly over its surface: one pole of the cell is stained with eosin dyes, the other pole is stained with basophilic dyes.
Prevention
There are no special measures to prevent the development of metaplasia. These are the principles of healthy eating, giving up bad habits and self-medication (including folk recipes), as well as feasible physical activity.
A normal psycho-emotional state is of great importance in the prevention of gastrointestinal problems, so it is advisable to exclude stress and nervous overload from your life. If pain of various localizations is detected, it is worth undergoing timely examinations, and also do not forget about the treatment of chronic diseases.
All these recommendations will help not only avoid the development of this terrible pathology, but also significantly improve the quality of life.
Gastric metaplasia is a serious disease that is difficult to treat. Many factors lead to the development of the disease, some of which are difficult to prevent.
If symptoms of gastrointestinal problems are detected, you should definitely visit a doctor for further examination. The danger of metaplasia lies in its asymptomatic onset and rapid progression to irreversible changes.
What factors can trigger the disease, what are the main symptoms and methods of diagnosing the disease, as well as suitable types of treatment - all the information of interest on the topic is in our article.
Sources of pathology
There is no complete confidence in the guaranteed list of negative factors that influence the development of pathological processes in the gastric region, but a group of provoking factors that are directly related to the development of intestinal metaplasia has been identified. These include:
- irritation of the inner surface of the stomach;
- chronic inflammatory phenomena of the mucous surface;
- prolonged depression or severe psycho-emotional stress;
- inflammation of the esophagus;
- ulceration of the mucosal surface;
- frequent reflux of the contents of the gastric and duodenal parts of the digestive tract into the esophagus.
Patients suffer from low acidity in the stomach. The consequence of this is a selective change in the microflora in the digestive tract: the death of gastric bacteria and the abundant proliferation of intestinal bacteria.
One of the dangerous “acquisitions” of the stomach at this time is the appearance of Helicobacter pylori.
The proenzymes secreted by this bacterium add salts of nitric and nitrous acids, thereby forming carcinogenic substances (nitroso compounds). Combining their effects with other carcinogens contained in food products, nitroso compounds damage the mucous membrane and contribute to the formation of a malignant tumor. The pathological process can be intensified by the abuse of salty foods and alcoholic beverages.
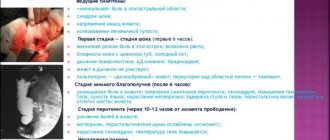
Main symptoms
One of the main threats of this disease is its almost asymptomatic course. In the early stages, when treatment is particularly successful, the disease manifests itself as minor discomfort, which usually no one pays attention to.
The situation is worsened by the fact that metaplasia usually develops against the background of chronic gastritis or ulcers, so patients mistake the signs for symptoms of existing diseases.
The main signs of gastric metaplasia:
- Nausea or vomiting.
- Burning feeling in the stomach.
- Feelings of hunger appear in the evening and at night.
- Heartburn and bitterness in the mouth.
- Periodic pain in the side.
- Loss of appetite.
- Weight loss.
In most patients, symptoms appeared irregularly and without great intensity. This significantly complicates the diagnostic task and also leads to significant progress of the disease.
Diagnosis of the disease
The disease is differentiated during fibrogastroduodenoscopy, after which a histological analysis of the contents is carried out. The biopsy reveals pathological enterocytes secreting sulfamucin, which is a powerful adsorbent of carcinogenic substances. With a high concentration of carcinogens, there is a high risk of developing a malignant tumor. A high concentration of carcinoembryonic antigen is also found in the blood. The diagnosis is formulated with the type of metaplasia and an indication of its localization in the parts of the stomach.
Features of nutrition in pathology
The diet for intestinal metaplasia should be gentle so as not to irritate the epithelial cells of the gastric mucosa. Food intake is increased to 5-6 times a day, eating in small portions in a warm form for better absorption of food.
Cooking methods: boiling, baking, steaming.
Prohibited:
- fatty meats and fish;
- canned pickled, salty, sour food;
- legumes, nuts, mushrooms;
- fresh vegetables with coarse fiber and essential oils (radish, radish, garlic, onion);
- sour fruits: citrus fruits, cranberries;
- any alcohol-containing and carbonated drinks.
Allowed:
- chicken, rabbit, veal;
- cod, pollock, hake;
- vegetable soups;
- porridge;
- low-fat dairy products: cheese, cottage cheese, fermented baked milk;
- animal fats in limited quantities;
- Drinks include weak tea, compote, and jelly.
Treatment of metaplasia
Treatment of intestinal metaplasia depends on the extent of the disease and its type. There are 2 treatment methods:
- Therapeutic treatment is aimed at destroying the bacterium Helicobacter pylori, preventing the appearance of malignant carcinoma and reducing the symptoms of gastroesophageal reflux pathology. It is impossible to do without the use of antibiotics in the fight against Helicobacter pylori. To restore beneficial microflora, preparations such as Linex are used. It is also necessary to take immunomodulators of synthetic and natural origin. For this purpose, treatment can be supplemented with traditional medicine based on herbal medicine. Drug treatment is carried out under conditions of dynamic monitoring of the patient’s condition and the progress of the recovery process in the stomach. If conservative treatment is unsuccessful, surgical intervention is resorted to.
- Radical treatment can be carried out by abdominal and laparoscopic methods. The advantage of surgery is to prevent the development of malignant tumors.
Why is “ordinary” atrophic gastritis dangerous?
Chronic gastritis with atrophy of the gastric mucosa is becoming an increasingly common diagnosis. At the same time, patients in whom it is detected have an ambivalent attitude towards their new disease.
Some “dismiss” it, believing that almost all of our adult contemporaries have gastritis, and therefore it is not worth special attention to it. Others, having gleaned superficial information from available sources, fall into horror and think that cancer is now inevitable for them.
Sometimes doctors are guilty of this because they did not explain to their patients the essence of the disease, its severity, the need for treatment and possible consequences. Let's try to at least partially fill this gap.
In a healthy person, in the mucous lining of the stomach there are glands that form the main components of gastric juice. They are hydrochloric acid and enzymes that break down the proteins of any food eaten by a person. In the case of atrophic gastritis, the cells of these glands are replaced by scar (fibrous) tissue and/or cells similar to intestinal ones.
Causes of atrophy
To choose the optimal treatment strategy, it is important to understand the causes of the disease.
Atrophy in the gastric mucosa may result from:
- presence of Helicobacter pylori microbes;
- immune breakdowns (autoimmune process);
- the harmful effects of environmental factors (smoking, diet lacking antioxidants, alcohol, salt, nitrites, food nitrates, etc.).
In individual patients, several causes may be present.
Types of atrophy
When assessing atrophy, doctors note that it differs by location, being divided into:
- atrophy of the mucous membrane of the fundus and/or body of the stomach (fundic);
- atrophy of the mucous membrane of the antrum (outlet) of the stomach;
- widespread (multifocal) atrophy (the mucous membrane of several parts or even the entire stomach is affected).
In addition, there are different degrees of severity of the atrophic process. According to the latest classification, actively recommended by international experts, there are four of them. Moreover, the severity and area of distribution of atrophy are in no way related to the patient’s subjective feelings and the severity of his complaints.
So, with 1st degree atrophy (in which there is no risk of stomach cancer at all), the patient may suffer from pain and nausea. And with atrophic changes corresponding to the 4th degree, and a high risk of possible development of an oncological process, the patient notes excellent health.
Consequences of atrophy
There is a threat of atrophy degenerating into a cancerous tumor.
Most patients think that with atrophy of the gastric mucosa, the digestion of the main components of food is disrupted and “indigestion” occurs.
Indeed, in the case of a severe and widespread atrophic process (especially with fundal atrophy), this is possible. However, atrophic gastritis is fraught with much more serious consequences.
International medical communities have unanimously recognized that the tiny bacteria Helicobacter pylori has proven to be the most proven factor that increases the risk of stomach cancer. The process of their formation goes through more than one stage. First, these microbes provoke non-atrophic gastritis.
Then it becomes atrophic. Subsequently, cells appear in the gastric mucosa that are similar to the cells of the small or large intestine (doctors call this transformation intestinal metaplasia). Gradually, intestinal metaplasia transforms into dysplasia.
And the final stage of this sequential process is stomach cancer.
Of course, not all patients with atrophic gastritis will develop all of the listed stages. The process is influenced by the genetic characteristics of a particular patient, the state of his immunity, the type of microbe Helicobacter pylori (they differ in their ability to cause cancer), environmental factors, and lifestyle. All these factors determine:
- presence and severity of atrophy (and intestinal metaplasia);
- influence on the production of gastric juice;
- degree of risk of cancer.
But in patients infected with these unfortunate microbes and having severe atrophic gastritis, the likelihood of cancer in the stomach is 5 times higher than in patients with Helicobacter pylori, but without atrophic gastritis, and 14 times higher than in the lucky ones who are not infected with these bacteria and not having atrophy of the gastric mucosa.
If atrophy is of autoimmune origin, then not only the risk of cancer increases (2-4 times), but also of hormonally active carcinoid tumors of the stomach.
Flow options
During many years of observations, researchers found that with atrophic gastritis, different options are possible, including:
- reverse development of atrophy (this occurs only in the body of the stomach);
- stabilization of atrophy (especially with a mild degree of the process);
- progression of atrophy (more often with moderate and severe atrophy, without treatment, in the elderly).
Of course, the last one is the most unfavorable. Reverse development of atrophy or its stabilization is possible with timely and adequate treatment.
Scientists involved in cancer prevention (cancer prevention) provide convincing evidence that eradication (complete destruction) of Helicobacter pylori microorganisms reduces the risk of stomach cancer. Of course, the effectiveness of treatment is significantly higher before the development of precancerous changes (that is, at the stage of non-atrophic gastritis).
But even in the case of atrophy, eliminating Helicobacter pylori can slow down its progression or even lead to reverse development. Particularly good results are observed when treating young patients.
According to Japanese gastroenterologists, in patients under 30 years of age, the cancer prevention effect reaches almost 100%, while in patients over 70 years of age, this figure drops to 41% in men and 71% in women.
Unfortunately, there are no such encouraging results in the treatment of autoimmune gastritis. Moreover, international-level recommendations have not yet been developed for doctors (taking into account all the rules and principles of evidence-based medicine).
Thus, although atrophic gastritis is considered a precancerous disease, it is by no means a “death sentence” and does not necessarily end in stomach cancer.
Malignant degeneration of the gastric mucosa is a complex, gradual and multi-stage process, which is influenced by many different factors. But the appearance of atrophy should be a signal for timely and competent treatment under the guidance of a specialist.
Which doctor should I contact?
Stomach diseases, including atrophic gastritis, are treated by a gastroenterologist. At the initial stage, both a therapist and a family doctor will help.
As the disease progresses, it will be necessary to undergo an FGDS, that is, it will be necessary to contact an experienced endoscopist. In some cases, the patient is examined by an oncologist to interpret the changes obtained.
For more thorough treatment, you need to visit a nutritionist, as well as a physiotherapist, and learn about acceptable methods of treating the disease at home.
Prepared based on the article: https://myfamilydoctor.ru/chem-opasen-obychnyj-atroficheskij-gastrit/