Colon cancer is one of the most common pathologies of the gastrointestinal tract, ranking 3rd in global clinical practice. In the Russian Federation, it is more common in men. As a percentage, the disease among Russian males is 5.3%. For women, this figure is 4.7%. Oncologists try to preserve the functions of this organ by performing surgery. This is largely determined not only by the use of the latest operating techniques, but by a properly conducted rehabilitation period. The choice of the only correct restorative technique and diet for such a patient is largely determined by the condition after removal of the intestinal tumor. This operation is one of the most traumatic types of surgical intervention. In addition, most often it has to be performed on elderly patients who have difficulty recovering after tumor removal due to the presence of concomitant diseases of systemic organs, which increase the risk of postoperative complications.
Diagnostic specifics
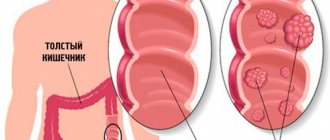
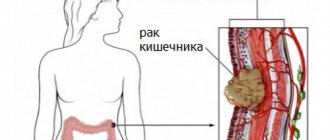
Cancer affects the intestine in different segments. The higher the tumor is localized in the rectum, the greater the risk of metastases that penetrate into the nearest lymph nodes.
The degree of malignant lesion is determined differentially: the higher its value, the greater the danger the patient is exposed to. Oncologists have developed the following gradation for this neoplasm :
- high, in which more than 95% of cancer cells are glandular tissue;
- moderate, for which the level of glandular structures is 50-95% in cells affected by cancer;
- low, in which neoplasms are occupied by extracellular mucus, ranging from 5 to 50% or higher;
- undifferentiated, in which no more than 5% of mutated cells are detected during diagnosis.
The degree of development of the oncological tumor will determine the condition after removal of the intestinal tumor.
To determine the stage of the disease and choose effective treatment tactics, doctors use different diagnostics:
- taking anamnesis;
- study of analyses;
- colonoscopy;
- MRI;
- Ultrasound;
- computed tomography of the peritoneum;
- X-ray;
- clinical and biochemical blood test;
- ECG.
Doctors also usually prescribe for older people who seek help an additional examination of blood coagulation, ultrasound diagnostics of the blood vessels of the cervical spine, legs, echocardiography, and also suggest examination by a cardiologist, neurologist and endocrinologist in cases where they have a number of chronic systemic pathologies organs.
The success of treatment directly depends on the quality and efficiency of diagnostic measures. Modern hardware examination of patients allows early detection of intestinal cancer in a patient with a high degree of probability. This ensures successful treatment. During the examination, ultrasound machines, MRI, colonoscopy and other examination techniques are used to accurately determine not only the presence of a malignant tumor in the intestine, but also its location.
Comprehensive diagnostics is especially effective in the early stages. The problem of oncology treatment is early diagnosis. Modern techniques make it possible to successfully treat the disease in the early stages, while maintaining patients’ usual lifestyle. Clinical practice statistics in developed countries show good results. In Japan, specialists were able to significantly reduce the mortality rate among people with this form of cancer.
A biochemical analysis of blood and urine is also performed. With their help, various substances are identified that leave cancer cells in the body:
- enzyme;
- proteins;
- hormones;
- antigens.
Cancer, like infection, causes the development of inflammatory processes in the body. An in-depth analysis of blood and biological fluids allows you to accurately determine the cause of inflammation and malaise. Such analyzes are carried out within one day. Having received them and the results of the hardware examination, the oncologist has the opportunity to obtain accurate information about the condition of the cancer patient at the stage of selecting a treatment system for the disease.
One type of analysis is not enough to make a diagnosis and prescribe a specific treatment. When taking blood, specialists examine the sedimentation rate of erythrocytes, leukocytes and hemoglobin. If there are deviations from the norms typical for a healthy person and the results of hardware diagnostics, an oncological disease is detected. Doctors always accurately determine the cause of the inflammatory process in the body.
Patients with cancer have an increased content of leukocytes in the blood, which in medicine is called leukocytosis. Against this background, ESR increases and hemoglobin levels sharply decrease. This result of a biochemical and clinical blood test does not always indicate the presence of cancer in a person. Such blood composition indicators are caused by any inflammation in the body.
Loss of hemoglobin can result from poor nutrition or extensive blood loss. When the intestine is damaged by cancer, hemoglobin also drops significantly at an early stage of its development. This is due to the fact that the specific structure of cancer cells does not allow it to be produced in the required volume due to changes in the condition of the blood. Because of this, the amount of oxygen in the blood decreases because hemoglobin cannot deliver it to healthy cells. If, after repeated biochemical analysis, a patient has low hemoglobin over a long period of time, it is necessary to undergo an in-depth diagnostic examination to identify the causes of this process.
Detection of intestinal tumors in the early stages significantly simplifies treatment and reduces the risk of postoperative complications.
Features of treatment of colon affected by cancer
When diagnosing a malignant neoplasm in the intestine, it is classified according to a certain scheme:
- by location on the intestine;
- size of the lesion;
- form;
- affected area;
- histological structure;
- by whether the lymph nodes are affected by it or not;
- the presence of metastases.
Oncological tumors have only four stages of development. At the beginning, it is easier for a specialist to select an effective treatment than at the final stages of the pathology. When choosing the appropriate method, the oncologist always proceeds from the presence of contraindications in the patient to a particular technique. In this case, most often the doctor uses surgery to combat such oncology. This technique can be complemented by chemotherapy. The operation itself can be not only open, but also minimally invasive. The type of complex treatment will directly determine what the condition will be after removal of an intestinal tumor. After any operation, the patient requires rehabilitation. The difficulty is that patients often seek medical help in the last stages of oncology.
Surgical treatment methods
This is the most common way to combat the disease and is considered the most effective. There are radical and supportive (palaitical) resections. In the first case, the tumor is removed from the intestine in those places where healthy soft tissue comes into contact with lymph nodes affected by cancer .
The supportive technique is used for inoperable patients. With its help, intoxication and pain are relieved, and the patient’s general condition is improved so that the last period of his life is as comfortable and long as possible.
Any type of treatment is aimed at saving a person's life. To achieve this goal, the period after surgery is important. At this time, the patient may be prescribed additional treatment in the form of chemotherapy. Continuation of therapy may also be required for chronic diseases of systemic organs. The choice of restorative and paleative therapy depends on what the patient’s condition is after removal of an intestinal tumor
conclusions
For some people with Crohn's disease, your doctor may recommend a bowel resection to treat severe complications such as strictures and fistulas. The surgery involves removing the damaged portion of the small intestine and then reconnecting the healthy portions. Successful bowel resection surgery can allow a person to live for years without symptoms. However, in some people, symptoms may return and sometimes a second operation may be necessary. It is important for a person to take care of their body before surgery and during recovery to give themselves a chance to heal. Working closely with your doctor can help support proper recovery and reduce the risk of complications.
The authors of another study claim that patients with Crohn's disease are more likely to have anxiety disorders.
Chemotherapy
This is a technique that kills cancer cells. Substances that are introduced into the human body are toxic, but they are the ones that cause the death of malignant cells. If a person has a strong immune system and a small focus of cancer, it is possible to achieve the complete destruction of cancer pathology in any organ, including the intestines.
These are strong drugs that often have strong side effects on important internal organs, primarily the liver and kidneys. In general, their effect on healthy organs is quite gentle; today this is the most common therapeutic technique in oncology.
However, when treating colon affected by cancer, chemotherapy is always used as part of a combination treatment. Surgery is always performed in this case, as it is the only way to save the patient’s life.
The doctor first looks to see if surgery can be performed. If this cannot be done immediately, then chemotherapy is prescribed, after which resection is performed. Then, depending on what the condition is after removal of the intestinal tumor , such treatment is prescribed or not prescribed.
The main side effect of chemotherapy is loss of nail plates and damage to hair follicles. Patients' hair falls out after chemotherapy. Also, side effects due to general intoxication may include nausea, vomiting, dizziness and loss of strength.
There are different types of drugs that are related to chemotherapy:
- anticancer antibiotics;
- hormonal drugs;
- immunosuppressants;
- alkaloids and other cytostatic drugs that are prescribed for intestinal oncology at all stages of the tumor in combination treatment and as independent therapy after surgery.
Chemotherapy may be given before surgery to shrink the tumor and stop its growth, and may also be given after surgery. Often, the use of such drugs is combined with radiation exposure, which results in effective treatment and a favorable prognosis. The use of combined or simple treatment methods will determine what the condition will be after removal of an intestinal tumor.
Preparing for surgery
Before each intestinal resection, the patient must undergo special preparation. This is a special organ that requires preliminary cleaning before surgery. A large number of microflora live in it, including pathogenic ones. Only in emergency cases, a limited amount of preparatory measures are carried out.
Due to preparation, it is possible to avoid sepsis and infectious complications . The intestines contain a lot of microflora, including pathogenic ones. You need to get rid of it before removing the tumor.
The intestines must be cleaned with liquids, enemas and special diets. Before the operation itself, food intake is stopped 12 hours. Later, the amount of fluid is limited. Before removal, the patient is prescribed antibiotics for complete sanitation of the peritoneum and rectum.
If the patient is taking anti-inflammatory drugs, the doctor should be told about this. You should stop taking such drugs before surgery, as they can cause bleeding. The specialist explains to the patient the reason for withdrawal and tells what the condition may be after removal of an intestinal tumor if you do not stop taking non-steroidal medications, including aspirin.
Indications for intestinal surgery are:
- benign and malignant neoplasms;
- gangrene;
- obstruction;
- adhesions;
- developmental anomalies of this organ;
- diverticulitis;
- volvulus.
Resection is not performed if there are:
- high risk of surgical intervention;
- terminal states when a person dies;
- coma;
- advanced cancer with metastases.
Doctors always begin operating on the intestines when they detect a tumor and mesenteric thrombosis in a patient . In the first case, the operation is not performed urgently. When the intestines are affected by cancer , the patient is first prepared for surgery, which may include chemotherapy and radiation as a complex treatment. Surgery can be performed in this case only after a certain period after diagnosis.
In case of thrombosis, immediate resection is performed, because ischemia and necrosis of the intestinal wall cause severe intoxication. Without surgical intervention, in this case, peritonitis may develop, followed by the death of the patient as a result of general blood poisoning. In this case, there is no time for preparation and diagnostics.
The structure of the rectum - a little anatomy
The rectum is a part of the digestive tract that, unlike other parts of the tract, has no bends.
It has three parts:
- anal;
- ampullary;
- supramullary.
The large intestine connects the small intestine to the anus and includes the colon and rectum. The colon has a connecting function; it connects the small intestine with the rectum.
The latter consists of the mucous membrane and submucosal layer. The length of the organ on which the malignant neoplasm of the rectum actually appears reaches 15-20 cm.
Features of surgical methods
Treatment of patients with cancer is carried out using surgery. In the early stages of the pathology, when its size does not exceed 30% of the circumference of the intestine, doctors remove a small affected part of the organ, trying to preserve its functionality as much as possible.
When the pathology affects the intestine in the middle or lower sections, complete resection is most often performed. In this case, the patient is deprived of a natural opening through which emptying occurs. The surgeon takes part of the colon out to drain the intestine. As a result, the patient experiences a change in his usual style and quality of life. He is prescribed a special regimen that he will have to adhere to for the rest of his life:
- strict diet;
- using the bone as an anus;
- the colon performs the functions of accumulating and retaining feces, which were previously performed by the rectum.
Surgical intervention can be performed using laparoscopy with minimal trauma in the form of a puncture of the peritoneum, or in the form of open access through an incision in the abdominal cavity. The choice of surgical technique also directly determines the condition after removal of an intestinal tumor.
If the cancer is stage 2-3, chemotherapy options are used. If the tumor has become motionless and has grown into neighboring organs and tissues, then its removal is impossible. First, the patient needs to undergo radiation and chemical therapy. the tumor can be removed surgically. If surgery is not possible, palliative therapy is prescribed and radiation therapy is continued. The use of chemotherapy continues for a certain period of time, since long-term use of drugs can completely damage blood vessels, liver and kidneys.
After removal, during the recovery period, doctors try to bring the metabolism back to normal in order to avoid exhaustion of the body, weakened by cancer and treatment, from a lack of nutrients.
After surgery, which is always dangerous, the patient often experiences various complications:
- pain;
- bleeding;
- the formation of a hole in the wall of the colon;
- intestinal obstruction.
The characteristics of complications also directly determine what the condition will be after removal of an intestinal tumor. The doctor observes such a patient continuously for 2 years. Then examinations are carried out once a year, sending the patient for a comprehensive diagnosis.
Features of the postoperative period
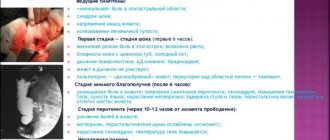
Time is needed for complete healing of the damaged cavity and fistula tracts. The stages of the postoperative period are divided into inpatient and outpatient.
The first part of recovery is when the patient is placed in a hospital for observation. A tube is installed to remove gases, analgesics and antibiotics are prescribed. Bandaging is carried out several times a day.
12 hours after the operation, you are allowed to eat food , always finely ground. Frequent fluid intake is recommended. In 90% of cases, baths are prescribed, to which an antiseptic solution and ointments are added for pain relief. If necessary, laxatives and other required substances. In the hospital, the patient is detained for the time required for partial restoration of functions and wound healing.
Benefits of laparoscopy
Colon surgery can be performed using laparoscopy. This is an operation in which the surgeon creates several puncture holes for the introduction of special instruments. After it, the patient recovers faster because he loses less blood. The type of operation chosen directly determines the condition after removal of an intestinal tumor.
But in some cases it is not technically feasible; sometimes for some patients it is safer to use an open technique.
During laparoscopy, instruments are inserted into the abdomen through punctures, and carbon dioxide is injected to improve visibility. After this, having discovered a tumor, the surgeon clamps the intestine above and below the location of the pathology, suturing the mesenteric vessels and removing the intestine affected by cancer.
About the technique of small intestine resection
The excision is done under general anesthesia so that the person does not feel pain and has an easier time undergoing the operation. There are 2 methods of performing the procedure: the first is open (the abdomen is completely cut), the second is laparoscopic (the specialist makes several small incisions into which cameras, light and the necessary sterile instruments are inserted).
The first method is classic and is rarely used. The second method of resection of the small intestine is new; it leaves no scars or scars. Other advantages of laparoscopy include: minimal risk of infection, much shorter postoperative period, less painful recovery process.
Step-by-step laparoscopic surgery:
- the patient is given intravenous anesthesia and other sedatives;
- A large needle is inserted into the abdominal area, through which the abdomen is filled with carbon dioxide (this is necessary so that the abdominal cavity enlarges and the procedure is easier to carry out);
- the specialist makes 4 to 6 incisions in the abdomen (a camera with an illuminating flashlight is inserted into one of the holes, and instruments are inserted into the others, for example, clamps, a scalpel and scissors);
- a section of the injured intestine is cut off, the resulting ends are stitched with a needle and thread or connected with special staples;
- the cut areas are lubricated with iodonate;
- All instruments are removed, gas is pumped out, incisions are sutured and a sterile dressing is applied.
The surgical intervention lasts from 2 to 3 hours. It happens that during the operation the surgeon can switch from laparoscopy to open (classical) resection.
In what cases is open surgery performed?
This method is most often chosen due to the risk of gangrene and extensive blood poisoning. Necrotic lesions result from atherosclerosis of the arteries in the peritoneum. It is necessary to remove such pathology using laparotomy in cases where it is large, or it is technically impossible to perform a closed operation.
With this method, the surgeon cuts the peritoneal wall into several centimeters. Laparotomy has a number of advantages:
- a good overview of the organs is created for more precise manipulations with them;
- high precision of manipulation, allowing removal of the organ within healthy tissue to prevent recurrent tumor formation;
- the possibility of performing it in any hospital, since most oncologist surgeons are fluent in laparotomy.
When performing laparotomy on a tumor-affected intestine, the surgeon needs to remove the damaged area of the organ as carefully as possible so as not to provoke the development of necrosis again. This is one of the main factors influencing the condition after removal of an intestinal tumor. If there is a tumor in the intestine, a colostomy is created to remove feces, which can remain forever, or after a few months it is removed to restore continuous bowel movement. This is a complex medical procedure performed under general anesthesia over several hours.
To reduce the risk of infection of nearby tissues with intestinal contents during surgery, nurses isolate them with napkins and tampons. It is practiced to change tools when moving from a more “dirty” stage to the next one.
The operation to remove the tumor is completed by washing the abdominal cavity, layer-by-layer suturing of the abdominal tissue and installing drainage tubes for the outflow of discharge.
Outpatient period
- The fistula takes a long time to heal, and the discharge does not stop for 3 to 5 weeks. It is recommended not to stop taking sitz baths at the end of the outpatient period or leaving the hospital. Carry out procedures in the morning and evening with the addition of prescribed medicinal infusions and antiseptic drugs. The wound should be covered with sterile bandages and lubricated with disinfecting ointments. Baths are also taken after the next bowel movement.
A mandatory measure if the rectum is susceptible to disease is diet. The patient consumes the required amount of fluid to soften stool and fiber. Spicy foods and alcohol are excluded. It is not recommended to sit/stand for long periods of time. Doing heavy physical work or lifting any heavy objects is prohibited.
- Any violation of the regime provokes wound opening and prolonged healing. Recommendations are described by the attending physician - proctologist.
- After some time (usually a day), the patient is allowed to drink water. After anesthesia, unusual sensations occur in the body, sometimes severe pain. For the first few days, the patient takes a course of painkillers.
- After the first dressing they are removed. Dressing is a painful procedure for the patient. Locally acting drugs on the body are required. The attending physician controls the healing: the edges of the wound should not stick together, there should be no accumulation of suppuration or non-drainable pockets.
- If the operation was complex, after a few days it becomes necessary to change the dressing under anesthesia. A deep treatment of the operation site is performed, and the ligature is tightened. To make the wound heal faster, baths with potassium permanganate or chamomile are performed.
How the intestines are connected after removal of a cancerous tumor
After removing the tumor, you need to connect the ends of the intestine. If the ends cannot be connected, the patient has an outlet placed on the abdominal wall.
If it is possible to connect the ends of the intestine after surgery, they can be connected:
- end to end;
- side to side, when the opposite ends of the intestine are connected by their lateral surfaces;
- side to end. This is how sections of the intestine that differ in anatomical characteristics are connected.
Surgeons can, in some cases, create a temporary or permanent overlay of the outlet on the anterior wall of the abdomen. This also determines what the condition will be after removal of an intestinal tumor.
This connection is called a colostomy. With its help, feces will be removed from the intestines on a temporary or permanent basis.
Features of intestinal surgery
This surgery is different from operations on other parts. This is due to the peculiarities of the structure and location of the organ, firmly fixed in the pelvis and close to the organs of the genitourinary system, as well as the functional characteristics of the rectum, which removes feces from the body. The other part of the colon cannot perform this function.
Surgery on the rectum affected by cancer is technically more complex and produces more complications and unfavorable outcomes than removal of a tumor in the thin or thick section. This also affects the condition after removal of an intestinal tumor.
The difficulty of operating on the rectum is that the doctor seeks to preserve the natural opening for bowel movements. After removing the affected part of the intestine, he creates a connection that is as similar as possible to the anatomy of the anus. If you have to remove all the components of the anal canal, then you have to do plastic surgery of this segment of the intestine after removing its part affected by cancer.
Such surgical intervention, leading to the removal of the anus, is performed today in rare cases when there are no other ways to fight for the patient’s life. If malignant neoplasms have not penetrated into the nearby tissues of the anal sphincter, then the natural opening is preserved. Laparotomy on the rectum is always performed under general anesthesia. It always ends with the installation of drains in the pelvis. In this case, it is important for the doctor to know what the condition is after removal of an intestinal tumor in severe patients in order to choose supportive treatment and prolong their life.
Menu after surgery
After bougienage of the rectum, maintaining proper nutrition allows you to achieve maximum results from the procedure. This technique is carried out using a specialized instrument - bougie. A bougie is inserted into the anus to expand the intestine. Its narrowing due to proven surgical intervention is the main indication for the procedure. Bougienage allows you to expand the anal canal and prevent it from narrowing again. The procedure is carried out for the purpose of diagnosis and treatment to facilitate the process of defecation.
To speed up the recovery process of the rectum, experts have compiled an approximate diet for a week.
- breakfast – fresh non-acidic fruits;
- afternoon snack - an omelet with a small amount of cabbage, tea is suitable as a drink;
- lunch - chicken puree soup without fatty broth, vegetable salad with vegetable oil, some bread and herbal tea are acceptable;
- dinner – buckwheat porridge boiled in water, black tea;
- second dinner - for the normal functioning of the rectum you need to eat yogurt.
- breakfast - berries combined with crackers made from wheat flour;
- afternoon snack – rice porridge cooked in water with the addition of dried apricots, weak black tea;
- lunch - cabbage-based vegetable soup, boiled chicken and weak tea with milk;
- dinner – barley porridge and cottage cheese (can be replaced with fermented baked milk or sour cream);
- second dinner - yogurt or one-day kefir.
- breakfast – juice based on vegetables or fruits;
- afternoon snack - any porridge with low-fat milk;
- lunch – vegetable-based puree soup, baked turkey with potatoes and fruit juice;
- dinner – vegetable salad and fresh juice;
- second dinner - fermented milk product.
- breakfast – half a glass of carrot juice;
- afternoon snack – porridge cooked in water, tea with milk;
- lunch - low-fat broth soup with chicken meatballs, boiled fish, vegetable salad and herbal tea;
- dinner – cheesecakes or cottage cheese casserole, cranberry juice;
- second dinner - yogurt or fresh fruit.
- breakfast – juice from fresh vegetables;
- afternoon snack – millet porridge on water with the addition of prunes, herbal tea;
- lunch - cabbage soup in low-fat broth, vegetable salad and herbal tea;
- dinner – baked fish with rice, berry juice;
- second dinner - yogurt.
Survival rate after tumor removal
For patients who have had a cancerous colon or rectum removed, survival after surgery directly depends on how quickly they seek medical help.
Survival is a medical indicator of the effectiveness of the chosen treatment technique in oncology. Prognosis always depends on the depth of tissue damage and the presence of metastases in the lymph nodes.
Those who begin treatment for colon cancer at an early stage live the longest after surgery. Oncologists predict a 5-year survival rate for them in 90% of patients.
Even in the presence of metastases in the lungs and liver, with timely chemotherapy and surgical treatment of the tumor, patients can gain an additional 5 years of life in 30-50%. On average, for patients who become ill for the first time, the prognosis for survival is one year for 46% and five years for 54%.
Rectal cancer is considered one of the most dangerous oncologies. Removal of a malignant neoplasm in any part of the intestine aims to preserve the patient’s life. After it, his usual life changes forever. A person will have to change his habits, hobbies, and adapt his entire life to the work of the body. To prevent the recurrence of a tumor, the patient must undergo regular examinations and follow the recommendations of doctors. All patients with this pathology need to know what the condition is after removal of an intestinal tumor in order to psychologically prepare for such changes.
Nutrition in the postoperative period for intestinal oncology should be therapeutic. It makes the digestion process more efficient, strengthening and gradually restoring the role of the intestines. Such patients eat by the hour, according to a certain diet, which helps to empty the body. The menu option is always agreed with the doctor.
Lifespan
How long patients live after surgery for rectal cancer depends on its success and the stage at which the disease was detected.
If surgery was performed without complications, with correct treatment, life expectancy in 60% of cases exceeds five years.
How long do you live with colorectal cancer?
- It is the first five years after surgery that are the most difficult ; if they are passed, we can say that the disease has been defeated and will no longer affect life expectancy.
- If the disease is detected at stage IV , the patient does not even have this time.
What consequences may occur after removal of bowel cancer?
Cancer of the digestive system, according to modern statistics, ranks first among cancer diseases and the prognosis for such pathology is often unfavorable. Of course, the health and vital activity of the patient depends on the histological structure of the cancer tumor, its location, stage of formation, treatment and postoperative recovery of the patient.
Cancer can affect all organs of the gastrointestinal tract.
The most common type of abdominal cancer is stomach cancer, followed by the esophagus. The latter is distinguished by a severe form of malignant neoplasm with an unfavorable prognosis. With the first and second stages of esophageal cancer after surgical treatment, patients live for about three years. Such a tumor is usually removed by surgery; there are also cases of effective therapy with radiation and chemotherapy. Such treatment is carried out before and after removal, as well as as an independent treatment technique. The most favorable prognosis is observed after combination therapy for esophageal tumors, in which case people live up to five years.
Upper cancer is less common than rectal cancer. Most often, elderly people after fifty years of age suffer from this dangerous pathology. Among patients, a higher percentage falls on older men.
Even with modern technology and compliance with all measures, complications may arise during surgery on the intestine affected by cancer . Its contents contain a large volume of microorganisms that are a source of infection. The most common negative consequences after resection are:
- the appearance of pus in the suture area;
- bleeding;
- peritonitis;
- stenosis of a section of the intestine;
- dyspeptic disorders.
Often patients have a question about what happens after removal of an intestinal tumor. The doctor will describe in detail his individual condition before the operation and tell him about possible complications, which are always individual.
Recovery after surgery depends on the complexity of the operation and the general condition of the person, and his compliance with doctors’ recommendations. In addition to generally accepted measures, including proper hygiene of the postoperative wound, early activation, in such pathology the diet and diet of the patient play an important role.
Causes of tumors in the intestine
A predisposition to pathological degeneration of the cellular tissue of the intestinal mucosa can develop after exposure to carcinogenic substances that enter the human body along with food. They are found in fried foods, smoked products and synthetic additives, substitutes for natural taste, smell and color. All this negatively affects the digestive process, the functioning of the stomach and intestines. A monotonous and unbalanced diet, weight loss diets can also be a factor in the development of inflammatory processes in the intestines that degenerate into cancer. The cause of a malignant neoplasm can be constant poisoning with surrogate alcohol and drugs, as well as poisoning with drugs and poor-quality food.
Those people who work in hazardous industries are also at high risk. Constant exposure to carcinogens can lead to the development of cancer.
Intestinal cancer can develop with frequent congestion, constipation and slag deposits on the walls of the intestinal canals. Long-term constipation increases the risk by negatively affecting the intestinal wall. The cause of the development of oncology can be infectious diseases and inflammatory processes in different parts of the intestine such as stomach ulcers, gastritis and other pathologies of infectious etiology.
Cancer can affect the intestine as a result of the formation of postoperative scars, polyps and other pathological changes. You can get colon cancer if you have a genetic predisposition.
Recovery after removal of intestinal cancer
The recovery of a patient after surgery on the intestines for cancer takes a long period. The function of the digestive tract, represented by a complex biochemical process, is disrupted as a result of surgical intervention. Therefore, it is difficult to improve the functioning of the intestines after removing part of it. The main role in this is played by nutrition, which should be dietary.
After intestinal surgery, you need to eat easily digestible foods that replenish minerals, vitamins, protein and other enzymes to increase hemoglobin and the body's protective properties. On the first day after surgery, the patient should drink more fluids and not eat.
After 3-4 days, the menu can include weak tea or compote of dried fruits, chicken broth, rice water, fruit jelly, pureed liquid porridge and hemoglobin-increasing rosehip infusion. The amount of food will depend on the condition after removal of the intestinal tumor in a particular patient.
On days 5-6, you can eat steamed meat and fish, and certain types of vegetable puree. The attending doctor must regulate and monitor the patient’s diet, determining the stages of restoration of intestinal function.
All patients who have undergone anti-cancer treatment and rehabilitation are registered in oncology centers, and every six months they undergo preventive examinations in order to exclude recurrence of the malignant process.
General information about the diet
Main indications for intestinal surgery:
- Detection of rectal fistula.
- Crohn's disease.
- Intestinal ischemia.
- Paraproctitis and diverticulitis.
- Injuries of the rectum and sigmoid colon.
- Oncology.
- Acute inflammatory processes.
- Hemorrhoids, fissures.
The operation is not prescribed in every case: for example, if the intestines begin to whistle, drug therapy is first prescribed. If medications are not effective, resection is used. The specifics of nutrition and care after surgery are determined by its complexity and the patient’s health status.
Principles of diet after surgery:
- You should avoid foods that cause flatulence, diarrhea or constipation.
- During the first three days, the patient is fed intravenously. If the resection was extensive, parenteral nutrition will last several weeks.
- Natural nutrition begins with treatment table No. 0, gradually moving to table No. 1a, 1b. After 1.5-2 months to table No. 15.
- For the first 15 days after surgery, you should not eat fresh vegetables, eggs, milk or legumes.
- From the diet we exclude canned food, pickles, marinades, spices, fatty meats, rich broths, and sausages. You also need to give up foods with flavor enhancers, fast food, processed foods, mushrooms, baked goods, sweets, sauces and mayonnaise.
- At first, we grind all the products in a blender or grate them - this way the food is better absorbed.
- The diet provides for fractional meals: 5-6 times a day.
- Food can be steamed, boiled or baked (but not until golden brown).
- To prevent constipation, you need fiber: these are vegetables (pumpkin, carrots, zucchini, cauliflower, etc.) and fruits (apple, banana, pear). Citrus fruits and berries with rough skin should be avoided for a while.
- The preferred meats are turkey, veal, chicken, and rabbit.
- To avoid increased gas formation, cabbage, legumes, white bread and pastries, and carbonated drinks are excluded from the diet.
- If a person suffers from constipation, it is worth giving up hard-boiled eggs, white rice, strong tea, pomegranates, and lingonberries.
- Keep your body hydrated: you need to drink at least 2 liters of water per day, in small portions. Fruit drinks, compotes, herbal teas, and vegetable juices diluted with water are also useful.
- Train yourself not to drink food. You can have a tea party only 1.5-2 hours after eating.
- Monitor the temperature of your food: very cold and hot food is harmful to the gastrointestinal tract.
- You can't go hungry. If your body requires it, you can make a healthy snack: vegetable puree, fruit juice, a glass of kefir or acidophilus milk.
Recommendations during the recovery period
Features of the body's recovery are as follows:
- The diet after rectal surgery is primarily aimed at restoring the balance of enzymes.
- Restoration of peristalsis.
- Improving the functions of the gastric mucosa.
- Prevention of complications.
- If necessary, care for the seam.
- Providing necessary and feasible physical activity.
We would like to immediately make a reservation that proper nutrition after rectal surgery is not enough. The doctor must prescribe medications that can prevent possible complications. Neuroleptics, immunomodulators, biological products, enzymes, painkillers, antibiotics and others can only be taken after consultation with a specialist. Physical rehabilitation is no less important: it helps improve blood circulation, tone of the muscle group and abdominal tissue. Some exercises can be performed as early as 2-3 weeks after surgery. In particular, breathing exercises help improve peristalsis and reduce intra-abdominal pressure.
Do not forget about timely examinations: x-rays, colonoscopy, ultrasound. It is mandatory to take tests in order to notice a relapse in time. There may be problems with stool for some time, but if you follow the diet, the situation will stabilize. The intestine has a good feature: in the absence of a specific section, the functions it performs are distributed among neighboring ones.
Indicative menu for the week
Ideally, the diet should be prescribed by the attending physician (photo: www.zhenskiy.club)
| Day of the week | Diet |
| 1st | For breakfast: 1 soft-boiled egg. For second breakfast: low-fat cottage cheese (120g). For lunch: vegetable puree soup (180g), boiled chicken (50g). Afternoon snack: banana. For dinner: pumpkin puree (80g), steamed meatballs (80g) |
| 2nd | For breakfast: oatmeal (100g). For second breakfast: baked apples (80g). For lunch: rice soup (180g), chicken cutlet (80g). For an afternoon snack: rosehip decoction with crackers. For dinner: mashed potato soup with broth (150g) |
| 3rd | For breakfast: 2 egg omelet. For second breakfast: applesauce (80g). For lunch: cauliflower soup (180g), boiled beef (80g). Afternoon snack: banana. For dinner: rice porridge (80g), chicken (80g). |
| 4th | For breakfast: buckwheat porridge (120g). For second breakfast: a piece of hard mild cheese (40g), biscuits. For lunch: fish soup (200g), a slice of whole grain bread (40g). For afternoon snack: baked apples (100g). For dinner: mashed potatoes (100g), boiled fish (80g) |
| 5th | For breakfast: chicken soufflé (120g). For second breakfast: banana. For lunch: puree soup with meatballs (200g). For afternoon snack: carrot puree with apple (120g). For dinner: zucchini puree with cheese (140g). |
| 6th | For breakfast: viscous barley porridge (200g). For second breakfast: fruit compote with crackers. For lunch: broccoli puree (80g), boiled fish (100g). Afternoon snack: yogurt. For dinner: chicken cutlet (80g), mashed potatoes (80g) |
| 7th | For breakfast: semolina porridge (140g). For second breakfast: grated apple (80g). For lunch: noodle soup (200g), boiled meat of your choice (80g). For an afternoon snack: cocoa, a piece of bread (40g). For dinner: rice porridge (100g), meatballs (80g) |
Taking anti-cancer drugs
Drug treatment for cancer uses drugs that destroy cancer cells and metastases. Chemotherapy is prescribed only in the first stages of oncology as an independent method of removing a tumor from the intestine, or as an additional treatment after surgery. The course of chemotherapy lasts 2-3 months, sometimes six months, and includes alternating the administration of anti-cancer drugs with a period of recovery of the body.
For its purpose, the characteristics of the tumor are important:
- size;
- dynamics of increase and development;
- presence of metastases;
- the degree of damage to the lymph nodes;
- hormonal background.
Chemotherapy helps make a malignant tumor operable. In this case, it is prescribed before surgery.
When conducting it, the individual characteristics of the patient, his age, gender, chronic diseases, and general condition of the body are taken into account. The doctor assesses the risk of side effects and complications. A responsible decision must be made about whether the risk is worth it and whether the treatment will be effective.
Indications for prescribing chemotherapy are:
- malignant neoplasms that become operable after a course of chemotherapy;
- prevention of metastases;
- the ability to make cancer operable.
All this is revealed at the stage of preoperative diagnosis.
Types of medications used
Most often, chemotherapy is used in combination treatment, which determines what the condition will be after removal of an intestinal tumor.
It is prescribed to remove metastases and prevent the appearance of secondary malignant neoplasms.
Chemotherapy drugs are prescribed as intravenous injections. The most commonly used drug is 5-fluorouracil, which is injected into a vein. This type of injection causes severe pain; special medical equipment is used to reduce pain.
Complex therapy for oncology also includes taking vitamins and Levamisole, which helps support the patient’s immune system. Treatment can take from several weeks to six months.
Cancer therapy is carried out both before and after surgery. In the preparatory period for the operation, it is needed in order for the following to happen:
- stopping the growth of a malignant neoplasm ;
- reduction in tumor size;
- elimination or reduction of metastases.
After resection, preventive therapy is necessary.
Surgery does not guarantee complete disappearance of cancer. Diseased cells can remain in the lymph nodes, where they are very difficult to detect even with modern diagnostics. After surgery they may begin to grow again. To avoid this, chemotherapy and examination by oncologists are prescribed. Courses of chemotherapy and radiation last a short period. After this, the body recovers, the doctor conducts an examination and decides on further treatment.
After any oncological resection associated with the removal of a tumor in the intestine, preventive therapy is carried out. Only in this case can a high percentage of patient survival and prolongation of their lives be achieved.