Today, kidney disease is a very pressing problem. According to statistical observations, the number of people with problems of the urinary system increases significantly compared to the general incidence.
There are anomalies when there are more than two kidneys; this defect is called complete or incomplete doubling of the kidneys.
Contours and size of the organ
In an adult, the normal organ size is as follows:
- thickness - 4−5 cm;
- width - 5−6 cm;
- length - 10−12 cm.
Information on the thickness and structure of the renal parenchyma
It is important! This parameter characterizes the part of the organ responsible for urine formation (functional part). Normally, the thickness of the parenchyma varies between 18–25 mm. An increase in these parameters may indicate inflammation or swelling of the organ; a decrease indicates dystrophic changes.
It is important!
This parameter is necessary to assess the condition of organs, with which you can study the structure of the renal parenchyma.
In order to have an idea of whether changes in the parenchyma are present or absent, it is necessary to determine what echogenicity is, the concept of normal echogenicity, and to get an idea of the reduced and increased echogenicity of the kidneys.
It is important!
Echogenicity must be understood as an ultrasound diagnostic term that is used by qualified specialists to describe the structure of the parenchyma of any organs, in this case the kidneys.
We can say that echogenicity is a property of tissue that characterizes the propagation of sound waves in them. Ultrasound can reflect differently from different tissues. The intensity of the reflection of sound waves directly depends on the density of the tissues, the image will look lighter, and for fabrics with low density the image will be slightly darker.
Healthy organ tissue has its own echogenicity, which is considered normal. It is homogeneous. If the image from the ultrasound signal is slightly lighter than normal, the echogenicity of the renal parenchyma is increased. Such phenomena are observed during tissue compaction, for example, during sclerotic processes in the kidneys and glomerulonephritis. Hyperechogenicity can be divided into homogeneous and heterogeneous. (alternating areas of hyperechoic normal tissue).
Information about the causes of increased echogenicity of the kidneys:
- Presence of diabetic nephropathy;
- chronic pyelonephritis.
- organ damage due to arterial hypertension;
- presence of glomerulonephritis;
- amyloidosis;
- the presence of individual hyperechoic areas may indicate the presence of benign or malignant neoplasms;
- the presence of other sclerotic processes.
In cases where the fetus has increased echogenicity of the kidneys, this indicates congenital kidney pathologies.
Now, having discovered in your conclusion the previously unfamiliar term echogenicity, you will not be at a loss. And all because after reading this article you have closed for yourself a previously unknown page of medicine.
Kidney parenchyma is the specific tissue of the organ that surrounds it. This is a kind of cellular “shield” and “filter”, thanks to which the organ is able to recover from numerous diseases and pathologies.
Parenchyma is a specific connective tissue surrounding the kidney. It performs the main function of this organ - maintaining fluid balance in the human body. It is thanks to this group of cells that the organ is capable of regeneration. Nevertheless, the kidney parenchyma is susceptible to frequent diseases, which leads to pathological transformations in the organ.
Structure and functions of tissue
The renal parenchyma is the main tissue of the kidney. The parenchymal layer performs such an important function as ensuring water-electrolyte balance in the human body, purifying the blood, and is directly involved in metabolic processes and the removal of metabolic products.
Its most important indicator is thickness; it is used to determine the performance of the organ. The thickness of this layer, even if the kidneys are normal, may vary depending on age.
Normally, the thickness of the kidney parenchyma can range from 14 to 26 mm; in old age, its size decreases to 10-11 mm. This fabric consists of two main layers:
- Cortical. This is the outer layer that is located under the capsule. The cortex contains a huge number of glomeruli and tubules (nephrons), where urine is formed. Each of these nephrons of the parenchyma is associated with many vessels. It is estimated that there are about a million of them, but only a third of them are used.
- Cerebral. It also plays an important role in the human urinary system. From the cortical layer, primary urine enters the cerebral layer, where the process of reabsorption (reverse absorption) occurs, resulting in the formation of secondary urine, which enters the renal cups and pelvis, which passes into the ureter. There is no clear boundary between these two layers.
It must be remembered that parenchyma tissue has a unique ability to recover, so timely therapy can completely restore the functioning of the organ. It is also worth noting that the recovery process largely depends on the metabolism and state of the patient’s immune system.
Diagnostic measures
Initially, parenchymal tissues are assessed by a physician using ultrasound. The main diagnostic sign of diffuse changes in the parenchyma is the changed size (thickening/reduction) of certain areas. Using a radioisotope examination, the doctor determines the condition of the borders of the kidney, whether it has moderate and clear outlines or wavy, and whether there is any asymmetry. With kidney damage, the patient has constant pain in the lower back (on the affected side - the left kidney or the right) and it is painful for him to urinate, and swelling of the lower extremities persists for a long time. In urine tests, the protein concentration will be higher than normal. To obtain more detailed information, the patient undergoes CT and magnetic resonance imaging (MRI).
Using ultrasound, diffuse changes in the parenchyma can be assessed.
The characteristics listed above appear when the parenchyma capsules are stretched. This occurs due to significant renal hyperplasia. Cysts are another cause of these symptoms because they compress blood vessels, thereby blocking them. If diffuse changes or cystic lesions are in advanced form, the patient requires urgent hospitalization. When ultrasound reveals hyperplasia of the renal parenchyma, which is not associated with congenital characteristics of a person, this indicates the presence of calcifications in the cavity or sinuses of the organ.
Echogenicity
The echogenicity of the kidneys is determined using ultrasound. If this parameter is elevated, this symptom indicates:
- early stage of development of the inflammatory process or incorrect and unproductive therapy for kidney disease;
- metabolic disorders, problems in the functioning of the endocrine system;
- advanced form of glomerulonephritis and other diseases.
If the diagnosis mentions “echoic formations,” it means that sand, its accumulations or stones were found in the organ cavity. The level of echogenicity directly depends on the type of stones. In a healthy state, the echogenicity of the kidneys on ultrasound will be within normal limits, and the renal structure will be homogeneous. When this research is uninformative, other methods are resorted to.
Diffuse changes
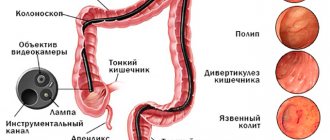
These disorders are changes in the size and structure of the organ noticeable on ultrasound; their main types include:
- exhaustion. The thickness of the kidney parenchyma less than 16 mm at a young age indicates the development of pathological processes, most often of an infectious and inflammatory nature. In this condition, the organ is unable to function normally and immediate treatment is necessary. If a violation of the tissue structure in the direction of exhaustion is diagnosed in patients over 60 years of age, then this condition is acceptable and can be considered the norm;
- thickening of tissues. Diffuse changes in the kidneys, in which tissue thickness of more than 25 mm is observed, most often indicate the formation of various neoplasms or cysts of the renal parenchyma. Also, this condition can provoke an acute inflammatory process that develops an abscess and thrombosis;
- disturbance of echogenicity. The concept of “renal echogenicity” characterizes how kidney tissue transmits ultrasound. If the kidney parenchyma is normal, its structure on ultrasound should be homogeneous; in the event of pathologies, this indicator may increase or decrease. This mostly occurs due to inflammation or the development of swelling;
- disturbances in arterial blood flow;
- fluid accumulation;
- presence of organ asymmetry.
One of the rare pathological changes in the renal parenchyma is the complete or partial death of cortical tissue.
This condition is called cortical necrosis and can occur at any age. Its cause may be bacterial sepsis or blood poisoning due to uterine bleeding, certain poisonings, etc.
Diffuse changes in almost 90% of cases indicate the development of some kind of kidney disease, which requires accurate diagnosis and timely therapy.
Meanings of the term
The term parenchyma can have two interpretations. If we are talking about plant parenchyma, then we are talking about homogeneous accumulations of soft tissues in the plant body, which fill the space between other tissues and serve to accumulate water and nutrients, as well as to support the plant stem.
If we talk about the parenchyma of animals, then we are talking about the tissue that makes up the main part of most organs and is responsible for their normal functioning. The parenchyma of the kidneys, liver, thyroid gland and other organs is especially often mentioned in medical articles.
Reasons for structural changes
Experts have proven that the most common causes of diffuse changes in kidney tissue are:
- Calcifications. These are kidney stones that form due to poor nutrition, improper metabolism, and other disorders. Such formations cause serious illnesses that can manifest with various symptoms and cause serious complications. The appearance of sand or stones delays the outflow of urine, provokes inflammation or the appearance of renal colic.
- Cyst. One of the common causes of changes is the formation of cysts that occur on both the right and left kidneys. When fluid is retained in the nephrons, a simple or solitary cyst often forms. In simple cases, a thin-walled oval or round formation develops, containing hemorrhagic or serous fluid. The size of such formations can be from 8 to 10 cm, and occasionally large ones can be found, which can contain about 10 liters of liquid. When the cyst is eliminated, the organ is restored and a rapid recovery occurs. Cystic-dysplastic changes provoke the formation of a multilocular cyst, which has the appearance of a multi-chamber formation with clearly defined outlines. The main problem with such formations is that they can become malignant.
- Tumor processes. The formation of a tumor even in one kidney will stop due to serious changes in the structure of the organ. This process can be either benign or malignant. To understand the nature of the formation, you need to undergo the necessary examination.
- The presence of pathologies of an infectious nature (pyelonephritis, pyelitis, etc.). With such ailments, especially in chronic form, the kidneys are most often depleted; prolonged inflammation leads to a decrease in the area of the kidney parenchyma, which significantly affects the functioning of the organ.
- A change in the echogenicity of kidney tissue is a sign of the development of pathologies such as glomerulonephritis, chronic renal failure, nephropathy as a result of diabetes, various inflammations, and disruptions in metabolic processes.
- Chronic kidney disease (nephritis, urolithiasis, etc.)
- Certain diseases of the endocrine system. Ailments such as thyrotoxicosis and disorders associated with the pancreas contribute to the thinning of the kidney parenchyma, followed by its atrophy.
In addition, pathological disorders in the structure of tissues can be caused by age-related changes, hereditary diseases, incorrectly prescribed therapy, the consequences of past illnesses, and in children - congenital anomalies that tend to develop rapidly and therefore pose a serious danger.
Pancreas
A person has organs that consist of internal filling (parenchyma) and connecting (stroma). Its basis is glands, divided into particles by connective tissue. All this is in a special “bag”. Its functions:
- Production of enzymes for the digestive system (gland juice).
- Hormones (insulin) enter the bloodstream and take part in all body processes.
Diffuse changes
It is monotonous in its composition. Inflammations and infections modify its structure, and connective and adipose tissue appears. The cause of diffuse transformations of the pancreatic parenchyma can be:
- Increased blood sugar.
- Inflammation of the gland.
- Diseases of nearby organs (liver, gall bladder).
- Various neoplasms and tumors.
- Uncontrolled consumption of alcohol and nicotine, unbalanced diet.
- Stressful situations, overwork, fatigue.
- Genetic failures. Age.
Echogenicity
- Normally, the parenchyma is homogeneous during ultrasound examination.
- There should not be any formations in it.
- Clear shape with smooth contour.
- Size - 35/30/25 mm.
- The length of the duct is about 2 mm.
If there is an increase in volume and uneven edges, we can talk about a low-quality tumor. Increased obstruction is inflammation of the duct (chronic pancreatitis).
Echogenicity is increased. As the indicators increase, the organ seems to thicken, moisture leaves it, and various formations appear in the tissues - fibromas, lipomas, tumors. Moderate diffuse changes, a decreased rate, indicate an inflammatory process or tissue swelling. The principle of echogenicity is the reflection of ultrasonic waves. Its indicator depends on the amount of liquid.
Homogeneity of the gland. Diffuse changes in the pancreatic parenchyma can manifest themselves in its composition. Enlargement of the organ, blurred edges, heterogeneity are signs of severe inflammation.
It causes diffuse hardening and the formation of cysts filled with blood or dying cells. Their size is not constant, it changes depending on the swelling. During inflammation, purulent cysts and cancerous tumors appear.
Reactive Changes
The pancreas and bile duct have a single duct. Their parenchymas are closely connected, when inflammation occurs in the liver or gall bladder - this causes allergies, and reactive changes in the composition of the gland occur.
With pancreatitis - impaired enzyme production, pain, diabetic manifestations (increased sugar). Diffuse modifications promote transformations throughout the entire organ, without the appearance of any formations or stones. This is one of the most common manifestations of pancreatic disease.
Signs of diffuse changes in the liver parenchyma
What are the dangers of such modifications? First of all, you need to know that this is a hematopoietic organ, consisting of many small capillaries filled with blood. Bile ducts pass through it, delivering bile.
Organ pathology can be determined by echo signs. They undergo changes over time - this is a constant process. If the functioning of an organ is disrupted under the influence of unfavorable conditions, its cells (hepatocytes) transform their structure.
It begins to accumulate fatty and connective tissue. The composition of the liver changes, dying cells, and other factors can form various cysts and hemangiomas. Signs of hepatomegaly (enlarged liver volume) appear.
Diffuse changes can be pronounced or weak. Minor ones occur during colds and infectious diseases. Signs and symptoms:
- Unpleasant nagging pain in the liver area after eating.
- It protrudes from under the rib, increasing in size.
- Bitter taste in the mouth.
- Skin rashes on the body, yellowing.
- General weakness, irritability.
These signs are a reason to consult a doctor. Changes in the structure of an organ can cause serious illnesses:
- Development of hepatitis of all types.
- Various neoplasms.
- Parasitic infestations.
- Inflammation of the bile ducts (angiocholitis).
- Cirrhosis.
- Steatosis is fatty degeneration of the liver.
Causes of diffuse changes:
- Bad habits. Alcohol, nicotine.
- Unbalanced diet. Fried, smoked, salted food.
- Diabetes of the second type. Hormonal disbalance.
- Constant use of medications.
Our liver is able to cleanse the body of harmful substances, provided they are received within acceptable limits. When poisonous components are constantly supplied, for example alcohol, or in a shock dose (mushroom poisoning), she is not able to cope.
Then the pancreas and liver work in “emergency mode,” causing diffuse transformations of these organs.
Symptoms
If the filtration and excretory functions of an organ are disrupted, this means that pathology of the organ tissue develops. Signs of diffuse disorders can either develop rapidly or increase gradually. For the most part, the following symptoms may indicate this:
- increased body temperature, especially in acute infectious pathologies of the kidneys;
- change in skin color, it acquires a yellowish tint and becomes dry;
- weakness, fatigue, possible headaches;
- impaired urination and changes in urine volume, which may decrease or increase;
- the presence of cutting and burning sensation when emptying the bladder;
- the formation of edema in the face; in certain cases, the arms and legs may swell;
- increased blood pressure, shortness of breath;
- lower back pain, both acute and aching in nature.
If kidney problems are diagnosed during a laboratory test, the urine is diagnosed by a change in its color; most often it is cloudy and dark, with pus or blood appearing in it. Also, decreased echogenicity may indicate fluid accumulation or tumor formation.
Diagnostics
The study of the renal parenchyma is carried out in several ways. Thanks to this, it is possible to identify pathologies of the urinary system, determine the structure and thickness of tissue, the size of organs, as well as some other parameters that make it possible to promptly identify disorders and take the necessary measures.
The most common diagnostic methods include:
- Ultrasound of the kidneys, which determines the size, echogenicity and structure (heterogeneity of kidney tissue). Moreover, using ultrasound, you can determine the presence of stones or neoplasms, as well as signs of inflammation.
- MRI is one of the most informative diagnostic methods and is prescribed for a more in-depth study. With this examination, thickening of the kidney parenchyma, congenital anomalies, pathologies of blood vessels, etc. are easily detected.
- A biopsy with histological examination of tissue is a microscopic examination of tissue, prescribed to identify chronic diseases, malignant tumors, nephrotic syndrome, etc. If there are contraindications, such as blockage of the kidney veins, low blood clotting, arterial aneurysm, the procedure is prohibited.
- In addition to these diagnostic methods that determine the condition of the kidney parenchyma, it is possible to conduct urine and blood tests.
In case of malignant tumors and the presence of metastatic processes, computed tomography of nearby organs and systems is performed as an auxiliary diagnosis.
Specifics
The parenchyma consists of small balls in which urine accumulates. Each kidney contains more than a million of these structural units. In the medulla of the parenchyma there are a lot of very thin pathways that merge with each other, and fluid flows through them into the pelvis and calyces.
Although the parenchyma is the protective layer of the kidneys, it can also be vulnerable. There are a number of diseases in which this tissue begins to change its structure. To detect such changes in time, a person undergoes an ultrasound of the organ, computed tomography or MRI.
If the thickness of the parenchyma exceeds 14-25 mm, then we can talk about the development of the disease.
The age of a person contributes to the thickening of the layer; the older he is, the thicker the layer becomes. In addition, some other reasons can lead to changes in the lining of the kidneys:
- Inflammatory diseases in the kidneys, as well as non-inflammatory diseases.
- Penetration of bacterial and viral infections.
- The appearance of malignant or benign neoplasms.
- Untimely or incorrect treatment of diseases of the urinary system.
- If one of the kidneys is removed or its function is impaired, then the other becomes the only working organ; if it works intensively, the parenchyma can also thicken.
If there are violations, the person most often complains of the following symptoms:
- nausea;
- poor appetite;
- fatigue and dizziness.
Treatment
If decreased kidney activity and changes in their tissues are detected, it is necessary to find out the cause of this condition and begin timely treatment.
This problem is dealt with by a urologist, depending on various pathologies, he determines treatment methods, if necessary, selecting anti-inflammatory, antimicrobial and other drugs necessary to restore the parenchyma.
In more severe cases, in the presence of stones and neoplasms, including cancerous tumors, they resort to surgical intervention in which the neoplasms are excised, causing minimal harm to the patient.
Kidney diseases are serious illnesses that affect the body as a whole. However, correctly prescribed treatment and the patient’s compliance with all doctor’s instructions will help restore their function and quickly recover.