Characteristics of the drug
Pancreatin is a digestive enzyme designed to compensate for the insufficiency of the exocrine function of the pancreas.
The main active ingredient is pancreatin, which includes enzymes - lipase, proteinase, amylase. Thanks to these components, proteins, triglycerides and starch are broken down.
According to the instructions for the drug, the medicine is indicated for chronic pancreatitis, which allows Pancreatin to be taken in diabetes complicated by this disease.
Forecast and general advice
https://www.youtube.com/watch?v=pTAQM7h9Jik
Clinical studies have shown that in order to obtain stable remission in chronic pancreatitis and diabetes, patients must, first of all, eat right. It is also important to drink enough water. It promotes better digestion of food, normalizes water-salt balance and helps remove waste products from the body.
- Pancreas transplantation for diabetes mellitus
- Treatment of blood vessels in the legs for diabetes mellitus - Treatment of diabetes
- Treatment of insulin-dependent diabetes mellitus
- Ayurveda pancreas – “PROYoga” and self-development
Rationale for use
Diabetes mellitus and chronic pancreatitis are interrelated.
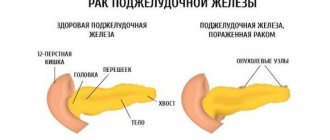
With the loss of exocrine pancreatic function, exocrine insufficiency occurs (enzyme production decreases), which can cause a complication - pancreatogenic diabetes mellitus.
The chronic inflammatory process in pancreatitis leads not only to exocrine insufficiency, but also to the destruction of the islets of Langerans. Exocrine pancreatic insufficiency is especially common in type 2 diabetes mellitus.
Pancreatogenic diabetes is characterized by the following symptoms:
- dyspeptic symptoms;
- pain in the epigastric area;
- increased blood glucose levels;
- skin diseases;
- frequent infections.
The combination of diabetes mellitus and chronic pancreatitis requires a special approach to treatment tactics.
Treatment methods
Due to the fact that the development of diabetes depends on the presence of chronic pancreatitis in the patient, treatment of the disease consists of eliminating the main cause - pancreatitis.
The basis of therapy is a strict diet and adherence to a diet . Drug treatment is complex and involves the use of enzyme preparations. It is recommended to take Pancreatin for type 2 diabetes.
Treatment of pancreatogenic diabetes requires compensation for exocrine pancreatic insufficiency, which can be achieved by using Pancreatin or its analogues: Festal, Mezim, Creon.
The effect of Pancreatin on diabetes mellitus
The administration of enzymes for diabetes mellitus helps:
- improving carbohydrate metabolism;
- stabilization of glycosylated hemoglobin levels;
- increasing glycemic control;
- reducing the risk of developing diabetes complications;
- improving the quality of life of patients and improving their well-being.
According to research by German scientists, Pancreatin therapy for exocrine pancreatic insufficiency in type 2 diabetes can be used together with hypoglycemic agents and does not affect the patient’s glycemic profile. This treatment is considered highly effective and safe.
Signs of the development of “sugar” disease
Pancreatic diabetes is characterized by individual symptoms, by which it can be distinguished from other types of diabetes. First of all, this is a rapid drop in the amount of sugar in the blood fluid, which provokes hypoglycemia. However, diabetic ketoacidosis, caused by a lack of insulin, is not inherent in this form of diabetes.
Damage to medium vessels, large arteries, arterioles and capillaries is a rare occurrence than in type 1 and type 2 diabetes. At the beginning of the development of diabetes, tablets that help lower blood sugar levels are still quite effective. As the disease progresses, they lose their medicinal power, so there is no point in taking them, and the need for insulin therapy is low.
Rehabilitation treatment is carried out with medications belonging to the sulfonylurea group, dietary nutrition and physical exercise.
In the event of type 2 diabetes, the pancreas undergoes extremely serious modifications, and it is possible to observe such an anomaly as deformation of the islets of Langerans, which entails a decrease in the size of endocrine cells and many of them die.
Next, 2 versions of modifications in the cells of the pancreas can be observed:
- Development of pancreatitis.
- Absolute cessation of pancreatic function.
This is explained by the fact that in those areas where the cells have died, the growth of connective tissue occurs, which inhibits healthy cells, contributing to their death.
Use
If you have diabetes, you should drink Pancreatin in strict accordance with the recommendations of the official instructions for the drug.
The individual daily dose is determined in terms of lipase, in accordance with the patient’s age and the complexity of the disease.
The average daily requirement for lipase for an adult patient is 150 thousand units. In case of complete insufficiency of pancreatic function - 400 thousand units.
It is recommended to take Pancreatin tablets after meals, 3 times a day. The duration of therapy is determined by the doctor and can range from several days to several months or years.
Concomitant use of the drug with drugs containing iron may reduce the absorption of iron.
Source: pillsman.org
Forms of release of the drug
Pancreatin is available in pharmacies in the form of tablets and dragees. Capsular preparations have a different name, although they also contain pancreatin. The surface of Pancreatin tablets is covered with a protective coating that prevents the contents of hydrochloric acid from being affected by gastric juice. Therefore, they are classified as gastroresistant. Pharmacologists can tell you the differences between dragees and tablets:
- the tablet is obtained by compressing the powder, looks flattened, then coated with an acid-resistant layer,
- dragees - have a spherical shape, the active ingredients are applied in layers, the additional components necessarily include sugar syrup.
Pancreatin in tablets is made by the Serbian company Galenika ad
The tablets are colored pinkish-brown, the dragees are bright crimson, and children's Pancreatin is green.
The mention of “pills” and the powder version of the drug should be left in the distant past. To this day, the network offers to buy pancreatin powder from the warehouse in bags by weight from 4.5 to 10 kg. The raw material has a grayish color, fine-grained structure, and a characteristic odor. But it is almost impossible to find a pharmacy that will do the hanging and make dosed sachets of 1.0 g. A special license is required for this.
It is completely impractical to engage in outdated production in the presence of a variety of cheap forms of Pancreatin.
Composition and beneficial properties
In composition, different types of Pancreatin differ in the number of enzymes and auxiliary chemicals. In international pharmacology, enzymes are usually evaluated in units of activity. For pancreatic juice, lipase is most sensitive. Therefore, Pancreatin packages indicate the name of the drug and a number indicating lipolytic strength.
Other enzymes are added in the ratio that exists in a healthy body:
- lipase - necessary for converting dietary fats into bile acids, which serve as emulsifiers during digestion,
- amylase - converts carbohydrates and starch into simple sugars, which are easily digested and sent to the liver for energy production,
- proteases - are involved in the hydrolysis of proteins, consist of various enzymes, trypsin and chymotrypsin are of particular value for digestion, they bring the breakdown of complex proteins to essential amino acids.
A description of the general properties of a natural pancreatic juice substitute is as follows:
- “extracting” energy from carbohydrates,
- providing cells with the necessary plastic materials for renewal, creation of immunity,
- supply of coenzymes for the synthesis of complex biochemical substances, vitamins,
- “feeding” beneficial bacterial flora.
These functions are violated:
- for diseases of the pancreas (acute and chronic pancreatitis, cystic degeneration, tumor),
- when used in the treatment of a surgical method of removal or partial resection of the gland, stomach or intestines,
- with a reactive inflammatory process with suppression of the production of pancreatic enzymes in diseases and functional overload of other organs.
Tablets and dragees differ in the method of recording the active substance. It is indicated in the annotation in mg or international units of activity.
The mass can be found in tablets of 100, 125, 250, 300 mg, in Pancreatin forte - 192 mg. Lipolytic activity varies depending on the type of tablet: 25, 30, 8000 units. For doctors, the best option is a drug with the specified enzyme activity. It is convenient in selecting the dosage and comparing it with analogues from different companies.
Each type of Pancreatin includes its own amount of enzymes. The minimum activity in the drug is considered to be:
- lipase - 4.3 thousand units,
- amylase - 3.5 thousand units,
- proteases - 200 or more units.
There may be differences in additional substances, but the required components are:
- talc - added to the powder to improve the structure, into the shell for easier sliding through the esophagus,
- Magnesium stearate - quickly crushes (emulsifies) components, mixes with food,
- polyvidone - promotes the formation of water-soluble complexes and improves the absorption of formed nutrients in the intestine,
- dyes - responsible for design and appearance.
To achieve the expected effect, you should take the drug correctly, taking into account its mechanism of action. There is only one way to take the medicine - swallow the tablet or pill without chewing it in your mouth. The enteric coating disappears only in the duodenum, where the reaction of the environment approaches alkaline. Enzymes are mixed with food and begin to act.
Please pay attention! Do not take the drug on an empty stomach. In the absence of a bolus of food, enzymes direct their breaking down abilities to the mucous membrane. With a peptic ulcer, this can lead to bleeding, which is expressed by black, loose stools.
The released enzymes actively stimulate the secretion of other organs (stomach, small intestine, liver) and improve the secretion of bile. The maximum surge in activity is recorded 30-40 minutes after use.
Diet and other recommendations
For a disease such as diabetes, it is recommended to consult not only a diabetologist, but also a nutritionist to treat the affected gland. It is he who will indicate what the diet should be and how long it should be followed. Speaking about all the features of the diet, pay attention to the fact that:
- A diabetic's diet, in order to ensure treatment of the pancreas, must include the strictest possible ratio of certain components. We are talking about proteins, fats and carbohydrates;
- carbohydrates, as the main component of nutrition, should be contained within 350 grams. during the day. The diet contains smaller quantities of proteins (about 100 g) and fats, the number of which should not exceed 60 g. within 24 hours;
- There should be at least four eating sessions during the day. The ideal amount is six times, but in small portions, so that the pancreas improves its functions gradually.
It is advisable to use a double boiler to ensure the preparation of certain dishes. Fried items should disappear from the diet of a patient diagnosed with diabetes for a long period of time. An acceptable method of preparation is boiling, while stewing and baking are allowed exclusively at the remission stage.
What does Pancreatin help with: indications for use
Pancreatin, as a substitute for its own enzymes, is indicated for patients with diseases and conditions caused by insufficient functional production of the pancreas. Exocrine disorders cause signs of digestive disorders and a predisposition to the inflammatory process. On the other hand, the presence of pathology in the liver, stomach, intestines, and gall bladder suppresses the synthesis of pancreatic juice.
Pancreatin is prescribed by doctors for therapeutic purposes for the following diseases:
- chronic pancreatitis,
- cystic changes in the gland in patients with cystic fibrosis,
- gastritis and peptic ulcer,
- cholecystitis,
- liver diseases,
- biliary dyskinesia,
- in the postoperative period, when part of the stomach and intestines is removed (Crohn's disease),
- in cases of compression of the ducts that carry contents into the duodenum, tumor, tissue edema after radiation therapy,
- development of autoimmune pancreatitis after organ transplantation,
- signs of enzyme deficiency in old age and in patients with type 2 diabetes mellitus, when fibrosis affects the glandular endocrine areas,
- forced immobility of patients (paralysis, paresis, fractures, obesity),
- consequences of cholecystectomy,
- failure to digest food caused by the inability to chew, dental problems, jaw fracture,
- unclear dyspeptic syndrome.
The body needs help if the breakdown is caused by overeating after fasting or on holidays, consuming a significant amount of fatty and fried foods that are difficult to digest, or a violation of the diet by diabetics.
Symptoms of disorder in the digestive system can be associated with the thoughtless use of fasting diets, significant breaks in nutrition, pregnancy, and stress. Children have to be treated for intestinal disorders caused by uncontrolled consumption of carbonated water, chips, fast food, when the baby is allowed to eat “adult” food.
Pancreatin can be used to cleanse the intestines of gases and normalize stools before ultrasound and x-ray examinations.
Clinical manifestations of enzyme deficiency are:
- dyspeptic syndrome (nausea, liquid stool with a greasy sheen, bloating),
- pain in the upper abdomen on the right, girdling in nature,
- heartburn and bitter belching,
- complaints from older people that “the chair either strengthens or weakens.”
You should not rely on a drug to combat obesity. The lipolytic enzyme transforms dietary fats into fatty acids, but does not remove endogenous and subcutaneous fat deposits. The drug helps restore metabolism. Perhaps if excess weight is associated with impaired absorption of fats, then the benefit will appear. However, using large doses without indications is strictly prohibited. A person will not stop getting fat, but will acquire additional dangerous problems caused by an overdose. You cannot treat yourself with Pancreatin.
In order to prevent exacerbation of chronic pancreatitis, patients during the period of remission receive a maintenance dose prescribed by the doctor. The theory of “pancreatic habituation” is not recognized by most gastroenterologists. Studies show the advisability of using enzyme preparations for compensation if the disease progresses and gradually affects a significant part of the organ.
Basic regimens and dosages
Pancreatin in any form is taken only when there is food in the stomach (during meals, immediately after). The drug should be swallowed whole; the tablet should not be chewed or crushed. To wash it down, half a glass of water or non-alkaline mineral water without gas is enough. Children are allowed to use tea and juice.
The dosage is selected by the doctor based on the clinical course of the disease, test results, and the patient’s age. The calculation is carried out in units, then the entire amount is divided into main meals (usually 3-4, but in case of chronic diseases it is possible more often, since fractional meals are indicated).
The daily amount of enzymes taken by an adult should not be higher than 15-20 thousand units. per kg body weight. For chronic pancreatitis, 2-4 tablets are prescribed per dose. If digestive breakdown is caused by overeating, then 1-2 tablets are enough. The sufficiency of the dose is determined by the elimination of signs of dyspepsia and pain. Correction is possible both in the direction of increase and gradual withdrawal of the drug after normalization of stool and well-being.
Regarding the prescription of Pancreatin to children, the official instructions indicate the possibility of safe use only after 6 years. Permitted dose:
- 6 years - 1 tablet per day,
- 8 years - 1-2 tablets or dragees,
- from 10 years - 2 tablets per day.
What is the need for a particular child is determined by the doctor, taking into account the recommendations of various manufacturers. For example, Pancreatin 8000 is generally not suitable for treating children; the instructions say that the drug has not been sufficiently tested in this age group.
The maximum dosages are used by patients with cystic fibrosis. For them, the daily requirement is 10 thousand units. (by lipase) per kg of body weight. It is more convenient to take drugs with high dosages of pancreatin (Creon 10000, 20000, 40000).
The duration of treatment for diet disorders and overeating is several days. To restore digestion during gastritis, peptic ulcers, cholecystitis, Pancreatin is prescribed for 1-3 months. In chronic pancreatitis, replacement therapy is carried out throughout life.
For gastrointestinal diseases
Reactive dysfunction of the pancreas accompanies inflammatory diseases of the stomach and intestines. The doctor judges the presence of organ failure based on tests and clinical symptoms and does not prescribe Pancreatin to all patients.
Excess enzymes can cause harm in the acute stage of the disease, because they stimulate hypersecretion of gastric and intestinal juice. Therefore, if necessary, the drug is used at the recovery stage, 1 tablet 3-4 times. This helps to expand the diet and switch to normal nutrition.
Pancreatin for diabetes
Diabetic patients need the drug if the disease is caused by primary pancreatitis or its connection to a violation of insulin synthesis by the endocrine part of the gland. The appointment is controlled by an endocrinologist. Forms of the drug without sugars are selected (dragées are not suitable). Low doses are sufficient - 1 tablet three times a day. Control tests include blood amylase and urine diastase.
For gallbladder diseases
Cholecystitis rarely occurs in isolation (without inflammation in neighboring organs). The gallbladder and the outflow tract into the duodenum are united with the pancreas by a common outlet and the work of the sphincter of Oddi at the exit border. Anatomical proximity made it possible to isolate the problem into the “common channel theory.”
When pancreatitis or cholecystitis spreads, it necessarily involves part of the excretory tract. A similar process accompanies the formation of salt concretions, which later turn into stones. Increasing secretion by adding enzyme activity causes the stones to move. This causes attacks of cholelithiasis (GSD), “hammers” and clogs small ducts. Stagnation promotes self-digestion of tissue.
Therefore, Pancreatin is contraindicated in the presence of stones, in the acute stage of the disease. To be sure of the choice, the patient must undergo an ultrasound examination. The drug is prescribed in the postoperative period following cholecystectomy. In this case, the absence of a bladder needs to stimulate the transport of bile through the ducts.
Pancreatin for the liver
Liver damage is caused by inflammation (viral and bacterial hepatitis), alcohol disease, fatty degeneration, tumors, and cystic changes. In patients with chronic diseases, liver function can be damaged by long-term use of drugs (anti-tuberculosis drugs, Paracetamol, Methyldopa, Nifedipine, Azathioprine, Amiodarone, tetracycline antibiotics, Clarithromycin, Ibuprofen, hormonal drugs, Indomethacin), contraceptives, poisoning.
If there is pathology of the organ, the need to use Pancreatin may be indicated by signs of involvement of the pancreas; the drug will not be able to cure the underlying disease.
Enzyme preparation is contraindicated:
- in the acute stage of hepatitis,
- with established liver failure,
- if the intrahepatic bile ducts are blocked or compressed by a cyst, tumor,
- when, based on biochemical blood tests, there is a suspicion of organ dysfunction.
Markers of damage to liver cells are considered to be the growth of enzymes: alanine and aspartic transaminases, lactate dehydrogenase, glutamyl transpeptidase, cholinesterase, arginase, bilirubin in the blood plasma.
special instructions
The use of Pancreatin should be taken seriously, carefully study the instructions and indications. In treatment, the drug is never used alone; a diet, regimen, other medications, and physical procedures are prescribed.
It should be remembered that with a long course the drug exhibits harmful effects:
- absorption of iron in the intestine is delayed,
- Not enough folic acid salts are supplied.
This provokes the development of iron deficiency and B12 deficiency anemia. Therefore, the doctor must monitor hemoglobin and red blood cells in the blood.
Pancreatin should not be taken simultaneously with antacids (calcium carbonate, magnesium hydroxide). They reduce the effect of enzymes. If necessary, take a break of 1.5-2 hours between doses.
Among the forms for children there is a version produced in Ukraine. It is allowed to be prescribed from the age of three. Do not follow advice about crushing tablets into pieces or crushing them into powder. You should consult your pediatrician about the possibility of opening the outer capsule when replacing it with a drug in microgranules. Cases of oral irritation, stomatitis, ulcers, and perianal dermatitis have been reported in children. Allergies are more common in premature babies and those who have suffered a birth injury.
For constipation or diarrhea in pregnant women, the cause is hormonal changes and impaired peristalsis. It makes no sense to prescribe Pancreatin; enzymes do not affect intestinal motility. All manufacturing companies warn in the instructions about insufficient research on the effect of the drug on pregnant women and the fetus.
When purchasing, you should pay attention to whether the drug is expired by the date indicated on the package.
Possible side effects
Side effects from the drug were recorded in less than 1 case per 10,000 uses. Most often they manifest themselves in the form of an allergic reaction to the dyes that make up the tablet. If itchy rashes, swelling of the face, tongue, or nasal congestion appear, then stop using the drug immediately, take an antihistamine (Diphenhydramine, Suprastin, Loratadine), and tell your doctor.
In patients with cystic fibrosis, at high doses, there may be a disturbance in the metabolism of uric acid, an increase in concentration in the blood and urine, the appearance of joint pain, and attacks of urolithiasis.
The rarest complication is the formation of adhesions and strictures in the border zone of the ileocecal region, where the small intestine passes into the ascending colon. It manifests itself as signs of obstruction.
Overdose
Overdose occurs with constant consumption of high doses by patients with cystic fibrosis, or when patients self-medicate. In addition to side effects, exacerbation of diarrhea, pain in the epigastric area, nausea and vomiting are possible.
Contraindications to the use of Pancreatin
The drug is contraindicated for people with the following pathologies:
- acute pancreatitis, exacerbation of chronic,
- hypersensitivity to components, manifested by allergies,
- constipation caused by intestinal obstruction,
- acute form of hepatitis.
Dispensing from pharmacies and storing the drug after purchase
Pancreatin in any dosage is available in pharmacies without a prescription. For storage, you need to choose a dry place with a temperature no higher than 15 degrees. Perhaps a refrigerator will do. If the packaging is stored correctly, the manufacturers guarantee the shelf life of the drug for a period of two years.
How much does Pancreatin cost: average price in Russia
The drug is inexpensive and accessible. The price of a package of 60 tablets in different regions of Russia does not exceed 30-40 rubles.
Pancreatin is a targeted enzyme drug, not prescribed unless indicated; you should not take it for any reason for digestive disorders. Before use, you must undergo an examination and make sure there are no signs of cholelithiasis or liver damage. If high doses are required, then microgranular analogs are used (Creon, Micrasim, Ermital).
Source: DiabetSahar.ru
Types of pancreatitis
The disease occurs in acute and chronic forms.
In acute form, due to inflammation, pancreatic juice does not pass into the lumen of the duodenum, but digests the tissue of the pancreas itself. This process causes necrotic changes in the cells of the diseased organ, and in especially severe cases, the complete death of the entire gland.
Symptoms of necrosis:
- High t;
- Nausea;
- Vomit;
- Cutting pains.
Chronic pancreatitis, depending on the cause of its occurrence, is classified as follows:
- Primary - originally arising in the pancreas for any reason.
- Secondary - is a consequence of diseases of other organs: cholecystitis, ulcers, enterocolitis.
- Post-traumatic - a consequence of mechanical impact or surgical intervention.
Types, symptoms and treatment strategy for pancreatitis
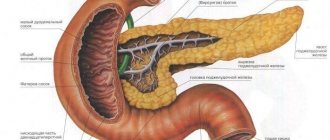
The pancreas is part of two body systems at once - digestive and endocrine.
Despite its light weight (about 70 grams), its role in the normal operation of these systems is very large.
It performs the functions of external secretion, secreting pancreatic juice for the duodenum. It contains 3 enzymes - lipase, trypsin and amylase.
https://www.youtube.com/watch?v=YkefLGAvbKg
Another function of the organ is the production of hormones that regulate several types of metabolism - protein, lipid and carbohydrate. The gland synthesizes 5 hormones, including insulin and glucagon.
Pancreatitis is inflammation of the pancreas. The importance of the organ in the functioning of digestion and metabolic processes leads to the development of significant changes in the patient’s condition and disturbances in the functioning of the entire organism during the disease.
The pancreas (PG) produces pancreatic juice, which is then transported through the ducts to the intestines for the digestive process. Enzymes neutralize hydrochloric acid in gastric juice and participate in the breakdown of nutrients in the intestines.
Inflammation of the organ tissue leads to blocking of the pathways for the free release of juice. It lingers in the gland and begins to affect its tissues - digests them.
Inflammation of the pancreas leads to the inability to produce juice; its composition and quantity become insufficient for normal digestion. An additional source of dysfunction of the gland can be neoplasms and stones that interfere with the normal outcome of enzymes.
Pancreatic juice, having no outlet, is activated directly in the organ. Enzymes literally destroy the pancreas. The process proceeds quickly and tissue necrosis may develop. The inflammatory process also affects nearby organs.
A large amount of toxins are released into the blood, which poison the entire body, and intoxication occurs. In severe poisoning, the heart, lungs, and brain are affected. Intoxication in acute pancreatitis can develop very quickly.
The cause of the development of pancreatitis is the retention of pancreatic juice in the gland and disruption of its outflow. An acute attack most often develops due to alcohol consumption and blocking the release of enzymes due to stones (cholelithiasis).
The causes of acute pancreatitis can be divided into 3 groups:
- Blockage of the duct and resulting delay of enzymes in the gland. This can occur due to stones, tumors and pathologies of nearby tissues.
- Increased production of enzymes, exceeding the required amount.
- Bile reflux into the pancreatic duct.
Various life factors in children and adults lead to the development of these causes.
The mechanism of diabetes
Diabetes mellitus type 1, with pancreatitis, appears due to the fact that the inflamed ducts of the pancreas do not allow digestive enzymes to pass into the lumen of the duodenum and self-digestion begins, the degeneration of cellular tissue into adipose, connective tissue, or the complete death of organ fragments. The body experiences an absolute lack of insulin, the level of glucose in the blood rises, which has a destructive effect on all systems of the body.
Type 2 diabetes occurs when there is insufficient insulin production. But due to disruption of metabolic mechanisms, it does not perform its main function, creating relative deficiency.
Pathological changes accumulate over time and are divided into four stages:
- At the first stage, short-term exacerbations are interspersed with long lulls. Chronic inflammation forms in the gland, mostly latent with rare pain syndromes. This period can last up to 10-15 years.
- The second phase is characterized by more pronounced dysfunction of the digestive system. Inflammation provokes uncontrolled releases of insulin into the blood, which can even lead to temporary hypoglycemia. The general condition is complicated by stool disturbances, nausea, loss of appetite, and gas formation in all parts of the gastrointestinal tract.
- The functionality of the pancreas is critically reduced. And, if on an empty stomach, tests do not reveal any abnormalities, then after eating, glucose in the blood plasma is determined far beyond the normal time interval.
- And at the last stage, secondary diabetes forms, affecting a third of patients with chronic pancreatitis.
Features of the course of diabetes in chronic pancreatitis
It would be logical to conclude that two diseases are much more difficult to treat than one. But practice shows the inconsistency of such a conclusion. The secondary process has a number of features that make it highly curable:
- Proceeds almost without ketoacytosis;
- Treatment with insulin often leads to hypoglycemia;
- Can be adjusted well with a low-carbohydrate diet;
- At the first stage, it is quite effectively cured with oral medications for diabetes.
Prevention and treatment of pancreatic diabetes mellitus
Not every chronic pancreatitis necessarily causes the development of diabetes mellitus . With properly prescribed treatment and a strictly followed diet, you can not only improve the health of the pancreas, but also prevent the onset of diabetes.
An endocrinologist selects individual treatment in each individual case. Depending on the level of production of digestive enzymes by the gland, a competent specialist will prescribe replacement therapy based on medicinal enzymes with a similar effect. As well as insulin injections if necessary.
Methods of treatment and prevention
Before starting drug therapy for the pancreas, a diabetic must go on a strict diet. This will improve the condition of the damaged organ. It is not possible to avoid taking medications - correction involves taking enzymes and hormones, and eliminating junk food from the diet.
The multifaceted symptoms of the pathology involve the use of drugs of various spectrums of action.
To alleviate the patient's condition, the following are prescribed:
- Painkillers;
- Enzymes that compensate for deficiencies in the body;
- Antibacterial agents to prevent the development and spread of infection;
- Complex-action drugs with the active substance metformin hydrochloride have a positive effect on well-being;
- Some other substances are prescribed that normalize metabolic processes.
Your doctor may recommend natural remedies to lower blood glucose levels, such as chicory root or sea buckthorn leaves. Control of the quality and quantity of food consumed is mandatory.
It will take up to ten years to restore the functioning of the organ, but these actions will support the organ during and after therapy, as a preventative measure for the disease. To achieve results, it is better to seek advice from a professional nutritionist.
The way to control your diet is to maintain the correct ratio of fats, carbohydrates and proteins in foods.
The doctor will tell you how to focus on the glycemic index and introduce you to the table developed for this. General recommendations:
- Daily fat intake does not exceed 60 grams, protein content is 100, carbohydrates up to 350;
- Eating occurs frequently and in small portions (5-6 times a day or more);
- It is useful to avoid fried foods; it is better to use a double boiler;
- During periods of remission, stewed and baked foods are allowed;
- It is better to avoid consuming hot and spicy seasonings that irritate the mucous membranes of the digestive tract;
- During periods of exacerbation (or better on an ongoing basis), spicy, fatty, salty, smoked foods are strictly contraindicated.
Starting treatment for diabetes mellitus precedes a trip to a specialist.
When conservative methods of treating pancreatic pathologies do not produce results, a decision may be made to transplant it. This method is used in the most extreme cases, since there is no guarantee that there will be no complications after the operation or confidence that the organ will take root. However, a successful transplant can relieve a diabetic patient from insulin injections. Organ transplantation is a complex process. This is due to the peculiarities of the structure, location and functioning of the organ.
- Location of the gland in the retroperitoneal space;
- Location close to many other vital organs;
- The presence of large blood vessels in the immediate vicinity;
- Sensitivity of organ tissue to any influences;
- A potential complication expressed in the gland processing itself;
- Injury to adjacent tissues in case of damage to the pancreas.
A risky, high-reward procedure can be very effective, as statistical analysis confirms. About a thousand cases of such medical intervention are recorded every year.
Inflammation in the tissues of the pancreas leads to the destruction of part of its cells responsible for the secretion of hormones. The beta cells that produce insulin are most affected. An alternative to whole organ transplantation is organ transplantation. This is an effective method of influencing type 1 diabetes in case of low effectiveness of insulin replacement drugs.
The process consists of stimulating the remaining functional cells. It is carried out using healthy cells from a donor, entering through a catheter into the portal vein of the liver. The result should be restoration of the functioning of the affected area of the organ, eliminating the development and complications of the disease. The operation has proven to be effective and not life-threatening for the patient.
The current state of development of the medical field allows, in some cases, to achieve success without resorting to surgical intervention. This method is based on the property of a certain protein to stimulate the ability of affected cells to recover. The substance is administered intramuscularly.
The development of this modern method is aimed at helping diabetics with a history of type 1, whose insulin-producing cells are destroyed by the body itself, which produces antibodies intended for this purpose due to a failure in metabolic processes. Scientists are actively exploring the possibility of creating a vaccine that induces the body's immune system to destroy such antibodies to allow the remaining beta cells to increase in number and restore function.
Diabetics with insulin dependence receive insulin injections. Injections are not given to patients with type 2 diabetes. Patients are prescribed medications that lower blood sugar.
Diet for acute destructive changes in the structure of the pancreas is an integral part of the entire treatment of the disease in adults and children.
Treatment of pancreatitis and diabetes is aimed at suppressing the destructive function in the pancreas. The method of therapy is determined by the endocrinologist depending on the patient’s medical history, the severity of the pathological processes and the individual tolerance of the body.
The following foods should be excluded from the diet:
- hot sauces and spices;
- various sweets;
- sweet pastries and white bread;
- fatty and fried foods;
- mayonnaise;
- smoked meats and sausages.
Diet therapy for diabetes in pancreatitis prohibits the consumption of foods containing large amounts of sugar and carbohydrates.
If you are diagnosed with type II diabetes, you must constantly count the carbohydrates you consume and completely eliminate sugar.
The daily diet of patients with diabetes and pancreatic inflammation should consist of the following products:
- a small amount of fresh fruit;
- no more than 300 grams of vegetables;
- no more than 200 grams of protein-rich foods;
- up to 60 grams of fat.
Treatment of patients with pancreatitis and diabetes mellitus is quite complex. First of all, all efforts are aimed at restoring carbohydrate metabolism in the body and the enzymatic function of the pancreas.
Basically, the doctor prescribes hormonal drugs, statins (drugs that lower cholesterol levels) and enzymes (drugs that normalize carbohydrate metabolism). The most common drug that breaks down fats, proteins and carbohydrates is Pancreatin; in type 2 diabetes it is especially necessary, since the treatment of this type of diabetes is mainly associated with proper nutrition and restoration of metabolic processes.
Pancreatin improves the enzymatic function of the pancreas.
Important. Drug therapy for pancreatitis in combination with diabetes is carried out in several stages. The duration of treatment may drag on for a long period. All medications should be taken only as prescribed by a doctor. Self-medication leads to irreversible consequences.
Diabetes mellitus always requires replacement therapy; it boils down to normalizing blood glucose levels and replenishing insulin deficiency. Taking into account the stage of the disease, the patient is prescribed insulin injections or tablets.
However, the patient’s health largely depends on properly adjusted nutrition. And, of course, do not forget to take pancreatin if you have diabetes, which will make it easier to absorb and process the food that enters the stomach.
The pancreas in diabetes mellitus is completely recoverable. After making a diagnosis, the endocrinologist himself draws up an individual nutrition plan for the patient or sends the patient to a nutritionist. This step is the main one on the path to restoration of the pancreas, since it is diet that is the basis for successful control of the process of the organ, including the level of glucose in the blood.
In addition to changing the nutrition plan, the attending physician prescribes regular performance of a special set of physical exercises.
If diet and exercise are not effective enough, the specialist prescribes medication. This could be a drug that stimulates the production of the desired hormones or drugs that increase the body’s ability to use its own insulin.
Pancreatitis can be fatal
Restoring the pancreas in the case of a combination of diabetes and pancreatitis is a more difficult task.
Treatment begins with placing the patient in a hospital. The primary task is to relieve inflammation. In case of pancreatitis, this process is performed only under the supervision of a doctor. The patient is injected with anti-inflammatory and analgesic drugs that suppress the action of pancreatic enzymes. In especially severe cases, the patient is prescribed antibiotics.
Diet for diabetes and pancreatitis
https://www.youtube.com/watch?v=3D9hQX2f27Y
During the first two days, the patient is prescribed fasting for medicinal purposes. This significantly speeds up the relief of acute inflammation and also reduces the amount of enzymes produced by the gland.
The next stage is a two-week therapeutic diet and the introduction of medications to the patient to replenish the lack of enzymes. Alcoholic beverages, everything spicy, fatty, smoked, and pickled are excluded from the list of products for consumption.
Pancreatitis leads to a decrease in the number of beta cells, which cannot be restored with drug therapy. Surgical transplantation of the islets of Langerhans has only a temporary effect, after which the cells begin to die again. This situation always occurs with type 1 diabetes. The only solution is insulin therapy.
Dietary rules for pancreatitis and diabetes mellitus
You need to know that properly selected treatment and strict adherence to a diet can lead to complete recovery from these serious illnesses. You need to eat food often and in small portions - 250-300 grams at a time. Give preference to foods containing proteins: soy, egg whites, meat, fish, nuts.
Remove from the diet acidic foods that provoke rapid secretion of gastric juice: sour, spicy, smoked, fried, containing alcohol, too hot or cold. In short, all the dishes. which can cause additional stress on pancreatic secretion.
It is advisable to steam food and eat it warm, not hot or cold.
If it is difficult to choose the right diet on your own, you can use specially developed dietary recommendations, collected under the names: table No. 5 - for patients with pancreatitis and table No. 9 - for diabetics. But before choosing this or that diet, you should definitely consult with your doctor.
Only after taking into account all the features of the course of the disease and the general condition of the patient, the doctor gives the most accurate nutritional recommendations.
Product selection
During different periods of the disease, the diet may vary slightly. So, for example, sweet and sour fruits or dishes based on rice, oatmeal and semolina are quite acceptable during periods of long remissions, but are completely excluded when the disease worsens.
Suitable products for each patient should be selected individually, taking into account:
- Personal preferences;
- Glucose sensing abilities;
- Intolerance to any substances;
- Correction of partial absorption of nutritional components.
In the acute period, it is strictly forbidden to consume foods with a high sugar content, fatty and smoked foods, baked goods, fried foods, porridges: rice, oatmeal, semolina; raw fruits and vegetables, white bread.
As for vegetable oils, it is better to use, in reasonable quantities, flaxseed and extra virgin olive oil, which have healing properties. Low-fat milk will also not be harmful. Milk enriches the body with vitamins, minerals and helps relieve inflammatory processes in the gastrointestinal tract.
Recipes of allowed dishes
The rules for cooking and limiting the choice of food remain general.
The proposed rules of diet No. 5p do not exclude use for concomitant diseases of the digestive system. They are important for creating maximum unloading of the pancreas.
- Cook food only when boiled, stewed, baked or steamed. The frying method is completely prohibited.
- Take care to spare the damaged organ by crushing all foods during the most acute stage of the disease.
- A moderate temperature regime is required (without sharp fluctuations from cold to hot).
- The patient must be fed small amounts of food, but every 3–4 hours.
- Do not allow one-time large meals, or overeating even dietary dishes.
- Maintain a daily caloric intake of at least 3000 kcal.
Clinical manifestations of acute and chronic pancreatitis in the acute stage (severe pain, vomiting, nausea, diarrhea) do not allow the patient to eat in the usual way. The treatment regimen requires complete fasting for two to four days. You can’t drink either; in the first days, liquid is administered intravenously.
After the vomiting and pain stop, the initial version of the 5p diet is prescribed. Its goal is to reduce the formation of gastric acid and enable the pancreas to concentrate all its forces on the process of fighting for survival.
The diet allows for use for no longer than two weeks, since the composition is not balanced (proteins are reduced to 60 g, fats to 50 g, carbohydrates to 200–280 g, with a total calorie content of 1800 kcal). Of course, bed rest and lack of physical activity are recommended.
Vegetable stew has a good effect on the digestion process if you prepare it according to a special recipe. You need to take five large potato tubers and cut them into medium cubes. After this, grate one carrot and finely chop the onion. To taste, you can add a small amount of tomatoes and pumpkin.
It is important for a patient with pancreatitis to know how to prepare fish for a diabetic and which varieties to choose. You can cook baked fish; the following fish are suitable for this: pike perch, pike, pollock, hake.
The fish can be cooked whole or cut into portions. The fish is placed on sheets of aluminum foil, sprinkled with chopped onions, grated carrots, and a large amount of lemon juice and salt are added.
Carrot pudding is a good alternative to junk food; you need to prepare the following products:
- 1 carrot;
- 5 g butter;
- 500 ml milk;
- 1 egg white;
- 2 teaspoons semolina.
Add half a teaspoon of sugar, a little low-fat sour cream and a teaspoon of wheat crackers.
The carrots are thoroughly washed, peeled, cut into pieces, and then stewed in milk until fully cooked (over low heat). When the carrots become soft, grind them using a blender, add sugar, half the butter, and semolina.
After this, beat the egg whites with a whisk and carefully pour them into the carrot mixture. If desired, you can add a small amount of apples, cottage cheese or berries to the dish. Grease the baking dish with the remaining butter and sprinkle it with breadcrumbs. The puree is poured into the mold, the surface is leveled, and sour cream is spread on top. The pudding is cooked in the oven until golden brown.
Let's look at several types of recipes with which you can prepare essential dishes. A popular dish in a diet for pancreatitis is chicken puree soup.
To prepare this soup, you need to follow these steps:
- First you need to take chicken meat, cut it into small pieces and boil it. When the meat is ready, it must be cooled and separated from the bone. After this, we pass the resulting meat through a meat grinder with a small mesh.
- When the meat puree is ready, we move on to preparing the vegetable broth. To do this, take potatoes, carrots, parsley, cabbage and boil them for 30 minutes. The vegetables should first be chopped, but into large pieces. After preparing the decoction, it should be strained through cheesecloth.
- We need a broth to which we should add the meat puree. After this, the resulting workpiece is placed on the fire and brought to a boil. After the soup has cooled, it is ready to be consumed. But to diversify it even more, you can add an egg-milk mixture. To prepare it, you need to mix the yolks with milk and put on fire. When the mixture thickens, it is added to the puree soup and served.
This soup is healthy and nutritious for patients with pancreatitis. An even simpler recipe can be prepared faster:
- To do this you will need to boil the carrots and rice.
- Rub the carrots through a fine grater and the rice through a sieve.
- The resulting mass is added to the vegetable broth and boiled for 5 minutes.
After this, the soup is ready to eat, but to add flavor, you can add 5 grams of butter.
Products allowed on the diet during and after acute pancreatitis can be combined with each other. It is useful to prepare main and additional dishes, desserts from them and introduce them into the weekly diet during the period of remission.
You can prepare steamed cutlets in several steps:
- Pass half a kilogram of low-fat meat through a meat grinder or blender, add chopped onion and bell pepper.
- Beat out the resulting minced meat. If necessary, grind it again. Add a little salt, mix, form cutlets and refrigerate for half an hour.
- Place the resulting cutlets in a steamer and boil for half an hour.
- Boil one hundred grams of fillet. Pass through a meat grinder or blender.
- Add chicken yolk, beaten egg white and salt to the minced meat and mix.
- Pour the mixture into the mold and steam for half an hour.
- Melt a teaspoon of butter, add half a spoon of wheat flour to it, boil for a few minutes, cool. Serve and eat the dish with the sauce.
- Boil half a kilogram of peeled potatoes. Crush.
- Pass half a kilogram of meat without fat through a meat grinder with a small onion, add a chicken egg to the minced meat.
- Place a centimeter layer of puree in a greased pan. Place the minced meat on top, cover it with the rest of the puree and grease the top with oil.
- Bake for half an hour.
The basic rules of nutrition for pancreatitis are to balance the nutritional value of the foods consumed. It is necessary to increase the amount of protein, reduce the consumption of simple carbohydrates and optimize the number of plant and animal products.
Regardless of the presence of diabetes in the anamnesis, split meals are important. The regimen involves 6 meals a day in portions weighing no more than 300 g.
For the treatment of aggravated and chronic inflammatory processes of the pancreas, a special diet table No. 5p has been developed. For diabetes, table No. 9 is used.
For patients with pancreatitis, it is important not to provoke strong secretion of gastric juice, as with a stomach ulcer. An increased content of hydrochloric acid causes the production of gastrin. The hormone stimulates the secretion of the pancreas, its digestive enzymes and insulin. It is necessary to exclude spicy and sour foods, fried and smoked foods from the diet. Drinking alcohol is prohibited.
The diet for ulcers, as for pancreatitis, involves steaming or boiling dishes, grinding them and serving them warm. Mechanical stress and temperature changes have an adverse effect on the gastric mucosa, causing inflammation and the production of pancreatic enzymes.
If you have pancreatitis, you should always eat food warm; you should avoid eating too hot or cold foods. The menu is always dominated by foods rich in protein, and carbohydrates and fats are reduced to a minimum. It is forbidden to eat foods that contain too many acids.
Doctors insist that you should avoid foods that contain a lot of coarse fiber. The average daily calorie intake should be within 2 thousand calories. Additionally, drink at least 1.5 liters of clean water; you need to rely on warm, mineralized drink.
The chemical composition of the daily menu is as follows:
- protein (80 g);
- carbohydrates (200 g);
- fats (40-60 g).
There are two options for dietary table No. 5. If a diabetic is diagnosed with an acute form of the disease, he will be prescribed table 5a; for the chronic form, table 5b is indicated.
Diet No. 5a provides for the consumption of no more than 1,700 calories per day, all dishes are served to the patient in a thoroughly pureed form. Completely exclude products that promote the secretory function of the pancreas. In addition to the basic chemical composition, there are strict limits on kitchen salt - a maximum of 10 g per day.
You should eat meals in small portions, at least 6 times a day, always within a certain period of time. The duration of such a diet for a diabetic is prescribed depending on the severity of pancreatitis, but on average it is at least 7 days.
Table 5b regulates 2700 calories per day, and the chemical composition of the dishes is as follows:
- fats (maximum 70 g);
- carbohydrates (up to 350 g);
- protein (no more than 140 g).
To get rid of attacks of pain and unpleasant symptoms of pancreatitis, you need to control your diet. If you do not adhere to a special diet, then the signs of the disease will not leave the person alone.
conclusions
Unfortunately, people are structured in such a way that, understanding the full value of health, they still “dig their own grave with a spoon.” But the same folk wisdom long ago found a simple solution to problems with the pancreas - hunger, cold and peace.
By adhering to this simple rule and following specially selected therapy, most patients could overcome many ailments and return to a healthy full state.
Source: PriDiabete.ru
The pancreas is involved in the process of digesting all major sources of energy (proteins, fats and carbohydrates). This ensures the complete absorption of digestive products in the cells. It is important to maintain a balance of both components.
Balance must be maintained both on the part of the exocrine function of the pancreas, the enzymes of which (proteases, lipases and aldolases) ensure the digestion of food in the gastrointestinal tract. So does the endocrine function of the pancreas, which through the hormone insulin ensures a decrease in blood sugar levels. And regulation of other types of metabolism of energy substrates (proteins, fats).
What happens with type 1 or type 2 diabetes ? Impaired absorption of glucose in cells occurs when there is insufficient production of insulin in the pancreas ( diabetes
mellitus
) or when the pancreas produces defective insulin, impaired sensitivity of receptors to insulin, and insulin resistance of the liver appears (
diabetes mellitus
). This is a standard situation accompanied by an increase in blood sugar levels.
How can mezim, festal, pancreatin, enzibene and other enzyme preparations affect this situation? Very simple. Introducing additional amounts of digestive enzymes into the body not only enhances, but also accelerates the digestion process. Which leads to an imbalance in the activity of the exocrine and endocrine parts of the pancreas. And a rapid increase in blood sugar levels and load on the pancreas. Which aggravates
both
type 1 and type 2 diabetes Because requires either more glucose-lowering drugs, in the case of type 2 diabetes. Or the introduction of additional units of insulin for type 1 diabetes.
What will you get if you do not administer an enzyme preparation if you have diabetes? Activation of intestinal microflora, the process of decay (protein foods) or fermentation (carbohydrate foods). Absorption of toxic substances into the blood, overloading the detoxifying functions of the liver and kidneys. In general, there is little good. Especially if you have type 1 diabetes.
What happens when enzyme preparations (Pancreatin, Mezim, Festal, Enzibene) are taken by people who do not have diabetes? On the one hand, improving the digestion process reduces bloating and rumbling. On the other hand, replacement therapy leads to a gradual decrease in the capabilities of the pancreas and its exocrine function. And it transfers a person to the constant use of enzyme preparations. And an increase in the absorption of digestive products into the blood overloads the endocrine function of the pancreas, and in the future
type 2 diabetes
mellitus A sharp increase in blood viscosity can lead to more serious consequences - an increase in cardiac risk, the risk of developing a hypertensive crisis, myocardial infarction, and stroke.
Do you want to depend on taking enzyme medications for the rest of your life? This is your choice. If you want to be independent, take the proven family recipe of traditional medicine “Doctor Skachko’s Health Formula No. 1.” Taking formula No. 1 ensures activation of the digestive process in the stomach and small intestine, increased secretion of pancreatic juice, and ensures the outflow of bile. At the same time, while taking formula No. 1, pathogenic flora in the intestines is suppressed, liver functions are enhanced, including the accumulation of glycogen in the liver (activation of the glycogen synthetic function of the liver) under the influence of insulin, and fatty hepatosis is reduced. Those. Formula No. 1 ensures enhancement of both exocrine (enzyme secretion) and endocrine (insulin production) functions of the pancreas. If you have diabetes: effective liver treatment will cure type 2 diabetes.
What else is Formula No. 1 needed for diabetes? Formula No. 1 helps to gain weight
in
diabetes . But not due to adipose tissue, but due to improved absorption of protein foods and accumulation of muscle tissue. And muscle tissue is one of the main consumers of carbohydrates in the body, allowing you to easily control blood sugar levels through optimal physical activity. And reduce sugar levels to the optimal range.
What to do if you already have insulin-dependent diabetes
mellitus
or non-insulin-dependent
diabetes mellitus ? Take Dr. Skachko's health formula No. 11. The family recipe of traditional medicine is intended for the treatment of diabetes mellitus
of the first and second types.
And it allows not only to regulate blood sugar levels. But also to prevent the main complications of diabetes mellitus
in the form of atherosclerosis of the aorta, coronary vessels, and diabetic angiopathy. And also their consequences in the form of diabetic retinopathy, polyneuropathy, nephropathy, gangrene of the extremities...
Good health to you. And a reasonable attitude towards him.
Source: www.sites.google.com
Pancreatic diabetes: features of the disease and risk groups
In this case, the diet is needed only to control weight and prevent an overdose of the hormone. It consists of limiting the consumption of fatty foods, carbohydrates and coarse fiber. In addition, you will have to forget about rich broths.
Dietary nutrition is the most reliable therapy
A common mistake a patient makes is switching to protein foods, because excessive consumption of protein, especially animal protein, negatively affects the functioning of the pancreas and can cause problems in the functioning of the kidneys.
As for carbohydrates, you shouldn’t go to extremes here either. Limiting sugar consumption goes without saying, but a complete rejection of carbohydrates is unacceptable, since excess hormones administered by injection begin to be stored “in reserve” and may one day cause insulin resistance.
To avoid such situations, it is better to entrust the preparation of the menu to a nutritionist and make a certain diet part of your lifestyle.
You need to eat food in small portions 4 to 6 times a day.
A steamer is the best option for cooking. During the period of remission, you can use boiling, stewing and even baking in the oven, but it is better to give preference to steamed dishes.
Safe foods for the pancreas for diabetes are:
- dietary (lean) meat;
- fish;
- vegetable broths and milk soups with whole grains;
- durum wheat pasta;
- porridge (without adding butter and sugar);
- diabetic bread;
- milk (no more than 100 milliliters per day);
- dairy products;
- omelette;
- fruits, vegetables and berries (fresh and baked);
- tea (weak with milk), freshly squeezed fruit and vegetable juices (not sour);
- honey or jam - only during remission.
As mentioned above, surgery does not guarantee recovery. Therefore, the answer to questions about how to treat the pancreas in diabetes mellitus and prevent the occurrence of crises and exacerbations will be to maintain a special lifestyle, including therapeutic nutrition, regular physical activity and, if necessary, drug therapy.
Do type 1 or type 2 diabetes provide disability?
Adelina Pavlova
General nurse. More than 40 years of working experience. Retired copywriter.
More about the author
Last updated: October 19, 2019
Pancreatitis is an inflammation of the pancreas, which often becomes chronic. In severe forms of the disease, a large part of the healthy working cells of the organ is replaced with fat cells belonging to connective tissue, or scar cells. Such disruptions cause a lack of hormones normally produced by the pancreas, which provokes a variety of disorders, including excessive accumulation of sugar in the blood.
The onset of symptomatic diabetes directly depends on lifestyle and diet.
The violation affects people of different genders, nationalities and ages. However, the advantage of such a disease is the possibility of preventing it. It is enough to control your diet and reduce exposure to bad habits in order to reduce the likelihood of pancreatic disease and avoid this type of diabetes.
Symptomatic diabetes does not appear overnight. Its formation often takes many years. The manifestation is preceded by an acute form of inflammation of the pancreas, its transition to chronic. The development mechanism has three conditional stages.
- Manifestation of pain of varying strength and localization. Periods of exacerbation are followed by remissions. The process can continue for many years;
- Dysfunction of the digestive system - loss of appetite, excessive accumulation of gases, nausea and vomiting, heartburn. The initial stage of disruption of the body's processing of carbohydrates begins due to the unstable functioning of the irritated pancreas, which periodically produces excessive amounts of insulin;
- The advanced stage of chronic disease is manifested by susceptibility to glucose. Its level in the blood rises too much after eating and remains so for an abnormally long time.
Next, a third of patients develop pancreatic diabetes. Untreated pancreas can lead to other types of diabetes, but this happens almost half as often.
The pathology exhibits similar features to the first and second types of diabetes mellitus, however, a number of special characteristics distinguish the symptomatic type of the disease. Often patients have low blood sugar levels. This leads to a state of hypoglycemia - a stable lack of glucose for the normal functioning of physiological mechanisms and associated symptoms.
Medicines that lower blood glucose levels are effective only at the initial stage of the disease.
Separately, it is worth noting the relationship between the manifestations of pancreatitis and type 2 diabetes. Inflammation of the pancreas provokes this pathology if the malfunction occurs simultaneously with an increase in the concentration of sugar in the blood fluid. The disease is characterized by acute pain in the abdominal cavity and dysfunction of the digestive tract.
As we have already noted, the pancreas is responsible for two main functions in the body.
| Function | Description of action |
| Exocrine | The production of pancreatic juice in conjunction with digestive enzymes. |
| Endocrine | Production of the hormone insulin, which is responsible for suppressing excess sugar levels in the blood plasma. |
The resulting inflammatory process in the pancreas negatively affects the production of pancreatic juice and the hormone insulin. Lack of the hormone leads to the fact that glucose entering the body loses its ability to pass into an altered state (glycogen) and be deposited in the cellular tissue of the liver, as well as in fat and muscle tissue.
Excess sugar content leads to relative destruction of pancreatic cells that produce insulin. It turns out that with sufficient production of the hormone, it is simply not able to fully perform its functions. This condition is characterized by a relative deficiency of insulin, and leads to pancreatitis and type II diabetes.
Important. Despite the fact that pancreatitis and diabetes are related, the development of pancreatitis in diabetes and vice versa is not always observed. Proper nutrition will eliminate the likelihood of developing various complications of diabetes. In some cases, nutrition is the main method of treating the disease.
It was already mentioned above that the main reason for the development of pancreatitis is the wrong way of eating. Indeed, nowadays people have lost the habit of natural food, switched to semi-finished products, food from supermarkets and, even worse, fast foods.
Instead of eating three times a day, a person sits down at the table only in the late afternoon and fills his stomach to capacity. During the day, only snacks in eateries are possible.
But dinner should not contain a lot of calories, and especially fatty or smoked products. In addition, people who are accustomed to eating fried, smoked and salty foods every day are prime candidates for the development of pancreatitis.
People who drink a lot of alcohol, spicy foods, and carbonated drinks are also at risk for pancreatitis. After childbirth, the pancreas is also stressed in young mothers, so it is especially important to take care of yourself in the first months after the birth of the child.
We have already noted that the period of development of diabetes against the background of existing chronic pancreatitis takes a long period of time. The disease is called pancreatogenic diabetes mellitus, its treatment directly depends on proper nutrition in combination with insulin therapy and taking medications containing digestive enzymes.