Unfortunately, inflammation of the pancreas secretory organ in children has recently become increasingly diagnosed. The reason for this, according to gastroenterologists, is a violation of the quality of food and the encouragement by many parents of fast food, which has begun to occupy almost the main place in the daily menu of a small child. All this leads to the appearance of acute symptoms that accompany pancreatitis. Treatment in this case is unthinkable without nutritional correction. A strict diet for pancreatitis in a child is prescribed from the 3rd–4th day of detection of the disease and continues for a week. Further, after the diseased pancreas begins to function normally, the baby’s diet expands. But this should happen only after consultation with a specialist.
Features of a child’s diet in different forms of the disease
In childhood, based on statistical data, a disease such as pancreatitis, which occurs in chronic or acute form, rarely occurs. Mostly children are susceptible to a reactive type of illness, which in medical terminology is called dyspancreatism. With this type of pathological condition, the children's pancreas, which is responsible for the production of digestive enzymes, ceases to function normally due to somatic disorders or frequent dietary disorders.
In order to help your child cope with the disease, it is necessary to correctly adjust the diet, including in the daily menu only those foods that the doctor allows.
All restrictions in the children's diet necessary for inflammation of the pancreas are directly dependent on the type of disease developing in a small child. To learn more about the nuances of the diet prescribed for children, you should look at the table below. It indicates the main characteristics of the children's dietary menu, which are recommended by the famous TV presenter, Dr. Komarovsky.
Principles of the dietary table for pancreatitis in a child
| Form of the disease | Principles of nutrition |
| Acute pancreatitis | From the moment the disease is diagnosed, diet No. 5 is prescribed, which is followed for at least a month. The first week she is very strict, and then as the baby’s health improves, the table begins to gradually expand. But the child must follow the principles of the dietary diet for at least five years, even if there are no negative symptoms. Gross errors in the menu and in the future are undesirable. |
| Reactive type of disease | The diet correction recommended for the baby by a gastroenterologist must be followed for at least 14 days. After this period, there will be no strict restrictions in the diet, but the doctor will advise you to feed the child according to his age, including only benign foods in the menu that do not cause damage to the mucous membrane. |
| Chronic process | After the exacerbation ends, the strict diet will be canceled and a less gentle diet option will be prescribed. But the diet will remain selective (many products will be completely prohibited) and it will be necessary to adhere to it for life. |
Each stage of the disease requires the baby to adhere to a certain diet with strict adherence to all doctor’s recommendations. But even despite the existing bans on certain types of foods due to this disease and strict requirements for food management, parents can make their child’s daily menu not only nutritious, but also tasty. By showing a little imagination when preparing a dish from a meager list of ingredients, you can please even the most capricious and picky eater of a child.
Diet 5P: features and recipes
Inflammation of the pancreas is a serious test for a child’s body. Therefore, when choosing products for a sick person, attention and caution are required. Experts recommend dietary table No. 5P for a child during this period. Its goal is to reduce chemical and mechanical effects on the stomach and be gentle on the pancreas. This diet will help restore pancreatic function and significantly improve the child’s health.
The 5P diet for pancreatitis is a therapeutic nutrition plan that includes meals with a high protein content and involves limiting carbohydrates, fats and sugar. Dishes that provoke increased secretion of enzymes, fried and fatty foods are completely excluded. The main cooking method is boiling in water, steaming, and baking. To reduce the mechanical impact on the stomach, it is advisable to wipe or chop thoroughly.
What to feed a child with pancreatitis?
Many children, even when they are completely healthy, eat very poorly, are capricious and picky when eating. During illness, feeding babies is even more difficult. This is why doctors are often asked: what to feed a child during illness? Parents are especially interested in the question of what children with gastrointestinal diseases can and cannot eat. Since children are most often exposed to the development of an inflammatory process in the pancreas, it is worth taking a closer look at the nutritional characteristics during this disease.
For pancreatitis, the children's diet in the first days of the onset of acute symptoms involves complete fasting. This is necessary so that the inflamed organ calms down, and doctors have the opportunity to begin carrying out adequate therapeutic measures.
After 2-3 days, after the child’s condition improves a little, he is prescribed table No. 5, which in the first days is very strict: pureed liquid porridge with water, slimy soups and vegetable purees. At approximately 7–10 days, the diet begins to gradually expand. From now on, children with pancreatitis are allowed to include the following list of products in the menu:
- cereals, buckwheat, rice, oatmeal,
- cottage cheese and other low-fat fermented milk products,
- durum pasta,
- vegetables and fruits (they are prescribed in each specific case by a specialist, based on the general condition of the baby),
- lean meat and fish,
- eggs (preferably quail).
The list of permitted products is quite meager, so parents should use their imagination to prepare quite healthy, satisfying and tasty dishes from them. You should definitely remember that culinary processing of products is only permissible by cooking, stewing or baking. Plant foods: vegetables, fruits and herbs must also be heat treated.
What foods should you exclude?
After a child is diagnosed with pancreatitis, he, as already mentioned, is prescribed a rather strict diet. In this case, many products are prohibited. First of all, the food that should disappear from the baby’s table is the one that has the ability to activate the production of enzymes and enhance the functioning of the pancreas.
You should also reduce the amount of carbohydrate-containing foods (sugar). Each form of the disease has its own list of prohibited and permitted foods, which the attending physician talks about in more detail when making prescriptions for a specific small patient. Only by following all his recommendations is it possible to achieve the baby’s recovery in a shorter time.
List of foods prohibited for all forms of illness
For almost six months, the nutrition of a child who has suffered an attack of acute or reactive pancreatitis, as well as another relapse of chronic pancreatitis, should be approached very strictly and prohibited foods should not be allowed to appear on the menu. These include:
- smoked fish and meat,
- any sausages,
- all kinds of canned food,
- fresh vegetables and fruits,
- hot spices,
- mushrooms.
It is strictly unacceptable for children with any form of pancreatitis to consume so-called fast food and instant noodles. These dishes contain a very large amount of flavor enhancers, dyes and preservatives that are dangerous to the pancreas and can significantly increase its functioning.
You should also significantly limit foods that have a high fat content (it is permissible to consume them, but in very rare cases and in minimal portions), fruits and vegetables with a sour or spicy taste.
List of foods that should not be used for acute and chronic symptoms
Children, as well as adult patients with primary inflammation of the pancreas or its relapse, in order to avoid increasing severe symptoms of the disease, should under no circumstances eat foods from the following list:
- canned, spicy and spicy foods,
- pickled, spicy and salty foods,
- fried and fatty foods,
- strong meat broths,
- sour and spicy vegetables and fruits,
- chocolate, baked goods.
As for drinks, it is necessary to completely remove all types of sweet soda, kvass, strong tea, and coffee from the children’s diet. Eliminating these products from the menu will help ease the work of the pancreas and speed up the onset of remission in the child.
How should a baby eat during the recovery period?
After relief of acute symptoms, the diet of children with pancreatic disease begins to gradually expand. New foods are included in the diet in minimal portions, and in case of any negative reaction from the pancreas, they must be completely excluded from the diet. And also during the child’s recovery, it is necessary to strictly adhere to the following rules for preparing and eating food:
- eating should be frequent, but in small portions,
- food must be boiled in water or steamed, stewed and baked,
- All prepared dishes should be thoroughly chopped and cooled to room temperature before serving.
This will avoid overloading the pancreas, and will also reduce the risk of additional thermal or mechanical damage to the mucous membrane of the digestive organ. During the recovery period, you can occasionally please your baby with berries such as strawberries or raspberries, which are strictly prohibited during the acute period of the disease. It also becomes acceptable to add a little (no more than 5 grams per serving) butter to porridge. But in this case, it is necessary to pay attention to the quality of the product, since the use of the spread by a recovering baby is categorically not recommended.
Menu (what products to make it from)
Of course, it is important for parents to know what dishes can be prepared and served, when the diet is prescribed for children (during illness, remission), what is the approximate menu for the week, how to correctly compose it so that children of different years receive with food everything they need according to their age nutrients.
List of products and dishes that are recommended to make up the daily diet of a sick child:
- Soups (vegetarian based on vegetables such as carrots, potatoes, zucchini, pumpkin; with the addition of herbs, cereals, a little butter, low-fat sour cream);
- Lean varieties of meat, poultry, fish (beef, veal, chicken, turkey, rabbit. Dishes should be served in small portions, finely chopped, boiled, steamed, baked).
- Low-fat milk (cottage cheese, milk, yogurt, kefir) in the form of casseroles, puddings, souffles, lazy dumplings.
- Omelettes made with egg whites. The yolk itself occasionally, a couple of times a week.
- Vegetables only in grated form, boiled, baked, stewed. For example, you can combine cauliflower, zucchini, potatoes, carrots, beets, pumpkin and green peas (not canned).
- Porridges based on various cereals (with the exception of millet and pearl barley). They should be boiled, preferably even slimy, cooked in water (with the addition of a small piece of butter). During the recovery period, pasta is also allowed.
- Fruits are ground, baked, always ripe, soft and not sour varieties (pears, apples). Based on them, you can cook compotes, and also add dried fruits for taste and benefits. You can make jellies and mousses.
- From sweets: dry cookies, bagels, bagels, crackers.
- Drinks: weak teas, preferably green, based on herbs, rosehip infusion, fresh, squeezed juices, not concentrated (with the addition of water), compotes.
Based, approximately, on this list, you can and should create a diet for your child; recipes for interesting dishes can be found on the Internet. The menu must be thought out in advance, preferably a week in advance.
Stick to the diet for as long as the doctor advises, and then gradually switch to a more familiar diet, but keep it under control, making sure that the disease does not return to your child again.
A lot depends on us, parents: what foods and dishes we teach our children from birth, whether we control where our children spend their pocket money, whether we worry about whether they eat on time, etc. Take care of the health of your children from a young age!
Nutrition in case of reactive pancreatitis
Quite often, after a small child eats unhealthy or heavy food, he develops negative signs indicating the onset of an inflammatory process in the pancreas. This usually indicates the development of reactive pancreatitis. It always occurs due to poor quality food or food that irritates the mucous membrane of the digestive tract and occurs only in an acute form. In order to get rid of negative symptoms, first of all you should adjust the child’s diet. To do this, experts recommend transferring the baby to table No. 5.
With reactive pancreatitis, children are prescribed a strict diet in the first week of illness. Subsequently, the diet expands to normal throughout the month, but with some restrictions.
If a pathological condition of this form develops in the pancreas, children can eat the following food without fear of exacerbation of the disease:
- steamed protein omelettes or soft-boiled eggs,
- low fat dairy and fermented milk products,
- slimy soups with vegetable broths,
- steamed or baked dishes from lean fish or meat,
- porridge with buttermilk or water,
- vegetable puree.
Children who have suffered an attack of reactive inflammation of the pancreas are strictly prohibited from eating fast food and adding large amounts of spices and salt to their dishes. It is also recommended to limit to a minimum the consumption of sweet, refined foods, which include cakes and pastries so beloved by children. Nutritionists advise parents to pay attention to such a nuance of the diet as protein deficiency. Due to the fact that the pancreas secretory organ reacts positively to protein, it is necessary to increase the number of dishes made from cottage cheese, lean varieties of fish or meat, and kefir in the daily menu.
In the case when the child is under one year old and is breastfed, the mother should monitor the diet, avoiding any errors in her diet. And you should also not give your baby new complementary foods without consulting a pediatrician. This will make feeding the baby safe and will prevent the recurrence of severe symptoms of reactive pancreatitis.
Therapeutic dietary food for children under three years of age
Babies of this age should receive a diet that is completely free of potentially harmful foods.
The diet for pancreatitis in a child who has not yet turned 3 years old excludes freshly prepared juices, as well as the consumption of berries and fruits with rough skin (remove it), citrus fruits and raw vegetables.
Even during periods of improvement, food is ground or crushed. This is explained by the fact that children at this age do not yet know how to chew it well, and large pieces of food will be slowly digested in the gastrointestinal tract and burden the pancreas with work.
An example of a menu during a period without exacerbation of the disease
- Breakfast. Steamed egg white omelette, oatmeal, cereal coffee with milk.
- Lunch. Low-fat cottage cheese or light cottage cheese casserole.
- Dinner. Rice puree soup with vegetable broth with the addition of sour cream (no more than 1 tsp). If desired, you can add fresh dill to the dish. Steam cutlet or beef soufflé, berry jelly.
- Afternoon snack. Rosehip drink with 1 tsp. honey, biscuits or white crackers.
- Dinner. Steamed cod cutlet with carrot and potato puree, baked apple without peel.
- Before bedtime. Low-fat kefir, a slice of dried white bread.
Sample menu during the period of non-exacerbation of the disease
After the acute attack subsides, the child’s diet gradually expands. But at the same time, it is necessary to take into account that the baby’s daily menu should be compiled taking into account the basic nutritional rules that are recommended by nutritionists for this disease. And also we should not forget that the dishes should not contain those products that can lead to complications of the disease. When creating a menu for a child with pancreatitis, you can rely on the following list of allowed dishes:
- Breakfast . In the morning, it is best for your baby to prepare porridge, steam omelet or curd soufflé. You can also offer your child to eat a soft-boiled egg. Children will also like baked apples stuffed with rice during breakfast. Moreover, this fruit is doubly useful for diseases of the gastrointestinal tract - it contains large quantities of iron, which is necessary for the spleen and improves blood composition.
- Lunch . It is a snack between the first and second main meals. A good option here would be fruit puree from fruits approved by the gastroenterologist, crackers, biscuits and a cup of jelly.
- Dinner . A must-have dish is soup. It can be cereal, vegetable, fish or meat. But in the last two options, it is necessary to take into account that meat and fish must be of lean varieties. For the second course, kids enjoy steamed cutlets and meatballs in milk sauce with side dishes of cereals or pasta.
- Afternoon snack . A good option for this snack would be a glass of milk with dry cookies. You can also offer your baby to drink rosehip decoction, jelly, weakly brewed tea, or eat low-fat yogurt.
- Dinner . It should not be dense, so nutritionists recommend that children with pancreatitis eat vegetable stew, buckwheat cooked in water, a piece of boiled chicken or fish in the evening meal.
- Before going to bed , kefir is the best option; you just need to remember that it must be alive, that is, its shelf life cannot exceed 7 days.
The dishes listed above can be combined at your discretion and made up of different types of menus. This will make your baby's table varied and prevent him from losing interest in food.
A few simple tasty and healthy recipes
As already mentioned, children are always picky about food and can refuse any healthy food that they do not like. That is why gastroenterologists recommend approaching the preparation of a children's dietary menu very carefully and showing maximum imagination when preparing foods for a sick child. There are several original and tasty recipes that are completely safe for any gastrointestinal diseases. Most often they are advised to be included in the menu for children whose pancreas (pancreatitis) or gallbladder (cholecystitis) is inflamed:
Rice porridge with pumpkin
Peeled pumpkin (0.5 kg), cut into small pieces, is poured with water so that it lightly covers the healthy summer vegetable, and boiled until soft. Salt and sugar are added in minimal quantities, just to slightly flavor the taste. After the pumpkin becomes soft enough, add 7 tbsp. l. rice and continue to cook over low heat until done. After there is practically no water left in the porridge, pour a glass of boiling milk into it, close the lid, remove from the heat and leave for half an hour to heat.
Carrot soup with semolina
Any picky little one will love this soup and will firmly become part of the family menu even after the baby recovers. To prepare it, 250 grams of carrots are stewed. After the vegetable is ready, it is cooled and thoroughly chopped, and in another bowl at this time, 2 tbsp is boiled in half a liter of water-milk mixture. l. semolina. As soon as the semolina base is ready, add grated carrots and a small amount of sugar and salt. The fully assembled dish is kept on the fire for no more than 2 minutes.
Fish quenelles
The fish fillet is scrolled in a meat grinder with the smallest grid. To the resulting minced meat add white bread soaked in milk, an egg and a little salt. Dip the finished mixture into boiling water with a tablespoon and cook for 20 minutes.
Banana cake
All children have a sweet tooth, so mothers want to pamper them with something tasty. But since with pancreatitis it is forbidden to consume culinary masterpieces in the form of cakes and pastries, you should use a little imagination and prepare a delicacy from fruits allowed for this disease. Moreover, it is very simple. Gelatin is soaked in cold water, and after it swells, mixed with low-fat yogurt without preservatives and mashed banana. A layer of dry cookies is placed on the bottom of the mold, and a banana-yogurt mixture is placed on it. The hostess decides how many delicious layers to make. The finished semi-finished product is placed in the refrigerator for half an hour to harden, and then served.
Oatmeal jelly
Oatmeal jelly is also very useful for children with pancreatitis. Regular use of it will allow you to launch restoration processes in the pancreas, which will quickly improve the general condition of the baby.
The recipe for this dish is very simple. A handful of oatmeal is soaked overnight in half a liter of cold water. In the morning, the infusion is filtered, squeezed out and brought to a boil over low heat, with constant stirring. After boiling, the jelly is removed from the stove and left for an hour. But this healthy drink should only be taken slightly warm, since a hot or cold drink can cause significant harm to the digestive organs instead of benefiting it.
General principles of nutrition
A key role in diseases of the gastrointestinal tract is played by therapeutic nutrition: the load on the digestive organs is reduced, and the volume of secreted enzymes is reduced. All this allows you to preserve the functions of various organs of the gastrointestinal tract and helps the body independently fight inflammation.
Portions should be small (fractional nature of food consumption): the frequency of feedings depends on the age of the child, on average 4-5 times. The intervals between feedings are 3-4 hours; it is important to follow a meal schedule. Thanks to this, pain subsides and the enzymatic function of organs improves.
At the very beginning of the acute process (1-2 days), it is recommended to observe complete fasting; hunger is applied to the area of gland projection. Fasting is not prescribed for children under three years of age, since their bodies are extremely sensitive to the lack of food.
Hunger
For several weeks, all food consumed should be prepared in accordance with the recommendations and served to the child in liquid or mushy form for comfortable digestion.
When choosing a method of preparing food, preference is given to baking in the oven, boiling and steaming.
The optimal food temperature is 35-40 degrees. Too hot or cold food has an irritating effect on the digestive tract and can worsen the child's condition.
It is recommended to saturate your diet with foods that are rich in protein. These include meat and poultry, cottage cheese, milk, fish. Carbohydrates, and especially fatty foods, are limited.
If the child’s illness is severe, there is a need to hospitalize him in a specialized department of a medical institution, where, according to indications, parenteral nutrition with nutritional mixtures is prescribed.
What do parents need to know?
In addition to following the rules for preparing and eating food for children with pancreatitis, there are some other nuances that parents should know in order to prevent accidental errors in the baby’s diet:
- Children of preschool age attend preschool institutions. In kindergartens, although exclusively dietary food is prepared, this food is not suitable for children with pancreatitis. Therefore, the mother should warn the teacher that the child has some dietary restrictions. You also need to give the baby’s medical record with the recommendations indicated in it to the nurse of the preschool institution.
- Sometimes, when children follow a gentle diet, a situation arises when children are invited to a birthday or holiday. It is under no circumstances recommended to skip such an event due to dietary restrictions, as this will negatively affect the social adaptation of a small child. In this case, in order to avoid dietary or psychological problems, you need to talk in advance with the parents of the inviting child about the diet prescribed by the doctor.
But gastroenterologists also recommend that mothers remember that new foods should be introduced into the diet of babies suffering from pancreatic problems with extreme caution. The initial portions are made tiny, not exceeding 5–10 grams, and if negative symptoms appear, they are immediately removed from the diet. But after some time, they try to introduce the removed product into the menu again. It is excluded completely only when the baby’s body shows a negative reaction for the second time.
Bibliography
- Baranov A.A. Problems of pediatric enterology at the present stage. Russian Gastroenterological Journal 1995 No. 1 pp. 7–11.
- Baranov A.A., Klimanskaya E.V., Rimarchuk G.V. Pediatric gastroenterology. M., 2002
- Zikeeva V.K. Therapeutic nutrition for acute and chronic pancreatitis. In the book “Handbook of Dietetics”, edited by V.A. Tutelyan, M.A. Samsonova. - 3rd ed., M., Medicine. 2002 pp. 209–217.
- Plotnikova T.V. Recipes of dishes for children's institutions. Phoenix 2013
- Ilyin V.F., Therapeutic diets for pancreatitis and other diseases of the pancreas. M.: Vector, 2010.
- Zikeeva V.K. Therapeutic nutrition for acute and chronic pancreatitis. Handbook of Dietetics edited by V.A. Tutulyana, M.A. Samsonova. 3rd ed., M.: Medicine, 2002, pp. 209–217.
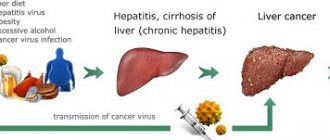
Development of chronic pancreatitis
Constant overeating and love of fatty foods increase the likelihood of developing in adults . The habit of drinking alcohol is a powerful factor in disrupting the functioning of the organ, since the constant presence of alcohol in the blood results in a change in the composition of gastric juice, its production is reduced. In both cases, conditions are created for the development of the inflammatory process.
There are several forms of the disease:
- painful – the pain is constant and intensifies during periods of exacerbation;
- recurrent – pain appears only during exacerbation;
- asymptomatic;
- pseudotumor - an increase in the size of the gland as a result of germination by fibrous tissue.
The variety is determined by symptoms. In chronic pancreatitis, tissue changes occur slowly but constantly. If left untreated, the entire organ is affected.
Symptoms:
- pain under the ribs during active movement or playing sports;
- attacks of aversion to food, especially fatty foods;
- frequent digestive disorders;
- losing weight too quickly;
- lack of appetite.
How is pancreatitis diagnosed?
If you experience chronic discomfort, pain, or indigestion, it is recommended that you visit your doctor to take action. Tests are prescribed to determine the level of bilirubin, serum enzymes, and insulin.
Examinations are carried out according to indications:
- ultrasonic
- fibrogatroduodenoscopy
- chest x-ray
- angiographic examination
- tomography
- laparoscopy.
During examination, the color of the skin and mucous membranes is recorded.
Treatment of the inflammatory process
The disease in its advanced form is life-threatening, since disruption of the normal amount of enzymes produced by the gland can destroy tissue. This leads to toxic poisoning and disruption of blood vessels.
Appointed:
- intravenous infusions to normalize blood composition;
- painkillers;
- medications to block excess enzymes;
- vitamins;
- strict diet.
Approximate diet
A weekly diet menu for a child with pancreatitis may be as follows:
- For breakfast, prepare pureed oatmeal, semolina porridge, and egg white omelette. You cannot add salt, sugar, or butter to porridge. As for drinks, it is better to give preference to rosehip decoction or unsweetened tea.
- For second breakfast, warm alkaline water with a couple of slices of toasted bread is great.
- For lunch you need to prepare soup from rice and mashed potatoes or mashed buckwheat, mashed boiled carrots. Drink with weak unsweetened tea.
- The afternoon snack includes still mineral water and two crackers.
- Dinner should consist of a small portion of rice porridge, diluted with two tbsp. l. milk. Wash down with apple compote without sugar.
- At night, just before going to bed, apple jelly is perfect.
A properly designed diet menu will provide the child with all the necessary vitamins and minerals, and also act as a therapeutic therapy, accelerating recovery
After 5 days, you can add to the diet of a child with pancreatitis:
- mashed potatoes with a minimum amount of butter and milk;
- mashed cottage cheese;
- beef cutlets, soufflé;
- boiled chicken fillet;
- For an afternoon snack, you can pamper your child with dry cookies, but no more than 3 pieces, or oven-baked apples.
Healthy recipes
Healthy recipes for pancreatitis will help parents expand their child’s diet.
Puree vegetable soup. You will need: 1 small zucchini, 100 grams of pumpkin, 2-3 potatoes, 1 medium carrot. All vegetables must be peeled, cut into pieces and simmered over low heat for 30-40 minutes. Then grind with a mixer or masher, add salt, and boil again.
Oatmeal jelly. You will need: 200 grams of flakes and water. Place the flakes in water and leave for 10-15 minutes to swell. Then put on the stove and cook for 40 minutes over medium heat. Strain the broth into a separate container, rub the porridge through a sieve, add to the broth and mix. Boil again for 5 minutes. Then cool and serve. Cook jelly in milk.
Soufflé with rice and chicken. You will need: chicken 300 grams, milk 100 ml, chicken egg, rice 100 grams, salt. Boil the rice until half cooked. Chop the meat and put it in a blender along with rice, milk, egg and beat. Add salt and beat again. Bake in the oven at 180˚C for 40-45 minutes.