Classification of gastric antrum cancer
In medicine there are several classifications of gastropathy.
Gastropathy is divided according to the type of course (acute and chronic), by stages, and by degrees of development. According to the degree of development, gastropathy can be:
- 1st degree. Manifests itself in slight deformation of the gastric mucosa, in a slight decrease in the synthesis of hydrochloric acid;
- 2nd degree. It is characterized by the appearance of stronger pathological processes, in which cell damage and necrosis of the gastric epithelium occurs faster than in the first case. These processes can be reversed with timely treatment.
The stage of gastropathy depends on its duration, the nature of its course, the effectiveness of treatment, and the condition of the gastric epithelium. The following stages of gastropathy can be distinguished:
- Initial - characterized by a slight inflammatory process of the mucous membrane without transformation of its structure.
- Chronic - at this stage, ulcers and erosions appear, the glands of the organ are affected. This stage occurs with advanced gastropathy - when the diagnosis was delayed or the treatment was incorrect.
- Atrophic - manifests itself in the degeneration of the gastric walls, replacement of certain areas with connective tissue, and poor health.
- Hypertrophic is the most severe stage, during which thickening and coarsening of the gastric walls occurs, adenomas and cysts form.
According to its form, gastropathy can be divided into:
- spicy. It appears when the stomach is affected by infections, alcoholic beverages, acids, alkalis;
- chronic. It is characterized by a slow course with a gradual transformation of the epithelium of the organ, its atrophy, and a decrease in the functions of the stomach. Often this form of gastropathy is asymptomatic;
- moderate. It is characterized by the degeneration of epithelial cells into connective tissue.
Antral
This type of gastropathy occurs in the antrum of the stomach, where food is crushed and subsequently moved into the duodenum. This type of gastropathy helps to reduce the rate of food processing, which causes food stagnation and fermentation. The patient feels heaviness and pain. Delayed treatment can lead to the appearance of ulcers, which can be treated well.
This type is caused by the use of non-steroidal anti-inflammatory drugs (NSAIDs). Such drugs can cause damage to the mucous membrane of the digestive organ, the formation of ulcers and erosions, bleeding, and provoke obstruction of the organ. Often these types of gastropathy are asymptomatic, so they are mainly discovered when complications have already developed.
Hyperemic
With this type of gastropathy, there is an influx of blood to the stomach, redness of the mucous membrane, swelling, and bruising occur. This form of gastropathy can spread to individual parts of the organ or to small areas of it.
Hyperplastic
There is a strong increase in the number of cells of the gastric glands, stomach tissue grows, folds and growths appear inside the organ. This form of pathology includes hypersecretory gastritis, Menetrier syndrome, Zollinger-Ellison disease.
Diffuse
Gastropathy of this type spreads to the entire gastric body, structural changes occur in the mucous membrane of the organ, the symptoms are similar to those of gastritis. This type of gastropathy can have an acute or chronic course.
Stagnant
This type of gastropathy is characterized by a malfunction of the gastrointestinal tract, the appearance of erosions and ulcers in the antrum of the stomach and in its upper section. The occurring disturbances in the blood supply system of the stomach originate from the negative effects of alcohol and nicotine, as well as the activity of Helicobacter pylori.
Grainy
Growths in the form of grains form (their size can be from several mm to cm) on the gastric walls. Gastropathy is more often found in men after forty years of age. The early stage of gastropathy is usually asymptomatic; further development leads to disruption of protein metabolism.
Catarrhal
Catarrhal superficial gastropathy is one of the simplest types of pathology, in which inflammation spreads only to the upper layer of the organ mucosa. There is an increase in the synthesis of hydrochloric acid, or its deficiency. The cause of this type of gastropathy is injury, food poisoning.
This form belongs to rare types of gastropathy. It is characterized by the appearance on the epithelium of the organ of lymphocytes that look like follicles. The cause of this form of gastropathy is the influence of Helicobacter pylori, which provokes the proliferation of lymphoid tissue.
Papular
It manifests itself as erosion that does not affect the deep layers of the gastric epithelium. With pathology, papules form in different parts of the digestive organ, which can be either single or multiple formations.
Portal
Appears due to vasodilation - pressure in the veins increases, capillaries expand, filling with blood, mosaic patterns, red fragments or a black-brown pattern may appear on the mucous membrane, characterized by the absence of inflammation.
The main cause of this type of gastropathy is considered to be bile reflux and prolonged use of NSAIDs. This form occurs more often in patients who have undergone gastric surgery.
Erosive
This type occurs when various factors influence the mucous membrane, characterized by the presence of erosions ranging in size from 1 to 7 centimeters, they resemble pimples in appearance with a depression. The disease may develop without symptoms or with slight pain on the right side in the hypochondrium; gastric bleeding is acceptable.
Erythematous
It is redness of the mucous membrane and is determined using endoscopic examination. It is possible to distinguish between focal, covering one or several zones of the stomach, and widespread, which covers the entire surface of the organ or most of it. Focal gastropathy occurs in the absence of symptoms; if it is more widespread, sensations inherent in gastritis may appear, namely: heaviness and pain in the epigastric area, a feeling of fullness in the stomach, heartburn, belching, and general weakness.
Ulcerative
This form is characterized by the presence of symptoms, as in intoxication. If blood clots are found in the vomit, be sure to consult a doctor.
Mixed
In some cases, patients may develop several forms simultaneously. Most often observed: superficial, erosive, hypertrophic and hemorrhagic gastropathy.
Uremic
This form appears in patients with chronic renal failure.
Exudative
This is a rare disease, it consists in the formation of deep folds on the gastric wall, the height of some can be 3-3.5 cm, in addition, the main and parietal cells decrease, and the number of cells that produce mucus increases. The reasons for the appearance of this form of gastropathy are not well understood.
According to the morphological classification of formations in the antrum of the organ, there can be three types, depending on the tissues from which the tumor arose:
- adenocarcinoma is the most common form, which occurs in 90% of patients and consists of glandular tissue;
- squamous cell carcinoma;
- small cell;
- glandular-squamous;
- undifferentiated.
There are 2 types of growth of stomach tumors: exophytic and endophytic. The type of cancer growth in the antrum is mainly exophytic (infiltrative), that is, it does not have clear boundaries, and is also particularly malignant with rapid metastasis. According to Professor of Cancer Pathology A.A.
What are gastrointestinal papules
When talking about the gastric mucosa, you can often hear the term gastric papule. These are superficial defects in the mucous membrane of the stomach or duodenum. Such defects do not involve muscle mass in the process and heal on their own without scarring. they are also called gastroduodenal erosions.
In 1761, these diseases were first described by the Italian scientist - pathologist Morgagni in his work on anatomy.
To date, 15% of patients who have undergone endoscopic examination are diagnosed with gastric papules and defects of the duodenal mucosa.
Types of papules
The term papule means an erosive formation. From here it becomes clear what gastric papules are, these are other forms of erosion on the gastric mucosa.
The duration of the disease directly depends on the type of gastric papules. So there are: single and multiple, acute and chronic, polypoid or flat, polygonal papules, bleeding, hemorrhagic, primary, secondary and malignant erosions.
Papules of the antrum of the stomach (chronic erosion) are characterized by the longest period, more than 4-5 years. Localization occurs in the outlet section of the stomach.
If gastric erosion is combined with duodenal erosion, then bleeding and relapses of the disease are characteristic.
Acute erosion, as a rule, heals within 10-12 days. Such erosions are localized mainly in the central part of the stomach. Only in extremely severe cases can such erosions develop into purple papules and take up to 8 weeks to heal.
Primary papules differ from secondary ones in that they resolve as an independent disease of the organ. Secondary papules occur with damage to the liver, cardiovascular system and many other diseases.
With Crohn's disease or cancer, a malignant papule occurs.
If the aphthous papule progresses, it will lead to a stomach ulcer.
Reasons for appearance
In fact, there are many reasons for the appearance of papules in the stomach. First of all, it should be noted that medications are taken that upset the balance between the aggressive and protective environment of the stomach. Papules may appear after mesotherapy. In addition, stomach imbalance is caused by:
- various abdominal injuries;
- operations on the gastrointestinal tract;
- psychological and emotional disorders;
- smoking;
- systematic exposure to heavy metals and salts;
- diabetes mellitus, sepsis and other diseases of the endocrine system;
- burns of the mucous membrane, which are promoted by spicy, hot food, alcohol.
Symptoms
In 30% - 90% of young people, aphthous papules can be asymptomatic or with very few symptoms. If we talk about chronic erosion, the symptoms are very similar to ulcerative ones.
It is worth paying attention to the frequently repeated ones:
- sour belching or heartburn;
- digestive disorders, including frequent constipation;
- disorder of the biliary system;
- feeling of heaviness, often in the right hypochondrium
When diagnosing erosion, anemia is often detected due to blood loss (occult blood in the stool) and loss of apatite. Patients often experience brittle hair and nails, as well as dry skin and mucous membranes, which occurs due to disruption of the process of toxin waste.
Treatment
Most doctors recommend complex therapy in the treatment of gastric papules, taking into account all the versatility of this pathology.
Usually the treatment process is long and uses endoscopic control.
Standard methods include antiulcer therapy using H2 blockers and proton pump inhibitor drugs. If the patient is diagnosed with the microorganism Helicobacter pylori, then antibiotics are included in the treatment.
Cytoprotective drugs are used to accelerate the healing process of the mucosa. And exposure to low-intensity laser improves blood microcirculation in the affected areas.
Laser treatment is carried out only in a hospital setting.
Nutrition during treatment
For stomach treatment to be successful, proper nutrition is an important factor.
First of all, it is recommended to eat small portions up to 6 times a day, but not less than 4. It is advisable to steam dishes. Kissel, semolina porridge, steamed cutlets, soft-boiled eggs, oatmeal are considered traditional dishes in the treatment of stomach papules. Low-fat cheese, sour cream, and milk are also important elements of the diet. It is these products that help produce enzymes that promote rapid healing of the affected areas.
The following should be strictly excluded from the diet:
- strong coffee or tea;
- hot or cold food;
- citrus juices;
- fried foods;
- alcohol;
- coarse fiber dishes (muesli, stringy meat, turnips, etc.)
- any spicy dishes.
It is also important to remember that for successful treatment you should avoid any stressful situations.
Reasons for the development of pathology
The impetus for the formation of papillomas is usually an inflammatory process in the organ. In turn, inflammation can be triggered by:
- improper, irregular diet;
- infection;
- hormonal imbalance;
- damage to the mucous membrane;
- low immunity.
Atypical proliferation of cells and their transformation into papillomas on the skin and on the mucous membranes of the mouth, nasopharynx, and stomach is caused by a viral infection. The size of papillomas can reach 3 cm. Gastric papillitis has its own characteristics, for example, erosive and chronic forms, localization of the accumulation of neoplasms in the bends, and a slight danger at the initial stage.
One of the factors that influence the development of cancer in the stomach is nutrition, in particular, the consumption of fatty, fried foods, smoked foods, and a lot of salt.
A connection between stomach tumors and the bacterium Helicobacter pylori has been proven. This microorganism is capable of causing infiltrative gastritis with cell proliferation, and such an environment is suitable for cancerous degeneration. According to statistics, people infected with Helicobacter pylori have a 3-4 times higher risk of developing cancer than healthy people.
Another infectious agent that possibly causes malignant transformation is the Epstein-Barr virus.
Smoking and drinking alcohol play an important role in the etiology of gastric carcinomas.
There are precancerous diseases that almost always cause cancer if nothing is done.
These include:
- polyps and polyposis of the stomach;
- colloid ulcer;
- rigid antral gastritis.
Rarely, oncology occurs in chronic atrophic gastritis, flat adenoma, pernicious anemia, Ménétrier's disease, and also after gastric surgery.
The causes of the disease can be divided into internal and external. The general list of reasons looks like this:
- improper diet;
- reflux of bile into the stomach;
- abuse of alcoholic beverages, strong coffee;
- burns and other injuries;
- stagnant processes;
- smoking;
- presence of infections;
- lack of enzymes in the body necessary for digestion;
- long-term use of medications;
- the formation of internal pathologies and the resulting incomplete blood supply;
- genetic predisposition;
- age over 50 years;
- hormonal changes occurring in the body.
Ulcers
Ulcerative lesions of the antrum are possible after the stage of inflammation, when focal atrophy of the mucosa passes through the stage of erosion to deep damage to the submucosal and muscular layers.
Ulcers located in the antrum account for up to 10% of all gastric ulcers
In addition to inflammation, the mechanisms of the disease include:
- low contractile function of the antrum;
- stagnation and fermentation of the food bolus;
- increased enzyme production.
The presence of risk factors provokes the transition of inflammation into an ulcer. Typical symptoms:
- pain in the epigastric region, becoming more intense at night;
- constant heartburn;
- nausea and vomiting;
- belching after eating;
- blood impurities in stool and vomit.
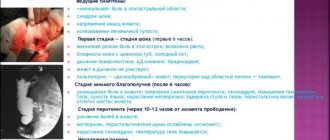
Symptoms of gastric antrum cancer
At the very beginning, the disease may not show any symptoms. Some time later, gastropathy may manifest itself with symptoms similar to gastritis - pain, heaviness in the stomach, flatulence, nausea, heartburn.
In addition, the following changes occur:
- appetite is impaired;
- vomiting may occur, bringing relief;
- In some patients, bile synthesis may be impaired;
- disturbance of intestinal tone, constipation occurs.
With pathologies of the antrum, bleeding may occur - the stool becomes reddish in color, and blood impurities appear in the vomit.
The erosive form may have the following symptoms:
- sour belching;
- heartburn;
- smell from the mouth;
- “gurgling” in the stomach;
- nausea, urge to vomit;
- epigastric pain.
Advanced papillitis becomes chronic and may degenerate into cancer. The chronic form is characterized by more dangerous conditions and symptoms:
- weakness, fatigue;
- rapid saturation with food, a feeling of a full stomach, heaviness in it;
- increased epigastric pain during and after eating;
- bloating;
- unpleasant taste in the mouth;
- unstable stool (diarrhea alternates with constipation);
- the pain can be either aching or sharp.
Additional symptoms in case of anemia due to gastric bleeding may include: dry, brittle hair and nails; pale skin; rapid heartbeat, shortness of breath; headache, dizziness; hair loss. These are not characteristic signs of papillitis, but they may indicate its presence.
Compared to neoplasms in other areas of the stomach, when localized in the antrum, symptoms occur quite quickly. Located in the lower part of the organ, the neoplasm progresses and spreads to the pylorus, which in turn makes it difficult for the digested mass to exit.
Lingering and decomposing in the stomach, it causes:
- feeling of a full stomach;
- belching with an unpleasant odor;
- heartburn;
- bloating;
- nausea;
- vomiting, which patients subsequently induce often themselves, unable to withstand the unpleasant symptoms.
Evacuation disorders initially occur only periodically, during the intake of heavy food or alcohol. When obstruction of the outlet section develops, abdominal pain and vomiting suddenly appear. It is noteworthy that if you follow a diet, these symptoms may temporarily subside.
For gastric stenosis, the typical picture is a relatively satisfactory state of a person in the morning, when the stomach is empty, and a deterioration in the condition with each meal. In the evening - nausea and vomiting, which brings relief.
Due to the lack of necessary microelements entering the body, intoxication occurs; patients quickly lose their appetite or completely refuse to eat. This leads to exhaustion, dehydration, loss of performance, irritability and depression.
All these symptoms cause sudden weight loss, even anorexia.
There are cases when oncology is not accompanied by obstruction, but the pylorus, infiltrated by the tumor, loses its functional abilities, as a result of which food from the stomach quickly falls into the intestines. Then the symptoms of gastric antrum cancer include a constant feeling of hunger. Patients eat, cannot eat enough and do not gain weight. The stool is frequent, liquid, with undigested food.
Tumors of the exophytic type often undergo ulceration (disintegration), which causes bleeding from the vessels into the lumen of the stomach.
The blood resulting from tissue breakdown is constantly filled with toxic elements, which causes:
- fever;
- increased body temperature;
- vomiting with blood;
- tar-colored stool with hidden blood.
Due to the reduction of the stomach due to the enlarged tumor, the organ shrinks and decreases in size.
In this case, the patient feels:
- pressure;
- bursting feeling;
- heaviness after eating;
- satiation from a small amount of food.
Further symptoms in the later stages of the disease no longer depend much on damage to the main organ. To these are added signs that occur after metastasis and the appearance of secondary foci in other organs.
Features of antrum polyps
Antral polyps are benign growths of epithelial tissue that grow inward. Almost 3 out of 10 polyps occur in the antrum of the stomach.
The growths can be single or multiple in nature, have a stalk or a flat wide base.
The main types are as follows:
- Peutz-Jeghers neoplasms;
- Adenomatous polyps of the stomach;
- Inflammatory polyps.
The hereditary factor is an important aspect in the formation of antral polyps. These neoplasms rarely arise on healthy tissue, therefore they are more of a secondary nature, formed as a result of an underlying disease of the epigastric organs.
Treatment
Any benign neoplasm, especially papilloma, can, under certain conditions, develop into malignant. This is the main danger of the disease. This condition becomes especially threatening in the absence of clinical signs or late diagnosis.
After determining the exact diagnosis and studying the number, location, and characteristics of papillomas, they are removed - resection. It is performed using a metal loop equipped with a gastroscope. Before inserting the device through the oral cavity into the esophagus, it is anesthetized with Lidocaine. In case of an allergic reaction to the drug, it is replaced with another anesthetic.
Pain relief is necessary not only to relieve discomfort, but also to prevent vomiting. Then the patient is placed on his left side with his knees tucked to his stomach. The day before the procedure, the patient must stop eating. The patient's stomach must be empty before surgery.
Medium-sized pedunculated papillomas are removed using a metal loop. To remove large papillomas, complex abdominal surgery is required. Multiple small flat papillomas can be removed with a laser.
The success of treatment of gastric papillitis depends not only on the professionalism of the surgeon, but also on the successful treatment of the underlying disease that accompanies papillitis.
There are traditional methods for treating papillomas, but they should be used only after consultation with your doctor, with great caution, strictly observing or selecting the required dosage. The basic rule: monitor your health when using folk remedies and stop taking them at the slightest deterioration in your condition.
To treat papillitis use:
- Lilac color - 2 tablespoons per 1-1.5 liters of boiling water, leave for at least 6 hours. Take half a glass three times a day for a month.
- Celandine and calendula - 5 g of mixture per 0.5 liter of boiling water, leave for 4 hours. Take a tablespoon 3 times a day for a month.
- Burdock root - wash, chop, take 2 tbsp. l. for 2 glasses of water, boil for 5 minutes. Allow to cool and take the strained decoction in a glass while warm, no more than 3 glasses per day. The course of treatment is 2-2.5 months.
- Celandine - 1 teaspoon of dried plant, pour 0.5 liters of boiling water, simmer in a water bath or low heat for 10 minutes. Leave in a warm place for 5 hours without straining. Drink 1 tablespoon 3 times a day for 1 month. Do not forget that celandine is a poisonous plant for humans.
Treatment of gastric antrum cancer is a difficult task, given that 90% of patients are admitted with highly advanced tumors and in serious condition. In addition, most of them are elderly people, with heart disease or other concomitant pathologies.
Surgery is recognized as the best treatment method. Only it gives hope for recovery. For the antrum, in more than 60% of cases of radical surgery, total gastrectomy is used.
Patients are removed:
- the whole stomach;
- regional lymph nodes;
- fiber.
In the presence of distant metastases, resection of the affected organs.
If total surgery is contraindicated, then subtotal resection of the distal part of the stomach is performed. Many doctors advocate performing total lymph node dissection on all patients, that is, removal of the entire lymphatic system, in order to reduce the risk of recurrence. This approach increases survival rate by up to 25%!
After resection of part or all of the stomach, the remaining half or esophagus is connected to the intestine using an artificial anastomosis.
The few percent of patients whose tumor is diagnosed at stage 1 can undergo endoscopic resection. This operation is the least traumatic, but relapses also occur after it.
Patients who have contraindications to radical surgery are prescribed palliative surgeries designed to eliminate stenosis of the lower stomach. They can also create a bypass anastomosis from the stomach to the intestines.
Since surgical treatment options for gastric antral cancer are limited, doctors are developing more effective techniques, complementing surgery with radiation and chemotherapy, as well as various alternative methods.
Preoperative external beam radiation therapy is often used. Its goal is to damage malignant cells, stopping their growth. Preoperative radiation therapy for gastric cancer is carried out in the mode of large (single dose - 7-7.5 Gy) and enlarged (single focal dose - 4-5 Gy) fractionation.
During surgery for stomach cancer, intraoperative radiation therapy may be used. The tumor bed is irradiated once for 30 minutes with a dose of 20 Gy.
Postoperative irradiation is carried out in classical or dynamic fractionation modes, the total dose is 40-50 Gy.
The inclusion of chemotherapeutic drugs in the treatment complex is aimed at preventing relapses and the occurrence of new metastases. They are prescribed before and after surgery according to a specific scheme chosen by the doctor.
Here are some examples of standard chemotherapy regimens for stomach cancer:
- ECF regimen: Epirubicin - 50 mg/m2 intravenously for 1 day; Cisplatin - 60 mg/m2 intravenously for 1 day; 5-fluorouracil - 200 mg/m2 continuous infusion for 21 days.
- ELF regimen: Etoposide - 20 mg/m2 intravenously 50 min 1-3 days; Leucovorin - 300 mg/m2 intravenously 10 minutes 1-3 days; 5-fluorouracil - 500 mg/m2 intravenously 10 minutes 2-3 days.
The course prescribed before the operation is repeated several weeks after it, if the effectiveness of the selected drugs has been confirmed. If there are no positive results, then other cytostatics are selected. Complex treatment may include immunotherapy, the purpose of which is to activate the body's defenses to fight the cancer process.
Drug treatment is carried out using the following drugs:
- Antisecretory drugs: Kvamatel, Ranitidine, Famotidine.
- Proton pump inhibitors - Omeprazole, Esomeprazole, Lansoprazole.
- Gastrocytoprotectors that protect the mucous membrane from aggressive influences: Almagel, Maalox, Gastromax, Phosphalugel.
- Sorbents (for acute pathology): Enterosgel, Atoxil, activated carbon.
- Enzyme preparations that promote food digestion: “Creon”, “Mezim”, “Festal”.
- To improve gastric motility: Motilium, Cerucal.
- To relieve pain and relieve spasms, the following are prescribed: “No-shpu”, “Riabal”.
If Helicobacter bacteria are present in the body, anti-Helicobacter therapy is carried out, which includes taking the following drugs: Amoxicillin, Ornidazole, Metronidazole, Vikalin, De-Nol.
In addition, vitamin preparations are prescribed, since there is a lack of them in the body due to disruption of the digestive process.
The purpose of vitamin complexes depends on the type of gastropathy and stomach acidity. For the hypoacid type, vitamin E is prescribed; this vitamin is found in vegetable oil, fats, and milk. For low acidity, vitamins C (found in citrus fruits, rose hips, cabbage) and PP (in fish, meat) are prescribed.
Vitamin B6 deficiency may occur, which leads to metabolic disorders and nervous disorders. This vitamin is found in grain bread, beans, and peas. Lack of B12 can cause anemia; absorption of the vitamin occurs better together with folic acid, which is found in products of animal origin.
Surgical treatment is resorted to if it is not possible to relieve pain or stop gastric bleeding. The most commonly used method is the laparoscopic method, which is carried out using special instruments and does not deeply injure the organ tissue.
In addition to drug treatment, physiotherapy is used. The following methods help to get rid of the disease:
- vegetative corrective (aerotherapy, electrosleep);
- stabilization of secretion (drinking mineral waters, magnetic therapy);
- regenerative (infrared laser therapy, infrasound);
- anti-inflammatory (UHF, cryotherapy);
- antispasmodic (paraffin therapy, galvanization);
- immunomodulatory (magnetic therapy of the umbilical region and thymus gland);
- sedative (mineral and pine baths).
All diets recommended for pathology are based on the following principles:
- fragmentation of nutrition, its regularity, small size of consumed portions;
- quality of products, exclusion from the diet of fatty, spicy foods, freshly baked baked goods;
- eating dishes prepared using gentle methods - boiling or steaming;
- exclusion of cold and hot foods from the diet;
- refusal of sour vegetables and fruits when increased stomach acidity is diagnosed;
- avoidance of foods that increase gastric motility with reduced secretion.
In addition to drug treatment and diet, traditional methods of treatment can be used, but only in combination with the main treatment.
Dissolve a spoonful of honey in 1 tbsp. warm water and drink 20-30 minutes before meals.
Mix aloe juice with honey in equal proportions and consume a tablespoon before meals.
It is good to take propolis tincture in the amount of 30-40 drops on an empty stomach. This remedy has an antiseptic and healing effect.
In addition to honey products, sea buckthorn has a positive effect on the body in this disease. Sea buckthorn oil has anti-inflammatory, analgesic, and regenerating effects.
Herbal treatment is often used for this diagnosis. These are products prepared on the basis of chamomile, St. John's wort, calendula, sage, immortelle, thyme, string, plantain, flax seeds, oak bark and others. They can be brewed as tea and taken before meals, or you can buy ready-made preparations at the pharmacy and take according to the instructions.
What causes antrum diseases?
All variants of pathology of the antrum are united by a single most common cause - the presence of a special pathogen Helicobacter pylori or Helicobacter. The fact is that the antrum is the favorite location of this microorganism.
Human infection occurs through the mouth. And, once in the stomach, in the pyloric part the pathogen finds the most convenient conditions for life. It tolerates the acidity of gastric juice well. It independently neutralizes it with the help of enzymes that release ammonia. Actively reproducing.
Due to the presence of antennae, the bacterium is able to move in the gel-like environment of mucus. Excessive alkalization is considered a mechanism that triggers pathological changes in the antrum, which subsequently leads to stomach diseases.
In addition to Helicobacter, the following risk factors are involved in the pathology of the antrum:
- alcohol abuse;
- smoking;
- long-term use of irritating drugs (from the Aspirin group, non-steroidal anti-inflammatory drugs, against headaches, for the treatment of tuberculosis);
- commitment to violating the rules of nutrition (passion for spicy seasonings, fried and smoked foods, very hot or cold foods, fast food, disproportionately long breaks in eating);
- stressful conditions in the family, at work, contributing to the emergence of neuroses;
- general vascular changes with severe atherosclerosis, arteritis, diathesis, disrupting the nutrition of the stomach wall;
- infection with parasites (helminthiasis, amoebiasis, giardiasis);
- allergic reactions to food;
- exposure to viruses (HIV, cytomegalovirus);
- decreased immunity caused by various reasons;
- hereditary genetic predisposition.
There was a connection between the frequency of gastric damage and diseases of the endocrine organs, bronchi, lungs and heart, iron deficiency, diseases of the urinary system, as well as the presence of chronic foci of infection (tonsillitis, sinusitis, caries, adnexitis in women and others).
Chronic pathology is accompanied by suppression of the body's defenses. In combination with Helicobacter, these factors cause gastric damage of varying extent and depth. Let's consider the most common diseases with features of symptoms and treatment.
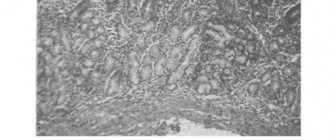
Diagnosis is based on identified morphological changes in tissues and endoscopic examination
Metastases in stomach cancer
As the neoplasm grows, it grows through the wall of the stomach and penetrates into the surrounding tissues. Such metastases are called implantation. Depending on the location of the tumor, it may invade the site or other neighboring organs. In the case of the antrum, the duodenum is more susceptible to metastases than others.
When cancer cells enter the lymphatic or blood vessels, lymphogenous and hematogenous metastasis is observed. Since the stomach has an extensive lymphatic network, spread by the lymphatic route occurs very quickly. This can happen already at the first stage.
First, the lymph nodes located in the ligamentous apparatus of the stomach are affected. Next, the process migrates to the lymph nodes located along the arterial trunks. Finally, metastases penetrate to distant lymph nodes and organs. Most often the liver, spleen, intestines, lungs, and pancreas are affected. Hematogenous metastases in gastric cancer are usually found in the lungs, kidneys, and brain. bones.
Secondary tumors are treated surgically. In infiltrative forms, preference is given to removing all lymph nodes susceptible to the appearance of metastases in them. The result is secured with chemotherapy, which helps destroy micrometastases - cancer cells located in the body.
Benign neoplasms of the antrum
Non-cancerous formations of the antrum include polyps and lymphofollicular hyperplasia. Polyps arise from the proliferation of glandular epithelial cells. The antrum accounts for 60% of all gastric polyps.
They are characterized by single growth or the formation of an entire colony. They differ in shape and size (up to 30 mm). Identified against the background of other stomach diseases. They pose a threat of cancerous degeneration. They practically do not give any symptoms. Pain is caused by eating disorders. They can become twisted or pinched, causing blood to appear in the stool.
Based on their origin, antral polyps are divided into three types:
- inflammatory - begin with lymphoid follicles (from 70 to 90%);
- adenomas - grow from the glandular epithelium;
- specific - neoplasms in Pattes-Jeghers-Touraine syndrome, which is a hereditary pathology including hyperpigmentation of the skin and polyposis of the intestines, stomach, differ in glandular structure, pigment content (melanin), and rarely - muscle fibers.
The first two types of polyps develop in old and senile age; specific ones are usually detected before the age of 30.
Pattes-Jeghers-Touraine syndrome is also characterized by the appearance of spots on the face (xanthomas), in which the melanin pigment is located at the level of the basal layer of the epidermis and in the mucous membrane. Pigmentation appears in childhood and may decrease or disappear with age.
Polyps can “sit on a stalk” or be attached with a wide base to the wall
Lymphofollicular hyperplasia is accompanied by the growth or formation of follicular tissue in the submucosal layer of the stomach. The disease has no age-related advantages. Among the reasons, in addition to those described above, a special place is given to:
- herpes infection;
- autoimmune diseases;
- endocrine disorders;
- contact with carcinogens.
It is important that, according to observations, this type of hyperplasia most often precedes the formation of polyps.
Diagnostics
Most patients come to the doctor when the disease is in an advanced stage. They experience severe digestive disorders, exhaustion, and weight loss. The tumor can be felt through the abdominal wall. Local and distant metastases can also be detected by palpation.
Laboratory tests include examining gastric juice and peripheral blood for tumor markers.
When the surgeon suspects cancer, he sends the patient an x-ray. To examine the stomach, contrast-enhanced radiography is used, when the patient has to drink a special substance to visualize the organ cavity in the pictures. In this way, a defect in the walls of the stomach and its filling is detected.
To obtain more accurate information about the nature of growth, localization and boundaries of the tumor in the organ, endoscopy is used. A flexible endoscope with a camera is inserted through the mouth into the stomach and inspected visually.
Next, a clarifying diagnosis is carried out to assess the prevalence of cancer in all organs and structures. To do this you will need to go through:
- Ultrasound and CT scan of the abdominal cavity and retroperitoneal space;
- skeletal scintigraphy;
- laparoscopy;
- angiography.
The decisive step in diagnosing stomach cancer is a biopsy. This is a procedure during which a piece of the tumor is taken for further microscopic examination and confirmation of its malignancy, as well as its histological type. A biopsy sample of a primary tumor is taken during an endoscopic examination, and from a secondary (metastatic) tumor - using a puncture biopsy or laparoscopy.
To accurately determine the presence of papillomas in the stomach, diagnostic studies are necessary - tests and instrumental examination.
The hollow organ, which is the stomach, is examined using an endoscope equipped with a video camera and a lighting device. Therefore, the doctor sees and studies the condition of the mucous membrane on the monitor, examining the presence, location, features of neoplasms, erosions, foci of inflammation, and smoothness of folds. Additionally, tissue fragments are taken for histology.
When examining stool, occult blood may be detected in it, which indicates the presence of bleeding. If necessary, the patient will be additionally prescribed radiography and ultrasound if the collected data is not enough. A complete blood count is also performed to detect anemia.
Causes and diagnosis
Erosion of the mucous membrane can be characterized as “corrosion” of the upper layer of the organ. This pathology can be caused by many factors:
- presence of chronic liver diseases;
- vascular pathologies;
- diabetes;
- burns of the mucous membrane by chemical vapors or liquids;
- intoxication of the body;
- surgical intervention in the organ;
- frequent eating of too spicy and/or hot foods;
- poor quality of chewing food;
- bad habits (smoking, drinking alcohol);
- entry of bile into the organ cavity;
- increased acidity of gastric juice with parallel resistance of the mucous membrane;
- long-term use of NSAIDs, antibiotics, heart medications;
- prolonged exposure to stress.
Doctors say that stomach papules do not degenerate into malignant formations, but can appear in parallel with these tumors, and also occur with inflammation in the intestines, liver failure, pneumonia and some cardiovascular diseases.
Diagnosis of gastric erosion is carried out using endoscopic examination. Gastrofagoduodenoscopy, taking a piece of tissue from the pathogenic area for further examination, as well as stool analysis for the presence of blood impurities - this option gives a complete picture of the patient’s condition and makes it possible to establish an accurate diagnosis.
Experts note that the presence of papules and ulcers on the walls of the organ and duodenum are the cause of bleeding in the gastrointestinal tract and occupy second place after gastric ulcers.
Stages of the malignant process
Stomach cancer can have the following stages of development:
- 1A: T1, N0, M0.
- 1B: T1, N1, M0; T2, N0, M0.
- 2: T1, N2, M0; T2, N1, M0; T3, N0, M0.
- 3A: T2, N2, M0; T3, N1, M0; T4, N0, M0.
- 3B: T3, N2, M0.
- 4: T4, N1-3, M0; T 1-3, N3, M0; any T, any N, M1.
T (tumor size):
- T1 – the tumor infiltrates the gastric wall to the submucosal layer;
- T2 – there is infiltration of cancer cells to the subserous layer. Possible involvement of the gastrointestinal, gastrohepatic ligament, greater or lesser omentum, but without penetration into the visceral layer;
- T3 – neoplasm that has spread to the serosa or visceral peritoneum;
- T4 – tumor growth into organs adjacent to the stomach.
N (metastases in regional lymph nodes):
- N0 – no metastases.
- N1 – metastases in 1-6 regional lymph nodes.
- N2 – regional nodes 7 to 15 are damaged.
- N3 – metastases in more than 15 lymph nodes.
M (distant metastases):
- M0 – no distant metastases.
- M1 – metastases in distant organs.
Features of the fibrogastroscopic picture: erosion and gastropathy
Consideration of erosive lesions of the antrum became possible only with the development of the fibrogastroscopic type of diagnosis. This pathology complicates gastritis and serves as the beginning of ulcers and tumor degeneration.
Erosion is a violation of the integrity of the mucous membrane without penetration into the deep parts of the stomach wall. The following varieties are distinguished:
- acute erosions - limited to compactions, cured in 10 days;
- chronic - look like spots with a diameter of up to 10 mm, require long-term treatment;
- hemorrhagic erosions - give a picture of the consequences of needle injections, the size of the lesion remains within 10 mm in diameter, the color takes on shades from scarlet to cherry-red (depending on the affected vessel, the vein gives dark spots), the mucous membrane surrounding the lesions is swollen, in it contains blood.
In the antrum, you can find a single erosion with all the described signs, as well as a complete type of erosion - characterized by spreading along the ridges of the folds of the stomach, the formation of a black coating. Antrum gastropathy is described by a doctor if there are no signs of inflammation, the entire mucous membrane is hyperemic, but the specific form of the disease is unclear.
Prevention of gastropathy
To prevent infection with the papilloma virus, including the appearance of gastric papillitis, it is necessary:
- Healthy food;
- avoid bad habits;
- strengthen immunity;
- use condoms;
- do not walk barefoot in public baths, swimming pools, or other places of high humidity;
- use personal hygiene products and utensils;
- lead a healthy lifestyle;
- Avoid shaking hands with unfamiliar, unhealthy-looking people.
But if infection has occurred, or there is a suspicion that it has occurred, you need to constantly take care of strengthening the immune system so that this virus does not begin its destructive effect, which often leads to malignant oncological diseases.
To prevent gastropathy it is recommended:
- take care of proper nutrition;
- get rid of bad habits - drinking alcohol and smoking;
- take medications strictly for medical reasons;
- avoid stressful situations.
Causes
A century ago it was believed that “chronic catarrh of the stomach is also observed in habitual drunkards, gluttons, and in general in people leading an immoderate lifestyle...” (A.P. Chekhov, “Everyday Adversity”). Today the list of reasons is much more extensive:
- poor nutrition - violation of the regime; fried, spicy, fatty, smoked, pickled food. Stale food, food that is too hot or too cold;
- alcohol, especially strong alcohol, dissolves the barrier mucus, allowing aggressive enzymes access to the defenseless surface of the stomach;
- smoking increases the secretory activity of the digestive glands;
- chronic gastritis with improper treatment or lack thereof;
- entry of bile from the duodenum through a loosely closed pylorus;
- long-term use of medications, including non-steroidal anti-inflammatory drugs (NSAIDs), which include Aspirin, Diclofenac, Ibuprofen, Ketorolac, Indomethacin;
- chronic congestion occurring against the background of pancreatitis, pathologies of the liver, kidneys, gastric ulcer;
- injuries, chemical and thermal burns of the gastrointestinal tract;
- poor blood circulation in the stomach;
- gastrointestinal infections (Helicobacter) and helminthiases (roundworms, pinworms);
- An increase in pressure in the portal vein leads to dilation of the arteries, veins, capillaries of the stomach, and their overflow with blood. Possible rupture of blood vessels with bleeding.
Conditions predisposing to the disease are retirement age, female gender, and rheumatoid arthritis.
Observation after surgery and relapses
After treatment, patients should be monitored by a local oncologist. In the first year, a person needs to be examined once every 3 months, then once every 6 months.
Scope of observation:
- general blood analysis;
- Ultrasound of the abdominal organs;
- X-rays of light;
- fibrogastroscopy;
- inspection and palpation.
Such measures are necessary to prevent relapses, which occur frequently, especially after non-radical operations. The patient may experience a second tumor next to the previously removed one, or metastases in other organs. In such cases, a new operation and/or chemo-radiation therapy is performed. With each new relapse, survival prognosis worsens and, ultimately, disease progression leads to death.
What is proximal erosive gastritis
Erosive disease of the duodenal bulb manifests itself in the destruction of the superficial epithelial layer of the organ without damage to deep tissues. Unlike peptic ulcers of the duodenum and stomach, treatment of erosions has a favorable prognosis, and surface defects heal quickly, without scarring.
Epithelial destruction is becoming increasingly common, and most duodenal pathologies are associated with the formation of defects and the appearance of erosive focal changes. In most cases, the pathology is characterized by a pronounced picture due to the presence of hemorrhagic syndrome. Thus, duodenal disease can be diagnosed on time and adequate treatment can begin.
Often there are erosions in the gastroduodenal region, that is, together with the duodenum, the mucous layer of the stomach is damaged.
The causes of erosion have now been well studied, and the main risk factor is damage to the stomach and duodenum by the bacterium Helicobacter Pylori, which colonizes these organs.
- Acute infectious gastroenteritis, with symptoms of intoxication of the body and disruption of the digestive system. Such a patient needs timely drug treatment, replenishment of fluid deficiency, and diet.
- Poor nutrition, addiction to spicy foods, hot foods, spices, and alcoholic beverages. Abuse of the listed products leads to disturbances in stomach acidity, dyspepsia, and general weakness; Treatment is quite simple and includes: dietary modification, drug therapy and regenerative medications.
- Chronic inflammatory damage to the wall of the stomach and duodenum, not associated with Helicobacter pylori infection. A long-term inflammatory process leads to the appearance of shallow defects in the mucosa - erosions.
- Long-term treatment with anti-inflammatory drugs, including reserpine, antibiotics, NSAIDs, steroid hormones.
The psycho-emotional factor also contributes to the appearance of erosion of the stomach and duodenum; the pathology is preceded by severe stress or chronic anxiety, depressive disorder. Treatment is effective only with the use of psychotherapeutic techniques in combination with drug therapy.
Symptoms of erosion appear depending on the severity of hemorrhagic syndrome, the number and size of defects, and the degree of the inflammatory process:
- painful sensations in the projection area of the stomach, duodenum (in the epigastric region);
- nausea, vomiting, sometimes streaked with blood;
- heartburn, belching with an unpleasant odor;
- against the background of hidden chronic bleeding of the stomach or duodenum, general malaise and pallor of the skin appear, less often acute anemic syndrome occurs, then immediate treatment begins and the symptoms are gradually eliminated;
- decrease in hemoglobin level in the blood;
- long-term erosion of the stomach or duodenum significantly worsens the quality of life and leads not only to physical illness, but also to psychological disorders.
Treatment begins with eliminating the causative factor. For this purpose, laboratory and instrumental diagnostics are carried out, the patient is examined by a surgeon, gastroenterologist and nutritionist (if necessary, by an infectious disease specialist or immunologist).
With erosion of the intestines and stomach, there is a deterioration in appetite, since eating is accompanied by pain. Chronic hemorrhagic symptoms and persistent inflammation lead to the appearance of deficiency anemias, which are characterized by damage to the gastrointestinal tract, skin, and nervous system.
Treatment of patients with erosion is based on a modern approach to the treatment of peptic ulcers, chronic gastroduodenitis and the elimination of the general symptomatic complex formed due to pathologies of the gastrointestinal tract.
Therapy includes targeted measures to prevent internal bleeding and accelerate the regeneration process of affected areas of the organ. For this purpose, antibiotics of the penicillin or macrolide series, antacids (omez, phosphalugel, ranitidn), prokinetics, and injectable vitamins (C, B6, 9 and 12, PP) are used.
The effectiveness of treatment is assessed according to the following criteria:
- Remission occurs, all symptoms subside, pain goes away, and the patient’s well-being improves significantly. During this period, supportive treatment is continued, a diet is prescribed, and activity restrictions are prescribed.
- The healing of superficial erosions begins, there are no hemorrhagic changes, swelling and redness disappear.
- Epithelization of chronic affected areas, endoscopic control is carried out.
Patients with bleeding and erosive gastritis are hospitalized in the surgical department. The stomach and duodenum are washed with cold water, which is both necessary for research and for treatment purposes. The next step will be the administration of hemostatic drugs, glucose-saline solutions and whole blood, if necessary.
Nutritional therapy is extremely necessary for patients with diseases of the duodenum. The diet involves eliminating irritating foods, hot dishes, and alcohol.
Proper nutrition is, first of all, eating healthy steamed and boiled foods rich in vitamins and microelements.
The diet is based on the following principles:
- during an exacerbation, a strict diet is prescribed, nutrition is selected by a specialist;
- be sure to adhere to the temperature regime so as not to irritate the sore stomach and duodenum;
- you need to eat in small portions five times a day;
- preference is given to liquid and soft foods, soups, cereals and purees;
- limit the consumption of fiber-rich foods;
- the last meal should be taken 3-4 hours before bedtime;
- all dishes are allowed boiled and steamed, fried foods, canned foods, salted and smoked foods are excluded;
- a therapeutic diet allows you to drink a little milk or kefir, but only with normal bowel movements.
Foods that can provoke increased secretion of gastric juice are prohibited:
- meat and mushrooms, everything salted, fish broths, seasonings, pickled foods, spices;
- rye and fresh bread, baked goods with yeast;
- sorrel, onions, radishes, cabbage, corn;
- products that increase gas formation and provoke pain: carbonated drinks, strong coffee and tea.
The right diet, medication and a positive psychological attitude will help get rid of erosions of the stomach and duodenum without consequences.
- 1Causes of the disease
- 2Symptomatic manifestations
- 3 Treatment methods
- 4People's Councils
The duodenum is one of the organs of the human digestive system, located immediately behind the stomach. It is more susceptible to the development of inflammatory processes than any other organ of the gastrointestinal tract, since it receives food from the stomach mixed with gastric juice and intestinal enzymes. The most common cause of the occurrence and development of inflammatory processes and the appearance of duodenitis in the human digestive organs is the presence of the pathogenic bacterium Helicobacter pylori, during the life of which a huge amount of pathological toxins are released that destroy the intestinal mucosa. The causes of the formation and development of erosive duodenitis can be:
- Poisoning with chemical acids, technical alcohol or other liquids (in this case, acute catarrhal duodenitis develops, which, in the absence of immediate treatment, can become chronic).
- Abuse or poisoning of low quality alcoholic beverages.
- Wrong diet - with a predominance of fatty, salty, smoked and stale foods.
- Frequent use of certain medications.
- Chronic diseases of the gastrointestinal tract, digestive organs.
- Stress and other nervous system disorders.
Duodenitis can sometimes develop against the background of chronic hepatitis, pancreatitis or gastritis. If a strict diet is not followed, the disease worsens, an inflammatory process begins, as a result of which duodenitis becomes chronic and affects not only the duodenum, but also the pancreas, gall bladder and liver. With each exacerbation, the form of the disease becomes more severe. But still, the main reason for the development of chronic erosive duodenitis is improper and irregular nutrition: abuse of fatty and spicy foods, spontaneous eating, eating “on the go” and dry food. All this in combination leads to an exacerbation of the disease and its transition to a chronic form.
Symptoms and treatment of pathology are inextricably linked, that is, the second depends on the severity of the former. It is very important to consult a doctor when you notice the first signs of the disease. The specialist will prescribe treatment that will help avoid the development of possible and quite serious complications and the transition of erosive duodenitis to a chronic form. Duodenitis is divided into several types depending on the duration and course of inflammatory processes: acute and chronic, which is more common. Proximal (with damage to the duodenal bulb) and distal (without changes in the duodenal bulb) types of duodenitis have similar symptoms, but differ in the location of the affected area.
The pathology is easy to diagnose, as the patient experiences increasing cramping pain, regardless of whether the person has eaten or eaten. With such pain, nausea is constantly felt, vomiting occurs, which does not bring relief. The vomit contains blood that oozes from wounds on the mucous membrane of the internal digestive organs. The patient's stool is disrupted, increased gas formation and rumbling in the stomach occurs, and a feeling of fullness occurs in the stomach, even if he has not eaten anything. Duodenofibroscopy, a special study, helps to correctly diagnose duodenitis.
What is it (duodenitis), you figured it out, but how to treat the pathology? Therapy consists of a set of measures aimed at eliminating the symptoms of the disease and helping to restore the structure of the affected mucous membrane. During treatment, the patient is prescribed bed rest, complete rest - not only physical, but also psychological. Smoking and drinking alcohol is strictly prohibited. In case of erosive duodenitis, it is strictly forbidden to rinse the stomach and warm the abdominal area with a heating pad. Such manipulations can lead to quite serious and dangerous internal bleeding and perforation of the intestinal walls.
For erosive duodenitis, treatment is carried out with the help of medications used for gastric and duodenal ulcers - taking De-Nol, Metronidazole and antibiotics containing tetracycline, and immunomodulating drugs and a strict diet will help get rid of the main symptoms of the disease, prevent the formation of a chronic form of the disease and stop intestinal and stomach bleeding. The patient is also prescribed sedatives and tranquilizers, which relieve the neurasthenic syndrome inherent in this disease.
Failure to comply with the recommendations and rules for the treatment of erosive duodenitis can lead to perforation of the intestinal wall and internal bleeding. In this case, conservative treatment is canceled, and the patient is prescribed surgical intervention.
Proper nutrition and diet, especially at the beginning of an exacerbation of the disease, help reduce the symptoms of the disease and alleviate the patient’s condition. During treatment, food should be consumed exclusively pureed and warm. Dishes made from vegetables and lean chicken should be well cooked, or better yet, cooked in a double boiler. Rice and vegetable broths, jelly and warm milk are useful. The consumption of sweets, sausages, sausages, tea and coffee is limited.
In addition to traditional treatment, it is recommended to use classical tips and recipes of traditional medicine, which are very helpful for exacerbations of duodenitis:
- A half-tablespoon of dry St. John's wort herb is brewed with half a liter of boiling water and drunk half a glass half an hour before meals.
- A small amount of plantain juice is mixed with the same amount of honey and taken three times a day before meals.
- Decoctions of nettle and oats are prepared separately; before use, the decoctions are mixed and taken half a glass before each meal.
If you follow all the rules and prescriptions of the recommended treatment, relief occurs within a few days. During exacerbation of duodenitis, it is advisable to fast for several days and not overexert yourself. Erosive duodenitis is a rather dangerous disease that requires constant monitoring both by the patient and by medical specialists, treatment and diet, since the disease can easily develop into more serious and dangerous ulcerative forms. It is necessary to closely monitor your health, pay increased attention to your diet and lifestyle, then the disease can be controlled and prevent the development of serious consequences.
Published: July 16, 2020 at 12:22 pm
Among the problems with the gastrointestinal tract, there are those that have similar symptoms. This sometimes complicates the diagnosis. Then you have to do a number of additional studies. Proximal gastritis (bulbitis) also belongs to this category of diseases.
Proximal gastritis refers to one of the forms of duodenitis, which is often associated with an inflammatory process in the gastric mucosa and has a similar symptomatic picture. The name speaks of its location. In this case, the part of the duodenum closest to the stomach, the proximal one, is affected. Therefore they are identified under this name. The disease occurs not only in adults, but also in children.
This disease has a number of causes: colonization of the duodenal bulb with bacteria Helicobacter pylori, the toxins of which provoke an inflammatory process, disruptions in intestinal motor function, affecting the length of time food remains in it, and causing stagnation, frequent stressful situations, abuse of medications and alcoholic beverages.
Less commonly, proximal gastritis occurs with helminthic infestations, Crohn's disease, giardiasis, unbalanced nutrition, or penetration of a foreign body into the digestive tract.
Typically, patients experience pain an hour after eating. They are localized in the area of development of the inflammatory process, but can be felt in the right or left hypochondrium, in the navel area. If the disease is accompanied by reflux, then the symptoms are accompanied by nausea, and soon vomiting containing an admixture of bile, which leaves a bitter aftertaste. With further aggravation of the condition, the following symptoms occur: a feeling of weakness in the body and increased fatigue, a noticeable decrease in immunity, headache, increased appetite.
Usually, to ascertain proximal gastritis, duodenoscopy and x-ray of this area are sufficient. To clarify the details, additional research methods are used. Any therapy is based on eliminating the causes of the disease. In this case, they are also guided by:
- If you are nervous, take sedatives.
- If poor nutrition occurs, then it should be reviewed and everything harmful should be eliminated.
- In case of helminthic infestation, appropriate medications are prescribed.
- Colonization of the digestive tract by Helicobacter pylori is treated with antibiotics.
- Next, it is necessary to establish intestinal motor function, reduce acidity, normalize the production of hydrochloric acid, and restore the duodenal mucosa.
The disease can be masked for a long time, but it cannot be neglected, and at the first manifestations you should consult a doctor.
source
Erosive gastritis is a single or multiple defects of the gastric mucosa. At the initial stage, the disease manifests itself as microscopic wounds that form only on the surface of the mucosa. In the international classification, it has the ICD code 10 (K00-K93).
Erosive gastritis can occur in chronic or acute form. The first option causes disruption of the digestive system, the second when consuming low-quality products or chemicals.
According to statistics, men are more susceptible to erosive gastritis than women; the manifestation of the disease in children is rarely observed.
Erosive gastritis can have not only external causes, but also internal ones.
- Prolonged, uncontrolled use of medications;
- Alcohol abuse;
- Prolonged stress;
- Insufficiency of the hormone insulin;
- Taking drugs;
- Disorders of the thyroid gland;
- Chronic diseases of all body systems;
- Binge eating;
- Starvation;
- Poor quality food;
- The influence of Helicobacter pylori bacteria and other pathogens;
- Reflux (stomach acid entering the esophagus);
- Living in an unfavorable area;
- Work in hazardous production;
- Failure of the hormonal system;
- Poor circulation of the gastric walls;
- Oncology.
Depending on the cause of erosive gastritis, it is divided into:
- Primary erosive gastritis. It is observed in most elderly people living in places with unfavorable ecology;
- Secondary erosive gastritis. Develops subsequently chronic diseases;
There are also several types of disease manifestations
- Acute ulcerative erosive gastritis. The cause of its occurrence is often mechanical damage to the walls of the stomach or chemical burns. Characterized by the blood content in vomit and feces;
- Chronic erosive gastritis. Occurs as a result of complications of chronic diseases. It is characterized by a change in exacerbations and weakening of symptoms. Erosion can reach up to 5 mm in diameter;
- Erosive antral gastritis. The most common type, caused by harmful microbes;
- Erosive reflux gastritis. A severe type of disease. Characterized by the formation of significant ulcers. When neglected, it is possible for mucosal tissue to detach and be released with vomit;
- Erosive-hemorrhagic gastritis. A complication of pathology causing heavy bleeding. In particularly severe manifestations it can lead to death.
The main clinical signs of erosive gastritis may appear several hours after the influence of external factors. They express themselves
- Heaviness and discomfort in the left hypochondrium;
- Fast fatiguability;
- Nausea;
- Violation of the vestibular apparatus;
- Vomit;
- Liquefaction of stool.
The patient's general condition worsens, increased sweating, dry mouth or excessive salivation are observed. The tongue becomes covered with a grayish coating, and the skin and mucous membranes become icteric.
Manifestations of acute erosive gastritis are characterized by severe pain in the stomach. Increased discomfort occurs after eating, or after a short time. Painful sensations are associated with damage to the deep layers of the mucous and muscle mass of the gastric walls.
The attack is often accompanied by vomiting containing blood, and because of this, the stool becomes almost black in color.
Symptoms of erosive gastritis of the stomach often go unnoticed. Patients complain of increased gas formation and an unpleasant taste in the mouth. Uncomfortable sensations in the esophagus, heaviness after eating and increased bowel movements.
Making a correct diagnosis depends on a thorough history taking. A significant loss of body weight in a short period of time, uncontrolled medication use and alcohol consumption speaks volumes.
The chronic form of erosive gastritis can be painless. Acute is characterized by cutting pain in the stomach and sternum.
Painful spasmodic attacks constrain the abdominal cavity. In some cases it can radiate to the back and under the left shoulder blade.
To diagnose erosive gastritis of the stomach, laboratory and instrumental studies are first performed. A blood sample is taken for a general analysis to confirm (refute) anemia. Feces for blood content.
Blood biochemistry reveals complications and concomitant diseases.
To identify the pathogen that provoked erosive gastritis of the stomach, a bacteriological analysis of the contents of the stomach, vomited and feces, is carried out.
- Of the instrumental methods, esophagogastrodudenoscopy with biopsy sampling is most often used. During the procedure, the degree of destruction of the mucosa, the depth and extent of erosions and the location of bleeding are assessed. In case of heavy blood loss, the manipulation should be carried out immediately, if the patient’s condition is stable, within 12-20 hours.
- If EGDS is not possible, the fluoroscopy method is used. The procedure can be carried out either through conventional gastrography or with the introduction of a dye into the organ. An x-ray can show swelling and an increase in the thickness of the folds of the gastric mucosa. Double contrasting of the gastric walls is more informative. With such a study, linear or extended defects of the shell can be seen and torn edges can be visualized.
- pH metering. Allows you to determine the content of hydrochloric acid in gastric juice.
Important! Examination of gastric juice is impossible after surgery and with stenosis.
When the first symptoms of the disease appear, you must contact a gastroenterologist at your local clinic to determine a diagnosis and prescribe adequate treatment.
Treatment of erosive gastritis must be carried out using a comprehensive method. The priority measures include the elimination of anemia and the elimination of blood flow disorders through blood transfusions.
Note! The treatment regimen for erosive gastritis is complex and only a specialist can make the correct prescription.
Symptoms and treatment of the disease depend on the form of its manifestation.
- Antibiotics. Used when Helicobacter pylori is detected. A combination of several antibacterial drugs is prescribed. Therapy lasts 7-10 days;
- Drugs that restore gastrointestinal motility. Prescribed when reflux is detected. Recently, drugs containing domperidone (Motilium) have been widely used for this purpose;
- Antacids are prescribed for diseases with significant mucosal defects and increased acidity of gastric juice. It is recommended to take non-absorbable antacids, which contain aluminum and magnesium salts (Maalox);
- Agents that regenerate tissues and improve their oxygen saturation (Iberogast).
- Enzymes are necessary when taking antacids, which significantly reduce digestive function (Mezim);
- Restorative drugs form a protective film on the surface of the gastric walls, prevent their further destruction and protect against irritation (Venter);
- Proton pump inhibitors are indicated for patients with high acidity; they inhibit the production of hydrochloric acid (Omeprazole, Omez).
Treatment with folk remedies has also proven itself well as an auxiliary therapy.
Important! You cannot replace medications with decoctions and herbal infusions without first consulting a doctor.
- Sea buckthorn fruit oil has wound healing and anti-inflammatory properties. For treatment, you can use a pharmacy product or prepare it yourself. To prepare it you will need equal amounts of sea buckthorn juice and high-quality olive oil. Combine the products thoroughly and let it brew for 3-4 days. The resulting mixture should be taken on an empty stomach, in the morning, 25 ml. Duration of therapy is 2 weeks.
- Propolis tincture will help reduce pain. Dilute 15 drops of alcohol tincture in 150 ml of cool water and drink before each meal. Course 3 weeks.
- Milk and chamomile. Place 5 tbsp in a glass of boiling milk. spoons of chamomile inflorescences, boil and leave for 1 hour. Drink 1 glass on an empty stomach. Course 5-7 days.
Important! Before starting treatment with folk remedies, you should make sure that there are no allergic reactions to the components of the recipes.
Treatment of erosive gastritis is impossible without dietary restrictions. In the first hours of an exacerbation, the patient is prescribed complete fasting. Fasting therapy can last from 6 to 24 hours, depending on the severity of the condition. A day later, dishes prepared in a double boiler or boiled are introduced into the menu. Meals for erosive gastritis of the stomach must be fractional (often in small portions).
Properly selected treatment and diet can alleviate the patient’s condition in a short time.
Erosive gastritis requires adherence to a certain diet; many ingredients are strictly prohibited.
- Baked goods, freshly baked bread;
- Rich meat and fish broths;
- Mushrooms;
- Spicy and pickled soups;
- Greasy meats and fish;
- Canned, pickled, spicy and salty foods;
- Pearl barley, barley, and corn grits;
- Fermented milk products with a high percentage of fat and acid;
- Cabbage, radish, tomato;
- Beans, peas;
- Liquids containing alcohol;
- Concentrated coffee and tea;
- Chocolate products.
The diet for erosive gastritis of the stomach should reduce the production of hydrochloric acid, therefore limiting the consumption of protein and fatty foods. Meat can be eaten 1 r. per day in small quantities.
Reference! After strict restrictions on food, you should switch to the usual menu gradually. After recovery, the attending physician advises the patient what can be eaten and in what quantities.
- Dried wheat bread;
- Grinded cereal soups with milk or vegetable broth;
- Milk;
- Protein omelet;
- Banana puree;
- Berry jelly with a neutral taste;
- Semolina, buckwheat and rice;
- Poultry or beef ground in a meat grinder;
- Potato, zucchini and cauliflower puree;
- Pasta.
Nutrition for erosive gastritis of the stomach should be balanced. The list of permitted products allows you to develop a fairly diverse menu for erosive gastritis. It is not recommended to eat scalding or icy food. The diet for erosive gastritis of the stomach excludes the consumption of “fast foods”.
- Morning. Well-cooked rice with milk and butter. Long loaf cracker, jelly;
- Snack. Sandwich made from a dried loaf with cheese, weak tea;
- Day. Grated vegetable soup with cauliflower and buckwheat, mashed potatoes with meat soufflé, compote, wheat croutons;
- Snack. Biscuits with milk, banana;
- Evening. Low-fat cottage cheese casserole, crackers with rosehip tea.
Desserts should be replaced with baked fruits with low sugar content.
Note! The diet prescribed for erosive gastritis is also good
prevention of disease. Experts recommend eating at night for erosive gastritis of the stomach no later than 2 hours before bedtime.
If erosive gastritis of the stomach is ignored and you do not consult a doctor in time, the consequences of the disease can become dangerous.
- Excessive internal bleeding;
- State of shock;
- Decreased red blood cells in the blood;
With long-term exposure to destructive factors on the gastric mucosa,
- Peptic ulcer disease. The cause is focal erosive gastritis. Inflammation affects not only the mucous membrane, but also the muscle tissue of the organ. This happens due to the influence of sulfuric acid and large pieces of swallowed food. An ulcer is dangerous due to the possibility of perforation (breakthrough) of the gastric wall and transformation into oncology.
- Oncology. Constant inflammatory processes of the mucous membrane with erosive gastritis can degenerate into a malignant tumor. If stomach cancer is detected, it is partially or completely removed, followed by chemotherapy.
Prevention of erosive gastritis should be carried out in two directions:
- Public activities include sanitary supervision of public catering establishments. Control is carried out over the quality of food, the cleanliness of kitchen linen and utensils. All kitchen workers must undergo regular hygiene inspections and an annual medical examination.
- An important role in the prevention of erosive gastritis of the stomach is played by health education work with people, which explains the importance of maintaining food hygiene.
- Individual prevention measures include dietary management. The menu should be complete and include all the necessary substances. Food preparation must comply with hygiene rules. Vegetables should be washed well under running water and avoid eating half-raw meat and fish. Compliance with food storage rules will protect them from infection by harmful bacteria.
All patients with erosive gastritis should undergo examination 2 times. in year.
Every patient with erosive gastritis of the stomach should have a doctor whom he trusts. It is with him that issues related to treatment, nutrition and disease prevention should be discussed.
source