Pancreatic stones are calcifications that form in the area of the ducts and parenchyma of the digestive system. The appearance of hardened formations leads to a deterioration in the intrasecretory and exocrine activity of the gland. Quite often their appearance is associated with pancreatitis and secondary diabetes mellitus.
To confirm the presence of stones in the pancreas, you will need to undergo a series of examinations, which will enable the doctor to prescribe effective treatment to relieve inflammation, swelling and restore organ function. Stones in the pancreas require immediate treatment!
Causes
The process of stone formation is always based on an imbalance of calcium metabolism in the body. Normal calcium metabolism depends on several factors:
- nature of nutrition;
- violation of calcium absorption;
- hormonal disorders.
Local infectious and inflammatory processes occurring in the immediate vicinity or at a distance from the pancreas can also initiate the onset of pancreolithiasis. Due to inflammation of the ducts, groups of cells exfoliate from the internal epithelium, which affects the functioning of the organ and disrupts the biochemical composition of the pancreatic secretion.
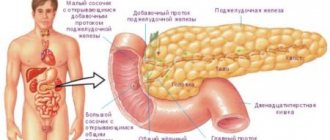
The following diseases also complicate the removal of pancreatic juice:
- dysfunction of the sphincter of Oddi;
- stones in the lumen of the bile duct;
- duodenitis;
- cholecystitis;
- pancreatitis;
- post-infectious swelling of the nipple of Vater.
Cystic and tumor processes often trigger the development of pancreolithiasis. In rare cases, the deposition of kidney stones occurs after syphilis or occurs from constant smoking or drinking alcohol. Substances contained in cigarettes and alcohol affect the composition of the secretory fluids of the pancreas and increase their calcium content.
Learn more about the effect of alcohol on the pancreas in this video.
An increased concentration of calcium leads to the fact that pancreatic juice becomes thicker than normal and provokes the formation of stones. This process occurs in three stages:
- At the first stage, the concentration of the juice increases, it becomes denser. After entering the ducts, it is transformed into an insoluble protein mass.
- At the next stage, the calcium flakes containing salts thicken. This continues to change the composition of the secretion towards the precipitation of sedimentary inclusions.
- Finally, an infection develops and obvious signs of pathology appear.
Stones can get stuck in the lumen of the duct, or they can form directly in the parenchyma of the gland. Immediately after formation, their structure is less dense, and over time they harden.
The risk of developing stones in the pancreas increases under the following conditions:
- high concentration of cholesterol or bilirubin in bile secretion;
- excess weight;
- inactive lifestyle;
- elderly age;
- diabetes;
- stones in the gallbladder;
- liver diseases.
This disease occurs more often in women, especially after 40 years.
Survey tactics
Diagnosis of pancreolithiasis is not difficult - modern examination methods make it possible to detect the smallest stones. Preference is given to instrumental methods. A general blood test is indicated to identify the general condition and the presence of inflammatory processes.
An examination for suspected stones in the pancreas includes:
- plain radiography of the abdominal cavity, on which stones are visualized as single or multiple oval or round shadows;
- ultrasonography to assess the condition of the gland, precise localization of stones;
- MRI and CT scan of the pancreas;
- retrograde cholangiopancreatography to assess duct patency.
Symptoms and signs
At the initial stages, a person may not be aware of the onset of the disease, since during this period the formation of calcifications does not affect well-being in any way and does not complicate the digestion process. After their increase, pressure on the organ begins to increase, which causes the appearance of the first uncomfortable sensations, reminiscent of the symptoms of pancreatitis.
Often the first manifestations occur after overeating, consuming fatty foods or drinking alcohol. In the abdomen, girdle spasmodic pains of a burning type are felt, reminiscent of colic. The pain can radiate to the right side, as well as to the shoulder, shoulder blade or collarbone. The attack is accompanied by nausea and vomiting mixed with bile, and sticky sweat may appear on the body. During and after attacks, the presence of undigested and undigested fat is noticeable in the stool, which looks like whitish inclusions.
The attack lasts from 15 minutes to several hours, the pain is very intense.
The first attacks can be significantly separated in time, sometimes months or years pass between them.
With the progression of blockage of the gland duct by calcifications, exacerbations occur more often. Symptoms differ somewhat depending on the location of the stones in the gland structure. Sometimes the disease does not manifest itself in any way until complications occur. In other cases, the following symptoms appear:
- an hour or two after eating, painful sensations arise in the abdominal cavity, radiating to the lower back or subscapular area;
- copious amounts of saliva;
- heartburn;
- vomiting with bile;
- the appearance of yellowness on the skin and sclera of the eyes;
- lightening of stool;
- fever.
Blood tests of such a patient may reveal leukocytosis, increased glucose, and an increase in the amount of enzymes in the liver and pancreas. Based on these indirect signs, the disease can be discovered by chance during periodic medical examinations.
As the disease worsens, necrosis of individual areas of the pancreas begins, enzyme production and secretion decrease. Often such changes are accompanied by a disruption in the production of hormones that control blood sugar levels, which can result in the development of diabetes mellitus.
If the stones begin to move and stop in the duct, closing the lumen, blockage and obstructive jaundice occurs with a high degree of yellowing of the skin.
If such stagnation continues for more than several hours, then bile has an aggressive effect on the parenchymal tissue of the gland. This can cause an inflammatory process, and in aggravated cases, provoke an abscess, bleeding or peritonitis.
In case of severe symptoms, you should not wait for a scheduled visit to the doctor; you need to call an ambulance, which will hospitalize the patient.
What are stones in the pancreas?
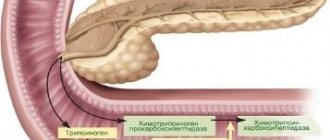
The composition of the formations includes chemical components: calcium salts - calcium orthophosphate and calcium carbonate, admixtures of aluminum and magnesium salts. They contain organic substances - cholesterol, protein elements, particles of epithelial membranes and leukocytes. The color of pancreatic calcifications is white or with a yellowish tint.
Stones in the pancreatic ducts vary in size and shape, and can be single or multiple. Large single stones are often located in the head of the pancreas, small multiple ones - in the tail and small ducts. The parenchyma of the pancreas also undergoes calcification.
Diseases of the pancreas are directly related to pathologies in the biliary system and gall bladder. The composition of gallstones and the mechanism of formation differ from pancreatic calcifications. Gallstones are formed as a result of dysfunction of the liver and gallbladder, excess cholesterol in the body and lack of bile acids.
The composition of gallstones and the structure of formations depend on the causes of their appearance, conditions of growth and development.
Diagnostics
Diagnosis of pancreolithiasis is complicated by the following factors:
- rare occurrence of the disease;
- similarity of symptoms with many more common diseases of the digestive tract - ulcers, cholelithiasis, etc.
A thorough examination is carried out by a gastroenterologist. After reviewing the patient’s complaints and examining the abdominal cavity, the specialist directs the patient to the main diagnostic method for this pathology - x-ray of the abdominal organs in several projections. With this type of examination, stones are easily detected as small darkened areas inside the gland.
In addition to radiography, the following research methods are prescribed:
- complete blood test to detect inflammation;
- endoscopic or classical ultrasonographic examination of the pancreas and its ducts;
- retrograde contrast cholangiopancreatography;
- magnetic resonance imaging and CT scanning to determine the number, position and size of calcifications.
All these procedures allow you to clarify the diagnosis and choose the type of therapy that is suitable for the existing clinical picture.
Treatment
Therapy for the presence of stones in the pancreas always involves an integrated approach. The main measures are aimed at:
- quick relief from pain and other symptoms;
- restoration of enzyme production;
- establishing metabolic processes;
- elimination of calcifications;
- preventing their re-formation.
Ways to combat calcifications in this organ are divided into conservative and surgical treatment.
Conservative treatment
This method brings tangible results with small stones and relatively rare attacks.
First of all, with conservative therapy, they try to eliminate the pathology that led to the onset of stone formation, stop the inflammatory process, establish the exchange of phosphates and calcium salts in the body, and also reduce the swelling of the gland parenchyma and ducts.
For this, the patient is prescribed the following medications:
- analgesics and antispasmodics to eliminate pain;
- antibiotics in the presence of infectious inflammation;
- choleretic drugs;
- secretory drugs.
When the patient's condition gets better, attempts begin to provoke the movement of calcifications and their release into the intestines. For this purpose, agents are used that can remove ductal hypertension.
If the stones are not dense, then they try to dissolve them in remission using tablets. Most often, Ursodiol or Henodiol is used for these purposes. These drugs are very effective against small and medium-sized loose cholesterol stones, but they are not suitable for stones with a different chemical composition.
Therapy is impossible without following a strict diet. For this pathology, gastroenterologists recommend adhering to the following rules:
- eat small portions to prevent pain;
- alcohol, sweets, fatty foods, smoked foods, coffee, soda are strictly prohibited;
- priority - vegetables, cereals, lean meat and fish, dairy products;
- Cooking methods include boiling and steaming.
Diet therapy can reduce symptoms and the load on the pancreas, which, together with the use of medications, will speed up recovery.
If there is no improvement, you should think about the advisability of a surgical method to solve the problem.
Surgical treatment
Surgical intervention is justified if the following list of factors is present:
- long-term course of pathology with frequent and severe attacks;
- positive dynamics of pancreatic insufficiency;
- inability to relieve pain using standard painkillers;
- serious condition of the patient.
There are several types of surgery. A specific type is selected individually in each individual case based on the size and location of the stones, the patient’s condition and the hospital’s instrumental base:
- The most modern and least invasive method is considered to be lithotripsy - crushing calcifications using shock wave energy. After crushing, the fragments or powder are removed from the glands on their own, and if this does not happen, they are removed forcibly. The advantage of the technique is that it is carried out on an outpatient basis. The procedure lasts just under an hour under general anesthesia.
- Endoscopic retrograde cholangiopancreatography is considered a minimally invasive method . During this operation, a flexible endoscopic tube equipped with a camera at the end is inserted into the digestive tract. With its help, it is possible to track deposits in the gland and remove them. This technique is characterized by a shortened recovery period and is much easier to tolerate by patients, but with multiple deposits and their large size, the endoscopic method is not effective.
- Laparotomy of the gland involves breaking the integrity of the organ to remove stones, so it is used in cases where other methods cannot be used. In this way, even the largest deposits can be eliminated.
- If examination indicates the presence of diffuse calcification in the parenchyma of the gland, total pancreatectomy . This is a serious step, so it requires strict indications. After total pancreatectomy, the patient must continuously use enzyme replacement therapy and insulin therapy.
In rare cases, it is possible to bypass and establish a bypass from the gland to supply pancreatic juice to the duodenum. But only a highly qualified surgeon can perform such an operation.