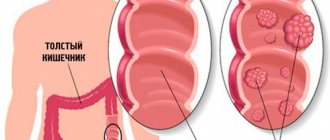
Obvious symptoms in most patients with colon diverticulosis (diverticular disease) are absent or identical to those of other intestinal diseases. But it has been found that the incidence of diverticulosis increases with increasing age. It is less than 10% among people under 40 years of age and about 50 - 60% over 80. On the European continent, diverticula are diagnosed in every 10th inhabitant before the age of 40, after 60 years - in every third, and from 75 years - every second resident .
Symptoms of intestinal diverticulosis are related to the location of the diverticula. Among the population of Western countries, most often, in 90% of reported cases, they are found in the distal parts of the colon, of which 50–60% are in the sigmoid colon and only 10% are in the right parts of the colon. The localization of diverticula in the rectum was not detected.
The main mechanisms of symptoms
The predominant frequency of sigmoid colon diverticula and corresponding symptoms are associated with anatomical and physiological characteristics. The sigmoid colon has a smaller diameter and more bends than the rest of the large intestine. It performs the function of a reservoir in which the formation, compaction and accumulation of feces occurs. By regulating their movement into the rectum, it is segmented much more often than other sections. All these reasons lead to increased pressure and stretching of the walls of the sigmoid colon.
The occurrence of diverticula is also facilitated by age-related changes in the connective tissue and muscle fibers of the transverse colon. As a result, muscle tension and resistance to the movement of feces, intraintestinal pressure and protrusion of the mucous membrane through defects in the muscular layer of the intestinal wall increase.
At the same time, pathological changes occur in the submucosal nerve plexuses with dysfunction of baroreceptors, thickening of the circular and longitudinal layers of the muscular lining of the intestine, a decrease in the extensibility and tone of its walls, and the convergence of the circular folds, as a result of which the intestine takes on the appearance of an accordion. This in turn leads mainly to:
- compression of blood vessels located in the intestinal wall;
- deterioration of blood microcirculation and the development of ischemia;
- atrophy of the muscle layer;
- impaired intestinal motility;
- the formation of weak areas on which diverticula form.
Possible consequences and complications
If diagnosis and treatment are not timely, patients may face the following serious complications:
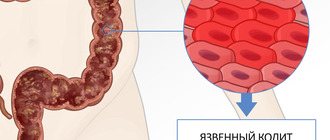
- Rectal bleeding. Pathological changes occur as a result of a serious violation of the integrity of blood vessels located close to the diverticula. Rectal bleeding can be detected after assessing the stool, which contains blood streaks.
- An acute form of diverticulitis accompanied by inflammatory processes of the sigmoid colon. Foci occur after the entry of pathogenic bacteria that linger in the intestines during constipation.
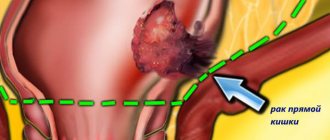
- The most dangerous complication of diverticulosis is rupture of the diverticulum. The contents of the intestine along with bacteria are released into the abdominal cavity.
If pain in the abdomen and abdominal cavity is accompanied by a sharp increase in temperature, then you should urgently consult a doctor.
Symptoms can signal danger and the presence of a serious pathology in the body. Taking good care of your health will prevent serious complications and promptly begin treatment.
Diverticulosis at the initial stage is successfully treated with antibacterial drugs.
Clinical manifestations of diverticulosis of the large intestine, sigmoid colon
All of these changes cause dysfunction of the intestine as a whole with the gradual development of symptoms of diverticulosis of the large intestine and its complications:
- Diverticulitis (inflammation of diverticulum)
- Bleeding
- Perforation (perforation)
- Formation of infiltrate
- Fistulas internal or external (rare)
- Acute or chronic intestinal obstruction
The disease is mainly progressive in nature with clinical manifestations, the severity of which depends on the duration of the disease, complications of diverticular disease, localization of diverticula, the presence of concomitant diseases, the age of the patient and his compliance with recommendations regarding proper nutrition.
The most common clinical form is uncomplicated diverticulosis of the large intestine. It occurs in almost 80% of patients with this disease. For many years it was believed that such forms of the disease proceed completely in the absence of symptoms. But studies in recent years have shown that in 85% of patients, even single diverticula of the colon, not to mention diverticulosis, are accompanied by clinical manifestations of varying severity.
However, the symptoms are nonspecific. Often, patients either do not seek medical help at all, or, if they do see a doctor, they are given diagnoses such as dysbiosis, chronic colitis, colon dyskinesia, etc.
The most common and main symptoms of uncomplicated diverticulosis of the large intestine:
- Intermittent, recurring pain of a spastic, paroxysmal or dull aching nature in the left (most often), middle (below the navel) or lower abdomen. It is assumed that these pains arise as a result of increased pressure in the intestinal lumen and impaired motility.
- The pain may go away on its own after a few hours, but may intensify, especially after eating.
- Pain similar to an attack of appendicitis may occur (in the right lower abdomen), even if the diverticula are not localized in the ascending sections (right), but in the sigmoid colon (left).
- Sometimes there is irradiation (spread) of pain: in the anus, lower back, sacrum, as well as in the groin or buttock area.
- Relief or complete disappearance of pain after passing gas or defecation.
In addition to the main manifestations of diverticulosis of the large intestine, there may be general symptoms characteristic of a violation of its function:
- constipation that is persistent;
- constipation followed by diarrhea;
- secretion of copious amounts of mucus;
- bloating and significant discharge of foul-smelling gases;
- false urges (tenesmus) or repeated acts of defecation;
- a feeling of incomplete emptying after defecation (often accompanies the presence of diverticula in the sigmoid colon).
Upon examination, the doctor notes bloating and pain on palpation (palpation) along the entire large intestine. These phenomena are most pronounced in the left sections, however, there is no protective reaction (tension) of the abdominal wall. The spasmodic part of the colon, in which diverticula are localized, is also palpated.
Some distinctive signs of diverticulosis in various parts of the transverse colon:
| Intestinal section | Changes in the muscular layer of the intestine and the nature of the chyme | Most common age of presentation | The nature of the most common complications |
| right | intestinal fragmentation and thickening of stool | young (up to 40 years old) age | Tendency to bleed |
| left | atrophy of muscle fibers, reservation and formation of dense feces | more often older people | Tendency to diverticulitis (inflammation) |
When complications arise in the form of diverticulitis, bleeding, perforation, and so on, the corresponding symptoms arise:
- with changes in clinical blood and urine tests
- the appearance of temperature
- blood in stool
- changing the nature of the pain syndrome, etc.
Diagnostics using basic instrumental methods, such as irrigography (x-ray examination after filling the intestine with a contrast agent), endoscopy, colonoscopy, computed tomography, allows you to more accurately determine the presence, location and condition of diverticula.
Features of the development of diverticulosis
Intestinal diverticulosis is an inflammatory pathological process characterized by the formation of special protrusions (diverticulum) on the sides of the intestine. The disease can be congenital or acquired, and is diagnosed mainly in old people living in highly developed countries. Women are more susceptible to the disease. Diverticula can appear in any colon other than the rectum. In most cases they are found in the distal colon. Sometimes they can form in the esophagus and stomach. The size of hernial protrusions can vary from microscopic to larger. Due to absent or mild symptoms, diverticular disease with complications is often observed.
Due to poor nutrition and lack of physical activity, intestinal peristalsis is disrupted, causing disruption of the functioning of the gastrointestinal tract. And as a result of constant problems with stool, intraintestinal pressure increases, provoking the formation of painful formations in the intestines. According to this principle, the formation of diverticula occurs, which can be congenital or acquired. Congenital protrusions occur due to abnormal development of the fetus in the mother's womb.
The causes of acquired diverticulum may be the following:
- Straining during bowel movements (constipation).
- Lack of physical activity.
- Excess weight.
- Impaired blood circulation in the intestines.
- Infectious lesion.
- Atherosclerosis of intestinal vessels.
- Excessive gas formation, flatulence.
- Uncontrolled use of laxatives.
- Weak intestinal muscles.
- Genetic predisposition.
A major role in the appearance of diverticula is played by poor nutrition, or rather insufficient consumption of plant fiber contained in vegetables and fruits. Residents of highly developed countries: the USA and Canada are most susceptible to diverticular disease. The reason for this is the abuse of fatty meat, flour products and various fast foods. Residents of rural areas, Asia, Africa, as well as vegetarians, are much less likely to suffer from this disease due to the peculiarities of their diet, rich in fiber. Also, the risk of diverticulosis increases with age as a result of the natural weakening of connective tissues.
Treatment of uncomplicated diverticulosis
The main thing in the treatment of intestinal diverticulosis (uncomplicated form) is eating foods rich in dietary fiber. According to the latest data, their use by patients with asymptomatic disease helps prevent its progression and complications. There is a conflicting opinion among some researchers that the inclusion of these products in the diet even leads to regression of diverticula.
Dietary, or dietary fiber, is plant fibrous substances of various composition and structure that are not digested or absorbed in the intestines. With a calorie diet of 2500 kcal, the daily physiological need for them is 30 g. Most types of plant fiber contain indigestible polysaccharides, pectin, cellulose and hemicellulose, lignin, alginates. Their main property is the binding of water in the intestinal lumen, which increases the volume of chyme, reduces pressure inside the intestine and promotes faster transport through the intestines and the removal of feces and toxins from the body.
In addition, insoluble dietary fiber, which covers about 6–9% of the body's energy needs, creates a large additional surface area in the colon on which a large number of beneficial intestinal bacteria are located and fixed. Fibers provide a breeding ground for “friendly” bacteria, on which they quickly grow and multiply, which leads to the suppression of pathogenic flora.
Table describing the positive effect of dietary fiber on the human body:
| Direct effect | Indirect action |
|
|
It becomes clear why dietary products containing bran are an effective diet for intestinal diverticulosis. Coarse wheat bran has the greatest ability to reduce intestinal pressure and increase the volume of chyme. They must be introduced into the diet gradually over a period of 2 weeks to 1 month. The daily norm starts from 5 - 10 g to 20 - 30 g. For this purpose, the daily dose (2 - 4 tablespoons) of bran is poured with 1 glass of boiling water and kept for 30 - 40 minutes, after which the water must be drained. Brewed bran can be added to vegetable dishes, fermented milk products, cereals, and soups.
During the first month of such a diet for intestinal diverticulosis, containing a large amount of plant dietary fiber, abdominal pain may appear or intensify. Therefore, it is recommended to take antispasmodic drugs, for example, no-shpa or mebeverine 20 - 30 minutes before meals in the morning and evening, 400 mg, meteospasmil, bucopan and others.
Mucofalk, Fiberlex, Ispagol, Solgar Psyllium preparations, consisting of the seed shells of plantain oval, which grows in the arid regions of the Mediterranean, Pakistan and India, are considered an effective source of dietary fiber. The shell of plantain seeds of this particular species contains high concentrations of mucous components, making the drug a soft dietary fiber.
Mucofalk, unlike bran, has almost no side effects in the form of flatulence and spastic pain, but it has an anti-inflammatory effect and is significantly superior to wheat bran in reducing intraintestinal pressure, and effectively promotes the proliferation of lacto- and bifidobacteria.
The dietary fiber that makes up Mucofalk has the following physicochemical characteristics:
- Slow down the process of evacuation of food mass from the stomach
- Increases the viscosity of food masses in the small intestine
- Increase the formation of mucus on the cells of the mucous membrane of the large intestine
- They bind and retain a volume of water exceeding the mass of the fibers themselves, thereby reducing the tension of the intestinal walls, moisturizing feces and ensuring their accelerated passage through the intestines.
- Collect and retain toxic elements of external and internal origin on their surface in a colloidal state
- They provide additional area for useful microbial associations and, undergoing enzymatic decomposition by microorganisms, become an energy resource for the latter
- Do not impede the absorption of microelements and vitamins in the intestines
It is recommended to include in the diet of patients with intestinal diverticulosis:
- bread made from bran or wholemeal white flour
- crumbly porridge from wheat and buckwheat with vegetable oil
- vegetable casseroles
- vegetable soups with meat broth
- dairy products
- baked vegetables (if tolerated)
It is advisable to exclude foods that are astringent and inhibit peristalsis from the diet. These include:
- bread made from finely ground premium flour
- pasta
- semolina and rice porridge
- jelly, coffee and strong brewed tea
- red wine, cocoa and chocolate
Dietary fiber is the main means of treating and preventing diverticulosis of the large intestine. In the absence of complicated forms of the disease, their constant use is recommended, with the exception of the summer and autumn seasons, due to the inclusion of a sufficient amount of fresh vegetables, fruits and herbs in the diet.
Recommended therapeutic diet
During the progression of diverticulosis without serious complications, doctors advise their patients to adhere to diet No. 4. It is necessary to include foods with a high amount of dietary fiber in your diet.
The main task of such dietary nutrition is to normalize intestinal motility, soften stool and increase the number of beneficial bacteria.
Below is a list of main products:
- Bran bread;
- Cereals seasoned with vegetable oil;
- Vegetable soup;
- Dried fruits that help stimulate active intestinal function.
During the diet, it is important to avoid eating nuts, seeds, popcorn, crackers, beans, raw cabbage, semolina, pasta of any kind, semi-finished products and white bread.
Drug treatment
For intestinal diverticulosis, treatment tactics are determined by the general health of the patient, the severity of the disease, and the presence of complications.
For asymptomatic diverticulosis
when the disease was diagnosed by chance (accidental finding), the patient is recommended to follow a diet only, with an increase in the daily diet of fruits, vegetables, beans, grains, and consumption of at least 2 liters of fluid per day (if there are no contraindications). According to indications, it is possible to use probiotics (see the list of drugs analogues of Linex), enzyme preparations, drugs that reduce flatulence (reasons).
In the presence of an uncomplicated inflammatory process
With the development of the inflammatory process and symptoms of intestinal diverticulosis, but without serious complications, outpatient treatment is possible. In addition to the diet described above with the maximum amount of fiber and drinking regimen, the following are prescribed:
- broad-spectrum antibiotics, preparations of 5-aminosalicylic acid, butyric acid
- enzymes to improve digestion
- stimulants of gastrointestinal motility, such as Domperidone (Motilium, Pasajix, Motilak), Metoclopromide, etc.
- antispasmodics - Noshpa, Drotaverine, Spasmol, Spasmonet
- laxatives - prebiotics (based on Lactulose - Normaze, Romphalac, Portalac syrup, Duphalac, Lactulose Poly, Goodluck, Lactulose Stada, Livolyuk-PB).
If the disease progresses during treatment, hospitalization is indicated
If there is no improvement within 3 days of therapy, then the patient is indicated for hospitalization, with correction of treatment and determination of further treatment tactics. Additional diagnostics are performed, infusion therapy is prescribed - glucose solution, saline solutions, and the issue of surgical treatment is decided.
Drug therapy, folk remedies
More often, diverticulosis of the large intestine occurs without obvious clinical signs and symptoms. This condition leads to serious conditions; it is important to pay attention to any changes in the body.
Diverticulosis does not go away on its own, so treatment should begin immediately after detection of pathological formations in the body.
If diverticulosis is accompanied by inflammatory processes, then patients are prescribed antibiotic drugs. The duration of such therapy, the method of drug administration and dosage are prescribed for a specific patient.
During treatment, you should stop taking stimulant medications, because they will cause increased pressure in the intestines.
At the initial stage of development of intestinal diverticulosis, patients can use traditional medicine.
Before using and consuming herbs and other recipes, you should consult your doctor.
Some medications are not compatible with traditional medicine, so uncontrolled treatment leads to complications and health problems.
The most effective treatment is eating bran. They help remove excess gases in the intestines, relieve spasms and pain. The dietary fiber they contain helps normalize stool.
When is surgery indicated?
If the patient has had 2 attacks of diverticulosis, according to the latest clinical studies, elective surgery is advisable. Since repeated attacks are poorly amenable to drug treatment and, as a rule, end in intestinal perforation followed by peritonitis. Moreover, in patients over 40 years of age, even after 1 episode of diverticulitis, surgical treatment is recommended.
Surgical treatment consists of removing (resection) the part of the intestine that is affected by diverticula. Indications for surgery are the following complications:
- heavy bleeding
- progressive intestinal obstruction
- perforation of the diverticulum with the development of peritonitis or retroperitoneal phlegmon
- opening of an abscess when external or internal intestinal fistulas develop
In each specific clinical case, the scope of the operation is determined individually; sometimes, during emergency surgery, the intestine is removed in an unnatural way onto the abdominal wall. Timely referral of the patient to a gastroenterologist and coloproctologist, adequate therapy and planned surgical treatment (especially after an attack) improve the prognosis. In 80% of cases, diverticulosis occurs without complications; in case of complications, the risk of relapse in the future is 25%.
Author:
Selezneva Valentina Anatolyevna physician-therapist
Diagnosis of diverticulosis, ICD code
If unpleasant intestinal symptoms appear, you should seek help from a gastroenterologist. Next, you may need to consult other specialists - proctologist, gynecologist, urologist, surgeon.
At the first appointment, the doctor interviews and examines the patient. This will help to find out the nature of the pain, the regime and diet that accompany the pathology of the digestive tract.
Instrumental methods include colonoscopy, irrigoscopy, laparoscopy and ultrasound examination of the abdominal organs.
Using them, you can find out the area and intensity of bleeding, the presence of adhesions and fistulas, perforations, accumulation of fluid in the peritoneal cavity, the density and size of the diverticulum, and intestinal obstruction.
A significant laboratory method is a blood test, which determines the presence of inflammation.
The ICD 10 code for colonic diverticulosis is K57.
Means for regulating stool for diverticulosis
Patients with diverticulosis of pre-retirement and retirement age are prescribed treatment with herbal preparations, combining them with diet therapy and drinking plenty of fluids. Middle-aged people undergo a course of systemic treatment to restore intestinal function.
For diarrhea, patients are given Rifaximin. The antibiotic slows down and stops the growth of pathogenic bacteria in diverticulosis, but it also causes:
- pain in muscles, stomach;
- dizziness and nausea;
- malaise and fatigue.
To treat long-term constipation, laxatives with an oil or plant base are used.
What diet should you follow if you have intestinal diverticulosis?
Slag-free diet therapy is mandatory for disorders of the gastrointestinal tract. During periods of exacerbation of the disease, restriction of fiber intake is required.
Folk remedies
The use of medicinal plants for diseases, the preparation of infusions and decoctions from them, and homeopathy are welcomed by orthodox medicine.
- Dried and crushed red elm bark is poured with 200 ml of boiling water and left for 60 minutes. Treat with infusion 3 times a day. The product promotes intestinal healing and relieves irritation from its walls.
- Taking 1/2 tsp. Aloe pulp before meals 3 times a day can normalize digestion and get rid of constipation. Aloe stimulates the growth of beneficial bacteria inside the gastrointestinal tract.
- An infusion of licorice root acts as a laxative. It is enough to pour 2 tbsp. crushed plant 0.5 liters of boiling water and simmer in a thermos for 2 hours. Take half a glass 2 times after meals. Continue treatment for 2-3 weeks.
- Folk remedies include the drug "Todikamp", which is an infusion of walnut extracts taken at a certain degree of maturity, and kerosene.
Treatment of disease with herbs at home
Occurrence of the disease
Today, all the mechanisms of diverticulosis are well studied. The impetus for the appearance of protrusion is given by two factors:
- Dystrophy of the muscular layer.
- High pressure in the lumen.
The first diagnosis is most often made in older people or children with congenital anomalies. There are indirect symptoms of diverticulosis that indicate the presence of this particular problem. These are chronic hemorrhoids, prolapse or prolapse of organs located in the pelvis, and the presence of hernias. When excess pressure forms inside the tract, long-term constipation occurs.
Doctors, studying the processes of development of diverticulitis, have identified four main causes of the disease:
- Protrusions appear due to a decrease in a person’s motor activity, due to age-related changes in the tone of the intestinal muscular frame.
- The appearance of diverticula is caused by disturbances in the blood circulation of the tract walls.
- Hereditary predisposition plays a major role.
- Hollow sacs are formed due to the formation of high pressure inside the walls of the organ.
The International Classification of Diseases has revised its positions and included the described pathology in a separate group with code 57. This section includes anomaly of the small intestine (57.0) and diverticulosis of the large intestine (ICD 57.2) with and without complications. Inflammation and bleeding of the appendix and congenital pathologies are not included in this list.
The duodenum is least often involved in the described process, but if a protrusion appears there, the consequences can be very serious. The first alarming symptom occurs when an acute inflammatory process develops in the suspended sac. Its presence is indicated by tension in the peritoneal wall, severe pain in the upper abdomen, and nausea that does not lead to vomiting. The danger lies in the possibility of perforation of the protrusion and the development of peritonitis.
Diagnostics
Asymptomatic diverticular disease is diagnosed accidentally, when examining the intestines for other pathologies.
Diagnosis of clinically significant intestinal diverticulosis is carried out using:
- collecting anamnesis, including family and life history;
- inspection and palpation;
- clinical blood test;
- biological blood test;
- stool examination for the presence of occult blood;
- coprograms.
The intestines are also examined for diverticulosis using irrigoscopy, sigmoidoscopy, and colonoscopy.
In order to assess the condition of other internal organs and exclude complications of the disease, computed tomography and ultrasound are performed.
Another article on this topic: What are the causes of constant burping of air?