General rules
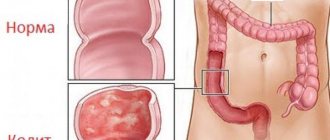
Colitis is an inflammation of the colon mucosa. enterocolitis ) and stomach ( gastroenterocolitis are additionally involved in the inflammatory process .
According to the course of the disease there are:
- spicy;
- chronic.
If acute develops as a result of eating food contaminated with microorganisms, then with pseudomembranous, which also occurs acutely, the cause is the use of medications (in particular, antibiotics cephalosporins , Clindamycin , Tetracycline and Erythromycin ).
At the initial stage of acute colitis, general malaise, nausea, loss of appetite, abdominal pain and diarrhea . The pain is most often localized in the iliac regions. The stools are frequent, offensive, and at first fecal in nature, and then become scanty with mucus and blood. In the first days of the disease, you need to follow bed rest and diet in addition to drug treatment. Acute colitis does not cause gross morphological changes in the intestinal mucosa.
Chronic colitis is accompanied by inflammatory-dystrophic changes in the intestine and there is always a violation of its functions.
The causes of the chronic form of the disease are:
- previous intestinal infections;
- uncontrolled use of medications;
- constant endogenous intoxication;
- alcohol abuse;
- nutritional disorders (consumption of spicy and coarse, poorly digestible foods, monotonous, protein or carbohydrate nutrition).
The main symptoms of chronic colitis are alternating constipation with diarrhea or pasty stools, accompanied by pain that intensifies with defecation. The pain is aching or spastic in nature and is localized in the lower and lateral parts of the abdomen. Occurs most often 7 hours after eating; they typically decrease after the passage of gas. Many patients are bothered by nausea, bloating and belching .
If digestion is impaired, starch grains, neutral fat, and undigested muscle fibers are found in the feces. With a long course, chronic colitis is characterized by the progression of intestinal digestive disorders, which is accompanied by weight loss, the development of atrophy of fatty tissue and skeletal muscles, and an increase in protein and vitamin .
Treatment of the disease should be comprehensive, including anti-inflammatory drugs ( Sulfasalazine , Mesalazine ), enveloping and astringent drugs (for diarrhea ), physiotherapeutic treatment ( electrophoresis , diathermy , ozokerite , radon baths ). A prerequisite is therapeutic nutrition.
For symptoms of colitis at different stages and for intestinal dysfunction, treatment with diet is prescribed differentially.
So, for acute colitis and for exacerbation of chronic colitis, occurring with diarrhea, Diet No. 4 . It involves the exclusion of foods that cause increased intestinal motility (vegetables, bran, fiber) and stimulate the secretion of the pancreas, stomach and bile secretion. All products that cause fermentation and rotting are also excluded.
If constipation , Table No. 3 , enriched with fiber (bran bread, vegetables, vinaigrettes, vegetable juices).
Diet No. 2 is indicated for chronic colitis (without exacerbation) and concomitant chronic gastritis with reduced secretion, therefore it includes dishes and products that stimulate secretion (fermented milk drinks, broths, juices, berries, vegetables and fried dishes without a rough crust).
Diet No. 4 for colitis with diarrhea provides intestinal sparing, reduces inflammation and normalizes digestion, because it limits all kinds of irritants (mechanical, chemical and thermal).
Basic Rules:
- six meals a day, the basis of which is pureed, slimy soups, pureed, mushy, semi-liquid dishes;
- reducing the amount of fat (up to 70 g) and carbohydrates (250 g);
- physiological protein content (90 g);
- exclusion of foods containing fiber (vegetables, fruits, rye bread, whole grain bread and bran);
- exclusion of very hot and cold foods;
- boiled (steam) method of preparation;
- prohibition on hard and thick foods;
- implementation of the water regime (1.5-2 l);
- salt in the amount of 8-10 g.
Diet for ulcerative colitis
Nonspecific ulcerative colitis is an inflammation of the large intestine with the presence of ulcerative lesions of the mucous membrane, necrosis and hemorrhage. Most often, the process is localized in the rectum and colon, and with severe damage, all parts of the colon are involved. The causes of the disease have not been established. It is assumed that the basis is immunological disorders and hereditary predisposition, and the predisposing factor is the presence of infection.
With nonspecific ulcerative colitis, the patient is bothered by diarrhea mixed with blood or pus. The frequency of bowel movements reaches 20 times a day or more (in severe cases). Often there is blood in the stool and blood loss of 100-300 ml is possible per day. UC is characterized by severe cramping pain that intensifies after eating.
In severe cases, intoxication syndrome is observed with weakness, fever, decreased appetite, and systemic manifestations are also characteristic ( polyarthritis , eye and liver damage). , dystrophic syndrome develops (dry skin, weight loss, hypovitaminosis ).
With this disease, complete restoration of the mucous membrane and normalization of digestion and absorption do not occur for a long time. And only strict adherence to dietary nutrition and medications create the conditions for achieving remission. In this case, Table No. 4 and its varieties are assigned depending on the stage of the process.
Rice porridge with fruits
During an exacerbation, the diet includes liquid and pureed porridge (rice, semolina) in water (milk and broths are excluded). Buckwheat porridge enhances motor skills, so it is not recommended during an exacerbation. It is convenient to use porridge for baby food, but it needs to be diluted by half with water.
Includes dishes from lean meat and fish (in the form of boiled minced meat, dumplings, steamed cutlets, pates). Protein omelettes made from eggs are useful (no more than two per day). During an exacerbation, the amount of protein in the diet should be increased to 120-125 g.
Drinks include herbal decoctions, compotes and jelly, chokeberry juice. Baked apples and pears are allowed. Particular attention should be paid to products that reduce intestinal motility - decoctions and jelly from bird cherry, blueberry, quince, dogwood, pear, strong black and green tea. During an exacerbation, some patients do not tolerate even boiled vegetables well, so it is better to exclude them. Consumption of milk, fermented milk products, sour cream, cheeses and cottage cheese is also not recommended.
For a month after an exacerbation, it is necessary to strictly adhere to the diet; subsequently, it is recommended to switch to Table 4B and 4B and the general table with the restriction of certain foods for health reasons. After an exacerbation, foods that promote hematopoiesis are introduced into the diet, red and black caviar, walnuts, and meat broths are gradually added. During the period of stable remission, the consumption of vegetables (broccoli, cauliflower, carrots, zucchini, onions) is allowed.
Consequences of ulcerative colitis
Boiled eggs and bread
As is the case with any other chronic diseases, a person with ulcerative colitis (UC) can essentially be in two states - remission and exacerbation.
In today's post, I will give you an example of a weekly menu that you can follow during an exacerbation of UC. The diet is based on what I was fed at the regional clinical hospital during my severe exacerbation.
Monday
Breakfast
- Overcooked rice.
- Sandwich made from day-old white bread with butter.
- Tea with sugar.
Lunch
- Steamed veal cutlet.
- Soup based on chicken broth made from vermicelli, carrots, and onions.
- Buckwheat porridge with ground chicken meat.
- Dried fruit jelly.
- Cottage cheese casserole with sour cream.
- Three-day kefir.
Tuesday
In case of exacerbation of colitis, gentle nutrition without milk, vegetables and fruits is indicated. As you improve, the diet is slightly expanded. The menu includes boiled and chopped dishes.
Nonspecific ulcerative colitis is a disease that occurs with intestinal inflammation and the formation of ulcerative defects in the colon and rectum. Accompanied by severe pain and diarrhea.
In case of severe exacerbation, patients are allowed to drink only tea and eat mashed apples for one or two days.
The same style of eating (table 4) is also used for exacerbation of non-ulcerative colitis with diarrhea, loss of appetite, and severe weakness. At the same time, the amount of nutrients remains unchanged: proteins 100 g, fats 100 g, carbohydrates 400 g. After 4-5 days, the diet is expanded - a diet of 4 b is prescribed for a month.
If an exacerbation of colitis is accompanied by constipation, then 4b is immediately prescribed with maximum mechanical sparing (mashed dishes) and limitation of irritants. Gradually, the patient is transferred to the unpureed version, and fruits and vegetables are added to the diet.
All products are boiled in water or steamed. Meals are recommended 5-6 times a day in small portions.
When preparing a diet, use:
- soup with water, a weak broth of meat with semolina, boiled rice or oatmeal, buckwheat flour, meatballs;
- rice porridge, buckwheat, oatmeal and semolina (mashed);
- cutlets and steamed meatballs from chicken, turkey, beef, pike perch, pike;
- calcined cottage cheese (from milk);
- steamed or soft-boiled eggs for omelet;
- jelly, jelly, juices half diluted with water, tea from blueberries (dry), black currants or rose hips;
- sugar 20 g, honey 2 tablespoons;
- butter 10 g;
- dried white bread, homemade crackers.
The following should be completely excluded from the diet of patients in the acute stage:
- all dairy products, whole milk (only calcined cottage cheese is allowed), first or second courses with milk;
- any fats except a small amount of butter;
- fresh and boiled vegetables, fruits, berries in their natural form;
- compote, jam;
- all canned food, marinades, pickles;
- strong brews, vegetable or cereal soup;
- fatty meat and fish products;
- snacks;
- all ready-made sauces, herbs, spices;
- millet, barley, barley, legumes, pasta;
- bread products, pastries;
- sweets;
- hot, cold dishes, drinks, carbonated drinks;
- coffee and cocoa with milk.
Alcohol is strictly prohibited until a period of stable remission, or better yet, its complete exclusion.
For nonspecific ulcerative colitis in the acute stage, as well as for inflammation of the intestines with diarrhea, you can use the following indicative menu:
- steam omelette, rosehip tea;
- blackcurrant jelly, calcined cottage cheese;
- chicken broth soup with semolina, steamed chicken meatballs with rice porridge;
- oatmeal jelly;
- pureed buckwheat porridge with steamed pike cutlets.
To prepare you need:
- eggs – 4 quail (2 chicken);
- water – 80 ml;
- butter – 5 g;
- salt – 1 g.
Beat eggs with cold water and salt. Place the mixture in a mold so that the layer of the mixture is no higher than 4 cm for good boiling. Cook in a water bath for 10 minutes.
To make jelly you will need:
- black currant – 2 tablespoons;
- water – 150 g;
- gelatin – 5 g;
- sugar - a teaspoon.
Grind the currants with sugar, add water, bring to a boil and strain. For 5 g of gelatin you need 50 g of water. It is left to swell for 60 minutes. The strained currant tea is placed on low heat, heated until a bubble appears, and the prepared gelatin is poured in. Immediately pour into molds and cool for an hour at room temperature, then in the refrigerator.
For 500 ml of milk you will need 10 ml of calcium chloride. The milk is brought to a boil, the solution from the ampoule is added, mixed and placed on gauze in two layers. After the whey has drained, the curd is ready.
For the dietary first course you need to take:
- chicken fillet – 100 g;
- water – 500 ml;
- semolina – 20 g;
- egg - one quail;
- carrots - half;
- parsley - a small sprig;
- salt 1 g.
First, fill the fillet (entirely) with water so that it covers it by 1 cm. Bring the liquid to a boil and drain. Refill with water (500 ml) and add carrots. Cook for 30 minutes. Then take out the meat and carrots, pour semolina into the boiling broth in a thin stream and cook for another 10 minutes, stirring. When serving, add a boiled egg and parsley to the plate.
A special feature of prescribing this therapeutic nutrition when an exacerbation of ulcerative colitis subsides is the gradual introduction of new dishes and products, monitoring based on tolerance.
What can you eat
Diet 4b allows:
- soup with a decoction of vegetables, meat, fish with pureed cereals, small noodles, vegetable puree, meatballs made from low-fat meat and fish;
- dried bread, dry biscuits, biscuits. No more than once a week you can bake homemade cakes with cottage cheese, apples or jam;
- milk, cream for adding to dishes;
- kefir, yogurt, homemade cottage cheese, casseroles, puddings;
- beef, chicken, turkey for cutlets, souffle, meatballs;
- chicken, rabbit and veal - boiled beef stroganoff;
- pike perch, perch, pike, boiled, steamed, for chopped products;
- mashed potatoes, carrots, cauliflower;
- boiled pumpkin, young zucchini;
- half a fresh tomato without skin;
- eggs for omelet, soft-boiled;
- oatmeal, pureed buckwheat porridge, casseroles, noodles;
- broth-based sauces made from meat or vegetables;
- dill, parsley;
- sweet and ripe fruits no more than 100 g fresh;
- mashed compote, mousses, baked apples;
- dessert – marmalade, marshmallows, jam;
- drinks - juices half and half with water, rosehip decoction, weak tea and coffee (can be with milk).
Not recommended for use in food:
- fresh bread, rye, with bran, products made from butter, puff pastry;
- borscht, beetroot soup, okroshka, rassolnik, soup with legumes, milk;
- lamb, pork, goose, smoked sausages, canned food, salted fish;
- fried eggs;
- pearl barley, millet;
- mushrooms, onions, turnips, radishes, beets, garlic, cucumbers;
- spinach, sorrel, wild garlic;
- plums, apricots, dried fruits, grapes;
- ice cream, cake, pastry;
- horseradish, vinegar, mustard, pepper.
Nutrition for patients with a subsiding exacerbation or with an initial tendency to constipation includes:
- oatmeal with apples, rosehip tea;
- cottage cheese with cream and pumpkin puree;
- zucchini and cauliflower soup with fish balls, steam omelette;
- baked apples and dried biscuit;
- chicken beef stroganoff with mashed potatoes and tomato;
- yogurt with biscuits.
To prepare you should take:
- pike perch fillet – 200 g;
- potatoes - 2 pieces;
- carrots – 1 piece;
- cauliflower - a third of a small head of cabbage;
- zucchini - a third of a small one;
- semolina - dessert spoon without top;
- egg - 1 piece;
- salt - to taste;
- water – 1.5 liters.
First, potatoes, carrots and cauliflower are thrown into boiling water. Cook them until fully cooked. At this time, the pike perch fillet is passed through a meat grinder twice, an egg, salt and semolina are added. Leave for 20 minutes.
The resulting vegetable soup is whipped with a blender, placed on low heat, and zucchini cut into small cubes is thrown into it. Then, using a spoon, form small meatballs and lower them into the soup; when they all float to the surface, boil for another 5 minutes and remove from heat.
For this dish you need:
- chicken fillet 150 g;
- carrots - one small;
- parsley root – 5 g;
- salt 1 g;
- sour cream 20 g.
Boil the chicken fillet until fully cooked with parsley root, carrots and cut into strips. Grind the carrots to a puree. Add carrots and sour cream, diluted half with broth, to the chopped boiled meat, simmer all together for another 5 minutes.
When a patient does not follow the recommendations of the attending physician, unpleasant consequences arise. Treatment of ulcerative colitis is carried out comprehensively; if only medications are taken, then the therapy will not bring a positive effect, and relapses will become more frequent. However, not only health, but also life is at risk.
The inflammatory process in the colon and rectum can progress. This leads to the manifestation of symptoms of complications. In this case, bleeding, perforation of the colon, peritonitis and cancer often occur. All these diseases develop against the background of untreated ulcerative colitis. However, in addition to diet, you can use traditional medicine methods.
The symptoms of the disease depend on where exactly the pathological process is localized and on its intensity. In addition, it is worth distinguishing between intestinal and extraintestinal manifestations.
Intestinal symptoms include:
- The appearance of diarrhea, in which blood impurities are found. Often, in addition to bloody clots, mucus and pus are present in the stool, which gives them a fetid odor. It happens that blood with mucus and pus appears in between bowel movements. The frequency of stool varies depending on the severity of the disease and can reach up to 20 times per day. A person can lose up to 300 ml of blood per day. With a milder course of the disease, a person defecates several times, more often in the morning and at night.
Pain symptoms also vary in severity. They can be either sharp, causing severe discomfort, or weak, not causing serious suffering to a person. Sometimes it is not possible to get rid of painful sensations even with the help of medications, which indicates the development of complications of the disease. The location of the pain is the left side of the abdomen or the left iliac region. As a rule, increased pain occurs before the act of defecation, and after it they subside somewhat. Also, the pain may increase in severity after eating.
Fecal incontinence.
Change from diarrhea to constipation. Such a transition is a sign that severe inflammation has begun to develop in the mucous membrane lining the colon.
Sometimes ulcerative colitis can develop rapidly. This form of the disease is called fulminant and will be discussed below.
Varieties
The varieties are Diets 4A , 4B , 4B , differing in the set of products and indications for use.
Thus, Table 4A is recommended for colitis with a predominance of fermentation processes, therefore carbohydrates are strictly limited in the diet (sugar up to 20 g, cereals, bread up to 100 g). Diet No. 4A for chronic colitis involves increasing protein intake through cottage cheese and meat dishes. Otherwise, it is not much different from the main diet and includes: one soft-boiled egg daily, slimy soups, pureed rice and semolina porridge, boiled meat and fish, low-fat kefir, decoction of blueberries and black currants, jelly and jelly from these berries.
Table 4B is prescribed for chronic colitis during the period of improvement (phase of fading exacerbation) or for mild exacerbation. The diet is characterized by a large amount of proteins (100-110 g), an increase in fats (up to 100 g) and carbohydrates (up to 400-420 g). The diet remains the same as with the main diet, but the list of permitted foods has been significantly expanded by including noodles, potatoes, noodles, carrots, cauliflower, zucchini, cream, sour cream, kefir, and sweet berries in the diet.
Table 4B is indicated during the period of recovery from acute colitis and the transition to normal nutrition. It is also prescribed for chronic intestinal diseases outside of an exacerbation or during the period of attenuation of an exacerbation. The chemical composition is the same as that of the previous table, but vegetable fats are already included and the list of products is expanding: pies, cabbage, savory buns, green peas, doctor's sausage, milk, ham, beets, oranges, grapes, watermelon, raspberries, tangerines, strawberries, increased the amount of butter to 15 g.
Forms of colitis and diet
Of course, the fundamental role in choosing a diet is played by the opinion of a doctor who specializes in developing nutritional systems for gastroenterological patients. When choosing a diet, specialists are guided by information about what stage the disease is at, how it progressed previously, and what degree of intestinal damage is currently present. If the diet was chosen correctly, then after the first week of following it the patient’s condition will improve significantly.
During treatment by adjusting the diet, the patient should remember the following rules:
- fried foods are vetoed; absolutely all food must be steamed or boiled;
- the food temperature should be as close to room temperature as possible, since too cold or hot food negatively affects the digestion process;
- the most high-calorie dishes present in the diet should be consumed before 12 noon;
- the main principle of nutrition should be fractionation, which is why the number of meals should range from 5 to 6 times a day;
- 3-4 hours before bedtime you must refuse food;
- it is necessary to constantly adjust food portions and try not to eat the entire daily diet at once after returning from work/school;
- the amount of protein in a person’s diet should be from 2-2.5 g per kg of person’s weight;
- products must be selected carefully, constantly paying attention to their quality and naturalness.
The main thing is to remember that if you follow all the rules prescribed by your doctor, you can significantly improve your own well-being and normalize the functioning of your digestive tract in a short period of time. You just need to want it!
Dietary nutrition for this disease is primarily aimed at alleviating the patient’s condition, reducing the inflammatory process and pain in a person.
Due to the fact that in most cases ulcerative colitis occurs in a chronic form, adult patients will have to follow this dietary menu for years, and in some cases, throughout their lives.
The following are the main dietary provisions for children and adults with ulcerative colitis:
- Meal frequency. The patient needs to eat at least five times a day. At the same time, portions should be small. This way, the person will be full, but at the same time, not overload the digestive system with too much food.
- Dishes must be served warm. You cannot eat hot or cold food.
- You should maintain a balanced diet and do not combine difficult-to-digest foods at one meal.
- Heat treatment rules. Cooking, stewing, baking, and steaming are allowed. Everything else (grilling, frying, smoking, etc.) is strictly prohibited.
- It is important to maintain a stable water balance in the body and drink at least two liters of water per day.
- Most of your nutritional intake should come before lunch. Thus, meat, fish dishes and cereals should be eaten before three o'clock in the afternoon. After this, it is advisable to give preference to light snacks and vegetable dishes.
- The time for dinner should not be later than seven o'clock in the evening. After this, you are only allowed to drink weak tea and chamomile decoction.
- The patient should receive more than 70% of all proteins from meat and fish. It is especially important to increase protein intake in acute ulcerative colitis.
- The menu should be enriched with foods that will reduce intestinal motility.
- The daily carbohydrate intake should not exceed 250 g.
- To support the body while following this diet, it is recommended to supplement the menu with vitamin complexes containing vitamin A, C, K and calcium.
In case of an acute attack of colitis, the diet should be very strict and restrictive in the first few days. In general, doctors in this condition recommend that the patient refuse food altogether for a couple of days and give the intestines time to rest. At the same time, the patient is only allowed to drink light teas, rosehip and blueberry decoctions.
A couple of days after an attack of illness, you can already add light boiled vegetables and porridge to the menu. Gradually, other foods should be introduced into the diet, including meat, fish and cottage cheese.
If a chronic form of colitis is detected, you need to follow a diet for at least five months to normalize your condition. In this case, a person needs to completely exclude from the menu those foods that can cause an exacerbation of the disease.
Only by carefully following all medical recommendations can a person minimize the unpleasant symptoms of the disease and normalize his condition.
If the patient’s colitis is in remission and significant improvements are observed, then the diet can be somewhat diversified and supplemented with regular foods. The main thing is not to overdo it and start eating everything.
These are not the only diseases that affect the small intestine, but the diet for most diseases is almost identical.
Authorized Products
The diet is based on pureed porridges: semolina, rice (white), buckwheat and oatmeal, which are cooked in water; you can also use low-fat broth. All dishes are boiled or stewed. Butter is added to dishes (5 g per serving). Wheat bread is allowed and only dried or in the form of crackers. You can eat 200 g of crackers per day. Dry cookies are allowed.
Soups are prepared with water or low-fat and weak fish/meat broth, adding a minimum of pureed vegetables (or vegetable broth), pureed meat, egg flakes, quenelles or meatballs. It is recommended to consume lean varieties of beef, chicken, veal or turkey. The meat is additionally degreased, and the poultry is cooked without skin. Steam cutlets or meatballs are prepared from minced meat.
Cutlets can also be stewed in a small amount of water. When preparing cutlets or meatballs, boiled rice is added to the minced meat. Use low-fat sea fish, prepare it in pieces or in the form of cutlets and meatballs. Up to two eggs per day (soft-boiled, steam omelet) are allowed; they can be added to soups.
Cottage cheese can only be freshly prepared, calcined, unleavened (non-acidic) and pureed. It is also used in casseroles. Vegetables are used only as an additive to soups. Mashed raw apples and applesauce are allowed. Berry jelly, decoctions and fruit drinks are prepared from blueberries, dogwood, quince, bird cherry, black currant, and blueberry pears. Allowed: herbal tea, rosehip decoction, green and black tea, still water up to 1.5 liters per day. If well tolerated, diluted fresh juices from non-acidic berries are allowed.
Table of permitted products
| Proteins, g | Fats, g | Carbohydrates, g | Calories, kcal | |
Fruits | ||||
| quince | 0,6 | 0,5 | 9,8 | 40 |
| pears | 0,4 | 0,3 | 10,9 | 42 |
| dogwood | 1,0 | 0,0 | 10,5 | 44 |
| apples | 0,4 | 0,4 | 9,8 | 47 |
Berries | ||||
| blackberry | 2,0 | 0,0 | 6,4 | 31 |
| blueberry | 1,1 | 0,4 | 7,6 | 44 |
Nuts and dried fruits | ||||
| dried pears | 2,3 | 0,6 | 62,6 | 249 |
| dried blueberries | 0,9 | 0,7 | 72,3 | 309 |
Cereals and porridges | ||||
| buckwheat (kernel) | 12,6 | 3,3 | 62,1 | 313 |
| semolina | 10,3 | 1,0 | 73,3 | 328 |
| oat groats | 12,3 | 6,1 | 59,5 | 342 |
| cereals | 11,9 | 7,2 | 69,3 | 366 |
| white rice | 6,7 | 0,7 | 78,9 | 344 |
Bakery products | ||||
| white bread crackers | 11,2 | 1,4 | 72,2 | 331 |
Confectionery | ||||
| Maria cookies | 8,7 | 8,8 | 70,9 | 400 |
Raw materials and seasonings | ||||
| dried bird cherry | 8,4 | 0,0 | 16,8 | 101 |
Dairy | ||||
| acidophilus | 2,8 | 3,2 | 3,8 | 57 |
Cheeses and cottage cheese | ||||
| cottage cheese 0.6% (low fat) | 18,0 | 0,6 | 1,8 | 88 |
Meat products | ||||
| boiled beef | 25,8 | 16,8 | 0,0 | 254 |
| boiled veal | 30,7 | 0,9 | 0,0 | 131 |
| rabbit | 21,0 | 8,0 | 0,0 | 156 |
Bird | ||||
| boiled chicken | 25,2 | 7,4 | 0,0 | 170 |
| turkey | 19,2 | 0,7 | 0,0 | 84 |
Oils and fats | ||||
| butter | 0,5 | 82,5 | 0,8 | 748 |
Non-alcoholic drinks | ||||
| mineral water | 0,0 | 0,0 | 0,0 | — |
| green tea | 0,0 | 0,0 | 0,0 | — |
| black tea | 20,0 | 5,1 | 6,9 | 152 |
| * data is per 100 g of product | ||||
Prohibited Products
There is a list of prohibited ingredients that can intensify the inflammatory process in the mucous membrane of the large intestine or cause a relapse of the disease. Thus, the diet for nonspecific ulcerative colitis involves avoiding:
- baked goods and confectionery products - they can provoke the appearance of symptoms such as painful intestinal spasms and constipation, which is extremely undesirable during the course of such an illness;
- fresh bread;
- fatty, spicy and salty dishes;
- chocolate and other sweets, including homemade ones, such as honey or jam;
- onions and garlic - they contribute to irritation of the mucous membrane, which, in turn, leads to pain;
- fast food - such dishes are often prepared with large amounts of oil, enriched with spices, flavor enhancers, carcinogens and preservatives, which are an irritant to the mucous membrane of the stomach and colon;
- pickles and marinades - they cause an increase in the acidity of gastric juice, which can cause heartburn;
- canned and smoked meats - worsen digestion processes;
- any carbonated and alcoholic drinks;
- mushrooms and legumes;
- whole milk;
- offal;
- pearl barley and millet;
- seeds and nuts;
- plums and apricots;
- mayonnaise and hot sauces.
It makes no sense to adhere to such dietary restrictions for nonspecific ulcerative colitis longer than the exacerbation of such a disease lasts. The attending physician may allow minimal consumption of prohibited foods. Restrictions can slow down metabolism and recovery. You can expand the diet five days after the onset or exacerbation of the disease.
Recommendations regarding sample menus and recipes for preparing dishes for UC are provided by a nutritionist or gastroenterologist.
Fully or partially limited products
In therapeutic nutrition, foods containing fiber are completely excluded: vegetables (even boiled), bran, rye and whole grain, bread with added seeds, since they injure the mucous membrane and are almost not digested.
Fresh bread, pastries, and flour products cause fermentation in the intestines, so they are completely excluded from the diet. For the same reason, jam, dried fruits, honey and other sweets are prohibited, and sugar is allowed in the amount of 50 g per day, including its addition to dishes.
Rich fatty broths are prohibited, as they increase peristalsis, fatty meats, any sausages, fatty fish and canned food (meat, fish). During the period of exacerbation, porridges made from coarse cereals (barley, millet, pearl barley) and poorly digestible legumes and pasta are excluded. Soups with whole grains, vegetables, pasta, and milk soups are not allowed. Hard-boiled and fried eggs should not be consumed.
Whole milk, cream and sour cream can cause diarrhea , so they are excluded. Milk is used in diluted form in the preparation of puddings. Kvass, cocoa and coffee with milk increase intestinal motility, and drinks with gas additionally cause bloating.
Table of prohibited products
| Proteins, g | Fats, g | Carbohydrates, g | Calories, kcal | |
Vegetables and greens | ||||
| vegetables | 2,5 | 0,3 | 7,0 | 35 |
| vegetables legumes | 9,1 | 1,6 | 27,0 | 168 |
| canned vegetables | 1,5 | 0,2 | 5,5 | 30 |
| horseradish | 3,2 | 0,4 | 10,5 | 56 |
Fruits | ||||
| bananas | 1,5 | 0,2 | 21,8 | 95 |
| melon | 0,6 | 0,3 | 7,4 | 33 |
Berries | ||||
| grape | 0,6 | 0,2 | 16,8 | 65 |
Mushrooms | ||||
| mushrooms | 3,5 | 2,0 | 2,5 | 30 |
Nuts and dried fruits | ||||
| dried fruits | 2,3 | 0,6 | 68,2 | 286 |
Cereals and porridges | ||||
| pearl barley | 9,3 | 1,1 | 73,7 | 320 |
| Wheat groats | 11,5 | 1,3 | 62,0 | 316 |
| millet cereal | 11,5 | 3,3 | 69,3 | 348 |
| barley grits | 10,4 | 1,3 | 66,3 | 324 |
Flour and pasta | ||||
| pasta | 10,4 | 1,1 | 69,7 | 337 |
Confectionery | ||||
| jam | 0,3 | 0,2 | 63,0 | 263 |
| jam | 0,3 | 0,1 | 56,0 | 238 |
| candies | 4,3 | 19,8 | 67,5 | 453 |
| pastry cream | 0,2 | 26,0 | 16,5 | 300 |
| cookie | 7,5 | 11,8 | 74,9 | 417 |
| shortbread dough | 6,5 | 21,6 | 49,9 | 403 |
Ice cream | ||||
| ice cream | 3,7 | 6,9 | 22,1 | 189 |
Cakes | ||||
| cake | 4,4 | 23,4 | 45,2 | 407 |
Chocolate | ||||
| chocolate | 5,4 | 35,3 | 56,5 | 544 |
Raw materials and seasonings | ||||
| seasonings | 7,0 | 1,9 | 26,0 | 149 |
| mustard | 5,7 | 6,4 | 22,0 | 162 |
| ketchup | 1,8 | 1,0 | 22,2 | 93 |
| mayonnaise | 2,4 | 67,0 | 3,9 | 627 |
Dairy | ||||
| milk | 3,2 | 3,6 | 4,8 | 64 |
| kefir | 3,4 | 2,0 | 4,7 | 51 |
| sour cream | 2,8 | 20,0 | 3,2 | 206 |
Cheeses and cottage cheese | ||||
| cheese | 24,1 | 29,5 | 0,3 | 363 |
Meat products | ||||
| pork | 16,0 | 21,6 | 0,0 | 259 |
| ham | 22,6 | 20,9 | 0,0 | 279 |
Sausages | ||||
| dry-cured sausage | 24,1 | 38,3 | 1,0 | 455 |
| sausages | 10,1 | 31,6 | 1,9 | 332 |
| sausages | 12,3 | 25,3 | 0,0 | 277 |
Bird | ||||
| duck | 16,5 | 61,2 | 0,0 | 346 |
| goose | 16,1 | 33,3 | 0,0 | 364 |
Fish and seafood | ||||
| dried fish | 17,5 | 4,6 | 0,0 | 139 |
| smoked fish | 26,8 | 9,9 | 0,0 | 196 |
| canned fish | 17,5 | 2,0 | 0,0 | 88 |
Oils and fats | ||||
| vegetable oil | 0,0 | 99,0 | 0,0 | 899 |
| animal fat | 0,0 | 99,7 | 0,0 | 897 |
| cooking fat | 0,0 | 99,7 | 0,0 | 897 |
Non-alcoholic drinks | ||||
| bread kvass | 0,2 | 0,0 | 5,2 | 27 |
| coffee with milk and sugar | 0,7 | 1,0 | 11,2 | 58 |
Juices and compotes | ||||
| apricot juice | 0,9 | 0,1 | 9,0 | 38 |
| grape juice | 0,3 | 0,0 | 14,0 | 54 |
| plum juice | 0,8 | 0,0 | 9,6 | 39 |
| * data is per 100 g of product | ||||
Prohibited Products
The menu of the treatment table for colitis should not include those foods that cause fermentation and putrefaction in the intestines, stimulate gas formation and peristalsis.
These include both coarse plant fiber and legumes. In addition, it is not recommended to consume spices - they are irritating to the digestive tract.
Fats, especially of plant origin, are also limited, as they interfere with the absorption of nutrients in the intestines and speed up bowel movements, which is not good for diarrhea. The same applies to dairy products, especially if you are lactose intolerant.
Stimulators of bile secretion and the release of pancreatic enzymes, for example, extractives, increase the load on the liver and worsen the course of colitis.
List of foods prohibited for colitis
- brown bread, wholemeal or whole grain bread, baked goods;
- rich meat and fish broths;
- pasta, beans, peas, lentils, beans;
- fatty meats and poultry, especially fried foods;
- pickles, marinades, smoked meats;
- canned food, caviar;
- fatty fish;
- mushrooms in any form;
- raw vegetables;
- raw fruits and berries, dried fruits, honey, jam;
- dairy products, whole milk;
- coffee and cocoa with milk;
- nuts;
- fast food, chips, crackers;
- fried or hard-boiled eggs;
- spices (mustard, pepper, vinegar, garlic and others);
- cereals: pearl barley, barley, wheat, wheat, barley;
- fats other than butter.
Menu diet for intestinal colitis (Diet regimen)
It is necessary to organize 6 meals a day and so that the food menu for the week includes alternating a variety of protein dishes (chicken, fish, beef, cottage cheese) and cereals. You can include egg dishes daily.
It must be remembered that with ulcerative colitis, the diet must be followed for a long time and new foods must be introduced very carefully. It is advisable to permanently exclude mushrooms, corn, legumes, seeds, poppy seeds and nuts, and give up hard meat.
When the process subsides, you can add pureed vegetables with low fiber content (pumpkin, zucchini, potatoes). If you are intolerant to dairy products, you can get calcium by introducing calcined cottage cheese from soy milk and broccoli dishes into your diet. The required amount of protein is calculated based on 1.5–2 g per kilogram of weight. During the day, 200 g of dried wheat bread is allowed.
Below is a sample menu for several days.
Monday
| Breakfast |
|
| Lunch |
|
| Dinner |
|
| Afternoon snack |
|
| Dinner |
|
| For the night |
|
Tuesday
| Breakfast |
|
| Lunch |
|
| Dinner |
|
| Afternoon snack |
|
| Dinner |
|
| For the night |
|
Wednesday
| Breakfast |
|
| Lunch |
|
| Dinner |
|
| Afternoon snack |
|
| Dinner |
|
| For the night |
|
Nutrition rules for ulcerative colitis
An important element of effective treatment of intestinal colitis is the patient’s compliance with the recommended diet, which is selected in accordance with the characteristics of the course and nature of the pathology. Nutrition for ulcerative colitis is carried out according to the following general rules:
- Eating meals six times a day on a fractional basis.
- The menu is based on semi-liquid, pureed, ground dishes.
- The main method of cooking is steaming or boiling.
- Hot and cold dishes, thick, solid foods are excluded.
- Maintaining water regime (from 1.5 to 2 l).
- Reducing the amount of fats and carbohydrates in the diet.
Recipes
First meal
Meat broth with egg flakes
Weak beef broth, egg, butter.
Add salt to the broth, bring to a boil, add butter. Through a colander, add a well-beaten egg into the broth and stir quickly.
Poultry puree soup with rice
Chicken meat, rice, water, butter, crackers.
Boil the rice well and puree. Also puree the pulp of boiled chicken or beat it in a blender. Combine the rice water with the pureed meat, add salt and oil, and boil everything together.
Second courses
Meat meatballs with rice
Beef, rice, salt.
Add boiled and grated rice to the prepared minced beef, add salt and beat. Cut the mixture into balls and cook in a double boiler.
Boiled cod with Polish sauce
Cod, for sauce - fish broth, flour, salt, egg.
Cut the fish into portions and boil in salted water. Dry the flour in a frying pan without oil, add fish broth, add salt and boil for 3-5 minutes. Add chopped or grated boiled egg. When serving, pour the sauce over a portion of cod.
Beverages
Blueberry jelly
Blueberries, sugar, potato starch, water.
Sort the blueberries, puree and squeeze out the juice. Pour water over the pulp and boil for 10 minutes. Strain the finished broth and add sugar, boil and gradually pour in some of the juice with starch. Stirring, bring to a boil and add the rest of the juice at the end.
Diet No. 4
Useful article? Share the link on VKontakte
What is the correct diet for colitis during an exacerbation? Experts in the field of gastroenterology recommend sticking to a special menu. It is also known as Diet No. 4. It is characterized by the following features:
| Characteristic | Description |
| Indications | Chronic or acute form of colitis |
| Target | Normalization of digestion, suppression of inflammation, inhibition of fermentation and putrefactive processes. |
| Mechanism | Reducing the amount of carbohydrates and fats (while maintaining normal protein content). Limiting chemical and thermal irritation of the mucous membranes of the stomach and intestines. The diet is based on the consumption of liquid dishes, steamed or boiled in water. |
| Chemical composition |
|
| Number of meals | 5-6 |
Reviews and results
Analyzing patient reviews, we can conclude that this therapeutic diet has a positive effect on the gastrointestinal tract: pain and stool frequency are reduced, bloating and rumbling in the intestines are eliminated. Most often there are reviews from patients with nonspecific ulcerative colitis, who are forced to constantly follow a very strict diet and expand it slightly if their health condition allows.
Here are some reviews:
- “... I am suffering from UC. For me, this is a way out, so I’ve been eating this way for several months. I cook everything in a slow cooker, and have already adapted to making many dishes. During this time, the stool almost returned to normal, the blood and mucus had long since disappeared. When the condition improves, I slightly increase the amount of sugar and vegetable oil, and add pureed boiled vegetables”;
- “... For chronic colitis during exacerbation, I adhere to this diet. The truth is that it doesn’t last long for me - three or four weeks, but even during this time I restore my intestines: there is no pain or bloating, heartburn disappears. At this time, the whole family eats steamed and stewed dishes, but they quickly get bored”;
- “... I prepared steamed dishes for a child with an intestinal disorder. She gave decoctions of blueberries and dried pears. I drank jelly with pleasure and ate crackers. The main thing is to eat little and often so that there is no deterioration. After two days, the stool returned to normal and the mucus disappeared.”
The need to follow a diet
Following a diet for colitis normalizes the functioning of the large intestine and the entire digestive tract as a whole. Also, a treatment table for illness will ensure the absorption of nutrients, vitamins and microelements, normalize appearance and weight, and stimulate the immune system.
Normal functioning of the gastrointestinal tract has a beneficial effect on the mental state, eliminates emotional excitability, and has a positive effect on sleep.
In addition, if the patient follows a diet, all the unpleasant sensations associated with colitis are relieved, abdominal pain disappears, and stool normalizes.
Recommended Products
People suffering from chronic or acute colitis are recommended to follow the so-called diet No. 4. It includes food that not only does not harm the intestines, but also helps maintain its functional state. Thus, a diet for colitis during an exacerbation involves consuming the following products:
- dairy products;
- slimy soups based on low-fat broth;
- white meat and fish, steamed or boiled;
- rice, semolina or oatmeal porridge cooked in water;
- jelly and jellies based on fruits and berries;
- boiled eggs or omelet;
- rosehip decoction;
- fresh fruits and vegetables in grated form;
- hard cheeses (unsalted);
- biscuits;
- cinnamon as a seasoning.
Inadmissible foods on the diet.
The following products are considered dangerous:
- cow or goat milk;
- meat from pork, lamb, duck, goose;
- fatty fish;
- barley or millet porridge;
- chocolate, sweets, confectionery, ice cream, etc.;
- food prepared from legumes;
- vegetables - cabbage, beets;
- conservation;
- alcoholic drinks;
- juices from peach, grapes, apricot;
- coffee, black tea, carbonated drinks.
Menu with nyak recipes |
The diet for nonspecific ulcerative colitis is designed to support the process of restoration of the colon mucosa. Our article is devoted to her recommendations.
What is ulcerative colitis?
Nonspecific ulcerative colitis (UC) is an inflammatory-dystrophic autoimmune lesion of the colon, accompanied by the development of erosions, hemorrhages and ulcers. The disease is characterized by some extraintestinal symptoms, in addition, it provokes the development of complications of various types.
Even after the clinical signs of UC disappear, a long period of time is required for complete restoration of the intestinal mucosa and normalization of digestive processes. Nutrition in UC plays an important role in reducing the duration of remission. It has been noticed that even minor dietary violations lead to a noticeable deterioration in the condition of patients.
Basic nutritional recommendations for UC
In case of nonspecific ulcerative colitis, nutrition is organized taking into account the fact that most patients have food allergies. In particular, this is manifested by increased sensitivity to the protein contained in cow's milk. The diet for UC excludes any dairy products from the diet (kefir, cottage cheese, fermented baked milk, sour cream, cheeses). The diet includes only melted butter.
It is recommended to cook all dishes in water or in weak fish and meat broth. You should eat 4-6 times a day (the number of meals depends on the stage of the disease). In the acute stage, you need to increase your protein intake (of the total norm, 65-70% should be animal proteins).
Particular attention is paid to products that reduce intestinal motility. Tannins and astringents are useful - jelly and decoctions of bird cherry, blueberry, pear, dogwood, quince.
Patients should pay attention to strong green and black tea, cocoa prepared with water, slimy soups, porridges (during an exacerbation, buckwheat should be avoided - it provokes increased intestinal motility). It is recommended to serve the dishes warm.
Optimal chemical composition of the diet
Nutrition for nonspecific ulcerative colitis should include the following set of elements:
- Proteins - 120-125 g (approximately 1.5-1.8 g / 1 kg of body weight) Fats - 55-60 g (vegetable and ghee oils should be present in the diet) Carbohydrates - 200-250 g
Serious restrictions are placed on foods rich in fiber. First courses should be cooked in water, as well as in fish or meat broth diluted with boiled water. You can add potatoes, rice, noodles, boiled meat or meatballs to soups.
When stable remission occurs, a small amount of vegetables is allowed into the diet (priority with cauliflower, broccoli, carrots, onions, zucchini).
It is worth excluding tomatoes, citrus fruits, peaches, raspberries, strawberries, grapes, melon, and watermelons from the diet. If tolerated well, you can eat pomegranates, blueberries, blackberries, cranberries, as well as oven-baked apples and pears. It is useful for patients to drink chokeberry juice.
Low-fat varieties of fish, meat and poultry are served boiled (the easiest to digest are soufflés, steamed minced meat products, and casseroles). As side dishes, you can use boiled potatoes, rice and wheat porridge, and boiled pasta.
Eggs may be present in the diet (if you are not allergic to them), but they should be boiled soft-boiled or served as a steam omelet. You are supposed to eat no more than two or three pieces per week.
The diet for nonspecific ulcerative colitis allows you to eat day-old white bread and dry biscuits. Pies, fresh bread, and sweets are prohibited.
Approximate diet for UC
- Breakfast: rice porridge with melted butter, steam cutlet and tea Second breakfast: boiled meat (about 40 g) and blueberry jelly Lunch: potato soup with meatballs, rice casserole with minced meat, dried fruit compote Afternoon snack: lightly brewed tea and croutons Dinner: mashed potatoes, steamed fish cutlet and tea Before bed: baked apple All day: 200 g day-old wheat bread
Nutrition for nonspecific ulcerative colitis is based on maximum sparing of the gastrointestinal mucosa. It is worth adjusting the diet taking into account the recommendations of the attending physician.
Diet for ulcerative colitis
This disease belongs to proctocolitis. Ulcerative colitis of the intestine manifests itself as diffuse inflammation of the intestinal mucosa, limited to the colon, and permanent damage to the rectum. Diet for this disease is one of the important components of successful treatment of the disease. What can you eat? Find more detailed information on this topic further in the article.
What should the diet be like?
Nutrition is aimed at eliminating the symptoms of the disease, while medications directly “fight” the disease. The main rules of the menu are:
Food should only be steamed, boiled, and eaten warm.
You need to eat at least five times a day.
Almost the entire prescribed diet should be eaten before lunch.
You can't eat after 7 p.m.
Low-fat varieties of meat, fish and poultry, stewed, boiled and, as an exception, fried, are suitable for the diet. Soups are prepared using weak and low-fat meat and fish broths.
Vegetarian first courses (including mushroom ones) are also allowed in the diet. They are seasoned with chopped vegetables and various cereals.
What should you eat in case of exacerbation of colitis?
During the period of exacerbation of the disease, rich food is poorly digested and absorbed, so frequent meals are recommended, but in small portions. The last meal is no later than 21:00.
Ulcerative colitis disrupts protein metabolism, especially in the recurrent period of the disease. At this time, it is recommended to eat foods that contain increased amounts of protein. Fluid intake is limited.
As your health improves, your diet will be expanded, but dairy products will have to be eliminated for life.
The diet for ulcerative colitis in the period of exacerbation of moderate severity has the following characteristics:
The diet should contain an increased amount of proteins, most of which are of animal origin (out of 100-110 g per day - 65%). Therefore, the patient should eat meat, fish and eggs, cottage cheese is possible. Dairy products in liquid form are contraindicated, and fish and meat should be low-fat and thoroughly chopped. Such dishes should be prepared by steaming or boiling.
The dose of carbohydrates daily should be 200-250 g, but fiber should be avoided. Possible semolina porridges, porridges from cereals, rice; Drinks you should consume include jelly, semi-sweet decoction of rose hips, blueberries, and black currants; It is possible to use juices with pulp. Fruits and vegetables should be consumed in pureed form.
Individual foods are gradually returned to the diet if improvements are noticeable.
Vitamins C, A, K, group B and calcium also need to be included in the diet for ulcerative colitis of the intestine in increased quantities, although they are usually already contained in medications.
In case of exacerbation of the disease, decoctions of rose hips, pears, blueberries and other sweet berries and fruits will be useful.
It is necessary to exclude everything fried, fatty, and salty from the diet. You should also limit the consumption of spicy foods, chocolate, legumes, mushrooms, fruits, vegetables, and plums.
Many patients do not tolerate various foods well, most often dairy products, so it is advisable to exclude them from the diet.
Until the exact reasons that cause ulcerative colitis are determined, a diet can help significantly improve your well-being.
It is recommended to eat lean meats (boiled or steamed), eggs, cereals, dry biscuits, and toasted white bread. You should also include walnuts in your diet.
There is no point in following a strict diet for a long time, since it will not be able to restore the metabolism and strength impaired due to illness. Dishes should be varied and tasty. A good sign is the patient's appetite returning. If an exacerbation occurs, you should immediately go to the hospital.
Diet for ulcerative colitis in remission. For approximately a month after an exacerbation, patients must adhere to a strict diet. Then the diet for ulcerative colitis is softened and with complete recovery you don’t have to stick to the diet.
If the patient's condition improves, the following diet is recommended: proteins - 100 g, fats - 100 g, carbohydrates - 400-450 g, table salt - up to 15 g.
You should eat food at least 4 times a day. It is steamed or boiled (sometimes it is possible to fry some dishes), and is served in crushed form.
For porridge, you can use any cereal, with the exception of pearl barley and millet. The diet includes pasta.
From dairy products you can eat fresh cottage cheese, non-acidic sour cream (as a seasoning for a dish), fermented milk products, milk (only in dishes), mild cheese. Eggs are cooked soft-boiled or scrambled. Unsalted butter is added to dishes.
As snacks in the diet for ulcerative colitis, lean ham, doctor's sausage, jellied meat or fish, beef liver or poultry liver pate, and soaked herring are offered.
Vegetables are served boiled or stewed. These are potatoes (mashed potatoes, casseroles), boiled cauliflower with butter, early zucchini and pumpkins (fried), white cabbage and beets (if well tolerated). Fresh tomatoes and cucumbers are not excluded from the diet.
You can eat any fruits and berries, with the exception of apricots, plums and melons. Fresh compotes, jellies, mousses, and rosehip decoction are relevant.
Drinks included in the diet include tea, water coffee with milk and cream.
You can add spices to dishes (in limited quantities): bay leaf, ground pepper, cinnamon, boiled onion.
Bakery products include day-old wheat bread, savory crackers and cookies, and, in limited quantities, pies with jam, rice, and meat.
- 1st breakfast: pureed fresh cottage cheese with sugar and sour cream, semolina porridge in milk with a piece of butter, raspberry juice (or rosehip decoction). 2nd breakfast: baked apple, tea with milk, crackers. Lunch in a diet for ulcerative colitis: noodle soup, potato roll with pureed meat, apple and pear jelly. Afternoon snack: rosehip decoction, a slice of toasted white bread. Dinner: steamed fish cutlet with mashed potatoes. Weak tea with crackers. At night: juice, crackers.
What can't you eat?
Prohibited in the diet:
Smoked meats and marinades.
Raw onions, garlic, sorrel, spinach, radishes, rutabaga.
Vinegar, mustard, horseradish, ground pepper.
Treatment for nonspecific ulcerative colitis
To effectively treat this form of the disease, you must follow a strict diet. It has its own specifics and is a necessary condition for successful therapy.
It is necessary that the dishes are tasty and varied. During the treatment of colitis, you can eat lean meat, steamed or simply boiled, mashed porridge, dry cookies, toasted white bread, and boiled eggs.
Be sure to eat walnuts.
In the acute form of the disease, it is recommended to use a decoction of rose hips, pears, blueberries and other sweet fruits and berries. You can even drink some juices - tomato, orange.
In the acute form of the disease, a large amount of food is very poorly digested and absorbed, so during the treatment period it is correct to eat in small portions with intervals between meals of no more than two and a half hours. It is better to have dinner before 21 o'clock.
With nonspecific ulcerative colitis, protein metabolism is quite severely affected. Disorders appear especially quickly during the period of relapse of the disease. For such problems, it is recommended to eat foods high in protein.
Also during this period it is worth reducing the amount of fluid intake. You need to focus on the nature of the feces. If they are abundant and watery, then you should limit yourself to five glasses of liquid per day.
If the condition improves, then it is allowed to slightly expand the diet, but poorly tolerated foods in the diet should not be consumed throughout life.
What should you not eat?
It is necessary to exclude fried, spicy, fatty, salty, chocolate and mushrooms, kiwi and beets, dried apricots and plums, legumes, fruits and vegetables from the diet for nonspecific ulcerative colitis.
During an exacerbation, you need to limit yourself from sweets and juices.
Many people who suffer from ulcerative colitis cannot tolerate various types of food, for example, dairy products. Therefore, by excluding them from your diet, you can significantly improve your well-being.
Source: https://imedic.club/menyu-pri-nyak-recepty/