Lower esophageal sphincter
In our country, traditional medicine actively uses for these purposes:
- surgical methods to strengthen the lower esophageal sphincter;
- stimulating its work through physiotherapy.
Other methods are not common among us. But if we consider the experience of all world practice, then an alternative technique already exists.
How to strengthen the esophageal sphincter? — There are several methods, which will be discussed now.
Non-traditional methods of treating the lower esophageal sphincter include therapeutic exercises. The complexity of this method lies in the lack of direct access to the muscles of the digestive system at this level. The esophagus, and therefore all its sections, are located inside the chest. This is not an area of the back or thigh muscles that can be easily toned. Even the stomach and intestines are easier to influence by contracting the abdominal muscles, or massage through passive movements.
The situation is more difficult with the esophagus; stimulating it requires great effort. But regular breathing exercises can help a little.
- The entire procedure must be carried out on an empty stomach (after all, any active movements on a full stomach lead to weakening of the lower esophageal sphincter).
- Almost the only organ in the chest area that can be controlled is the lungs. Therefore, we begin quite familiar and simple breathing movements. We inhale and exhale alternately.
- There is one small feature - the exercises are done not only with chest, but also with abdominal breathing. This is when, in the process of inhalation and exhalation, not only the chest rises and falls, but also the shoulders, plus the abdominal muscles are involved.
- This is the only way to increase the tone of the esophageal sphincter. Many internal organs are involved in the training process: the digestive and cardiovascular systems, respiratory organs, nearby muscles and blood vessels.
- It is necessary to inhale and exhale at different speeds: quickly, slowly, very slowly, gradually accelerating.
In the final stages of sphincter weakening, exercise will not help. But in the initial stages of loss of the sphincter’s ability to perform full contractions, it can be restored with the help of breathing exercises. It is enough to perform such active breathing movements daily for 10-15 minutes. And don’t be too lazy to do them 2-3 times at least 3 times a day.
Physiotherapy
One of the attempts to strengthen the sphincter comes from our physiologists. It was they who tried to approach the treatment of insufficiency of this muscle in a comprehensive manner - in the process of conventional conservative treatment (this also applies to the acute period of development of the disease), the esophagus and nearby organs are exposed to currents. Effectively used:
- DDT (diadynamic currents);
- electrophoresis with drugs;
- through a probe inserted inside.
How to strengthen the gastric sphincter using these effects? These methods also do not directly affect the affected area of the esophagus, since it is difficult to reach. They stimulate the phrenic nerve, which also innervates the esophagus. The electrodes through which the current is supplied are placed on the back of the cervicothoracic spine, and the second one is placed slightly behind the angle of the lower jaw. This is done from 7 to 10 procedures daily or every other day.
Electrophoresis with drugs is carried out in a similar way, but medicinal substances are additionally applied to the cuff with the electrode, which can inhibit excessive stimulation of hydrochloric acid production, which will directly lead to quiet functioning of the esophagus. What happens?
- Blood supply to tissues and organs improves.
- Healing processes occur much faster.
- The person notes a slight analgesic effect.
This way, without interfering with the integrity of the digestive organs, you can strengthen the tone of the lower esophageal sphincter.
The following method can be called an extreme case. It is used when everyone else is powerless, drug treatment does not help, and following a diet and rest regime is already pointless. Other criteria under which surgeons will take on you are deterioration in the functioning of other organs and systems, suppression of the nervous system and the appearance of complications associated with sphincter insufficiency.
The essence of this operation is to strengthen the lower esophageal sphincter. This is done thanks to the walls of the stomach, which line the lower part of the esophagus, creating a cuff. This creates additional pressure on the lower esophageal sphincter, which causes it to work better.
Having unsuccessfully tried all possible medicinal methods to get rid of heartburn, if you have problems with the esophagus, you should think about alternative methods of dealing with it. How to increase the tone of the esophageal sphincter yourself? Do some breathing exercises, even if such treatment raises some doubts, but this is another chance for a calm life.
A malfunction of the esophagus can provoke severe pathologies.
The cardia of the stomach is a valve that separates the abdominal cavity from the tissues of the esophagus (it is located between them). In other words, this is the vestibule of the stomach. The cardia has the main function of blocking the reflux of food. The contents of the organ include acid, and in the esophagus the reaction can be neutral or alkaline. The pressure in the stomach is higher than inside the esophagus, so it is important that when the lower sphincter opens, the contents do not end up on the esophageal mucosa.
What everyone needs to know about the gastric sphincter and how to prevent its diseases
The stomach is one of the most important digestive organs, which grinds food, mixes, disinfects and moves it further into the intestines. It is located under the diaphragm and borders the pancreas, duodenum, spleen, left edge of the liver, left kidney and adrenal gland.
The stomach wall has a three-layer structure:
- A layer of mucous membrane that produces hydrochloric acid (provides an acidic environment), hormones, and gastric juice. A certain amount of nutrients is absorbed in the mucous membrane.
- The muscle layer, which is formed by three groups of muscles - straight, circular and oblique, which allows you to grind food to a homogeneous consistency. Well-chopped food does not injure the delicate inner layer of the small intestine, moves easily through the intestines and is well absorbed.
- A layer of serous membrane, which is represented by connective tissue. It forms the ligaments that hold the stomach together and is the site of passage of nerves, arteries, veins and lymphatic vessels.
The shape of an empty stomach resembles a cow's horn or a bag; the shape of a filled organ is not constant and depends on the food consumed - liquid, gases, solid and dry food give different shapes. In people of asthenic physique, thin, with long and thin limbs, it has a more elongated and narrow shape; in children and people of hypersthenic physique #8212; more rounded shape. It contains the upper part or bottom, the body, two sphincters, the greater and lesser curvature.
The role of gastric sphincters in the human body
The human stomach has two sphincters #8212; cardiac and pyloric (gastroduodenal). Sphincters are formed by circular fibers of the muscle layer and folds of the mucous membrane.
Their main function is to move food forward through the intestinal tract and prevent it from being thrown back.
Cardiac sphincter
Located between the esophagus and stomach. It is a layer of ring-shaped muscles 0.5-1 cm long, which, by contracting, prevent the acidic contents from being thrown back into the esophagus. The fold of the mucous membrane acts as a barrier valve.
The sphincter opens when eating and closes when the food is digested, preventing backflow. The acidic contents of the stomach, namely hydrochloric acid, irritate the esophageal mucosa, leading to unpleasant sensations. The one-way movement of food is facilitated by the acute angle of confluence between the stomach and esophagus. The more the stomach fills, the smaller the angle becomes and the stronger the sphincter tone.
The tone of this sphincter is influenced by a number of factors:
- internal abdominal pressure,
- food consumed (sour, baked goods, salty, fast food),
- level of stomach distension,
- hormonal disorders,
- medications.
May change with straining or severe coughing.
Pyloric sphincter or pylorus
It is the final part of the stomach, located between the stomach and the small intestine (duodenum).
- Separates the gastric space from the intestinal;
- Controls the amount of acidic content that must enter the intestines to digest food;
- The pyloric sphincter of the stomach sets the tone for peristaltic movements of the intestine.
The pyloric sphincter opens according to a signal from the nervous system, receptors of the stomach and duodenum.
Diseases due to dysfunction of the sphincters
Esophageal achalasia (food cannot pass through the opening that is too narrow and gets stuck in the esophagus).
Gastroesophageal reflux disease (heartburn), esophagitis (inflammation of the esophagus), reflux is often the cause of asthma and laryngitis.
Pylorospasm (tight compression of the sphincter) and, in a more advanced state, pyloric stenosis.
Gastroduodenal reflux (reflux of contents from the duodenum back into the stomach). With a long-term untreated condition, gastroduodenal reflux can cause the development of metaplasia, that is, when the gastric epithelium located near the sphincter degenerates into intestinal epithelium. Metaplasia is a precancerous condition and must be treated and monitored.
Disease Prevention
- Eat food more often, but make smaller portions, do not overeat;
- Reduce the amount of coffee, fatty and fried foods you drink in your diet, do not abuse alcohol, citrus fruits and chocolate, do not drink mint tea, limit the consumption of garlic and onions, especially at night, exclude carbonated drinks, champagne;
- Do physical exercises to strengthen your abdominal muscles, but avoid strenuous exercise after meals;
- Control your weight;
- Do not eat 2 hours before bedtime;
- Stop smoking;
- Do not wear tight, tight clothing (corsets, tight belts, tight, high-waisted trousers);
- Consult a doctor in a timely manner if the functioning of the digestive system is disrupted.
Food through the intestinal tract should only move forward. Casting causes local irritation and inflammation, which leads to serious consequences. Long-term inflammation is a risk factor for the development of cancer.
Read also: Metal mouthpiece for hookah
Please note that heartburn is not a harmless complaint; such people should undergo a full examination and take medications that eliminate heartburn (omeprozole, ranitidine). Mild but prolonged pain in the upper abdomen may be a signal of a malfunction of the pylorus.
Conclusion . any symptom of digestive disorders should be monitored by a doctor, because it is much easier to treat them in the early stages.
Author . Pristavko Tatyana Aleksandrovna, pediatrician, especially for the site Moizhivot.ru
Gastroenterologists in your city
Terminology
Achalasia cardia is a disease of neuromuscular etiology and belongs to the chronic form. The disease is characterized by the absence or partial opening of the cardia when swallowing food. Against this background, the patency of the esophagus is disrupted, and chaotic contraction of the smooth muscles of almost all parts of the esophagus develops.
The cardia is a valve, or, in other words, the sphincter of the esophagus. The location of this organ is on the border between the esophagus and the stomach. The main purpose of the sphincter is to regulate food and feces as they move between parts of the body.
If the functioning of the valve is disrupted, then this pathology is called cardia insufficiency, or reflux.
Structural features
The esophagus has 2 valves:
- the lower one, connecting the esophagus and the section of the stomach located below, is also called cardiac;
- The pyloric sphincter of the stomach is also called the pylorus, which separates the duodenum and the pyloric region.
The fibers form the sphincter. When the muscles contract, the opening in the sphincter area closes (reduces in diameter). The organ has two sphincters:
- Pyloric sphincter or pylorus (superior). Separates the pyloric region of the stomach from the duodenum. Its functions include regulating the flow of stomach contents into the duodenum.
Job
Decreased tone. This pathology is characterized by the reflux of food particles or stomach contents into the upper esophageal region, sometimes into the pharynx. The socket begins to close insufficiently. Such disturbances in the functioning of the cardia can affect the lower esophageal sphincter or both sphincters simultaneously. Sometimes non-closure (when the sphincter does not close completely) and pressure provoke vomiting and nausea.
- Cardiac or lower esophageal sphincter. This sphincter is located at the border of the esophagus and the stomach. As food moves into the stomach, the cardiac sphincter opens slightly. Before this, it is closed due to muscle tone. This prevents stomach contents from entering the esophagus.
- Pyloric sphincter or pylorus (superior). Separates the pyloric region of the stomach from the duodenum. Its functions include regulating the flow of stomach contents into the duodenum.
Causes
Insufficiency of the cardia rosette can be caused by changes in the structure or structure of various esophageal sections. Scar formation can lead to a narrowing of the sphincter, which persists if the muscles are relaxed. The diameter of the sphincters may increase with diverticulum. In addition, expansion sometimes provokes stretching of the tissues of the lower region of the organ due to disruption of the functioning of one of the sphincters (cardiac). In such cases, it is weakened and cannot work properly.
Etiology
Cardiac failure is a polyetiological disease. There are many provoking factors that can cause this state of cardia. In some cases, valve failure occurs due to a complex of reasons.
- the presence of spasms in the pylorus;
- unhealthy diet, overeating;
- adynamia, swelling or high intra-abdominal pressure;
Pathology can manifest itself even in those people who do not have stomach problems. The risk group includes people over thirty-five years of age. With age, the disease manifests itself more intensely. This is explained by atrophy of the abdominal muscles and low motor activity.
According to medical data, stomach problems are less likely to occur in people with developed muscles and a toned stomach. Malfunction of the sphincter can occur during pregnancy, which is explained by the location of the internal organs.
Development mechanism
When the disease occurs, the lower esophageal sphincter stops relaxing during meals. If pressure on the inferior valve increases, the valve narrows further and the esophagus re-expands. As a result, undigested food accumulates.
Most often, the disease develops against the background of pathological changes in the nerve cells located between the walls of the esophagus and the muscle layers. The development of malignant neoplasms and diabetes mellitus can also cause the disease. A possible cause may be dystrophic changes in both muscle fibers and the plexuses of the esophagus, or Chagas syndrome after bedbug bites.
The pathology of achalasia cardia develops quite slowly. The diagnosis can only be made by X-ray examination or endoscopy.
Content
Formed by the lower constrictor of the pharynx (lat. musculus constrictor pharyngis inferior), its cricopharyngeal part. It is a thickening of the circular layer of striated muscles, the fibers of which have a thickness of 2.3-3 mm and which are located at an angle of 33-45° relative to the longitudinal axis of the esophagus.
The muscles of the upper esophageal sphincter are normally constantly contracted outside the act of swallowing. This is ensured by continuous nerve stimulation by somatic fibers, the motor neurons of which are located in the nucleus ambiguus. The sphincter remains closed due to the elasticity of the esophageal wall and the tonic contraction of the sphincter muscles.
During sleep, sphincter tone decreases. Its closed state is maintained only by basal muscle tone. However, the sphincter instantly responds to breathing, head position, stretching, stimulation and tension and thereby protects the esophagus.
The pressure that is created in the upper esophageal sphincter outside the swallowing phase reaches approximately 80-120 mmHg. Art..
Functional disorders of the upper esophageal sphincter can cause a variety of diseases. The most specific ones are listed below.
Dysphagia
The causes of dysphagia (impaired swallowing) can be pathologies of the upper esophageal sphincter caused by various diseases: bulbar poliomyelitis, cerebrovascular disorders, multiple sclerosis, muscular dystrophy, myasthenia gravis, dermatomyositis, pharyngoesophageal diverticulosis.
Degrees of deficiency
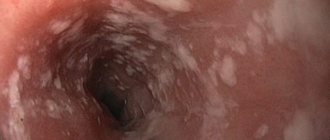
Pathology has several degrees of severity, which must be taken into account when prescribing therapeutic therapy. In many cases, the disease freezes at the first stage and does not progress. The symptoms bother you from time to time, without causing much discomfort. The severity of the disease can be determined using an endoscope, which can show whether the thickness of the cardia is increased and whether there are other lesions and complications.
To strengthen the cardia, there are special exercises, the implementation of which provides excellent results.
Stages
Today, there are several stages of pathology development:
Clinical picture of the pathology
Treatment for gastric cardia insufficiency is prescribed by a doctor. The course of therapy includes taking medications, exercise therapy and a diet. Signs of the disease in the initial stage may not appear or have insignificant intensity. Over time they become more pronounced. The main symptom of the pathological condition is heartburn, independent of food consumption.
After some time, a painful syndrome develops. The pain is concentrated behind the sternum, namely at the point of projection of the esophagus. The nature of the pain is cutting, burning. Belching of food or air occurs. It has a predominantly sour taste and unpleasant odor, which indicates the presence of gastric juice. If bitterness predominates, it means bile acid has entered.
In many cases, dyspeptic symptoms are observed, namely vomiting, nausea and heaviness. The disease may also be accompanied by dizziness, fatigue and weakness. The listed symptoms are similar to those of many other gastrointestinal diseases. Therefore, it is not recommended to self-medicate. See a doctor, get examined and take the necessary tests. To quickly get rid of the symptoms of the disease, you should strictly follow the instructions of the gastroenterologist.
Diagnostics
If suspicious signs appear, the patient should consult a doctor as soon as possible. If necessary, the specialist will refer the patient for further examination. To examine patients suffering from this pathology, it is customary to use the following diagnostic methods:
- X-rays help detect reflux esophagitis;
- gastrofibroscopy is considered the most informative type of research, as it allows for visualization of pathologies;
- study of the work of the cardia, esophagotonokymography, determination of the pH level in the esophagus, etc.
Diagnostic measures consist of conducting research methods aimed at differentiating other diseases of organs or systems with similar manifestations. The main measures include:
- study of clinical history;
- examination and palpation of the epigastric space;
- scintigraphy of the esophagus with contrast agent;
- performing FEGDS (fibroesophagogastroduodenoscopy);
- daily measurement of stomach acidity;
- X-ray.
Constant belching of air is a characteristic symptom of stomach problems. Belching can also occur in healthy people, but is often episodic and associated with large meals.
Individual signs
If gastric cardia insufficiency is diagnosed, doctors distinguish several syndromes:
- Dysphagia syndrome. Clinical manifestations in this case are as follows: a feeling as if there is a “lump” in the chest;
- hard to swallow;
- The patient constantly chokes while eating.
It is easier for the patient to eat solid than liquid food. This is due to the fact that solid foods put a lot of pressure on the pyloric sphincter and promote its opening. Simply put, there is a violation of the passage of food. These symptoms are very important for a correct diagnosis; for example, in the presence of cancer or stenosis, the clinical picture is the opposite, and it is difficult for the patient to eat solid food.
If the cardiac sphincter loses its functionality, then in addition to the syndromes described above, the patient also experiences other symptoms:
- unpleasant odor from the mouth due to changes in the diameter of the valve and the constant retention of food particles in the esophagus. Over time, this can cause erosions and ulcers on the mucous membrane;
- heartburn, the patient feels that the pain is burning and moves from bottom to top;
- some patients even feel how food moves through a valve that does not close, leaving behind a sour taste;
- belching with a sour taste;
- excessive salivation;
- hoarseness in the throat;
- problems with teeth and gums, caries;
- increased heart rate.
This pathology is a progressive condition, so exhaustion and deterioration are increasing.
Types of disorders and diseases
- Increased tone. With this disorder, it does not open completely when food particles pass through. The patient has impaired swallowing function. This pathology develops when exposed to ANS impulses. It is customary to distinguish between two types of this condition (the classification depends on where the pathology is located). Thus, improper functioning of the pharyngeal esophageal sphincter provokes disturbances during swallowing food. In this case, painful sensations arise, the patient may choke, and sometimes a cough appears when food enters the larynx area. If the esophageal sphincter, located between the abdominal cavity and the esophagus, begins to function incorrectly, then food can accumulate in the esophageal sections, which leads to expansion of the organ.
- Decreased tone. This pathology is characterized by the reflux of food particles or stomach contents into the upper esophageal region, sometimes into the pharynx. The socket begins to close insufficiently. Such disturbances in the functioning of the cardia can affect the lower esophageal sphincter or both sphincters simultaneously. Sometimes non-closure (when the sphincter does not close completely) and pressure provoke vomiting and nausea.
- With the 3rd degree of insufficiency, a gaping sphincter is formed.
Symptoms
Changes in the functioning of the sphincters affect the functioning of the organ, which causes the appearance of various symptoms - odor from the mouth, pain in the esophagus, dysphagia.
- Odor from the mouth. Changes in the diameter of the esophageal sphincters provoke the appearance of such a symptom. This is due to a number of pathogenetic reasons, including the accumulation of food particles and gastric contents in the esophagus. If the upper and lower esophageal sphincter do not function correctly, the ingress of gastric contents can cause inflammation of the membranes, the formation of erosions, and various infections.
- Painful sensations. Pain can appear due to various disorders of the sphincters. Sometimes pain develops when swallowing; at rest, such sensations may be absent. The development of the symptom is triggered by irritation and damage to the membrane due to the regular ingestion of gastric contents.
- Swallowing dysfunction. Dysphagia is considered the most common symptom of cardia failure. In most cases, it occurs when swallowing solid food particles. Drinks and dishes that have a liquid consistency do not cause discomfort when swallowed.
Return to contents
Diagnosis methods
The main goal of diagnosis is not only to confirm or refute cardiac spasm, but also to exclude the presence of cancer in the stomach.
As a rule, laboratory tests do not provide any information at all, which is why they are used to determine concomitant pathology.
To determine how the upper and lower esophageal sphincters work, first of all, X-ray examination is used. Diagnosis is carried out with a barium element, which is injected into the stomach on an empty stomach to determine whether the lower valve is closed, which is typical for this type of pathology. The shape of the esophagus may take on something similar to a "bird's beak". The lower esophageal sphincter is usually unchanged in size, and fluid accumulation can be seen above it. At an advanced stage, the esophagus takes on an S-shape.
To clarify the diagnosis of esophageal achalasia and identify the degree of damage to the mucous membrane, and to refute or confirm cancer, esophagoscopy is used. This study is also a preparatory stage in preparation for surgery.
Manometry is designed to assess the degree of contractile activity and the development of achalasia of the cardia, the work of peristalsis.
Methods for strengthening the lower valve
As a rule, patients are offered all treatment methods. In our country, alternative methods of strengthening the sphincter are not widely used, although world practice proves their high effectiveness.
There are breathing exercises for gastric cardia insufficiency that allow you to get rid of symptoms in the first stages of achalasia. Therapeutic exercises must be carried out on an empty stomach, using abdominal and chest breathing.
Restoration of the sphincter can be carried out with the help of physical therapy. Treatment is best carried out against the background of conservative therapy, even in the acute period. Electrophoresis and DDT are usually used. Naturally, it won’t work directly on the valve, but the phrenic nerve is stimulated with current. The procedures are carried out about 10 times, every other day.
The electrophoresis method is similar, but medications are applied to the cuff with electrodes. The therapy allows for improved blood supply and healing occurs much faster. Some patients note a slight decrease in pain.
Forecast
If the disease is at stage 1, then the prognosis is quite favorable. Especially if the patient strictly follows the doctor’s recommendations. Physiotherapy and breathing exercises will help restore the sphincter.
The second and third stages are no longer the best prognosis for the patient’s recovery. Most often it is not possible to do without surgical intervention. Patients at this stage after treatment will have to be regularly examined to avoid exacerbations.
If left untreated, esophageal achalasia leads to carcinoma in approximately 5% of cases, and aspiration pneumonia occurs in 10% of cases. Patients will have to give up irregular meals and heavy physical work.
Food must move forward through the gastrointestinal tract. When casting, irritation of the membranes and inflammatory processes are possible, which can lead to complications and other unpleasant consequences. Advanced inflammation can provoke the development of malignant tumors, ulcers and erosions.