Features of manifestations of dysbacteriosis
Toxic elements released by bacteria seep into the circulatory system. Cellular and humoral immunity is activated. Antibodies released by the immune system eliminate toxic elements. But in large quantities they continue to circulate in the blood.
IgE immunoglobulins are the main type of antibodies that act as protection against toxic elements. They react to any foreign body that appears in the blood and cause skin rashes. In such a situation, it is difficult to identify the factor that provoked the syndrome of bacterial overgrowth in the intestines.
Clinical picture:
Tingling and itching are rare symptoms of an allergic reaction. If the microflora in the intestines is disrupted, disorders of the gastrointestinal tract may not appear. For such purposes, accurate diagnostics will be required.
Symptoms of allergies due to dysbacteriosis are:
- Swelling of the nasal mucosa.
- The patient feels pain in the eye area.
- The whites of the eyes become red.
- Whistling breathing occurs, the patient has difficulty taking a breath, and an asthmatic spasm appears.
- Loss of hearing, pain in the ear canals.
- A rash, irritation, and small red spots appear on the skin.
- Rarely has a headache.
In adult patients, anaphylaxis may occur.
Rash due to dysbacteriosis - etiology
Skin rashes due to dysbacteriosis are quite easy to explain. Changes in the composition of the gastrointestinal tract microflora lead to hyperimmunization and allergization of the patient, which leads to the appearance of a rash and other manifestations. Remember, almost everyone who has experienced an allergy to flowers or anything else has suffered from rashes and other skin manifestations. Rash due to dysbacteriosis in children is explained by the same reason.
Video: Doctor Komarovsky about dysbiosis
In general, a rash due to dysbacteriosis in infants may appear due to the presence of an allergic agent in the lumen of the gastrointestinal tract. Most often, young patients suffer from hives, spots, rashes of various locations (limbs, face, back, abdomen, chest).
Etiological causes of rash due to dysbacteriosis
Dysbacteriosis in children, rashes, can have different etiological causes that can lead to a similar manifestation of pathology:
- Constant use of antibacterial agents without a systemic treatment regimen,
- Previous infections of the gastrointestinal tract or other complicated infectious processes,
- Dysbacteriosis complicated by pancreatitis, gastritis, ulcers or gallbladder pathology,
- Violation of the diet - abuse of flour, spicy and fatty foods. Often, the lack of fermented milk products and vegetables and fruits in the diet can lead to dysbacteriosis, a rash on the face,
- Pathologies of the immune system or its individual elements,
For any manifestations of rash due to dysbacteriosis in an infant, complex diagnostic measures and treatment are required. Remember that self-treatment, especially with the use of highly active pharmacological agents, is unacceptable.
The similarity of allergies with rashes from dysbacteriosis
Sometimes dysbiosis and its consequences as a rash on the body can be of a similar nature to an allergy to new foods or ordinary irritation. If such a manifestation disappears within a few days, then there is no need to sound the alarm. Otherwise, you should consult a pediatrician. In any case, dysbiosis and rashes on the face are not an independent disease. That is why it is necessary to look for the real cause of skin rashes, but not to treat them without examination. Such a stupid approach can only lead to the transition of dysbiosis to the chronic stage, which will then lead to delayed growth and development, as well as severe disorders of the gastrointestinal tract.
Is intestinal dysbiosis the cause of allergic diseases?
Allergy due to dysbacteriosis in a small child is closely related to a violation of the intestinal microflora. Dermatitis and rashes in a child have something in common with dysbacteriosis. Rash in newborns occurs as a result of an immune barrier to allergens.
The mucous membrane of the digestive organs takes the brunt of the attack. Negative changes occur in the absorption of food and local mucosal immunity, toxins seep into the child’s blood. The result is a persistent reaction of the body that turns into an allergy.
Conclusion - intestinal dysbiosis can be a cause of allergic diseases. Often, for the purpose of therapy to eliminate reactions, the doctor prescribes drugs that normalize the intestinal microflora.
Dysbacteriosis
The human body is populated by a huge number of microorganisms. Some of them (normoflora) contribute to the normal functioning of organs and tissues. Others (pathogenic microflora) produce toxins and cause various diseases.
The microflora of the oral cavity consists of streptococci, enterococci, lactic acid bacteria, etc. It varies depending on the condition of the gums, teeth, tonsils and nasopharynx. In the stomach of a healthy person, microorganisms are usually absent due to the antimicrobial properties of gastric juice. The contents of the small intestine are either sterile or contain a small number of microbes. The abundant microflora of the colon of a healthy person consists of 90% bifidobacteria. There are also E. coli, streptococcus, lactobacilli, etc.
The microbial flora of the gastrointestinal tract has important physiological significance. She takes part:
- in the digestion of food by the intestines;
- synthesis of vitamins (in particular, vitamin K, necessary for the formation of prothrombin in the blood);
- in the synthesis of enzymes necessary for the full function of the gastrointestinal tract;
- in the production of various organic acids (acetic, butyric) involved in metabolic processes, redox reactions;
- in stimulating the body’s immune system, providing local protection against the colonization of pathogenic microorganisms.
Violation of the quantitative and qualitative composition of normal microflora is referred to as dysbacteriosis. Dysbacteriosis is not one local disease, but the foundation on which many seemingly independent serious diseases arise.
There are three degrees of dysbiosis:
I degree - a significant decrease in the number of normal microorganisms in their natural habitats;
II degree - the disappearance of some symbionts (normal intestinal microorganisms) and the increase of others with altered properties (hemolytic, lactose-negative and weakly enzymatic Escherichia), the appearance of bacterial flora in the small intestine.
III degree - against the background of a pronounced disruption of the normal composition of the microflora, pathogenic strains of bacteria (Proteus, staphylococci, clostridia), as well as fungi, appear.
Symptoms of dysbiosis:
- gastrointestinal dyspepsia (abdominal pain, flatulence, diarrhea or constipation, and sometimes their alternations, belching, heartburn, nausea, rumbling in the stomach, bloating, unpleasant taste in the mouth);
- allergic reactions characteristic of those suffering from dysbacteriosis (urticaria, skin itching, diathesis in children, food allergies);
- syndrome of malabsorption in the intestine, leading to a lack of vitamins (especially group B, D, E, K), folic acid, proteins, microelements, carbohydrates and expressed by decreased appetite, sleep disturbances, and in severe cases, weight loss, anemia.
The causes of dysbiosis are:
- irrational use of antibacterial drugs, leading to the death of a significant part of the normal microflora;
- starvation, malnutrition;
- long-term retention of feces in the large intestine;
- diseases occurring with intestinal damage, intestinal infections (such as dysentery, salmonellosis, viral lesions, helminthic infestations);
- chronic diseases and dysfunctions of the digestive organs (chronic gastritis, peptic ulcer, cholecystitis, pancreatitis, liver disease);
- decreased general and local immunity (due to stress, unfavorable environmental factors);
- severe injuries, extensive operations, radiation and chemotherapy for cancer patients.
Treatment of dysbiosis is mandatory even at the mildest stage I, since even minor changes in the normal composition of the microflora significantly disrupt the processes of absorption of nutrients by the body, change enzymatic reactions, sharply reduce the synthesis of vitamins, etc.
An effective means of correcting mild disorders of the gastrointestinal microflora is the biological product Floranorm , which supplies the body with a complex of bifidobacteria and lactobacilli, and also provides them with a nutrient medium and protection. Pectin and lactulose in the product help retain bacteria in the intestinal lumen, giving them the opportunity to move from a dormant state to an active physiological phase.
Floranorm helps restore normal intestinal microflora, is indicated for frequently ill weakened patients, before surgery, under stressful conditions and exposure to aggressive environmental factors (radiation, chemicals and toxic substances), for constipation, diabetes, to relieve alcohol intoxication. Doses and duration of treatment are individual. For preventive purposes, take Floranorm 1 sachet 1 time per day before meals (14 days), for therapeutic purposes, 2-3 sachets per day.
For intestinal dysbiosis caused by the presence of opportunistic microflora, brown seaweed gel due to the antibacterial properties of sodium alginate, the specific gravity of which is 35% among the gel components. It is important to note that the most sensitive were: staphylococci, hemolytic streptococcus, Proteus and their associations. we recommend brown seaweed gel twice a year as a therapeutic and prophylactic nutrition.
For more severe degrees of dysbiosis, antibiotics are traditionally used to suppress pathogenic microorganisms, which creates a number of complex problems. Firstly, due to the predominance in the body of a patient with dysbiosis of microbes that are resistant to a number of antibiotics, it is necessary to use the most aggressive and toxic of them. Secondly, along with pathogenic microflora, antibiotics also destroy normal flora, thus disrupting the physiological functions of the gastrointestinal tract. Finally, antibiotics have powerful side effects, dramatically weakening the immune system, having a toxic effect on the body's systems and organs, and causing a variety of allergic reactions.
As an antibiotic for suppressing pathogenic microflora, the Shuang Huang Lian Extract . This broad-spectrum antiviral, antibacterial and antifungal agent has virtually no contraindications, side effects or age restrictions. Doses are selected individually depending on the severity of dysbiosis and the age of the patient: from 5 to 10 ml 3 times a day. Treatment is long-term, no less (14 – 30 days).
Elixir “Quing Regida” (Liquid for heat and poison) 10 ml once a day at night for 10–14 days
To normalize impaired digestion and absorption processes, as well as eliminate hypo- or avitaminosis and deficiency of micro- and macroelements, it is recommended to use “Tsar Vitamin” , Royal Jelly with Ginseng and “Laojan” Decoction .
Thus, in relation to dysbiosis, the well-known statement that it is easier to prevent a disease than to treat it later is especially relevant.
All these natural preparations of the Greenhelp Program are general strengthening, restorative and immunomodulatory agents, suitable even for pregnant women and children from the neonatal period.
Diagnosis of allergic dysbiosis
Diagnosis is carried out in the following stages:
If it is not possible to determine the reaction factor, a general stool analysis will be required. It will help indicate the number of beneficial bacteria in the stomach.
- A general blood test will determine the presence of a toxin in the bloodstream that causes rash and swelling.
- A one-time use of drugs that block histamine receptors will help determine the presence of allergenic factors after a few hours. If the relationship between the two diseases is confirmed, complex treatment is prescribed.
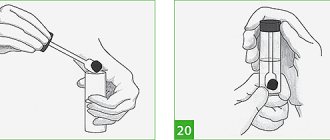
- A genetic test (PCR) will help identify bacterial activity and highlight allergenic toxicity. Fast and accurate method.
- The scratch test is determined by introducing the allergen into the thickness of the skin of the forearm or back using an intradermal injection. The result in the presence of allergies is local redness of the skin or the appearance of hives after 30 minutes. Economical, simple, optimal way to perform diagnostics. Has complications: hypersensitivity to the injected substance, develops 6 hours after administration, duration of exposure to the element is 24 hours; the emergence of a new type of allergic reaction as a consequence.
- Determination of the total and specific IgE levels contained in the patient’s serum. It is carried out thanks to colorimetric and radiometric analysis.
Diagnostic methods are determined by the doctor based on the etiology of the disease.
Therapy methods
Allergies due to severe dysbiosis require the following medications:
- Solution for injections "Adrenaline".
- Antihistamines.
- "Sodium cromoglycate."
The substances reduce the manifestation of allergy symptoms and disruption of digestive functions due to pathologies of microflora in the intestines in adult patients. But you should not use it for a long period. In case of anaphylaxis, use as an “ambulance”.
Rashes due to microflora disorders are treated with “Histamine”, increasing the dose.
To avoid chronic pathologies, the following measures will be required:
- Follow the diet prescribed by a nutritionist.
- Take probiotics or prebiotics (Linex, Hilak Forte, Baktisubtil).
Take medications under the supervision of a doctor.
Therapy for dysbiosis and allergies in infants is determined by a specialist. You can avoid a negative reaction by adhering to the following points:
- Determine the appropriate diet for the mother if she is breastfeeding.
- Eliminate potential external allergens.
- Temporarily stop bathing your baby in herbal baths.
- Apply external effects on the skin using Bepanten cream, and eliminate internal infections with Smecta powder. Give plenty of fluids throughout the day.
- Beneficial bacteria for the baby's intestines come from breast milk. They fight pathogenic microorganisms, providing lasting immunity. When artificial feeding, give preference to adapted formulas.
- Mom shouldn't worry about anything. Stress is passed on to the child. If the baby’s behavior is normal, you should not run to the doctor the first time the baby cries.
- Maintain room temperature at +18-19°C. At this temperature, the skin is able to breathe, the child sweats less.
- Provide natural humidity in the room using damp towels or a humidifier.
According to mothers, good products for bathing children are “Oilatum” and “A-derma”.
For preventive purposes, mother and child can take the drug “Likopid”. Use probiotics during lactation.
GUT MICROECOLOGY AND ALLERGY
The problem of intestinal dysbiosis is today the subject of a lively discussion among gastroenterologists and pediatricians. The reasons for this lie in the absolute importance of the state of the intestinal microflora, the elevation of the concept of “dysbacteriosis” to the rank of a nosological form or “clinical and laboratory syndrome”. In practice, this interferes with the correct understanding of the pathological process, timely diagnosis and selection of an adequate method of therapy.
In healthy individuals, there are about 500 species of various microorganisms in the intestines, most of which are representatives of the so-called obligate microflora (bifidobacteria, lactobacilli, non-pathogenic Escherichia coli, etc.)
Normal microflora is a qualitative and quantitative ratio of various microbes of individual organs and systems, thanks to which the biochemical, metabolic and immune balance of the macroorganism is maintained, which is necessary to maintain human health. That is, intestinal microflora is an important factor contributing to the normal development and functioning of the child’s body.
The intestinal microflora consists of 92-95% obligate anaerobes. The composition of the intestinal microflora is quite individual and is formed in the first days of a child’s life. The most important factor in the formation of normal microflora are the following criteria.
Before and during childbirth:
- genetic;
- mother's microflora;
- microflora of medical personnel;
- hospital microflora;
- medicines.
After birth:
- composition of breast milk;
- composition of the artificial mixture;
- pro- and prebiotics of food.
Natural feeding is extremely important for a young child, since human milk contains a number of prebiotic substances that contribute to the colonization of the intestines by certain types of microorganisms in certain quantities. Even minor troubles in the first days of a child’s life, and especially pathological conditions of the gastrointestinal tract, can cause severe disturbances of the intestinal biocenosis that are difficult to correct in the future. Irrational antibiotic therapy can cause particular damage to the intestinal microflora during this period.
Some of the most important representatives of the intestinal microbiocenosis and their functions are presented in the table.
Disturbance of microbial balance in the intestine is called dysbiosis or intestinal dysbiosis. According to the industry standard, which is soon to be adopted, intestinal dysbiosis is understood as a clinical and laboratory syndrome that occurs in a number of diseases and clinical situations and is characterized by:
- symptoms of intestinal damage;
- changes in the qualitative and/or quantitative composition of normal microflora;
- translocation of various types of microflora into unusual biotopes;
- excessive growth of microflora.
However, most practicing gastroenterologists do not agree with this formulation, since symptoms of intestinal damage do not arise from dysbiosis, but from a specific disease, the consequence of which is often a violation of the intestinal microecology.
The main causes of intestinal dysbiosis:
- late breastfeeding;
- poor nutrition of the child (especially in the first months of life);
- functional disorders of the gastrointestinal tract;
- diseases of the gastrointestinal tract, especially those associated with malabsorption syndrome (lactase deficiency, celiac disease, cystic fibrosis, etc.);
- antibiotic therapy (especially in the first days of a child’s life);
- Features of the immune system.
Intestinal dysbiosis is always a secondary condition. The root cause of its development is a change in the internal environment of the intestine, disruption of digestive processes, a damaging effect on the intestinal wall, and malabsorption. Intestinal dysbiosis closes a “pathogenetic vicious circle”, which must be broken both for the successful treatment of the underlying disease and for eliminating its consequences. Below is the classification of intestinal dysbiosis proposed in 1991. However, based on the position of the secondary nature of dysbacteriosis and the absence of any specific clinical picture, this classification, in the opinion of the author, is of purely historical interest.
Today, the following methods for diagnosing intestinal dysbiosis are proposed:
- bacteriological analysis (determination of the composition of fecal microflora, reflecting the microbial composition of only the distal parts of the intestine - the most accessible method, but not sufficiently accurate);
- biochemical rapid method for determining the proteolytic activity of fecal supernatants;
- high-voltage electrophoresis on paper to detect b-aspartylglycine, b-aspartyllysine, b-alanine, 5-aminovaleric and g-aminobutyric acids, etc.;
- ion chromatography (determination of biogenic amines, bile and carboxylic acids, aromatic compounds);
- gas-liquid chromatography (detection of volatile fatty acids in feces - acetic, valeric, nylon, isobutyric, etc.);
- the study of microflora in a biopsy of the jejunum obtained during an endoscopic examination is the most accurate method, which, however, due to technical difficulties cannot be used widely enough.
Unfortunately, we have to admit that traditional clinical ideas about intestinal microflora are outdated. And primarily due to incomplete information about the microbiocenosis:
- out of 500 species of microbes inhabiting the intestines, only 10-15 fecal microbes are analyzed;
- mucosal and small intestinal microbial flora are not taken into account;
- difficulties in interpreting the results (wide fluctuations and rapid variability in the composition of the microbial flora of the colon).
Correction of microecological disorders is based on the following principles:
- treatment of the underlying disease;
- correction of dysbiotic disorders;
- correction of complications.
For this purpose, a targeted impact on the microflora is carried out with selective destruction (antibiotics, bacteriophages) of unwanted microorganisms and colonization of the intestine with missing representatives of the flora, as well as a general impact on the microflora in order to create conditions in the intestine that would be unfavorable for unwanted microorganisms, but conducive to colonization missing.
To normalize the intestinal microflora, various groups of drugs are used, including probiotics - live microorganisms and substances of microbial origin, which, when administered naturally, have positive effects on physiological and metabolic functions.
Primadophilus preparations contain a wide range of strains of highly implantable microorganisms: primadophilus (Lactobacillus rhamnosus and Lactobacillus acidophilus), primadophilus bifidus (Lactobacillus rhamnosus, Lactobacillus acidophilus, Bifidobacterium breve, Bifidobacterium longum), primadophilus children (Lactobacillus rhamnosus, Lactobacillus acidophilus, Bi fidobacterium infantis, Bifidobacterium longum), primadophilus junior (Lactobacillus rhamnosus, Lactobacillus acidophilus, Bifidobacterium breve, Bifidobacterium infantis, Bifidobacterium longum).
Linex, a three-component complex of live lyophilized bacteria that acts throughout the intestine, is promising for the treatment of dysbiosis.
Nevertheless, it is necessary to note the imperfection of traditional treatment of dysbiosis, associated with the shortcomings of antibacterial therapy (suppression of microbiocenosis, growth of resistant forms), phage therapy (narrow specificity of phages, rapid emergence of phage-resistant strains) and probiotic therapy (difficulty in selecting and inadequacy of drug doses for the purposes of their use, limited the possibility of implanting individual strains into already established intestinal ecosystems, the instability of their colonization, limited antagonistic activity of the strains used, a narrow spectrum of dysbiotic correction).
In this regard, the use of prebiotics, metabolic products of normal microorganisms, has recently been shown to be promising. Drugs in this group include Hilak Forte, which is a sterile concentrate of metabolic products produced by the normal flora of the small and large intestines. Hilak forte helps restore the biological environment in the intestine, creating conditions for the growth and restoration of all types of its own microflora, and improves the physiological functions and reparative processes in the mucous membrane of the gastrointestinal tract. It should be noted that Hilak Forte is used at all stages of treatment, is compatible with other drugs and can be used at any age without restrictions.
Recently, a domestically produced combined prebiotic, Lactofiltrum, appeared on the Russian market, containing an enterosorbent based on hydrolytic lignin (a wood processing product), which absorbs toxins and pathogenic microflora in the intestines, and also contains lactulose, a powerful stimulator of the growth of bifidobacteria and lactobacilli.
In addition, prebiotics are added to the Nutrilon Omneo infant formula.
Since the 80s, the importance of gastrointestinal microbiocinosis disorders in the pathogenesis of atopic diseases has been widely debated. Until recently, a generally accepted, although not sufficiently proven, theory was the influence of infectious agents on the mechanisms of development of atopic diseases. This scheme generally suited both doctors and pathophysiologists. However, at the end of the twentieth century, an increase in the number of atopic diseases was recorded in economically developed countries. The allergy epidemic began in the generation of people born after the 60s. Most often, this trend is associated with the Western lifestyle, which implies a decrease in the frequency of viral and bacterial infections, which to a certain extent contradicted traditional ideas about the role of infection in the genesis of atopy. The so-called “hygienic” hypothesis was formulated. This model, the validity of which has been confirmed by a number of studies, has radically changed views on the possibility of using probiotics in allergic diseases. It has been suggested that the beneficial role of infection in curbing the development of allergies may be replaced by the use of probiotics. Several pathways through which probiotics modulate allergic inflammation have now been identified.
- Changing the immunogenicity of allergens by proteolysis. Probiotic proteases destroy cow's milk casein, thereby changing the immunogenic properties of the protein. I would like to emphasize the fact that casein enhances the production of IL4 and g-interferon in children sensitized to cow's milk, while casein split by Lactobacillus GG reduces the production of IL4 and does not affect the release of g-interferon. This finding indicates the ability of probiotics to inhibit IgE synthesis and eosinophil activation.
- Reduced secretion of inflammatory mediators in the intestine, for example after administration of Lactobacillus rhamnosus GG (ATCC 53103), in turn reduces the level of tumor necrosis factor-a in the feces of patients suffering from atopic dermatitis and cow's milk allergy.
- Reducing increased intestinal permeability.
- Targeting the antigen to Peyer's patches, in which interferon promotes antigen uptake and in which IgA-producing cells are generated. It is likely that lactobacilli, which increase the synthesis of interferon, contribute to this process.
It should be noted that postnatal maturation of the mucosal IgA system usually occurs much faster in developing than in industrialized countries. This is probably due to insufficient microbial stimulation in the latter. At the same time, an increase in systemic and secretory IgA is indicated with oral administration of lactobacilli. Supplementation with Lactobacillus casei and Lactobacillus bulgaricus leads to a decrease in increased phagocytic activity in children with food allergies, whereas in non-allergic individuals, probiotics increase phagocytic activity. That is, probiotics modulate phagocytosis activity differently in allergic and non-allergic patients. This means that the immunomodulatory effect of probiotics may depend on the initial immunological status of the patient. Unfortunately, there are no clinical studies conducted taking this position into account. There are also no controlled studies establishing differentiated indications for the use of certain strains of probiotics in children with atopic diseases. Certain strains of gastrointestinal flora can release low molecular weight peptides that modulate the immune response. Thus, probiotics suppress the proliferation of lymphocytes and the production of cytokines by T cells.
Russian scientists pointed out the connection between food allergies and intestinal flora disorders in the early 1980s. A striking example of the relationship between intestinal microbiocinosis and the prevalence of atopic diseases is the situation that has developed in two neighboring countries. Thus, in Sweden, the intestinal microflora of children contains a significant amount of Clostridium sp., while a similar population in Estonia is characterized by a high level of Lactobacillus sp. and Eubacterium sp. Perhaps these microbiotic features explain the low level of allergic diseases in Estonia compared to Sweden. Moreover, a study conducted at the end
90s, showed that the intestinal microflora in children in Estonia is similar to that which was identified in children in Sweden in the 60s. It must be emphasized that healthy Estonian children have higher levels of lactobacilli compared to those with allergies.
A reduction in the risk of developing atopic eczema during the first two years of life was shown in children whose mothers received probiotics compared to the placebo group. The amount of transforming growth factor b 2, which has anti-inflammatory properties, increased in breast milk. In Finland, pregnant women whose children were at high risk of developing atopic eczema received lactobacilli daily 2–4 weeks before expected delivery. In the experimental group, 36 children were bottle-fed and received lactobacilli per os during the first 6 months of life, while 28 breastfed children received lactobacilli only prenatally. Atopic eczema was diagnosed at 12 months in 15/64 (23%) treated children and in 31/68 (46%) in the placebo group. Thus, it can be argued that Lactobacillus GG effectively prevents early manifestations of allergies in children at risk. At the same time, the level of total and specific IgE, as well as skin tests, did not differ between children in the experimental and placebo groups. That is, the decrease in the frequency of atopic eczema can hardly be explained on the basis of the ratios, as well as the predominance of TH1/TH2 types of immune response.
Speaking about the treatment of atopic diseases with probiotics, it is necessary to note the priority of Russian research in this area. It has been shown that the introduction of a mixture of Propionibacteria and Lactobacillus acidophilus leads to a decrease in the manifestations of food allergies. However, these and many other studies were not controlled.
In the first gold standard study demonstrating the effectiveness of probiotics for allergic diseases, infants with a proven cow's milk allergy were fed a highly hydrolyzed formula or a highly hydrolyzed formula with Lactobacillus rhamnosus GG (ATCC 53103). In another study, 27 4.6-month-old infants with food allergy symptoms while exclusively breastfed were given a highly hydrolyzed formula or a highly hydrolyzed formula with the probiotics Bifidobacterium lactis Bb-12 or Lactobacillus GG (ATCC 53103). After two months, children showed significant improvement in skin condition, as assessed by SCORAD, in children receiving both Bifidobacterium lactis Bb-12 and Lactobacillus GG compared to the control group.
Thus, reliable clinical data confirming the effectiveness of probiotics in the prevention and treatment of atopic diseases in children is clearly insufficient. At the same time, experimental data and single clinical studies confirm the need for further research that would allow us to determine doses, administration regimens and indications for the use of probiotics.
Literature
- Bondarenko V. M., Uchaikin V. F., Murashova A. O., Abramov N. A. Dysbiosis. Modern possibilities of prevention and treatment. M., 1995.
- Dorofeychuk V. G., Lekomtseva G. A. Intestinal dysbiosis in children during the newborn period and its consequences // Pediatrics. 1982. No. 1. P. 72-74.
- Korshunov V. M., Ivanova N. P., Kafarskaya L. I., Gladko I. A., Efimov B. A., Smeyanov V. V. Normal intestinal microflora, dysbiosis and their treatment: Methodological developments. M., 1994.
- Krasnogolovets V. N. Intestinal dysbiosis. M., 1989.
- Kuvaeva I. B., Ladodo K. S. Microecological and immune disorders in children. M., 1991.
- Pinegin B.V., Maltsev V.N., Korshunov V.M. Intestinal dysbiosis. M., 1984.
A. I. Khavkin, Doctor of Medical Sciences, Professor of the Research Institute of Pediatrics and Pediatric Surgery of the Ministry of Health of the Russian Federation, Moscow
Linex is a promising drug in the treatment of dysbiosis
Properties of Linex that ensure its leading role in the correction of dysbiosis:
- Natural origin. Linex is a three-component complex of live lyophilized bacteria (Bifidobacterium infantis v. Liberorum, Lactobacillus acidophilius, Streptococcus faecium), acting throughout the intestine and not normally present in the intestinal microflora.
- Physiological normalization of intestinal microflora in patients with acute intestinal infections and dysbiosis: once living bacteria enter the intestine, they settle throughout its entire length, performing all the functions of normal intestinal microflora - antimicrobial, digestive, vitamin-forming.
- Prolonged action due to the constant production of the most important substances of the natural intestinal microflora.
- A three-component composition of bacteria with a synergistic effect and antagonistic activity against pathogenic and opportunistic microorganisms and enzymatic activity.
- High degree of resistance to antibiotics, allowing the drug to be prescribed simultaneously with antibiotics and chemotherapy drugs.
- Complete safety - possibility of administration to patients of all age groups.
Classification of intestinal dysbiosis according to I. B. Kuvaeva, K. S. Ladodo (1991)
The first degree - the latent phase of dysbiosis, manifests itself only in a decrease by 1-2 orders of magnitude in the amount of protective microflora - bifidobacteria, lactobacilli, as well as full-fledged E. coli - up to 80% of the total amount. The remaining indicators correspond to the physiological norm (eubiosis). As a rule, the initial phase does not cause intestinal dysfunction and occurs as a reaction of the body of a practically healthy person to the influence of unfavorable factors, such as, for example, poor diet, etc. In this phase, vegetation in the intestine is possible for a small number of individual representatives of opportunistic flora.
There are no clinical manifestations of dysbacteriosis in this phase.
The second degree is the starting phase of more serious disorders, characterized by a pronounced deficiency of bifidobacteria against the background of a normal or reduced number of lactobacilli or their reduced acid-forming activity, an imbalance in the quantity and quality of E. coli, among which the proportion of lactose-negative or citrate-assimilating variants is increasing. At the same time, against the background of a deficiency of protective components of the intestinal microbiocenosis, the proliferation of either plasma-coagulating staphylococci, or Proteus, or fungi of the genus Candida occurs. Vegetation in the intestines of Proteus or plasma-coagulating staphylococci at this phase of the development of dysbacteriosis is often transient rather than permanent.
Functional digestive disorders are not clearly expressed - sporadically loose stools of greenish color with an unpleasant odor, with a shift in pH to the alkaline side, sometimes, on the contrary, stool retention, and sometimes nausea may be noted.
The third degree - the phase of aggression of the aerobic flora - is characterized by a clear increase in the content of aggressive microorganisms; at the same time, Staphylococcus aureus and Proteus, hemolytic enterococci multiply (up to tens of millions in association); replacement of full-fledged Escherichia with bacteria of the genera Klebsiella, Enterobacter, Citrobacter, etc. is observed.
This phase of dysbiosis is manifested by intestinal dysfunction with disorders of motility, enzyme secretion and absorption. Patients experience frequent, loose stools, often green, decreased appetite, deterioration in health, children become lethargic and moody.
The fourth degree - the phase of associative dysbiosis - is characterized by a deep imbalance of the intestinal microbiocenosis with a change in the quantitative ratios of the main groups of microorganisms, a change in their biological properties, and the accumulation of toxic metabolites. Vegetation of enteropathogenic serotypes of E. coli, Salmonella, Shigella and other pathogens of acute intestinal infections is characteristic. Clostridia may multiply.
This phase of dysbiosis is characterized by functional disorders of the digestive system and disturbances in general nutritional status, body weight deficiency, pale skin, decreased appetite, frequent stools mixed with mucus, greens, and sometimes blood, with a sharp putrid or sour odor.
Possible complications
With a systematic allergic response, an adult patient develops anaphylaxis, which provokes complications:
- decreased blood pressure;
- swelling;
- severe skin rashes;
- bronchospasm;
- to whom.
Sometimes the disease can lead to death.
Dysbacteriosis is dangerous if the child is allergic. Excessive synthesis of toxins leads to a constant response from the body. Children may experience digestive system disorders related to intestinal flora. The baby may develop:
- diseases of the rectum;
- allergy status to certain foods, other antigenic forms.
Rashes in a child
The intestinal microflora in young children is still in the formative stage, so children are at risk for the development of dysbacteriosis. With this pathology, the number of beneficial lactobacilli and bifidobacteria in the intestines is reduced, against the background of which opportunistic and pathogenic pathogens are activated. With dysbacteriosis, a baby may develop rashes on the skin in the first days of life.
Causes
The risk of dysbacteriosis in children, which may be accompanied by skin rashes, increases with:
- Refusal to breastfeed.
- Early transition to artificial formulas.
- The mother is taking hormonal or antibacterial medications.
- Treating a child with antibiotics.
- Insufficient synthesis of digestive enzymes (may be normal or pathological).
- Physiological immaturity.
- Development of a variety of diseases.
- Injuries that occurred during birth.
- Infectious diseases in the mother, mastitis, etc.
Sometimes the cause of dysbiosis and rashes in infants is a combination of several factors.
A rash can appear for completely different reasons that have nothing to do with the composition of the intestinal microflora. An experienced doctor can make an accurate diagnosis.
Symptoms
The rash that appears against the background of dysbacteriosis has the appearance of allergic rashes. Doctors associate its appearance with an increase in sensitization of the body. Visually, the rash may look like:
- Areas of redness on the skin.
- Small red rash.
- Peeling.
- Red spots merging with each other.
- Weeping areas, etc.
In parallel, dysbiosis also manifests itself in other health disorders associated with the functioning of the gastrointestinal tract:
- Pain in the stomach and intestines (the child becomes restless).
- An audible rumbling in the stomach.
- Frequent and loose stools.
- Constipation.
- Insufficient weight gain.
- Flatulence (intense colic).
Quite often, parents and even doctors mistake a rash due to dysbacteriosis for an allergy and begin to treat it without the expected success. Without correcting the normal composition of the intestinal microflora, the child’s well-being will suffer for a long time.
Is it itching?
Rashes on a child’s skin due to dysbacteriosis may well be accompanied by obsessive itching sensations, since the mechanism of their development is clearly related to the release of histamine (typical of allergies). And allergic rashes, as you know, can itch. Therefore, babies can become doubly restless, sleep poorly and even scratch their skin a lot. This possibility must be taken into account during treatment - it is very important to protect the baby from scratching and prevent secondary infection.
Allergies and intestines
From the first days of life (and before that, in utero), the intestine influences the formation of the immune response.
The formation of protective mechanisms and their activity in the future depends on how stable and balanced the composition of the microflora that begins to inhabit the sterile surface of the mucous membrane of the digestive tract of a newborn is.
Thus, the prerequisites for the occurrence of disorders in the immune system appear in early childhood. The immature body of a small child is forced to adapt to new, sometimes hostile conditions. Initially, protection received from the mother helps cope with threats (antibodies, or special protein complexes, are transmitted through the placenta and breast milk). However, it only lasts for a few months - after this period, the child needs to have his own, albeit imperfect, immunity.
The gastrointestinal tract is a physiological barrier to antigens, that is, substances foreign to the body. It traps hundreds and thousands of pathogens every day - such as:
The microbial flora that populates the intestines is actively involved in maintaining local (local) and general (systemic) immunity. It interacts with the cells of lymphoid tissue (a physiological structure that performs a protective function) - this is what researchers see as the basis for the relationship between the allergy and intestines system. If the flora is normal and includes predominantly the “correct” types of microorganisms (bifidobacteria and lactobacilli, etc.), the immune system reacts only to the necessary antigens - for example, infectious agents. And the mechanism for the formation of tolerance, that is, immunity to proteins supplied with food, works smoothly and accurately.
At the same time, allergy as a pathologically exacerbated sensitivity to antigens of food, animal hair and saliva, cosmetics, household dust and other environments can be associated with a change in the ratio of beneficial and opportunistic flora, or dysbacteriosis. The last group always lives in the intestines, but if the “right” microbes predominate, it does not pose a danger. However, in certain circumstances, there is a sharp increase in colonies of unfavorable microorganisms; it is no longer possible to suppress their growth, which affects the processes of digestion and immune defense.
How to explain a rash on the face due to dysbacteriosis?
We all know very well that the gastrointestinal tract is filled with bacteria that form a beneficial symbiosis with our body. Microorganisms play an important role in the process of our life - they secrete a number of vitamins, activate peristalsis, etc.
At the slightest disturbance, the balance between “beneficial and harmful” bacteria collapses, which leads to an atypical number of certain bacteria. Opportunistic and pathogenic microorganisms are capable of releasing a number of toxins and enzymes that are absorbed into our bloodstream, which leads to allergization of the body.
It is for this reason that rashes appear on the skin of a child due to dysbacteriosis. Among other things, chronic intoxication with toxins and products of metabolic activity of bacteria can lead to general disorders in organs and systems.
Intestinal dysbiosis, possibly a rash, begins with increased functioning of the sweat and sebaceous glands, which secrete their secretions onto the surface of the skin. At the initial stages, slight darkening, oiliness, and an inconspicuous rash appear on it, and later an unpleasant odor appears in the sweat secretions.
Most often, pathological rashes appear on the skin of the hands and face. This distribution is explained by the thickness of the skin - in these areas it is thinnest, which leads to its rapid inflammation and rash. Often this manifestation is accompanied by infection, which leads to the appearance of hives and other spots.
Why do intestinal allergies occur?
Its development is explained by the presence of dysbiosis in the patient - a condition caused by the predominance of opportunistic microflora in the intestines. This group of bacteria, unlike the “correct” one, does not help to realize immune tolerance, but, on the contrary, contributes to the occurrence of sensitization - heightened sensitivity of a specific nature (in relation to specific antigens). If it is formed, immune reactions occur. Initially protective, they become dangerous and, attacking an unnecessary target, damage the body’s own tissues, provoking allergic inflammation.
However, dysbiosis is not a final diagnosis, since a violation of the composition of microorganisms is not an independent disease. Many scientific works emphasize the secondary nature of this pathology - it is formed as a result of such reasons as:
Diseases of the digestive system (enteritis, colitis, cystic fibrosis, celiac disease, lactase deficiency).- Poor nutrition, use of antibacterial drugs (especially important for children in the first months of life).
- Late breastfeeding or lack of natural feeding.
- Long-term stay of a newborn in a medical institution (where the intestines could be colonized by unfavorable microorganisms).
- Infections in mother and child, complicated pregnancy and childbirth.
Allergies can be both a consequence and the primary cause of the development of dysbiosis.
It is formed not only due to changes in the composition of the microflora - this is only one of the factors. What matters is hereditary predisposition, massive intake of antigens against the background of weakened immunity (infections, incorrectly formulated diet, use of medications). When triggers come together, the result is sensitivity. In this case, disruption of the physiological intestinal barrier can play a decisive role.
What are “microflora” and “dysbacteriosis”?
Health is impossible without the normal functioning of the intestines, which play a large role in detoxification and immunological processes that occur in the human body. The intestinal mucosa is the point of contact between the body and the environment. For comparison: the surface of the skin is about 2 square meters, while the area of the mucous membrane of the gastrointestinal tract is about 400 square meters. Therefore, the intestinal mucosa is considered the largest part of the body's defense system.
For reliable protection against external interference in the digestive tract, the microbiological barrier turned out to be the most important.
- The protective intestinal microflora is the most numerous (95%) and is represented mainly by bifidobacteria, lactobacilli and E. coli. These microorganisms secrete lactic and acetic acids and other substances that have an antimicrobial effect and prevent harmful microorganisms that are not characteristic of humans from penetrating and attaching to the intestinal mucosa. They stimulate the human immune system and are sorbents that are capable of accumulating significant amounts of heavy metals and other toxic substances.
- The saprophytic intestinal microflora is represented by staphylococci, enterococci and other microorganisms, the main role of which is the utilization of the final metabolic products of the human body.
- Opportunistic microflora is represented by various microorganisms (streptococci, Staphylococcus aureus, gram-negative enterococci, Candida fungi, etc.), which under certain conditions cause a pathological process.
It is extremely important for the human body to maintain the required composition and quantity of intestinal bacteria. Optimal conditions can be disrupted due to poor nutrition, diarrhea pathogens (bacteria and parasites), additional negative factors can be toxic substances coming from the environment, for example, heavy substances - cadmium, lead, mercury, as well as travel to other countries with other microorganisms .
Food allergies have become an epidemic in our modern world.
While food allergies were considered an anomaly just a few decades ago, today one in 13 children in the United States suffers from life-threatening anaphylactic shock from a food allergy.
And this figure does not include those people who have celiac disease, gluten sensitivity, lactose intolerance, or any other type of food intolerance.
It is necessary to know that the intestines are a key player in the pathology of food allergies.
The human intestine is lined with millions of epithelial cells, which are responsible for maintaining a barrier between the intestinal contents (in the intestinal lumen) and the blood. In a healthy intestine, small-sized nutrients are absorbed from broken down proteins.
When the intestinal barrier is compromised (ie, leaky gut syndrome), large dietary proteins are able to enter the bloodstream, stimulate the immune response, and cause symptoms characteristic of various allergic diseases.
So how does this relate to microbes?
https://www.youtube.com/watch?v=23F6XO4x51c
Studies in mice have shown that disruption of the microflora by antibiotics or low-fiber diets can cause this increased barrier permeability.
On the other hand, some strains of Clostridium bacteria can protect against intestinal permeability to food allergens.
Researchers are working to develop probiotics containing these strains as a potential treatment for food allergies.
Even cataclysms that are insignificant for adults in the first hours and days of a child’s life cause damage to the process of formation of a young organism. It is welcome if the baby begins to feed from the mother quickly, a couple of hours after birth. It is not recommended to prescribe antibiotics to infants. Let us list the reasons for the development of dysbiosis in newborns:
- Late start of breastfeeding.
- Poor nutrition (human milk does not count).
- Gastrointestinal disorders (celiac disease, lactase deficiency).
- Taking antibiotics.
- Immune system disorders.
The first year of life is considered key in the process of microflora formation. An immature immune system cannot recognize pathogenic strains. To avoid the negative consequences of artificial feeding, lactose and oligosaccharides are added to adaptive milk formulas, trying to create the effect of the presence of the mother. Up to 8 months it is recommended to use adapted or partially adapted mixtures.
The presence of lactose and oligosaccharides allows bacteria to form an environment suitable for the development of colonocytes.
Of great importance in the treatment and prevention of dysbiosis in children is the natural feeding of the child, the predominance in the “artificial” menu of lactic acid products fermented with bifidobacteria, and sufficient intake of vitamins and microelements into the body. At the same time, allergic manifestations should be eliminated and concomitant diseases should be treated.
In the acute period, when the child is bothered by bloating and loose stools, to treat intestinal dysbiosis in newborns, it is necessary to take enterosorbents that help the body get rid of toxic products. We are well aware of the drugs in this class: activated carbon, polyphepan, smecta, polysorb, enterosgel. And be sure to create an appropriate sanitary and hygienic regime around the child.
However, the attitude towards cleanliness must be reasonable. Creating a sterile environment in the home is not only not welcomed by modern scientific views, but is also recognized as harmful to the health of the child. It is known that immunity is formed in constant interaction with the environment. Every contact with microorganisms, heat, cold, wind, sun and other environmental factors stimulates the immune system to develop resistance and immunity to negative factors.
In a child raised in greenhouse conditions, the immune system is inactive, since there are no harmful factors in the immediate environment, and there is simply no one for it to fight. Such a child will be defenseless against various infectious agents when he leaves sterile conditions and moves into the big world.
The intestinal mucosa has a rather complex structure. In addition to epithelial cells (the cells that line the intestinal wall), there are cells that secrete mucus, as well as various cells of the immune system:
- T-lymphocytes – recognize, kill and remember foreign agents;
- B lymphocytes that synthesize immunoglobulins (especially Ig A);
- Macrophages that capture pathogenic bacteria;
- Dendritic cells that receive information about a foreign agent and then transmit it to other immune cells.
Immune cells are scattered throughout the intestinal wall, but their concentration is especially high in the so-called Peyer's patches - clusters of lymphoid nodules in the intestinal wall.
The intestinal immune system has two important functions:
- Recognize, destroy and remember the alien agent;
- Obtain and save information about “your” bacteria and not destroy them, but, on the contrary, create conditions for their normal development and reproduction.
There are a huge number of bacteria in our intestines - more than 500 different species, some of which have not yet been studied. The contents of the intestine are considered the most intense microbial habitat on our planet. If you weigh all the intestinal bacteria, their weight will be at least 1 kg. Most intestinal bacteria belong to the class of bifidobacteria, lactobacilli, clostridia, streptococci and Escherichia coli.
A serious contribution to the study of microbial associations was made by I.I. Mechnikov. He suggested that it is the microbial flora that largely determines human health. Modern science has certainly stepped forward in this matter, although not all processes are still clear.
The relationship between immune cells that are located in the intestinal wall and bacteria is currently being studied. There are more questions than answers here. At the same time, certain patterns have been established between the presence of one or another type of bacteria and the formation of certain immune response cells (lymphocytes). It has also been proven that every living organism has its own unique set of bacteria.
https://www.youtube.com/watch?v=Z9UOtQgL20M
The bacteria that live in the intestines have certain effects on the body. To date, many studies of intestinal flora have been carried out on mice and some interesting results have been obtained. For example, in completely sterile mice that received bacteria from an animal with type II diabetes, an increase in blood sugar levels was observed. Another group of mice received bacteria from an obese animal, and as a result, they began to become overweight.
The main task of the intestines is to neutralize all harmful substances, toxins, foreign bacteria, viruses and fungi that come from food. To be fair, it should be noted that it is not only the intestines that fight “strangers.” Throughout the gastrointestinal tract there are special mechanisms for disinfecting food - saliva, acidic gastric juice, bile and others. But the intestines have a much higher level of immune protection than other organs, since 80% of the immune cells are concentrated there.
Microflora protects our intestines from pathogenic microorganisms. This happens due to competition for the nutrient medium. If the entire intestine is populated with normal flora, then “unnecessary” bacteria simply come out in transit - there is no place for them here. This property of intestinal bacteria to independently get rid of foreign agents significantly reduces the load on our immunity.
Microflora also corrects the functioning of the immune system, namely, it breaks down foreign proteins, making them less of an irritant to the immune system. Then it directs the antigens to Peyer's patches, where they are quickly destroyed. In addition, bacteria reduce the activity of inflammatory mediators.
Bacteria cover the intestinal mucosa with a thin layer, forming a biofilm, which represents a mechanical defense against physical and chemical aggression.
Symptoms
Allergies caused by disorders of the digestive system can manifest themselves in different ways, and are not at all limited to signs of damage to the stomach and intestines. The following groups of antigens can cause a reaction:
- food (fish, cow's milk, citrus fruits, peanuts);
- inhalation (animal hair, household dust, pollen);
- medications (antibiotics, vitamins, non-steroidal anti-inflammatory drugs);
- infectious (bacteria, viruses, fungi, parasites);
- contact (metals, chemicals, cosmetics, latex).
There are several main forms of flow that develop with sensitivity to these triggers. Let's take a closer look at them.
Atopic dermatitis
This is a disease whose development is based on a hereditary predisposition - that is, the presence of genes that cause excessive production of IgE class antibodies. In children of the first years of life, the most significant role is played by proteins obtained from food: milk, eggs, cereals. It is at this time that intestinal dysbiosis can lead to significant changes in the immune response and the development of a disease characterized by symptoms such as:
Skin rash. It is represented by nodules, vesicles, spots, plaques; elements often become wet and crusty. Areas of localization are the face (without affecting the nasolabial triangle), limbs, buttocks, and various parts of the body.- Itching. Quite strong, it leads to scratching, traces of which can be seen on the patients’ skin even during a quick examination.
- Dryness. Patients complain of tightness, peeling, and sometimes the appearance of cracks.
Treatment
An imbalance of intestinal microflora is a secondary disorder; The goal of therapy is to influence the root cause of the pathological process. This may be inflammation (not always of an infectious nature), enzyme deficiency, functional changes - for example, ineffective motility of the digestive tract. The main provoking factor must be eliminated; To do this, use the methods described in the table:
| Methods | |||||
| Basic | Additional | ||||
| Elimination | Use of antiallergic drugs | Diet | Using Probiotics | Treatment of primary pathology of the digestive tract | |
| Target | Protect the sensitive body from contact with the trigger. | Stop the development of the reaction and remove symptoms | Improve the condition of the stomach and intestines, eliminate irritation of the mucous membrane. | Correction of microflora composition and quality of immune response | Reducing the activity of the inflammatory process, normalizing intestinal function |
| Execution algorithm | Elimination of provoking substances from the contact zone: wet dust removal, refusal to consume causative food products, keeping animals, leaving for a safe region during plant dusting. | Prescribing tablets, ointments, drops with antihistamines (Zyrtec, Fenistil), cromones (Intal, Ketotifen) and topical glucocorticosteroids (Elocom, Mometasone) for a limited period of time (several days, weeks). In the acute stage, sorbents (Smecta, White Coal) may be needed. | It is recommended to steam, boil, stew or bake food. It is worth choosing foods rich in fiber (vegetables, fruits, cereals), as well as foods with a low level of allergenicity (excluding citrus fruits, tomatoes, seafood, peanuts). You should not eat spicy seasonings, drink carbonated drinks, alcohol, fatty or fried foods. | Taking medications containing beneficial bacteria and substances that stimulate their growth (Lacidophil, Bifiform, Lactulose, Hilak forte). | A balanced diet and medication are required: prokinetics (Motilium), enzymes (Mezim), and sometimes antibiotics (Imipenem). |
Thus, there is no single cure - a comprehensive approach is needed.
You should not use overly aggressive methods - for example, colon cleansing through fasting is contraindicated.
It leads to defects in the mucous membrane of the digestive tract, exhaustion, anemia, reduces resistance to infections and, in general, does not give the effect that can be achieved by correcting the diet (with normal calorie content) and adequate drug therapy.
Dysbacteriosis and allergies are mutually related pathologies. Often in young children, an allergic reaction occurs due to a violation of the microflora. The connection between these pathologies arises because the local intestinal immunity is responsible for the perception of other cells.
Dysbacteriosis and vitamin deficiency
Nowadays, people, trying to lead a healthy lifestyle, have learned to eat a balanced diet. They consume proteins, fats, carbohydrates in the correct ratio and quantity. Despite this, many suffer from vitamin deficiency.
The problem is that modern technologies process food so much that they do not give vitamins and microelements a chance to remain in it. Also, people who consume normal amounts of vitamins may suffer from vitamin deficiency. The cause is intestinal dysbiosis.
The absorption of nutrients, vitamins, and microelements directly depends on the intestines. Dysbiosis prevents the intestines from functioning normally. Therefore, vitamin deficiency and dysbacteriosis often go together.
No matter how expensive and high-quality preparations with vitamins a person consumes, the body has no chance to absorb them until the dysbiosis is cured.
Symptoms appear more often in adult women, because they are the biggest fans of extreme weight loss methods.
Strict restriction in food provokes an imbalance in the intestines, as well as a lack of vitamins and beneficial microelements. To avoid this situation, you need to consume probiotics and fermented milk products on diet days.
Symptoms of vitamin deficiency against the background of dysbacteriosis can manifest themselves in the following:
- skin problems;
- hair loss;
- nausea, vomiting;
- lack of appetite;
- decreased immunity;
- sensitivity, tooth decay;
- rapid weight loss;
- decreased mental activity;
- diarrhea;
- pain in the limbs.
If you have these symptoms, you need to take care of your intestinal microflora.
- Introduce coarse fibers, cereals, bran bread, fruits, vegetables, and dairy products into the diet;
- Limit the consumption of sugar, white bread, baked goods, sweet drinks, and alcohol.
- Do not eat food that contains preservatives, dyes, or flavors.
- Take probiotics and vitamins regularly.
- Eat regularly.
- Eat only freshly prepared food.
The connection between allergies and dysbiosis
In the human body, all processes are interconnected. Digestive disorders affect a person’s well-being and emotional state. This often becomes the cause of the development of new diseases. Allergy is one of them.
Digestive disorders are accompanied by changes in the skin. A rash and redness appear. These are the first signs of allergic dysbacteriosis. For many people, this relationship is surprising. Pathogenic microorganisms produce toxins that can cause intoxication.
Local immunity reacts aggressively to these toxins and produces antibodies to them. In this way, an allergic reaction develops. Harmful cells enter the bloodstream. Signs appear on the skin, mucous membranes, eyes, digestive and respiratory systems. In its advanced form, the disease requires long-term treatment. It is worth noting that signs of this pathology may not appear for several years.
Clinical picture
Symptoms of allergic dysbiosis rarely appear in the initial stage. A person can live with this pathology for several years and not suspect its presence. Signs resemble indigestion:
- diarrhea, which alternates with constipation;
- vomit;
- abdominal pain;
- increased gas evolution;
- skin rash (especially on the back, stomach, cheeks);
- swelling of the mucous membranes;
- itching;
- redness;
- headache;
- increased irritability;
- insomnia.
Against the background of this pathology, frequent colds and food poisoning are observed. A person may lose weight due to lack of appetite. You feel increased fatigue and drowsiness. The emotional state also suffers. The person is irritable and restless. The number of stressful situations and nervous tension increases.
Diagnostic methods
First of all, you should contact a leading specialist. During the initial examination, it is difficult to suspect this type of disease. A true diagnosis can only be discovered after laboratory tests. Diagnosis of allergies includes the following methods:
- General blood analysis. Shows the level of eosinophils. An increase in their number often confirms the presence of allergies or helminthic infestations.
- Enzyme immunoassay blood test. Determines the presence of antibodies.
- Skin tests. They are carried out in the form of subcutaneous injections. Within a short time they help identify the irritant.
- Allergy tests.
- Provocative tests.
After identifying the irritant, treatment is prescribed. In some cases, diagnosing allergies is not as easy as it may seem. Re-diagnosis is often carried out, the patient follows a strict diet and keeps a food diary. Do not forget that medications often cause such a reaction.
Diagnosis of dysbiosis is generally reliable. It is carried out using the following methods:
- bacteriological analysis of feces (determines the presence of pathogenic microorganisms, E. coli, helminths);
- colonoscopy;
- irrigoscopy;
- gastroscopy.
An instrumental examination is carried out to determine the condition of the intestinal and gastric mucosa. With chronic dysbiosis, severe inflammation begins, which can cause the development of serious diseases.
Treatment options
Treatment of allergy symptoms consists of the use of medications of different groups:
- Antihistamines. Eliminate symptoms, prevent the development of severe complications, and promote rapid recovery. These drugs include: Tavegil, Claritin, Loratidine, Fenistil; Citrine. Use strictly as prescribed by a doctor.
- Enterosorbents. Removes toxins and waste from the body. Used when signs of an allergic reaction develop. The use of activated carbon and Enterol will be effective.
- Glucocorticosteroid ointments and moisturizing creams. Used to eliminate symptoms that appear on the skin. Eliminate rash, itching, peeling, and dryness faster. Products such as Lokoid, Aquaderm, Bepanten are effective.
Drug therapy is necessary for the development of moderate and severe stages. When the allergen cannot be identified for a long time, the patient is prescribed a strict diet and immunotherapy. Treatment of dysbiosis with drugs begins with the development of the second stage. The initial development of pathology does not require drug therapy; it is enough to balance the daily diet and adhere to a nutritional schedule. The following drugs are prescribed for treatment:
- probiotics;
- prebiotics;
- bacteria and live strains;
- bacteriophages;
- immunostimulants;
- enzymes;
- anti-inflammatory drugs;
- antibacterial drugs.
Restoration of intestinal microflora is long-term and requires complex treatment. It is important to pay attention to nutrition. During the period of drug therapy, it should be complete, vitamin, and dietary. Eating unhealthy foods can cause allergies.
Young children, especially infants, often experience dysbacteriosis and allergies. The reason lies in a weakened immune system and an underdeveloped digestive system. They are susceptible to infection with staphylococcus, salmonella, and E. coli, so it is important to monitor the quality of the products consumed.
Formation of infant microflora and possible risks
With a systematic allergic response, an adult patient develops anaphylaxis, which provokes complications:
- decreased blood pressure;
- swelling;
- severe skin rashes;
- bronchospasm;
- to whom.
Sometimes the disease can lead to death.
Dysbacteriosis is dangerous if the child is allergic. Excessive synthesis of toxins leads to a constant response from the body. Children may experience digestive system disorders related to intestinal flora. The baby may develop:
- diseases of the rectum;
- allergy status to certain foods, other antigenic forms.
Untimely treatment of the disease leads to a decrease in the functioning of the baby’s immune system.
Accurate and timely diagnosis of allergies due to dysbiosis helps determine the optimal therapeutic treatment and eliminate the cause of the pathology. A diet on the recommendation of a nutritionist, a comfortable temperature in the house for the baby will help prevent the onset of the disease.
Smecta prevents the absorption of toxins, and Bepanten prevents minor skin rashes. When treating dysbiosis, experts recommend taking medications aimed at eliminating the cause of the disease - prebiotics and probiotics.
The article has been approved
by the editors
In the womb, the fetus has no contact with any bacteria, which the mother’s body takes care of; all nutrients enter through the bloodstream. When a baby is born, he comes from an absolutely sterile environment into a world full of various microbes, which almost immediately begin to populate his body.
The baby's intestines are partially filled with microbes during childbirth. But these microbes are not enough. It is believed that when applied to the mother’s belly, her skin partially gives up its microflora, thereby protecting the newborn from the initial colonization of “foreign” microbes.
Feeding newborns in the first days is especially important. After the first meal, the intestines become the habitat of a huge number of microorganisms. In general, the formation of intestinal microflora takes several months after birth.
At the same time, children experience transient dysbacteriosis, which does not require treatment. Due to negative factors, the balance between beneficial and pathogenic organisms may be disrupted, which is caused by several factors:
- Lack of breastfeeding or no milk at all, which means you have to switch to formula too early. Unlike breast milk, they are less conducive to the normal formation of microflora.
- Taking antimicrobial drugs, which kill beneficial bifidobacteria and lactobacilli. Even if antibiotics were prescribed to the mother, the baby also has a risk of developing dysbiosis.
- Introducing complementary foods ahead of time. Up to six months, infants are not able to digest solid food, so the inclusion of “adult” foods in the diet can significantly disrupt digestion.
- Intestinal infections that inflame the mucous membrane, this entails the growth of pathogenic bacteria.
- Food allergies. Allergens lead to damage to the cells of the gastrointestinal tract, thereby disrupting the functioning.
- Poor nutrition, unsanitary conditions and other factors that weaken the immune system.
Prevention and useful tips
Allergic dysbacteriosis occurs quite often. Diagnosis becomes more complicated due to the long-term concealment of characteristic symptoms. Preventive measures will help prevent the development of such pathology:
- healthy, nutritious nutrition;
- daily consumption of fermented milk products;
- checking the quality and freshness of products before use;
- increasing immunity;
- correct use of medications;
- Avoid consuming allergenic foods.