General concepts
The pancreas (Pancreas) (Latin - pancreas) is a double secretion gland with a lobular structure.
The pancreas secretes the hormones insulin, glucagon, somatostatin and other biologically active substances.
The first endocrine role of the pancreas was noticed by attentive German scientists J. Mering and O. Minkowski in 1889. During experiments, it became known that when the pancreas is removed in dogs, the symptoms are the same as in a person with diabetes: the level of sugar in the blood becomes elevated, and it is excreted in large quantities in the urine; Appetite and thirst increase and urine output increases significantly. All noticed symptoms disappear if the animal’s pancreas is transplanted under the skin.
In 1901, the Russian doctor L.V. Sobolev confirmed the opinion of his German colleagues that the endocrine function in animal organisms is performed by the pancreas. According to L.V. Sobolev, the pancreas secretes hormones involved in the regulation of carbohydrate metabolism. However, for a long time hormones could not be isolated from pancreatic tissue.
That is why pancreatic hormones are polypeptides that are destroyed under the influence of proteolytic enzymes of pancreatic juice. L.V. Sobolev presented two methods for obtaining the pancreatic hormone (insulin). In the first method, the animal's excretory duct is interrupted several days before the pancreas is removed. In this case, there is no release of pancreatic juice into the cavity of the duodenum, and the acinar tissue atrophies. As a result, the possibility of pancreatic juice enzymes affecting insulin is eliminated and it can be detached from the gland tissue. In addition, L.V. Sobolev proposed extracting insulin from the pancreas of embryos and newborn calves, since insulin synthesis is already taking place, but the pancreas does not form digestive juice. And only 20 years later, Canadian scientists were able to create an active drug.
Glucagon
Glucagon restores normal blood glucose concentrations if they decrease.
Glucagon has the form of a single-chain polypeptide, which, together with insulin, is actively involved in the regulation of carbohydrate metabolism and is its antagonist in its action. It protects the body from hypoglycemia and restores normal glucose concentration when it decreases. Thus, it helps maintain a constant level of glucose, which is very important for the normal functioning of nervous tissue.
The biological action of this hormone is as follows:
- activation of glucose synthesis from amino acids and other non-carbohydrate compounds;
- acceleration of glycogen breakdown and inhibition of its synthesis;
- reduction of cholesterol and triglycerides in the blood;
- increased lipolysis and formation of ketone bodies;
- increased renal blood flow and glomerular filtration rate;
- slowdown of platelet aggregation and activation of glycogenolysis in the heart muscle (increased cardiac output, decreased vascular resistance);
- increased formation of catecholamines, insulin, calcitonin;
- decreased secretion of digestive enzymes, pancreozymin, gastrin.
Glucagon activity increases in the following cases:
- with hypoglycemia;
- decreasing the concentration of free fatty acids in the blood serum;
- increasing the tone of the sympathetic nervous system;
- activating influence of gastrointestinal peptides.
Conversely, with hyperglycemia, an increase in the level of free fatty acids in the blood, as well as the influence of somatostatin, glucagon secretion decreases.
The normal functioning of α- and β-cells of the pancreas with adequate secretion of hormones ensures the constancy of glycemia and the internal environment of the body.
Function of the pancreas:
- The release of digestive juices into the duodenum and helps in the digestion of food, thanks to enzymes.
- The islet portion of the pancreas releases hormones directly into the blood.
Hormones secreted by the pancreas regulate metabolism - carbohydrates, proteins, fats.
External secretory (exogenous) function of the pancreas. The main product of the exocrine secretory function of the pancreas is digestive juice, which contains 90% water and 10% solid sediment. Juice density from 1.008 to 1.010; pH from 7.2 to 8.0 (horses 7.30-7.58; cattle 8). The composition of the dense sediment includes protein substances and mineral compounds: sodium bicarbonate, sodium chloride, calcium chloride, sodium phosphate, etc.
Pancreatic juice consists of:
Nucleoteolytic and proteolytic enzymes (trypsin, chemotrypsin, carboxypeptidase, elastase, nuclease, aminopeptidase, collagenase, dipeptase), amylolytic enzymes (a-amylase, maltase, lactase, invertase) and lipolytic enzymes (lipase, phospholipase, cholinesterase, carboxylesterase, monoglycerides, alkaline phosphate aza ).
Under the influence of trypsin, proteins are broken down into amino acids, after which trypsin is released in the form of inactive trypsinogen, which is activated by the enzyme enterokinase of intestinal juice.
Chemotrypsin also breaks down proteins and polypeptides into amino acids and is then released as inactive chymotrypsinogen, which in turn is activated by trypsin.
Carboxypeptidases affect polypeptides by separating amino acids from them.
Dipeptides are broken down into free amino acids under the influence of dipeptidase.
Elastase acts on connective tissue proteins (elastin, collagen).
Proteinase breaks down protamines and nucleases into nucleic acids, mononucleotides and phosphoric acid. Proteolytic enzymes are activated inside the gland during inflammation or autoimmune diseases, destroying it from the inside.
Starch, glycogen - a-amylase, maltose maltase glucose.
Milk sugar - lactase, glucose, galactose (important for the digestion of young animals).
Sucrose - invertase glucose, fructose.
Fat - lipase and other lipolytic enzymes, glycerin, fatty acids.
Features of the gland structure
The pancreatic gland is a key organ of the digestive system. It consists of two different fabrics:
- The secretory part of the organ is penetrated by a mass of excretory ducts, which are connected to the duodenum. Pancreatic enzymes (lipases, amylases, nucleases, elastases, trypsin, chymotrypsin, carboxypeptidases, collagenases) are synthesized here.
- The endocrine part (only 3% of the total mass of the gland) includes the islets of Langerhans. These areas have different morphology and biochemistry; here the synthesis of hormones occurs that regulate the metabolism of carbohydrates, proteins and lipids.
Important! Endocrine dysfunction of the pancreatic gland provokes the development of a number of pathologies. With hypofunction of the organ, glycosuria, hyperglycemia, polyuria and diabetes mellitus develop. With hyperfunction, hypoglycemia and obesity are observed.
Endocrine functions (hormonal) of the pancreas.
The pancreas in animals and humans secretes hormones - insulin, glucone and somatostatin, which are the most important hormones that regulate metabolism.
Insulin is considered the main hormone of the pancreas. It helps normalize blood sugar levels. This process occurs due to the following mechanisms: activation of cell membranes, as a result of which the body’s cells begin to better absorb glucose, the role of insulin in the body stimulates glycolysis (glucose oxidation process); slowing down the process of gluconeogenesis (glucose biosynthesis from non-carbohydrate substances such as lactic acid, glycerol, etc.); improves the supply of nutrients to body cells (phosphates, magnesium, potassium); protein synthesis is significantly enhanced, and at the same time its hydrolysis is suppressed.
So, the pancreas secretes the hormone insulin. Thanks to this hormone, protein deficiency is also eliminated, thereby strengthening the immune system and improving the synthesis of various substances of protein origin; the functions of fatty acid synthesis are activated. It is with a sufficient amount of insulin in the blood that the risk of developing atherosclerosis is reduced, the level of “bad” cholesterol is reduced and it becomes possible for fatty acids to enter the circulatory system.
What hormones does the pancreas secrete?
- Glucagon
- Insulin
- Somatostatin
Another hormone secreted by the pancreas is glucagon.
Based on the functions it performs, glucagon can be called an insulin antagonist hormone. The main function of glucagon is to increase the amount of glucose in the blood, which is achieved by the following functions: activation of gluconeogenesis (production of glucose from components that are not of carbohydrate origin); acceleration of enzymes, due to which the amount of energy increases during the breakdown of fats; Glycogen is broken down, which then enters the circulatory system. In its structure, glucagon is an endocrine type of peptide. A decrease in quantity can negatively affect the functioning of many systems, as it is responsible for many physiological processes.
Hormone production disorders
Most of the diseases associated with the production of glucagon involve increased secretion of this hormone. It signals the following diseases:
- insulin-dependent diabetes mellitus;
- glucagonoma, that is, a benign tumor of the alpha cell zone4
- acute inflammation of the pancreas;
- alcoholic, viral or drug-induced cirrhosis of the liver;
- Cushing's syndrome, which occurs due to too long exposure of the body to adrenal hormones;
- chronic renal failure can also be manifested by an increased level of glucagon in the blood;
- acute hypoglycemia, that is, a sharp drop in blood glucose to very low levels;
- severe stress for the body is surgery, burns or injuries, everything that one way or another leads to the release of adrenaline into the blood.
Good to know
The pancreas or, as it is also called, the pancreatic gland is an important organ of the digestive system, which is responsible for endocrine and excretory functions. Thanks to all the biologically active substances synthesized by the pancreas (PG), biochemical balance is maintained in the body. What pancreatic hormones exist and what are their functions in the body - all this will be discussed in this article.
Pancreatic hormones and their functions
Somatostatin
The synthesis of somatostatin occurs not only in the cells of the pancreas, but also in the anterior parts of the hypothalamus. It provides:
- inhibition of insulin and glucagon production;
- suppression of the secretion of hydrochloric acid and gastrin in the digestive tract;
- activation of cholecystokinin;
- regulation of blood flow speed in the vascular bed of the digestive system;
- contraction of smooth muscle fibers of the gallbladder;
- processes of nutrient absorption in the intestines.
The release of this hormone is stimulated by:
- introducing glucose or amino acids (leucine, arginine) into the body;
- gastrin;
- secretin, etc.
Some biologically active substances, such as norepinephrine and diazoxide, have the ability to inhibit its synthesis.
Under various pathological conditions, changes in the level of somatostatin in the blood are possible. Its concentration decreases in insulin-dependent diabetes mellitus. The literature describes cases of pancreatic tumors arising from δ cells that actively produce somatostatin.
How does the gland work?
The organ is divided into two parts: exocrine and endocrine. They all serve to perform their specific functions. For example, the exocrine part occupies most of the pancreas and serves to process gastric juice, which contains a large number of various enzymes necessary for digesting food (carboxypeptidase, lipase, trypsin, etc.).
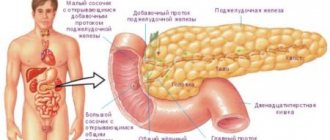
Structure and functions
The pancreas is the largest among the endocrine glands. Located retroperitoneally. The structure distinguishes: a rounded head, a wider body and an elongated tail. The head is the widest part, surrounded by the tissues of the duodenum. The normal width reaches five cm, the thickness is 1.5–3 cm.
Body - has front, back and bottom edges. In front it is adjacent to the posterior surface of the stomach. The lower edge reaches the second lumbar vertebra. The length is 1.75–2.5 cm. The tail part is directed posteriorly and to the left. Contacts the spleen, adrenal gland and left kidney. The total length of the gland is 16–23 cm, and the thickness decreases from three cm in the head area to 1.5 cm in the tail.
The central (Wirsungian) duct runs along the gland. Through it, the digestive secretion directly enters the duodenum. The structure of the parenchyma consists of two main parts: exocrine and endocrine. They differ in functional significance and structure.
Exocrine - occupies up to 96% of the mass, consists of alveoli and a complex system of excretory ducts, which are “responsible” for the production and release of enzymes into the digestive juice to ensure the digestion of food in the intestines. Their deficiency has a serious impact on the processes of digestion of proteins, fats and carbohydrates. The endocrine part is formed by an accumulation of cells into special islets of Langerhans. This is where the secretion of hormonal substances important for the body occurs.
Classification of synthesized substances
All hormones formed by the pancreatic gland are closely interrelated, so disruption of the production of at least one of them can lead to the development of serious disorders in the body and diseases that need to be treated for the rest of your life.
The pancreas produces the following hormones:
- insulin;
- glucagon;
- somatostatin;
- pancreatic polypeptide;
- vasointense peptide;
- amylin;
- centropnein;
- gastrin;
- vagotonin;
- kallikrein;
- lipocaine.
Pancreatic hormones
Each of the above hormones performs its own specific function, thereby regulating carbohydrate metabolism in the human body, as well as influencing the functioning of various systems.
The role of the pancreas in digestion
Clinical significance of pancreatic hormones
If everything is clear with the hormones produced by the pancreas, then with the main functions that they perform, everything is much more complicated. Let's consider each pancreatic hormone separately.
Of all the hormones that the pancreas synthesizes, insulin is considered the most important. It helps normalize blood glucose levels. The implementation of this process is due to the following mechanisms:
- activation of cell membranes, due to which the body’s cells begin to better absorb glucose;
The role of insulin in the body
Based on its functions, glucagon can rightfully be called an insulin antagonist hormone. The main task of glucagon is to increase the amount of glucose in the blood, which is achieved through the following functions:
- activation of gluconeogenesis (production of glucose from components of non-carbohydrate origin);
- accelerating the work of enzymes, due to which the amount of energy increases during the breakdown of fats;
- Glycogen is broken down, which then enters the circulatory system.
Since glucagon is a peptide type of hormone in its structure, it is responsible for many functions and a decrease in its amount can adversely affect the functioning of many systems.
Another hormone produced by the pancreas. It belongs to the group of polypeptide hormones and serves to suppress the synthesis of substances such as glucagon, thyroid-stimulating compounds, and insulin. When the level of somatostatin decreases in the gastrointestinal tract, serious disorders occur. First of all, this reaction is due to the fact that this hormone is directly involved in the production of digestive enzymes and bile (somatotropin reduces their secretion).
In modern pharmacology, somatotropin is used to create various medications that are prescribed to patients suffering from impaired synthesis of growth hormone in the body. If the amount of this hormone significantly exceeds the norm, then the risk of developing acromegaly increases, a pathology that is accompanied by an excessive increase in the size of certain parts of the patient’s body. As a rule, the feet, head bones, lower or upper limbs grow. In rare cases, individual internal organs undergo pathological changes.
Hormones are produced by small organs - endocrine glands. But the importance of these substances in the body is enormous.
This hormone was discovered not so long ago, so experts have not yet fully studied all its functions and methods of influencing the human body. It is known that pancreatic polypeptide is synthesized during the intake of food containing fats, proteins and glucose. It performs the following functions:
- reduction in the amount of substances produced by digestive enzymes;
- decreased muscle tone of the gallbladder;
- preventing the release of bile and trypsin.
On a note! According to numerous studies, pancreatic polypeptide prevents increased waste of bile and pancreatic enzymes. With a deficiency of this hormone, metabolic processes in the body are disrupted.
The peculiarity of this neuropeptide hormone is that it can be synthesized not only by the pancreas, but also by cells of the spinal cord, brain, small intestine and other organs. The main functions of the vasointense peptide include:
- normalization of the synthesis of pepsinogen, glucagon and somatostatin;
- slowing down the processes of water absorption by the walls of the small intestine;
- activation of biliary processes;
- synthesis of pancreatic enzymes;
- improving the functioning of the pancreatic gland in general, which helps to increase the amount of bicarbonates synthesized.
Mechanism of action
The brain, intestines, kidneys, and liver are the main consumers of glucose. For example, the central nervous system consumes 4 grams of glucose in 1 hour. Therefore, it is very important to constantly maintain its normal level.
The pancreas is a mixed secretion gland - it produces intestinal juice, which is secreted into the duodenum and secretes several hormones, so its tissue is anatomically and functionally differentiated. In the islets of Langerhans, alpha cells synthesize glucagon. The substance can be synthesized by other cells of the gastrointestinal tract.
Several factors trigger hormone secretion at once:
- Reducing glucose concentrations to critically low levels.
- Insulin level.
- Increased blood levels of amino acids (in particular alanine and arginine).
- Excessive exercise (for example, during vigorous or strenuous exercise).
The functions of glucagon are associated with other important biochemical and physiological processes:
- increased blood circulation in the kidneys;
- maintaining optimal electrolyte balance by increasing the rate of sodium excretion, which improves the functioning of the cardiovascular system;
- restoration of liver tissue;
- activation of cellular insulin release;
- increase in calcium content in cells.
In a stressful situation, when life and health are threatened, the physiological effects of glucagon appear together with adrenaline. It actively breaks down glycogen, thereby increasing glucose levels, and activates the supply of oxygen to provide muscles with additional energy. To maintain sugar balance, glucagon actively interacts with cortisol and somatotropin.
The main consumers of sugar are the kidneys, intestines, brain and liver. It is worth considering that the nervous system consumes 4 g of the substance per hour. That is why it is so important to control its normal volumes.
Glycogen is a substance that is primarily stored in the liver. This reserve is approximately 200 g. When there is a deficiency of glucose or the need for additional energy, glycogen breakdown occurs. As a result, the blood is saturated with glucose.
This volume is enough for about 40 minutes. Therefore, athletes often say that fat deposits begin to burn only after 30 minutes of training, when energy reserves in the form of sugar and glycogen are spent.
The pancreas belongs to the category of organs of mixed secretion. It produces intestinal juice that enters the duodenum and produces several hormones. Therefore, its tissue has a different structure from an anatomical and functional point of view.
The islets of Langerhans produce glucagon. Alpha cells are responsible for this. The element is also produced by other cells of the digestive organs.
Glucagon secretion depends on a number of factors:
- Reducing glucose levels to critical parameters;
- Insulin level;
- Increasing the level of amino acids in the body – primarily arginine and alanine;
- High physical activity.
The functions of glucagon help solve important problems:
- Increase blood flow in kidney tissues;
- Maintain an optimal balance of electrolytes - this is achieved by increasing the rate of sodium excretion, thereby normalizing the functioning of the heart and blood vessels;
- Activates the release of insulin from cells;
- Restores liver tissue;
- Increases calcium levels in cells.
This helps increase glucose levels, stimulate oxygen uptake and provide additional energy to muscle tissue. To maintain normal sugar balance, glucagon interacts with other hormones. These include somatotropin and cortisol.
The main site of action of this compound is the liver. Under its influence, glycogenolysis occurs in this organ first, and a little later - ketogenesis and gluconeogenesis.
This hormone cannot enter the liver cells on its own. To do this, it has to interact with receptors. When glucagon interacts with the receptor, adenylate cyclase is activated, which promotes the production of cAMP.
As a result, the process of glycogen breakdown begins. This indicates the body’s need for glucose, so it actively enters the blood during glycogenolysis. Another option is to synthesize it from other substances. This is called gluconeogenesis.
It is also an inhibitor of protein synthesis. Its effect is often accompanied by a weakening of the process of glucose oxidation. The result is ketogenesis.
This compound does not affect glycogen contained in skeletal muscles, which is explained by the absence of receptors in them.
The increase in cAMP caused by glucagon leads to inotropic and chronotropic effects on the myocardium. As a result, a person’s blood pressure increases, heart contractions become stronger and more frequent. This ensures activation of blood circulation and replenishment of tissues with nutrients.
A large amount of this compound causes an antispasmodic effect. In humans, the smooth muscles of the internal organs relax. This is most pronounced in relation to the intestines.
Glucose, keto acids and fatty acids are energy substrates. Under the influence of glucagon, they are released, making them available to the skeletal muscles. Thanks to active blood flow, these substances are better distributed throughout the body.
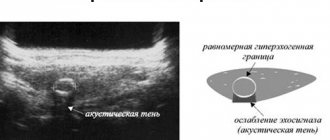
Diagnostic methods
Violation of the production of one or another hormone of the pancreatic gland can lead to various pathologies affecting not only the pancreas, but also other internal organs. In such cases, the help of a gastroenterologist is required, who, before prescribing a course of therapy, must conduct a diagnostic examination to make an accurate diagnosis. Below are the most common procedures performed for pancreatic dysfunction.
Diagnosis of pancreatic diseases
Table. Diagnostic studies of the pancreas.
| Procedure name | Description |
| Ultrasound examination is one of the most popular and effective methods for diagnosing pathologies of the pancreas and other internal organs. It can be used to identify tumors, cysts, the appearance of stones or the development of an inflammatory process. | |
| During endoultrasonography, pancreatic tissue can be examined for pathological changes. Also, using this procedure, the doctor examines the lymph nodes, if necessary. | |
| An effective way to diagnose the pancreatic gland, since computed tomography can detect possible atrophic processes, pseudocysts and various neoplasms. | |
| During this procedure, a microscopic examination of pancreatic tissue is performed. With its help, you can identify the inflammatory process and determine whether a malignant or benign formation has arisen in the organ under study. | |
| Blood and urine analysis | Based on the results of the tests, it is possible to determine the level of amino acids, direct bilirubin, seromucoid and other substances that indicate the development of a particular disease. |
| During a laboratory examination of stool, the doctor may identify particles of starch, fat, muscle fibers or fiber - all this indicates a disruption of the pancreas. |
On a note! In addition to the above diagnostic methods, the doctor may prescribe another procedure - a biochemical blood test. Unlike a general analysis, a biochemical blood test allows not only to determine possible infectious diseases, but also their type.
What causes hormonal imbalance
As noted earlier, pancreatic hormones are essential elements involved in the digestion process. Even minor disruptions in their synthesis can lead to serious complications (diseases, malfunctions of certain systems or organs, etc.).
Human endocrine system
With an excess of pancreatic hormones, for example, a malignant formation may occur (most often due to an increase in the amount of glucagon) or glycemia (with an excess of insulin in the blood). It is possible to determine whether the pancreas is working correctly and whether the hormone levels are normal only after a diagnostic examination. The danger is that many diseases associated with a decrease or increase in hormone levels can occur without any pronounced symptoms. But violations can be identified by monitoring your body’s reactions over a long period.
Normal, hypo- and hyperglycemia
First of all, you need to pay attention to the following points:
- decreased visual acuity;
- excessively high appetite (the patient cannot eat enough);
- frequent urination;
- increased sweating;
- severe thirst and dry mouth.
The role of pancreatic hormones in the functioning of the human body cannot be underestimated, since even with minor disturbances in the synthesis of these hormones, serious pathologies can develop. Therefore, it is recommended, as a preventative measure, to undergo diagnostic examinations with doctors in order to prevent disturbances in the functioning of the pancreas. It is enough to consult a doctor 1-2 times a year for a preventive examination in order to prevent not only various disorders in the functioning of the pancreatic gland, but also other problems with the gastrointestinal tract. It is also recommended to undergo periodic examinations with other doctors, for example, a dentist, dermatologist, neurologist. Read our article about the difference between a colostomy and an ileostomy.
Pancreatic hormones are very important
All pancreatic hormones are important to the body because they work to maintain biochemical balance.
Pancreatic diseases - symptoms and treatment
Timely consultation with a doctor in case of problems with the functioning of the pancreas can prevent the development of many serious diseases, in particular diabetes mellitus. You should contact a medical facility as soon as possible if you have the following symptoms:
- the appearance of painful sensations after eating fatty foods, as well as alcoholic beverages and excessive overeating. As a rule, there is girdling pain;
- painful sensations along with a feeling of nausea, vomiting;
- pressing on the stomach causes unpleasant feelings in the navel area;
- increased body temperature;
- constant problems with the digestive system, diarrhea;
- reduction of pain when bending forward.
The main problem is that pancreatic diseases are often not identified, misdiagnosed and erroneous treatment prescribed. Unfortunately, such diseases develop most rapidly and subsequently become chronic. The most common complications that you may encounter are diabetes, pancreatitis, and cancer.
As you know, diabetes mellitus is one of the most insidious diseases caused by insufficient production of the hormone insulin by the pancreas . This disease requires prompt treatment. Accompanied by such symptoms as constant loss of strength, long healing of any scratches, wounds, weight loss for no reason, tingling sensations in the arms and legs, poor vision, hearing loss, and a constant desire to drink.
Pancreatitis is characterized as severe inflammation of the pancreas. An acute cutting pain is felt; an experienced specialist can easily identify this ailment and perform palpation. Other symptoms of acute pancreatitis include sharp pain in the navel, indigestion, fever, nausea and vomiting. In the chronic form, rapid weight loss, lack of appetite, upset stool, and aversion to heavy fatty foods are observed. Pancreatitis is one of the most dangerous diseases that can lead to death if left untreated.
To maintain the health of the gland, it is very important to lead a healthy lifestyle. In particular, it is worth reviewing your diet and, if possible, excluding fatty, difficult-to-digest foods. Sweets and alcoholic drinks also have a detrimental effect on the condition of the organ. In addition, it is very important to exercise regularly and get rid of bad habits. Attentive and careful attitude towards yourself will extend your life and maintain health for many years.
Having considered which pancreatic hormones are involved in carbohydrate metabolism, and what their improper production can lead to, you should immediately reconsider your attitude towards your own body.
Insulin
The cells that produce it occupy a lot of space in the islets of Langerhans, accounting for 80% of the total number of all cells of these formations. Insulin is a very important hormone that regulates the use and storage of nutrients in the body. People diagnosed with diabetes due to insulin deficiency must take insulin by injection daily or several times a day.
The effect of insulin on carbohydrate metabolism
Insulin enhances the transport of glucose into cells (for example, into liver or muscle cells). It enhances the process of using glucose in intracellular compounds, that is, its combustion. In the liver and muscles, it increases the production of glycogen, which is stored in cells and used when necessary for the body. If there is a deficiency of glucose in biological fluids or tissues, glycogen breaks down and releases the necessary glucose. The result of all these metabolic processes is a drop in blood glucose levels. The stimulus for insulin secretion by the B cells of the islands of Langerhans is an increase in the amount of sugar in the blood, for example, after a meal. Insulin secreted by the pancreas normalizes the so-called glycemic index. If glycemia decreases, insulin secretion stops. Thanks to this self-regulation, there is no excessive drop in blood sugar. Injectable insulin leads to a decrease in blood glucose concentrations. If you take too high a dose of this hormone, hypoglycemia will occur, which is life-threatening. This condition can cause dysfunction and then damage to brain cells.
How to stabilize regulator performance
It is important to analyze the factors influencing pancreatic hormone secretion. If you violate the rules of nutrition, are addicted to protein diets, or consume large quantities of proteins to build muscle mass, you need to adjust your diet. If glucagon levels are low, the amount of protein needs to be increased, and if the levels are too high, it should be reduced.
If an increase in insulin antagonist secretion is associated with severe mental or nervous overload, it is important to change your occupation or stabilize the microclimate in the family. Long-term deviations in glucagon levels negatively affect insulin secretion, which can lead to excess or decrease in glucose concentration. Both conditions (hyper- and hypoglycemia) are dangerous for the body.
If sugar levels are critical (sharp decrease), it is important to promptly administer a synthetic analogue of the hormone glucagon. After the injection, the patient's condition quickly stabilizes, and glucose levels return to normal. It is important to monitor sugar levels to correctly calculate the total norm of pancreatic hormone.
If diseases are identified that negatively affect the level of insulin antagonist, you need to undergo therapy under the guidance of a specialized specialist. In most cases, a tumor process requires surgery to remove the tumor. You cannot trigger pathological processes in the stomach and intestines: a decrease or increase in the concentration of an insulin antagonist in the blood plasma disrupts the functioning of the digestive tract.
As the body recovers from burns and injuries, glucagon levels gradually return to normal. It is important to provide psychological rehabilitation to the patient to reduce the risk of fluctuations in insulin antagonist levels.
Learn about the causes of functional ovarian cysts in women and the treatment of the tumor.
The symptoms of an enlarged thymus gland in children and treatment options for the pathological condition are written on this page.Go to https://fr-dc.ru/vnutrennaja-sekretsija/shhitovidnaya/oftalmopatiya.html and read about how to treat endocrine ophthalmopathy and prevent the development of dangerous complications.
The effect of insulin on fat and protein metabolism
Insulin increases the production of fatty acids. Enhances the production of triglycerides. It also inhibits lipolysis, that is, the breakdown of fats. The result of its work is the storage of fat in tissues. Anabolic hormones of the pancreas enhance protein production and at the same time inhibit its breakdown. They increase the transport of amino acids into cells. Insulin, affecting metabolic processes, affects primarily:
- on the muscles in which it activates the process of using glucose as an energy source;
- to adipose tissue, where its main task is to quickly convert glucose into fat and maintain this supply;
- on the liver, where its effect is manifested in increased production of glycogen (storage sugar), triglycerides and proteins.
Consequences of insulin deficiency
Insulin deficiency causes metabolic disorders, including the metabolism of carbohydrates, proteins and fats. A disease in which there is a deficiency or absence of insulin is called diabetes mellitus. The first sign of diabetes is an increase in glucose levels in the bloodstream. Then other violations appear. In case of type 1 diabetes, regular administration of insulin is necessary. Type 2 diabetes mellitus often occurs due to the fact that the pancreas produces hormones in sufficient quantities, but the body does not respond to them (insulin resistance). This form of diabetes is treated with medications and a healthy lifestyle (diet, exercise).
Indications for use of the glucagon drug
The effect of the hormone on the concentration of glucose and glycogen is used to treat various pathologies. Indications for use of the drug are as follows:
- severe hypoglycemia, when glucose cannot be administered through an IV;
- suppression of gastrointestinal motility during radiation diagnostics;
- for patients with mental disorders as shock therapy;
- acute diverticulitis (inflammation of the intestines with the formation of pouch-like protrusions);
- pathologies of the biliary tract;
- to relax the smooth muscles of the intestine.
Synthetic glucagon is used in medicine in two cases. The first purpose is the correction of severe forms of hypoglycemia, when for some reason glucose infusion (dropper) is impossible. The second meaning of glucagon is the preparation of examinations of the upper and lower gastrointestinal tract, especially for radiological diagnostics.
Glucagon-like peptide can also be used to treat type 2 diabetes. This substance has a structure similar to glucagon, but is an incretin - synthesized in the intestines after eating. The drug is designed to correct glucose levels, in some cases even without additional insulin.
The list of indications for taking hormonal glucagon preparations includes:
- shock therapy for patients with mental disorders
- diabetes mellitus with simultaneous hypoglycemia
- auxiliary drug for laboratory diagnostics
- relieving spasms in acute intestinal diverticulosis
- relaxation of smooth muscles of the stomach and intestines
There are 3 main options for glucagon injection - intravenous, intramuscular and subcutaneous. If emergency assistance is required (for example, in case of hypoglycemic coma), exclusively the first two options are used.
The standard dose of a hormonal drug for medicinal purposes is 1 mg. Improvement usually occurs within 10 minutes. To prepare for diagnosis, 0.25-2 mg is needed, the dosage is determined by the attending physician.
There are special recommendations for the use of the drug for children and pregnant women. Since glucagon does not penetrate the placental barrier, it can be used during pregnancy. But - only in emergency cases and according to the doctor's decision. The use of glucagon drugs for children weighing less than 20-25 kg is not recommended.
When treating with glucagon drugs, the recovery period is also very important. After improvement, the patient needs protein foods, sweet tea and complete rest for 2-3 hours. If hormonal medication does not help, intravenous glucose is required.
The drug containing glucagon (the instructions confirm this) contains substances extracted from the pancreas of animal origin (pork, bovine).
They are identical to those components produced by the human body. The effect of Glucagon on the concentration of substances such as glucose and glycogen allows its use for therapeutic purposes in the following cases:
- in severe conditions caused by hypoglycemia. It is observed most often in patients with diabetes. It is used mainly in cases where it is not possible to administer glucose intravenously;
- in radiological diagnostics as a means of suppressing the motility of the digestive system;
- during shock therapy in patients with mental disorders;
- in the presence of acute diverticulitis as a means of eliminating spasms;
- in the presence of pathologies of the biliary tract;
- to relax intestinal smooth muscles.
The instructions for glucagon indicate that this drug is used for hypoglycemia in an amount of 1 ml intravenously or intramuscularly. An increased glucose level is observed 10 minutes after administration of the medication. Often this is enough to avoid damage to the central nervous system.
Instructions for use of the drug indicate that it can be used in an amount of 0.5-1 ml for sick children whose body weight exceeds 20 kg. If the child weighs less, then the permissible dosage is no more than 0.5 ml, which corresponds to 20-30 mcg/kg. If after the first injection of the hormone the desired effect does not occur, it is recommended to repeat the injection after 12 minutes.
The following factors are considered contraindications to the use of this hormonal drug:
- hypersensitivity to the components of the medicinal product;
- hyperglycemia;
- insulinoma;
- pheochromocytoma.
This drug is indicated for the treatment of certain problems in pregnant women. It does not penetrate the placental barrier and does not affect the fetus in any way. During breastfeeding, this hormonal drug is prescribed with caution.
- Guide to pediatric endocrinology / Ivan Ivanovich Dedov, Valentina Aleksandrovna Peterkova. – M.: Universum Publishing, 2006. – 595 p. : ill.
- Ocular manifestations of diabetes / ed. L. I. Balashevich. – St. Petersburg. : St. Petersburg State. honey. acad. postgraduate education, 2004. – 382 p. : ill. – Bibliography at the end of the chapters.
- Secrets of endocrinology: textbook. allowance: trans. from English – 2nd ed., rev. and additional – M.: BINOM; St. Petersburg : Nevsky Dialect, 2001. – 464 p. : ill.
- Diabetic foot syndrome: diagnosis, treatment and prevention / M. B. Antsiferov, E. Yu. Komelyagina. – Moscow: Medical Information Agency, 2013. – 304 p. : rice. – Bibliography at the end of the chapters.
CONSULTATIONS WITH A THERAPIST OF THE FIRST CATEGORY. ONLINE CONSULTATIONS, OUTPATIENT APPOINTMENTS, HOME CALLS.