One of the functions of the gland, called the pancreas, is to produce pancreatic enzymes for the functioning of the gastrointestinal system. The pancreatic ducts are considered one of the main participants in the transportation and removal of digestive secretions. Through them, enzymes produced by the acini are excreted into the duodenum. There are main pancreatic canals, accessory and small ductal canaliculi.
- 3.1 Anomalies and dilation of the duct
Types of pancreatic ductal system
The pancreatic ducts are considered one of the main components of the digestive tract. They promote the excretion of enzymes that are located in pancreatic juice. Typically, the pancreatic duct opens into the intestine.
In medicine, there are 4 types of ducts.
- First form. One ampoule is formed, which implies the union of the common bile and pancreatic ducts. It exits through the nipple of Vater using the sphincter of Oddi.
- Second form. There is a connection of two channels that are close to the sphincter of Oddi. But in this case, the formation of a common ampoule does not occur.
- Third form. The bile and pancreatic ducts enter the intestinal lumen and pass through the nipples of Vater.
- Fourth form. Two large canals connect near the papilla of Vater.
The anatomy and physiology of the excretory ducts are quite complex. But they play an important role in the digestion of food.
The concept of the Wirsung duct
In medicine it is indicated that this path is one of the main ones, the pancreatic duct flows into the intestinal canal. The duct of Wirsung is necessary for the juice produced by the stomach to enter the duodenum. Its length ranges from 15-20 cm. The size depends on the individual characteristics of the organism. The width of the duct may vary depending on the specific part. So the diameter of the head is 4 mm, and in the tail it narrows to 1.5-2 mm.
The Wirsung duct is shaped like an arc. Often follows the curve of the pancreas. But there are various anomalies. It can be S-shaped or follow the bend of the knee.
In the body of every person there are additional ducts that flow into the main one.
- If the main channel has a main structure, it means that up to 30 smaller channels flow into the main channel.
- If it is characterized by a loose structure, then the number of small channels is 50.
With a trunk structure, lobular-type paths are observed. They are located 1.5-2 cm apart. With a crumbly structure, the distance between them decreases.
Often, a fusion of the Wirsung duct and the bile ducts is diagnosed. Against this background, they open slightly into the duodenum.
There are situations when the structure of internal organs is significantly changed. Then the main duct flows directly into the intestinal canal. This situation occurs in 20-30% of people around the world. But experts do not consider this process anomalous.
There are also cases when a bifurcation of the duct is observed in the structure of organs against the background of unfavorable factors. Their functionality is considered separate and equal in impact. These changes relate to congenital and rare pathologies. But they are dangerous, because they may narrow or completely overlap.
Where do the ducts of the gland and liver open?
In the region of the head of the Wirsungs, the canal merges with the Santorini and common bile ducts. Afterwards, through the lumen they open into the intestine with the large nipple of Vater (duodenal). The confluence of the liver and pancreas excretory ducts passes through the common bile duct. It is formed after the fusion of the gallbladder duct with the common hepatic duct in the liver. In 40% of people, the accessory duct opens into the intestine separately through the small duodenal nipple.
In 40% of people, the accessory duct opens into the intestine separately through the small duodenal nipple.
In the anatomy of the junction of the excretory ducts of the pancreas and the liver, 4 structures are distinguished. The first case is typical for 55%, when a common ampulla is formed at the confluence of the ducts. With this structure, the sphincter controls both exits. In the second case, the excretory channels merge without forming an ampoule, and then open into the intestine. This arrangement occurs in 34% of people. The 3rd type of exit location (4%) is considered rare, when the main ducts of the liver and pancreas flow separately. The fourth case is characteristic of 8.4%, in which both excretory ducts are connected at a great distance from the duodenal nipple.
Anomalies and dilation of the duct
Changes and deviations in the anatomy of an organ are classified as developmental anomalies. The causes are usually congenital. Genetic defects can cause the main channel to bifurcate, resulting in a pair of main output branches. A narrowing called stenosis may occur. As a result of stagnation or blockage of small tubules and the main channel, pancreatitis develops. Narrowing of the excretory tubules leads to digestive problems. Stagnation and changes in fluid provoke cystic fibrosis, which causes modifications not only of the gland, but also of some body systems.
In 5% of people, an additional duct may form, which is called an aberrant (accessory) duct. It originates in the head area, and through the Helly sphincter it removes digestive enzymes into the intestine. An additional excretory duct is not considered a disease, but requires special study and treatment. It should be noted that blockage often causes attacks of acute pancreatitis.
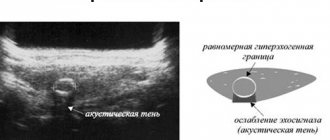
The normal size of the Wirsung duct is 0.2 cm. A change in size leads to a malfunction of the pancreas. Dilation of the duct can lead to the appearance of a tumor or stones in the gland. There are frequent cases of blocking of the intrapancreatic duct in the pancreas and the development of chronic pancreatitis. Acute forms of the disease often require pancreatectomy (removal of an organ).
The concept of the Santyrinian channel
This type of duct is considered accessory. It is localized in the middle region of the head of the pancreas. It may flow into the main channel. Doctors say that this phenomenon is diagnosed in 35% of patients. When it is detected, it is observed to be open above the location of the duodenal nipple.
If the main duct atrophies or there is a malfunction in functionality, then all work moves to the additional channel.
Through the sphincter, which is called Helly, gastric juice enters the small intestine. But this part of the organ has its own peculiarity. It blocks the process of reverse movement of juice and the possibility of contamination of the canal with stomach contents.
The head of the pancreas is distinguished by its duct system. Through them the process of elimination occurs.
At present, the excretory ducts of the pancreas are divided into three types.
- Top type. Its opening is observed in the Santorini channel. In some cases, its combination with the head of the lower duct is observed. The upper type does not have an independent outlet into the duodenum.
- General type. This type of canal is characterized by its origin in the body of the pancreas.
- Bottom type. It is distinguished by the presence of a connection with the upper type, resulting in the formation of one duct.
If the additional ducts stop functioning due to their blockage, the person will experience a severe attack of acute pain.
Additional treatments and prevention
With early diagnosis of single tumors, the survival rate for 5-10 years is almost 90%. The prognosis worsens if there is a history of MEN and a tendency to re-form and metastasize tumors. In patients with inoperable forms of gastrinoma, the 10-year survival rate is about 25%.
There is no specific prevention, since the disease is associated with hereditary factors. Currently, developments are underway in the direction of gene therapy for such conditions. People with a complicated medical history are advised to regularly visit an oncologist and gastroenterologist in order to notice the appearance of a tumor in time. Early detection and treatment of gastrinoma improves prognosis.
Izvozchikova Nina Vladislavovna
Gastroenterologist, Infectious disease specialist, Pulmonologist. Work experience: 36 years.
1975-1982, 1MMI, San-Gig, highest qualification, infectious disease doctor
Ask a Question
angiography;
- study of portal venous blood samples to determine the gradient of hormone concentrations.
A person with gastrinoma needs a certain regimen and diet. Correctly selected additional treatment methods depend on the chosen patient management tactics. If the gastrinoma is benign, then a regimen similar to that for peptic ulcers is recommended.
When treating gastrinoma conservatively, you should adhere to a diet. The diet is selected depending on the patient’s condition. The required menu is based on diet No. 1. The purpose of the diet is to moderate the mechanical, chemical and thermal effects on the gastrointestinal tract, relieve inflammation, accelerate the healing of ulcers and normalize the motor and secretory functions of the stomach. It is recommended to adhere to the diet prescribed by the doctor for approximately 3-5 months. In this case, you need to eat fractionally 6 times a day.
| Eating | Monday | Tuesday | Wednesday | Thursday | Friday |
| Breakfast 1st | Meat cheese Mashed rice porridge with milk Tea with milk | Curd cheese Semolina milk porridge Tea with milk | Boiled tongue Buckwheat porridge pureed Tea with milk | Grated cottage cheese with sugar and sour cream or curd paste Oatmeal porridge with milk pureed Tea with milk | Steamed meat soufflé Semolina milk porridge Tea with milk |
| Breakfast 2nd | Curd paste | Baked or fresh apples | Curd or fruit soufflé | Baked apples | Potato soufflé with sour cream |
| Dinner | Oatmeal soup with pureed vegetables | Vegetarian pureed pearl barley soup | Puree rice soup with vegetables | Semolina milk soup | Milk noodle soup |
| Eating | Saturday | Sunday |
| Breakfast 1st | Herring pate Puree buckwheat porridge Milk tea | Curd cheese Semolina milk porridge Milk tea |
| Breakfast 2nd | Fresh apples | Carrot-apple soufflé |
| Dinner | Puree rice soup with vegetables | Vegetarian pureed pearl barley soup |
With gastrinoma, it is better to limit the consumption of foods that increase gastric secretion, irritate its mucous membrane and are difficult to digest. Dishes must be cooked by steaming or in water, and often taken in pureed form. Some dishes are baked, but do not allow a crust to form. Meat and fish can be eaten in pieces. Table salt is acceptable in small quantities. Very hot and cold dishes are completely prohibited.
Preventive measures for gastrinoma are still unknown. Therefore, if you have health problems, you should consult a doctor.
Types of pathological processes
The duct of the pancreatic organ can open into any part of the organ. Such a process may occur as a result of abnormal development. There are two types of pathologies: congenital and acquired.
Genetic diseases include bifurcation of the canal, resulting in the formation of two branches. Each of them can contain several additional paths.
There are other types of diseases:
- stenosis of the duct system;
- abnormal dilation of the duct;
- obstruction of the pancreatic and biliary tract;
- inflammatory process.
In the pancreas, fibrosis often develops in the parenchyma area. The cause of the anomaly is the development of congestion or a change in the composition of pancreatic juice.
Consequences and possible complications
Gastrinoma can cause consequences in the form of metastases. The tumor can spread to other tissues and organs, resulting in the appearance of new foci of a tumor nature. A hormonally active tumor caused by a large amount of gastrin may be accompanied by complications:
- ulcerative bleeding;
- ulcer penetration (gastric ulcer extends beyond its boundaries);
- perforation (the appearance of a through defect in the stomach, during which the contents of the intestine or stomach can escape into the abdominal cavity);
- pyloric stenosis (the passage of food is disrupted when the opening between the duodenum and the stomach narrows).
Causes of abnormal formation of ducts
Many patients, after diagnostic measures, do not understand why the pancreatic duct is enlarged. The reasons for this process are:
- the appearance of a localized tumor in the head of the pancreas or the presence of the ampulla of the papilla of Vater in the small intestine. Against the background of these processes, the patient is diagnosed with obstructive jaundice;
- accumulation of stones with further blocking of the pancreatic passage. The stones usually pass from the gallbladder;
- chronic inflammatory process.
The main reason for the narrowing of the ducts is the development of stricture. Most often, this phenomenon occurs after surgery.
Narrowing of the duct system can occur due to parasitic infection of the body. Then there is a significant increase in liver size.
Diagnosis of the disease
Since gastrinoma occurs in the presence of ulcers of the stomach and duodenum, an endoscopy and x-ray of the stomach will reveal their presence. Thanks to such a diagnosis, it is possible to detect ulcers that exceed 2 cm in size, their localization, and hypertrophy of the folds of the mucous membrane in the stomach.
Quite often, a study of the level of gastrin in the blood serum is required. This diagnosis is carried out on an empty stomach. As a rule, the amount of gastrin in the disease exceeds the norm (60 pg/ml) by 5-30 times. To differentiate hypergastrinemia, gastritis and hyperthyroidism, functional provocative tests are used - administration of calcium or secretin.
Additionally, MRI, CT and ultrasound of the abdominal pancreas are required for topical diagnosis. Selective abdominal angiography is used to determine the amount of gastrin in the blood and to accurately diagnose gastrinoma.
Various diagnostic measures will be required to identify gastrinoma.
Note! It is very important to conduct a number of studies to distinguish gastrinoma from ulcers, duodenal tumors, medullary thyroid cancer and celiac disease. Sometimes it is necessary to perform an X-ray of the sella turcica, MRI or CT scan of the brain to exclude multiple endocrine neoplasia grade I.