How is gastroscopy (esophagogastroduodenoscopy) performed?
In order to conduct the examination with the greatest information content, it is important to know how the preparation for the gastric endoscopy procedure goes:
- To prevent a gag reflex and cough, the patient’s mouth and throat are treated with a solution for local anesthesia. In exceptional cases, anesthesia is appropriate for gastric endoscopy;
- The patient should lie in a position on his left side and press his knees as close to his stomach as possible;
- A mouthpiece in the mouth will make it possible to quickly install the endoscope without damaging the tube during swallowing;
- To better visualize the internal organs, the abdominal cavity is filled with a small amount of air.
How is it carried out?
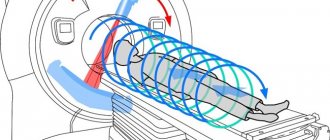
The research technique is as follows: an endoscope is inserted through holes into the human body. Various types of devices are used in different fields of medicine. The ways of its administration are different. For example, during an endoscopic examination of the stomach, the device enters through the oral cavity.
Modern devices are equipped with light and image transmission systems. After the endoscope gets inside, the image is displayed in real time on the screen, the doctor has the opportunity to examine the required organ in an enlarged size and identify pathological processes.
General information about the procedure
Endoscopy of the stomach is called fibroesophagogastroscopy. A similar procedure is carried out by inserting a special flexible endoscope into the stomach, which is a tube with a video camera and a light source at its end. As a result of this, the attending physician is able to visually examine the mucous membrane of the organ, as well as carry out a number of simple manipulations, such as a biopsy of the inner layer, microsurgical procedures (stopping bleeding, removing a polyp, etc.).
For examinations in children, there are special types of endoscopes that have a shorter length and smaller tube diameter.
An endoscopic examination of the gastrointestinal tract is carried out in a hospital setting after a clinical examination of the patient. This allows you to prevent the development of complications from the procedure and increase its information content for the doctor.
During esophagogastroduodenoscopy, a thin flexible endoscope tube with a small video camera at the end is guided in stages from the esophagus to the small intestine. Endoscopes equipped with a fiber optic system and lens transmit the image to an online monitor, which allows the doctor to immediately diagnose the condition of the subject. Then carefully remove the device.
Capsule gastroscopy differs in that instead of a probe, the patient swallows a plastic capsule containing a video camera (after 8 to 15 hours it is removed from the body naturally during bowel movements).
The duration of the procedure is determined individually. With local anesthesia, the manipulation time takes 5-10 minutes. With general anesthesia, the examination lasts about 30 minutes.
IMPORTANT! After endoscopy of the esophagus and stomach, it is not recommended to drink or eat for 30 minutes.
Gastric endoscopy is a procedure that requires preliminary preparation. The presence of food in the organ or muscle spasm will interfere with the examination.
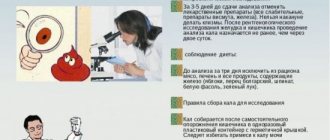
1. 3 days before the start, the patient must follow a slag-free diet.
To do this, the following are excluded from the menu:
- fresh vegetables, fruits, mushrooms, berries, nuts;
- Rye bread;
- fatty meat, fish and dairy products;
- salty, hot and spicy dishes;
- alcoholic and carbonated drinks.
Allowed to use:
- boiled or baked vegetables, lean meats and fish;
- light broths;
- wheat bread.
2. A day before endoscopy, you can eat liquid cereals, purees, and broths. Drinks include jelly, juices without seeds and pulp.
3. The last portion of food consists of broth and should be consumed no later than 10 hours before the procedure.
4. Before going to bed, it is advisable to perform an enema or use laxatives (bisad, laxbene, dulcolax). It is also recommended to take medications to reduce the amount of gas in the intestines (espumisan, disflatil, imodium).
5. 3 days before endoscopy, you must stop taking medications (with the permission of a specialist). It is especially important to exclude iron-containing products and activated carbon. These drugs may be mistaken for false bleeding.
On the day of the procedure, you are allowed to drink 50-70 ml of clean water. Breakfast, cigarettes and chewing gum are excluded. Tobacco and chewing products cause increased production of gastric juice and mucus, which will affect the result of the procedure.
In case of severe anxiety, the patient may be prescribed medications (diazepam, sibazon, relanium). Since worry and fear can provoke muscle spasms.
Anesthesia (local or general) is used according to the indications of the patient’s general condition. When using it, an initial examination is carried out to determine the tolerability of the drug and the state of the cardiovascular system.
Lidocaine is most often used for local anesthesia. It is sprayed onto the root of the tongue, this anesthetizes the process of guiding the endoscope tube and reduces the urge to gag.
The procedure is less painful for the patient.
General anesthesia is prescribed in extreme cases:
- if the procedure will be accompanied by taking material for a biopsy or coagulation of a damaged vessel;
- with severe nervousness and fear of the patient, which cannot be eliminated with medication due to drug intolerance;
- during the duration of the procedure or in patients with an unbalanced psyche.
General anesthesia is more convenient for a specialist, since he can calmly carry out the necessary manipulations. For the patient, the procedure may be burdened by the development of complications (impaired brain function, decreased vision and hearing).
Most often, endoscopy is performed using local anesthesia.
In this case, the procedure will take place in the following stages:
- An anesthetic is applied to the patient in a sitting position. After about 5 minutes, a feeling of numbness in the throat appears, which indicates the onset of anesthesia.
- The patient is placed on his side (usually the left). It is recommended to bend the right leg at the knees, and the patient should hug himself with his arms.
- To prevent damage to the endoscope tube by teeth, a “mouthpiece” is inserted.
- To prevent saliva from interfering with the process, it flows into a special bowl, located near the patient’s mouth, or a saliva drain is inserted.
- The specialist begins to insert the endoscope tube, while the patient must breathe through his nose and swallow at the request of the doctor. Otherwise, the tip of the device may get into the trachea.
- To ensure that the tube passes easily through the digestive tract and to improve visibility, air is periodically supplied.
- After examining the condition of the organs, the device is immediately removed. This process may be accompanied by gagging.
Endoscopy may be accompanied by abdominal discomfort. This is caused by the fact that the body tries to get rid of the foreign object on its own through contraction-pushing movements of the muscles. The examination procedure (without additional procedures) lasts 7-10 minutes.
Intestinal endoscopy
As you know, the intestine has several main sections: small, large and rectum. There is a separate method for conducting research in each department.
Colonoscopy
The endoscope is inserted through the anus, which helps to examine the entire inner lining of the large intestine. This examination is of great importance in the diagnosis of oncology and precancerous diseases (polyps). This method is also used for medicinal purposes - for the local treatment of various pathologies, for the removal of polyps and benign neoplasms.
Capsule endoscopy of the gastrointestinal tract
This diagnostic method appeared relatively recently and has not yet become widely known. Using a small capsule (about 2cm) with a built-in camera, doctors can examine the entire length of the small intestine. Unfortunately, so far only large clinics have such a device at their disposal.
Preparation for intestinal endoscopy
To minimize errors during diagnostics, you should follow a few simple rules.
Cleansing the intestines is important: a day before the endoscopy session, it is advisable to perform a cleansing enema or take laxatives.
A good help in preparing for this type of gastrointestinal endoscopy will be a special diet that excludes the following foods:
- thermally unprocessed vegetables, fruits and berries;
- cereals;
- greenery;
- legumes;
- dairy products;
- black bread.
In the days before the procedure, it is better to eat fish, dairy products, and chicken.
Contraindications to intestinal endoscopy
Contraindications include:
- severe ulcerative inflammation of the intestines
- possible perforation (through hole in the intestine)
- toxic megacolon (pathological enlargement of the colon).
As you can see, gastrointestinal endoscopy is an important diagnostic and therapeutic measure. Its type and appropriateness are determined by the attending physician!
Tavaluk Natalya, medical columnist
12, total, today
( 200 votes, average: 4.55 out of 5)
Blood test for tumor marker SCC (SCCA) - advantages and disadvantages of the study
About methods of radiation protection in medicine and false methods of removing radiation from the body
Related Posts
Preparation and performance of capsule endoscopy
Endoscopic examination of the esophagus and stomach
Gastric endoscopy is carried out in accordance with the available indications and contraindications, which must be taken into account for each patient. Indications include:
- Suspicion of benign or malignant tumor growth in the gastric wall.
- Finding the site of intragastric bleeding and the need to stop it.
- The need for a biopsy for differential diagnosis of similar diseases.
- Performing microsurgical operations, such as removing small polyps.
- Evaluation of the effectiveness of drug therapy against gastric and duodenal ulcers.
In addition to the indications, it is very important to consider contraindications to the procedure:
- Severe stenosis of the lumen of the esophagus, making it difficult to insert an endoscope.
- Decompensation of the patient’s somatic diseases (coronary heart disease with myocardial infarction, respiratory failure, etc.).
- Blood clotting disorders of various origins.
- Relative contraindications are convulsive syndrome and mental disorders in the patient.
If there are contraindications, it is necessary to refuse the procedure and choose other methods of examining the stomach (ultrasound examination, computed tomography, etc.).
Endoscopy can be prescribed by the treating specialist, the main purpose of which is to determine the condition of the organ.
1. For pain in the abdomen to identify the presence of pathology (ulcer, gastritis, colitis) and determine the state of severity.
2. If surgical intervention is necessary, the location and size of the lesion is determined.
Gastric endoscopy is performed for esophageal diverticulitis
| Contraindications | Relative prohibitions |
| Ulcer during exacerbation | Mental imbalance (depending on the severity of the pathology) |
| Cancers in the last stages | Increased presence of fat cells (obesity) |
| Pathologies of the pulmonary and cardiovascular systems, grade 1 and 2 | Severe exhaustion of the body |
| Recent heart attack or stroke | Inflammatory processes of the larynx and nasopharynx |
| Violation of the elasticity of blood vessels with the possibility of their damage with subsequent bleeding | Presence of HIV infection and jaundice |
| Critical patient condition | |
| Impaired functioning and circulation of the brain | |
| Presence of epileptic seizures | |
| Changes in the condition of the digestive tract, making it impossible to insert a tube | |
| Patient refusal to undergo examination |
3. To assess the dynamics of therapy, treatment can be adjusted based on endoscopy data. Or monitor the process of scarring of ulcers or sutures after surgery.
4. To detect internal bleeding in the presence of anemia of unknown nature.
5. If it is necessary to take tissue from the organ being examined for a biopsy.
Also, simple surgical interventions can be performed using endoscopy:
- stopping minor bleeding by cauterizing the damaged vessel;
- removal of a foreign object (small size) from the upper digestive tract;
- elimination of small tumors and neoplasms;
- preliminary preparation of the digestive tract before surgery.
Before prescribing endoscopy, the doctor must initially exclude existing contraindications or take into account the presence of relative prohibitions.
When the procedure is planned to be performed using anesthesia, the reaction to drug tolerance is additionally checked. The quality and capabilities of the endoscope determine how accurately the diagnosis will be made.
You can check the functioning of the digestive tract and identify the development of pathologies using video capsule endoscopy. To do this, the patient needs to swallow a capsule that contains a microvideo camera with a transmitter and a battery. The device is designed to operate for 8-14 hours.
Additionally, a special belt is put on the belt, to which the captured images are sent (their frequency is 2 frames per second). This procedure has pros and cons compared to the standard endoscopy method.
| Advantages | Flaws |
| The procedure is completely painless and does not cause discomfort. | Decryption takes from 2 hours. Images arrive for processing after 8 hours. The results of the examination can be obtained no earlier than one day after the start of the procedure. Standard decryption may take 3 days. |
| There is no risk of injury or infection. | While the capsule is in the body (20-24 hours), you should not eat food. |
| Allows you to check the functioning of the entire digestive tract, including the small intestine. | There is no way to take tissue for biopsy. Or immediately stop bleeding if it is detected. |
| There is no need to use anesthesia. | The movement of the capsule cannot be coordinated. |
| High-quality and clear photographs. | In rare cases, the capsule may become stuck. An endoscope will be required to remove it. |
During the procedure, physical activity is prohibited. The capsule leaves the body naturally. To speed up its release, it is recommended to take a laxative 8 hours after the start of the examination. Capsule endoscopy occurs in stationary conditions from the moment the capsule is taken until the signal to stop its operation. Usually after 8-14 hours.
Before using the capsule to examine the gastrointestinal tract, it is necessary to take into account the indications and contraindications for the procedure.
1. Indications for capsule endoscopy:
- abdominal pain of unknown origin;
- bowel dysfunction (constipation alternates with diarrhea without the presence of provoking factors);
- causeless weight loss;
- anemia of unknown nature;
- for examination of the small intestine and other organs of the digestive tract, the examination of which is difficult;
- if you suspect the presence of ulcers, benign or malignant tumors;
- the presence of hidden blood in the stool;
- to identify helminths;
- to monitor the dynamics of treatment.
2. Contraindications to capsule endoscopy:
- the presence of bleeding in the digestive tract;
- intestinal obstruction;
- impaired swallowing reflex;
- when carrying a child;
- presence of electronic devices in the body (pacemaker);
- violation of psychological balance;
- epileptic seizures;
- severe pathologies of the heart and lungs;
- poor blood clotting;
- the presence of perforation in the digestive tract;
- age up to 16 years and after 70.
If there are contraindications, they must be reported to the supervising specialist. Then a different diagnostic method will be selected.
Endoscopy of the stomach (this method is considered the best for diagnosing gastrointestinal pathologies), using a capsule, also requires preparation. The patient must give up heavy, difficult-to-digest foods 5 days before the procedure. And also from products that cause gas formation. A menu of products is followed, as in preparation for a routine endoscopy.
On the eve of the procedure, it is necessary to cleanse the intestines using an enema or laxatives. Consume only liquid foods. Last meal 12 hours before swallowing the capsule.
On the day of the procedure, it is recommended to drink 200-250 ml of water every 60 minutes. And try to be in an upright position, so the capsule will pass through the digestive tract faster.
After swallowing, the capsule enters the esophagus and then into the stomach, where it remains for up to 2 hours. Progress through the small intestine will last up to 8 hours. And the capsule can remain in the rectum for up to 14 hours. After which it is excreted along with the feces. Over the course of 8-14 hours, the camera in the capsule will take pictures and send them to a device on the belt. Next, specialists perform decryption.
After the procedure, the first meal is allowed after 4 hours, only liquid meals and after 8 hours full meals. If the capsule does not leave the body for more than 2 days, it is necessary to take an x-ray to detect and remove it.
The biggest cost of the procedure is the capsule itself. It also includes prices for consultation for preparation and interpretation of testimony.
| City names | Minimum cost (rubles) | Maximum cost (rubles) |
| Moscow | 15000 | 75000 |
| Saint Petersburg | 25000 | 80000 |
| Ekaterinburg | 31000 | 40000 |
| Permian | 30000 | 85000 |
| Novosibirsk | 29500 | 78900 |
| Volgograd | 28500 | 76700 |
| Sochi | 35000 | 77000 |
Gastric endoscopy allows you to more accurately determine the condition of the internal organs of the digestive tract, including the esophagus, stomach and duodenum. A complete examination of all gastrointestinal organs is possible using capsule endoscopy. But this procedure is more expensive.
What is endoscopy or endoscopic examination method
A whole group of instrumental manipulations that allow studying a specific organ belongs to endoscopic studies.
Endoscopy is performed using special devices - endoscopes (rigid metal or flexible plastic). In addition, modern endoscopy has invasive and non-invasive methods. The latter includes capsule diagnostics. To carry it out, the patient just needs to swallow a miniature video camera. When the capsule passes through the small intestine, it is possible to carefully examine this section, but this is not possible with classical research.
Instrumental and endoscopic methods are used for research, as well as for therapeutic purposes:
- Diagnostic. The cavities of the internal organs are examined to detect pathology or the presence of foreign bodies.
- Therapeutic. They allow you to administer medications, stop bleeding, remove tumors and remove foreign objects.
In addition, new endoscopic techniques such as virtual endoscopy are emerging. Special computer equipment recreates the image of the organ being examined on the monitor screen, allowing you to virtually move inside it, making the method similar to classical endoscopy.
Virtual endoscopy allows you to examine not only the condition of the stomach or intestines, but also large vessels and bronchi. But still, it cannot completely replace traditional examination, since it does not justify itself in cases of suspected early forms of cancer.
From this section you can learn how intestinal endoscopy is done and what kind of procedure it is.
Preparation:
- Before the procedure, exclude from the diet foods that cause increased gas formation: cabbage, peas, beans, bananas and other foods. On the day of the study, you should not eat or drink;
- cleansing enemas are done the day before and in the morning before the procedure;
- Instead of enemas, you can take the laxative Fortrans, Moviprep and others.
Carrying out a diagnostic procedure with the introduction of an endoscope through the oral cavity:
- An anesthetic spray is applied to the throat area of an adult;
- A mouthguard is placed in the oral cavity to prevent compression of the endoscopic tube;
- the patient lies on his side, swallows the probe, and as it moves, the doctor assesses the condition of the mucous membranes of the gastrointestinal tract;
- the probe is removed through the mouth.
Carrying out a diagnostic procedure with insertion of an endoscope through the anus. Patients often ask whether it hurts. The procedure is painful, so it is often performed under general anesthesia, but it can also be performed under local anesthesia. Algorithm:
- the patient lies on the left side or is in the knee-elbow position;
- First, a solid tip is inserted into the rectum, and then a flexible endoscope is inserted through it;
- After the examination is completed, the endoscope is removed.
An endoscopist performs examinations using an endoscope. An endoscope is the general name for an instrument for examining organs from the inside. It is equipped with a lighting system, optical system and camera. The name of the instrument and the examination itself vary depending on which organ the endoscopist is examining.
It is important to note that very often endoscopy is used as a way to get to the desired organ and conduct another study - X-ray contrast examination or catheterization (insertion of a thin hose to obtain fluid from the organ). If the purpose of endoscopy is to introduce a substance through the endoscope that “colors” an organ on an x-ray, then in this case the name of the study undergoes another change - the particle “scopy” is replaced by the particle “graphy,” which means “drawing” (the outline of a specific organ is drawn on the x-ray ).
For patients, endoscopy is not a very pleasant procedure, and they try to avoid it, agreeing to undergo even more expensive, but “comfortable” examinations. These tests include computed tomography (CT) and magnetic resonance imaging (MRI). Doctors often call CT virtual endoscopy, emphasizing that CT seems to replace endoscopy.
Studies performed by an endoscopist
| Study | How is it carried out? | What does it reveal? |
| Fiberoptic bronchoscopy | The particle “fibro” indicates that the study is carried out using a flexible fiber endoscope – fiberscope (fiber – fiber), which can “wriggle”. A fiber endoscope (for any organ) contains several separate channels - a channel for instruments, a channel for supplying liquid and insufflation (injection) of air, a channel for supplying light and a channel for transmitting images. Fiberoptic bronchoscopy is performed under local anesthesia. The bronchoscope is inserted through the mouth and trachea (which is why the study is often called “tracheobronchoscopy”). This does not affect the general act of breathing, since the bronchoscope is alternately inserted into each bronchus. Due to its flexibility, the fiber bronchoscope penetrates into the smallest bronchi and allows for biopsy and some medical procedures. Bronchoscopy allows you to inject a radiopaque substance into the bronchi and take a series of x-rays (bronchography). |
|
| Rigid bronchoscopy | The absence of a “fibro” particle means that the examination is carried out using a rigid endoscope. A rigid endoscope is a thin metal tube through which instruments can be inserted, as well as a flexible endoscope. Bronchoscopy with a rigid endoscope is performed under general anesthesia, while the bronchoscope is connected to a mechanical ventilation device (ALV). Rigid bronchoscopy also allows for biopsy, curative and minor surgical procedures. | |
| Fibroesophago-gastroduodenoscopy (FEGDS, FGDS) | FEGDS is the name for endoscopy of the upper parts of the digestive tract - the esophagus (esophagus), stomach (gaster), duodenum (duodenum). If the endoscopist is not interested in the esophagus, and he is going to examine only the stomach and duodenum, then a piece of “esophago” is omitted, and an FGDS (fibrogastroduodenoscopy) is obtained. For the study, a flexible endoscope (fibrogastroscope) is used. During the study, a biopsy and collection of the contents of the stomach and duodenum (bile, intestinal juice) can be performed for laboratory testing (acidity determination). In addition, modern gastroscopes allow you to enlarge the image 115 times (zoom endoscopy) or conduct an examination in the light spectrum and reveal what is not visible during a normal examination (virtual chromography). |
|
| Endoscopic retrograde cholangiopancreatography (ERCP) | Retrograde (in the opposite direction) cholangiopancreatography (cholangio - related to the bile ducts, pancreato - related to the pancreas) is an X-ray endoscopic examination. First, fibrogastroduodenoscopy is performed, after which the endoscopist determines the area of the major papilla in the duodenum and inserts a catheter through the endoscope. Through the catheter, a radiopaque substance enters the papilla and then into the bile ducts and pancreatic ducts. Immediately after the administration of radiocontrast, a series of x-rays are taken. |
|
| Thoracoscopy | Thoracoscopy is an examination of the pleural cavity using an endoscope (thoracoscope), therefore the second name of the method is pleuroscopy. The thoracoscope is inserted into the pleural cavity after puncture of the chest. During thoracoscopy, the pleura is inspected, material and fluid of interest are collected, as well as some medical procedures and operations. |
|
| Mediastinoscopy | Mediastinoscopy is an endoscopic examination of the mediastinum (the cavity that forms between the organs of the chest). The examination is performed under general anesthesia. The mediastinoscope is inserted through an incision in the dimple area on top of the sternum (jugular notch). This test allows for a biopsy of an enlarged lymph node or tumor. |
|
| Laparoscopy | Laparoscopy is an endoscopic examination of the abdominal cavity (lapara - abdomen). To examine the abdominal cavity, air or nitrous oxide is first pumped into the abdominal cavity through a needle. This is called “the imposition of pneumoperitoneum” (pneumo - air, peritoneum - peritoneum). The pneumoperitoneum allows organs to move apart and allows maneuvering of endoscopic instruments. Then one or more punctures are made in the anterior abdominal wall. A stent is installed into the hole - a round “mold” with several holes (a sort of “tee”), through which several instruments and a laparoscope (endoscope for laparoscopy) are inserted. During laparoscopy, a biopsy of the desired area can be performed. |
|
| Sigmoidoscopy | Sigmoidoscopy is an examination of the rectum and the initial part of the sigmoid colon using a rigid endoscope (does not bend, unlike flexible ones), which is inserted through the anus to a depth of 20 - 25 centimeters. A rectoscope allows you to examine the rectum through an eyepiece (as in old cameras) or on a monitor screen if the endoscope is equipped with a video camera. | |
| Colonoscopy | Colonoscopy (colon - large intestine) is performed using a flexible endoscope (colonoscope), which is inserted through the anus to examine the colon along its entire length to a depth of 1 - 1.5 meters. Particular attention is paid to the affected areas, which can be examined in different spectra and modes (enlarged image). |
|
| Intestinoscopy (enteroscopy) | Intestinoscopy is an examination of the small intestine using a thin tube and two balloons on it. The tube is inserted in the same way as a regular gastroscope and brought to the desired part of the small intestine. The endoscope is advanced by inflating and deflating the balloons, as a result of which the intestine is threaded onto the endoscope. The study is carried out under general anesthesia and x-ray control. |
|
| Capsule endoscopy | Capsule endoscopy allows you to examine the gastrointestinal tract without inserting a probe. The autonomous disposable capsule is equipped with a video camera, a light source and radio sensors. The patient swallows it, and the capsule moves through the digestive tract along with food and intestinal contents, transmitting 2 pictures per second to a recording device (the patient wears it on a belt throughout the day). |
|
| Endoscopic ultrasound examination | This study allows you to conduct an ultrasound examination using an endoscope, which acts as a conductor for the ultrasound sensor. The endoscope is inserted in the same way as during a conventional endoscopic examination into the digestive tract, rectum or bronchi. |
|
How to prepare for gastroscopy?
Before undergoing gastroscopy, you need to prepare for the procedure. And, first of all, consult a specialist (gastroenterologist):
- Based on your medical history, he will determine indications or contraindications for gastric endoscopy. If necessary, he will prescribe additional tests for FGDS;
- Determine the type of anesthesia based on the patient’s response to certain medications;
- The doctor will find out bad habits that may affect the outcome of the endoscopy;
- Prescribe a diet before the procedure;
- The doctor will warn you about symptoms that may occur after the procedure;
- He will answer all your questions (for example, is it painful to undergo an endoscopy).
Two to three days before the procedure, you should not eat spicy foods, smoked or fried foods. But lean meat, steamed, light soups with vegetable broths and porridges, on the contrary, are welcome. The bread should be slightly dry.
On the day of gastroscopy, if the procedure is scheduled for the first part of the day, you should not eat. And if it’s in the second half of the day, then you can allow yourself to have a snack, but no later than 6-8 hours before the test.
Particular attention should be paid to the drinking regime! Drinking is prohibited before the examination. And during preparation, alcohol, soda and coffee are excluded.
Without fear and doubt
And yet, no matter how you convince a person how important and necessary it is to undergo an endoscopic examination, many try to avoid it: to put it mildly, the procedure is not a pleasant one. It's time to forget about it! At the Institute of Plastic Surgery and Cosmetology, the patient is put into medicinal sleep - this is a type of anesthesia used to eliminate pain and discomfort during the examination.
The patient is injected into a vein with a special drug - unlike anesthesia, this anesthesia acts more gently and gently, plunging the patient into a controlled drug-induced sleep, without stopping breathing and is easily tolerated. The doctor clearly and quickly examines all the necessary areas and can accurately and accurately perform various diagnostic procedures.
Before an endoscopic examination with anesthesia, you must take blood and urine tests and do an ECG, and also tell the anesthesiologist about concomitant diseases and pathologies, the medications you are using, and tell them if you are allergic and to what exactly.
Indications and contraindications for capsule endoscopy
Endoscopy of the stomach (this process occurs with the preparation of a protocol) allows you to assess the condition of the examined organs. After it has been carried out, the therapist or gastroenterologist can prescribe therapy according to the examination data.
The examination report contains information:
- where, when and by which doctor the procedure was performed;
- Full name, age and gender of the patient;
- if anesthesia was used, what drug was used;
- general condition of the inspected organs. If there are pathologies, their characteristics and location;
- when additional manipulations are carried out (cauterization of a vessel, removal of a polyp), a description of them is made;
- conclusion of the specialist who conducted the inspection;
- recommendations for treatment and further examination. And also, if there is a need to repeat the procedure, then after what period.
When visiting a paid clinic, the examination results are kept by the patient and can be provided to any medical institution for treatment.
Endoscopy can detect the following changes in the digestive tract:
- inflammatory processes;
- disturbance of blood supply;
- benign and malignant tumor formations;
- changes in the condition of tissues and mucous membranes (ulcers, scars);
- dynamics of treatment of pathologies.
Any deviations are recorded in the examination results. The specialist conducting the treatment can prescribe therapy according to the data received.
During endoscopy, the esophagus, stomach and duodenum are examined.
At the conclusion of the examination, the specialist indicates:
- Are there any disturbances in the functioning of organs, if so, what kind;
- the presence of pathological narrowings, adhesions and scars;
- the condition of the walls of organs, their elasticity and motor activity;
- presence of abnormal mucus or fluid;
- existing changes from therapy, if the procedure was carried out to track the dynamics of treatment.
Using these data, the gastroenterologist can make an accurate diagnosis of the patient (gastritis, ulcer, tumor) and determine treatment. It is not possible to understand the examination results and select therapy on your own (without medical education).
The cost of endoscopy depends on the qualifications of the specialist, the modernity of the device used and the type of anesthesia. If there is video recording, the price also increases.
| City names | Minimum cost (RUB) | Maximum cost (RUB) |
| Moscow | 500 | 8000 |
| Saint Petersburg | 700 | 9000 |
| Ekaterinburg | 650 | 8990 |
| Permian | 600 | 8560 |
| Novosibirsk | 550 | 8150 |
| Volgograd | 490 | 7800 |
| Sochi | 520 | 8100 |
After the endoscopy, the examination result and a receipt with a full breakdown of payment are issued.
You must come to FGDS on an empty stomach
How to prepare for gastric endoscopy? It is necessary to consult with your doctor and get a list of recommendations. As a rule, serious preparation is not required due to the rapid examination, the absence of anesthesia and the easy tolerance of the procedure in most patients. However, there are a number of recommendations that prepare the patient for endoscopic examination of the stomach:
- The patient should not eat food 8-10 hours before the examination. This helps prevent the reflux of gastric contents into the esophagus and stomach, as well as reduce the risk of developing aspiration injuries.
- On the day of the study, the patient should not smoke cigarettes or other similar products.
- Before the procedure, you are allowed to drink only very small amounts of clean water.
Proper preparation for gastric endoscopy is the key to a highly informative procedure and its safety for the patient. If the study is planned to be carried out using general anesthesia, then the patient’s preparation for the procedure expands and includes a number of additional measures, such as the use of sedatives, etc.
An endoscopic examination of the stomach is carried out after proper preparation of the patient for the upcoming examination. After the patient is placed on the table, local anesthesia is administered to the oral cavity to suppress the gag reflex and facilitate the examination. If the patient is young, has mental illness, or is overly anxious, general anesthesia may be used.
The endoscope itself begins to be carefully inserted into the patient’s esophagus, moving it towards the stomach. Already at this stage, the attending physician begins to assess the condition of the mucous membrane, which can help identify various diseases and their complications, for example, gastroesophageal reflux disease. It is very important that when inserting the fiberscope, the patient breathes through the nose and swallows. This further reduces the gag reflex and facilitates the advancement of the device.
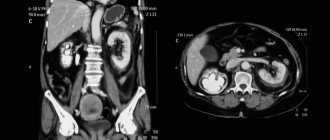
After the fiberscope is in the stomach, the attending physician begins to carefully examine the mucous membrane along its entire length. Areas of the inner layer with pathological changes are especially actively subject to examination: reddened, with plaque, with visible dilated vessels, etc. If necessary, the doctor can perform a biopsy of a suspicious formation or perform microsurgical intervention, for example, to remove a small polyp or foreign body.
If necessary, the doctor performs a biopsy
At the end of the procedure, the fiberscope is carefully removed, and the patient remains in the endoscopy room for 20-30 minutes to monitor his well-being. If during the endoscopy it was decided to undergo general anesthesia, the patient is transported to a ward, where he must be under medical supervision for 24 hours.
Peculiarities
The individual characteristics of the preparation should be explained by the doctor. We will just look at the main points.
- How to prepare for gastroscopy in the morning. Typically, the endoscopist begins the appointment around 9 am. Therefore, if you were prescribed the procedure in the morning, your last meal should be at 19-20 pm the previous day. Although it is recommended not to eat 8-10 hours before, the resulting gap is explained by the fact that after dinner you will go to sleep at night around 10 pm and have a good rest. If you have dinner at 12 am, healthy sleep will occur no earlier than 2 am.
- How to prepare for a gastroscopy in the afternoon. If the procedure is scheduled around 1-3 p.m. or in the evening, then a very light breakfast is allowed at 6-7 a.m. You should not eat food that coats the walls of the stomach, such as oatmeal. Limit yourself to a baked apple with a glass of weak tea.
- If a biopsy is planned. This procedure does not require a special approach. However, you should not take blood thinning drugs : aspirin (acetylsalicylic acid), warfarin, pentoxifylline, cardiomagnyl, rheopolyglucin, etc. You should avoid taking Citramon, as it contains not only caffeine, but also acetylsalicylic acid.
- If FGDS simultaneously with colonoscopy. This combination is called combined diagnostics. It is performed only under anesthesia. Preparation begins 4 days before the study: diet described earlier; fasting for 12 – 14 hours before the procedure; Avoid drinking an hour before diagnosis; on the eve of the study, Fortrans or an enema is prescribed.
For patients with diabetes and bronchial asthma
Do not use nebulizers before the procedure, as they may stimulate the formation of bronchial secretions. Take your inhaler with you. Patients with diabetes must agree in advance on the exact time of the procedure , since insulin intake depends on this. If the procedure is in the morning, the patient does not eat, but takes food with him. You should also take insulin with you. After the procedure you should eat. When performing fibrogastroduodenoscopy during the day, the patient has breakfast and receives a dose of insulin according to his usual schedule. Then the procedure is carried out after 4-5 hours.
What to expect after gastroscopy?
Thanks to anesthesia, the person does not cough or feel the urge to vomit. Breathing is not difficult and attacks of suffocation are excluded, since the endoscope does not block the airways.
The main thing is to mentally prepare for the procedure, then a calm state will not lead to spasm of the gastrointestinal tract muscles, and the examination will be easier for both the patient and the doctor.
If gastroscopy is performed correctly, then, as years of practice have shown, the patient does not experience any discomfort after the procedure. The only thing you may feel is some discomfort in the throat and a slight soreness. But these symptoms disappear within 24 hours.
Endoscopy of the stomach, in very rare cases, can cause complications - these are:
- damage to tissue integrity as a result of tube advancement. In severe cases, bleeding may occur. At the same time, abdominal pain appears, and general health quickly deteriorates;
- numbness of the throat, which makes swallowing movements worse. After 24-36 hours, functioning is restored;
- allergies to medications used;
- reflux of vomit into the respiratory system;
- increased flatulence;
- infection due to poor disinfection of the drug;
- pain in the digestive tract along the route of the tube.
If you have severe pain in the abdomen or difficulty breathing after the procedure, you must immediately contact the nearest medical facility. To prevent bleeding or mucus getting into the lungs.
Restrictions to the procedure
It helps to carefully examine the mucous membrane from the inside. But there are several restrictions. There are absolute contraindications in the form of:
- severe stricture of the esophagus;
- nodular goiter grade 3-4;
- diseases of the digestive canal in combination with hemophilia;
- angina pectoris in a calm state;
- heart failure of the 3rd degree against the background of gastrointestinal diseases;
- acute stroke;
- acute myocardial infarction with rhythm disturbance.
If the patient has had a heart attack, stroke, or other pathologies are discovered, then the procedure can be performed only after 3-4 weeks.
There are also relative contraindications in the form of:
- mental disorder;
- history of epilepsy;
- glaucoma;
- acute inflammatory processes that affect the tonsils, bronchi, and larynx.
Endoscopic examination of the stomach should not be performed on people suffering from tuberculosis, HIV or infectious jaundice.
What are the possible complications of gastroscopy?
When examining the gastrointestinal tract using a capsule, in rare cases it gets stuck in the intestine due to obstruction.
And also with depletion of blood vessels or erosions, the device can provoke bleeding. Elimination of bleeding or removal of the capsule can be done surgically or using standard endoscopy.
Possible complications during endoscopy of the stomach and duodenum include perforation (perforation) of organ walls and bleeding caused by trauma. But such side effects are extremely rare.
As a rule, gastroscopy is performed once a year. But if pathologies are detected, the gastroenterologist prescribes this examination individually, depending on the severity of the disease.
Any medical procedure can lead to complications, and gastric endoscopy is no exception. It is important to note that if you follow the rules for preparing the patient and following the rules for conducting the examination, the risk of complications during fibroesophagogastroscopy is minimal. However, the following negative consequences may occur:
- The use of medications for local or general anesthesia can cause the development of various allergic reactions: Quincke's edema, urticaria, anaphylactic shock, etc.
- Violations of the integrity of the mucous membrane of the esophagus or stomach with the development of erosions. With excessive mechanical impact from the endoscope, their walls may rupture with the development of mediastinitis or peritonitis.
- Intragastric bleeding of varying severity.
- If the patient is not properly prepared and general anesthesia is used, aspiration syndrome may occur with the development of pneumonia.
- Heart rhythm disturbances of varying severity.
If such complications develop, the procedure must be stopped and therapeutic measures initiated (stopping bleeding, using medications, etc.).
FGS usually resolves without complications
Endoscopy of the stomach is the “gold” standard for diagnosing gastric diseases. In this case, the method can be used to identify and determine the severity of such ailments as peptic ulcers, acute and chronic gastritis, various types of tumors, etc. The minimal invasiveness of the procedure and short duration allow endoscopic examination to be widely used in clinical practice. At the same time, the risk of complications remains minimal in all age groups of patients.
Indications for endoscopy of the esophagus and duodenum
Gastroscopy is prescribed if any disease of the gastrointestinal tract is suspected, for example:
- gastritis;
- stomach and duodenal ulcers
- acute or chronic pancreatitis ;
- diseases of the esophagus;
- bleeding;
- cough of unknown etiology.
- examine the lesions to assess the result of treatment ;
This procedure, during which you can also :
- stop the bleeding;
- remove polyps in the stomach;
- remove stones from the cavity of the major duodenal papilla;
- take a piece of tissue for cell research ( biopsy );
- inject drugs into the affected area;
- remove foreign body .
The essence and purpose of the study
Endoscopy is the most informative method for determining the type and location of pathologies (compared to ultrasound, X-ray, MRI). The endoscope used for the procedure consists of an elastic fiberglass tube, at one end of which a camera, a flashlight and an air supply element are installed. On the other side there is an eyepiece.
During an endoscopy, a specialist can visually assess the condition of the organ (through an eyepiece or on a monitor screen), take photographs and record the procedure. Simple surgical interventions can also be performed (cauterization of a damaged vessel, tissue sampling for examination), for this purpose biopsy forceps are additionally attached to the endoscope.
The purpose of the procedure is to detect or exclude pathologies:
- inflammatory process, polyps or tumor formations;
- vascular damage, erosion and ulcers;
- change in organ size;
- tracking the dynamics of treatment to adjust treatment.
After the endoscopy, the patient receives a conclusion and photographs (if the process was recorded, this is also given to him). Based on examination by a gastroenterologist or therapist, therapy is prescribed.
Features of stomach examination in children
For abdominal pain of unknown origin, children are also prescribed an examination using an endoscope. Since gastrointestinal pathologies at an early age can develop more rapidly than in adults. Therefore, timely diagnosis and treatment are required.
For manipulations, more flexible tubes of smaller diameter are used (selected according to age and diameter of the hole in the larynx). The anesthesia used depends on the age parameters.
For infants under 2 months of age, any use of anesthetics is strictly contraindicated. From 3 months to 7 years, the procedure is performed under general anesthesia. Since the child’s reaction to endoscopy is unpredictable.
From the age of 7, it is allowed to use local anesthesia, after careful psychological preparation and explaining to the child the rules of behavior during the procedure.
If necessary, 30 minutes before the manipulations, children may be prescribed potent sedatives. The child is under the supervision of a specialist until the anesthesia or sedative wears off.
How is endoscopy done?
The technique of endoscopic examination differs in each clinical case. This is due to the characteristics of the organ being examined, the goals of endoscopic diagnosis, the age category and general health of the patient, as well as the type of endoscopic equipment.
In many cases, to make the procedure more comfortable for both the patient and the doctor performing it, anesthesia is performed during endoscopy. When the procedure is performed without anesthesia or under local anesthesia, the patient experiences quite unpleasant sensations when the endoscope is inserted. Different types of diagnostics use their own specific anesthesia technique.
Colonoscopy or endoscopic surgery is performed under general anesthesia (mask), and during examination of the upper digestive tract, the patient’s airway should not be obstructed. If anesthesia is used during the procedure, patients are more willing to agree to it, because they know that in this case endoscopy is not painful.
How often can endoscopy be done?
Gastric endoscopy is a safe procedure (provided it is performed by a qualified specialist and if all rules are followed). The frequency is determined by the treating specialist.
If surgical manipulations or therapeutic treatment were carried out, then at the end of the course a repeat procedure may be prescribed. Sometimes examinations are prescribed several times during the treatment process. To track dynamics or, if necessary, adjust treatment.
. For preventive purposes, if there is a predisposition to gastrointestinal pathologies, then endoscopy is performed at intervals of 12 months. In the presence of chronic diseases, the procedure is repeated every 4-6 months.
Concept of gastric endoscopy
Gastric endoscopy is a diagnostic procedure. Using this technique, you can carefully examine the mucous membrane of the internal organ. During the examination, the doctor takes tissues and sends them for histology. The doctor also often removes small formations.
The procedure is carried out using an endoscope. This is a thin tube that is made of fiberglass. At its end there are optics, a small camera and a magnifying device. Thus, it is possible to completely examine the walls of the organ. Diagnostic activities last from 3 to 10 minutes. If material is being collected, it will take a few more minutes. When removing benign tumors, it takes up to 30-40 minutes.