Conditions are needed for nutrition and breathing
Microbiologists now know that each pathogen needs its own “native” environment, taking into account its pH, redox potentials, viscosity, humidity and osmotic properties.
Media can be soft and hard, simple and complex, universal and not very universal, but in all cases they must provide nutrition, respiration, reproduction and growth of the bacterial cell. Some media (thioglycolate, Sabouraud) are suitable for a wide range of microorganisms and are called universal. Others are intended only for certain species, for example, pneumococcus and Staphylococcus aureus, which produce hemolysins, grow on blood agar, which serves to isolate particularly “capricious” and, at the same time, dangerous strains. Thus, there are many types of media, where each of them grows its own range of microorganisms.
Screening children for intestinal infections
Tests for intestinal infections in children show the amount of normal and pathogenic flora. These include stool and blood tests.
Examination of a child's stool is carried out by bacteriological determination of the type of pathogen. To do this you need:
submit feces for analysis to a laboratory; it is important to collect feces in a special container; if the child has diarrhea, you can donate a small amount of feces; You should not give your child an enema before collecting material.
The day before the pick-up, you should not give your children laxative products. You also need to avoid taking antibiotics and enterosorbents.
The results of a stool test in children may be as follows:
- a large number of lactobacilli;
- absence or presence of pathogenic flora.
Blood tests in children have their own characteristics. They are due to the fact that normal values for a child differ from those for an adult
This is important to understand when assessing the results
A general blood test for intestinal infections will show leukocytosis, ESR is higher than normal. An increased number of leukocytes indicates an inflammatory process. The higher this level, the more active the process.
Serological testing in children is also based on the determination of immunoglobulins.
An intestinal group test is prescribed for children in the following cases:
- symptoms characteristic of intestinal infections;
- in contact with a sick person;
- to determine the pathogen and prescribe adequate therapy.
Intestinal infections are a group of microbes that require properly selected treatment and timely diagnosis
Therefore, it is important to conduct laboratory tests to identify the type of microbe. Correctly selected treatment prevents the development of serious complications
Analysis of stool and blood for the intestinal group is an important and necessary type of diagnosis.
What information is obtained from the analysis?
In laboratory conditions, the composition of feces is assessed by the content of beneficial and pathogenic and opportunistic organisms. Due to various factors, the flora loses the necessary bacteria, and the volume of pathogenic flora increases.
Analysis is necessary for the following symptoms:
- diarrhea, constipation;
- flatulence;
- discomfort or pain in the abdomen;
- intolerance to certain foods;
- intestinal infection;
- allergy;
- skin rash;
- disruption of intestinal biocenosis;
- long-term therapy with anti-inflammatory drugs.
What does a stool test for dysbacteriosis show?
Stool culture is often prescribed for newborns at risk and adolescents suffering from regular allergies and acute respiratory viral infections.
In addition to the presence of symptoms, a doctor may refer a patient for testing for many reasons:
- rickets, anemia in children;
- consequences of an intestinal infection, which was accompanied by bloody diarrhea;
- hormone therapy;
- weak immune system;
- taking antibiotics.
Newborns whose mothers have mastitis or vaginitis and infants whose stay in the maternity hospital exceeded certain standards are also sent for analysis.
Breast with mastitis
A referral for testing is issued by a gastroenterologist, infectious disease specialist or therapist. The patient is required to collect the material correctly in order to obtain reliable results.
What pathogenic microorganisms are most often detected?
A patient with an acute digestive disorder and suspected infection is sent to an inpatient infectious diseases department. Children are hospitalized together with their mothers. In a hospital setting, it is possible to isolate the patient and conduct the most complete examination and treatment.
The most common intestinal pathogens are manifested by the following diseases:
- Dysentery - caused by Shigella, the main “blow” is dealt to the stomach and large intestine. The pathogen is characterized by good adaptability to environmental conditions. They live in garbage and feces for up to two months. A person gets the infection through dirty hands or contaminated food.
- Salmonellosis - the favorite site of infection is the small intestine. The disease is accompanied by severe intoxication. For young children it is especially dangerous because it causes severe complications (pneumonia, meningoencephalitis, general sepsis). Pathogens are divided into types, except for salmonellosis, typhoid fever is caused by infection through the fecal-oral route, through insufficiently processed foods, and dirty water.
- Coli infections are diseases caused by E. coli of different serotypes. Occurs more often in infants. Affects the large intestine. They are transmitted from carriers or sick adults if the basic rules of hygiene and baby care are not followed.
These examples show how important it is to timely analyze not only feces, but also food, drinking water, and swabs from the hands of personnel. Especially if the disease is detected in children's institutions
What is included in a stool test for the intestinal group and what microorganisms are detected most often?
Among the most detected bacteria are the following:
- Bacteria of the dysentery group that cause shigellosis (dysentery) is an acute infectious disease that has a fecal-oral route of infection. It affects the large intestine and causes symptoms such as diarrhea, abdominal pain, fever, blood and pus in the stool.
- No less dangerous are bacteria of the typhoid-paratyphoid group. These include the causative agent of typhoid fever - Salmonella typhi and the causative agent of paratyphoid fever - Salmonella paratyphi A, B, C, as well as causative agents of other salmonellosis. The pathogen is transmitted fecal-orally and mainly affects the gastrointestinal tract. Observed symptoms: vomiting, nausea, cramps, bowel dysfunction, fever. With typhoid fever, damage to the central nervous system may occur in the form of lethargy and impaired consciousness.
- Pathogenic E. coli are the cause of escherichiosis, an acute infectious intestinal disease that mainly affects children. Among pathogenic Escherichia coli, those leading to cholera-like diarrhea are distinguished, causing diarrhea mainly in children, leading to dysentery-like diarrhea and the presence of blood in the stool.
The presence of pathogenic microorganisms and their sensitivity to antibacterial therapy can be determined using a microbiology method such as cultivation on nutrient media.
What does UPF reveal?
It is designed to detect elements such as staphylococcus, streptococcus, Klebsiella and other equally dangerous microorganisms. But in addition to harmful microorganisms, it also includes the presence of beneficial bacteria
Particular attention is paid not only to their presence, but also to their quantity
| Bifidobacteria | Beneficial inhabitants, their optimal amount should consist of at least 95%; a decrease in its amount to 10*9 degree means the presence of dysbacteriosis. | Their purpose is to ensure proper functioning of the intestines. |
| Lactobacilli | A good indicator is their presence is about 5%. If this percentage decreases, constipation will appear, caused by a lack of lactose. | Designed to produce lactic acid, which helps normalize intestinal function. |
| Escherichia coli | Occupies 1% of microflora. If the indicators are lower or higher than normal, it indicates dysbacteriosis and worms. | Prevents the proliferation of opportunistic microorganisms, absorbs oxygen, thereby ensuring the existence of bifidobacteria and lactobacilli. |
| Coccus bacteria | The optimal ratio reaches 25%. An increase in the ratio indicates a violation of the microflora and the possible development of infection in the genitourinary system. | They are always present in the intestines. |
| Hemolytic Escherichia coli | Normally it is not available. If present, indicates the presence of disturbances in the microflora. Provokes the appearance of skin problems and allergies. | It is a competitor of bifidobacteria and latcobacteria. |
| Staphylococcus aureus | Should not be detected. The appearance of even a minimal amount can cause vomiting and diarrhea. | They can appear due to a decrease in good microorganisms in the microflora. |
| Pathogenic bacteria | They are harmful, and due to their appearance, an infectious disease develops. Under normal conditions, they may still be present, but have a sluggish form. | When analyzing stool for dysbacteriosis, they are the first in the result list. |
It is worth noting that it is with the help of the UPF that the exact type of bacteria that provokes the development of infection is determined.
Decoding the results
More than 400 species of bacteria live in the intestines. Approximately 20 of them are of clinical significance. The analysis result form indicates the main microorganisms and their quantity per 1 g of biomaterial. Unit of measurement – CFU/g.
Normal bacteria
Main article: Normal (useful) representatives of intestinal microflora
Microorganisms of this group make up up to 98% of all intestinal bacteria. They are involved in the digestion of food, the synthesis of vitamins, and inhibit the growth of pathogenic microflora. Normal bacteria are included in probiotic preparations, which are prescribed to correct dysbiosis.
- bifidobacteria – 108 – 1010;
- lactobacilli – 106 – 108;
- typical E. coli – 106 – 108.
We recommend reading:
Stool analysis for calprotectin: what does it show and how to take it?
Opportunistic bacteria
Main article: Representatives of opportunistic intestinal microflora
Conditionally pathogenic flora are present in feces in small quantities. Bacteria break down food components and stimulate the immune system. Exceeding permissible limits disrupts the functioning of the digestive tract and provokes allergic reactions.
- lactose-negative E. coli – no more than 105;
- bacteria of the genus Proteus – no more than 102;
- enterococci – 106 – 107;
- yeast-like fungi – no more than 104.
Pathogenic bacteria
Main article: Representatives of pathogenic intestinal microflora
These microorganisms cause infectious diseases. In healthy people, there are no pathogenic bacteria in the stool.
- salmonella;
- shigella;
- Staphylococcus aureus;
- Pseudomonas aeruginosa;
- hemolytic Escherichia coli.
When a pathogenic microorganism is identified, its type and sensitivity to bacteriophages and antibiotics are indicated.
To distinguish true dysbiosis from short-term dysbiotic reactions, stool cultures are prescribed twice with an interval of 1 week. With persistent changes in the intestinal microbiocenosis, the results of both analyzes will be the same. The doctor will compare the data obtained with clinical manifestations and determine further tactics for managing the patient.
In continuation of the topic, be sure to read:
- Bacteriological culture (tank culture) of feces: essence, preparation and analysis
- How to take a stool test for intestinal microflora?
- Stool analysis for UPF: preparation, delivery and interpretation
- How to take a stool test for the intestinal group?
- Taking a stool test for dysbacteriosis + interpretation
- Analysis of stool for disgroup: essence, preparation and delivery of analysis
- Preparing and submitting a stool test for dysbacteriosis in infants
- Escherichiosis: details about the infectious disease
- Klebsiella in the intestines: danger of bacteria, symptoms and treatment (drugs, diet)
- Intestinal microbiota: what is it and how to check its condition?
The role of gut bacteria
The realization that there are myriads of colonies of microscopic bacteria living inside is amazing. Many are accustomed to the fact that microbes are foreign agents against which a constant struggle is waged. It turns out that humanity would not have survived without such invisible creatures.
Let us list the functions of the intestinal microbiota:
- are a “second stomach” - they participate in the digestion of incoming food;
- take part in the exchange of bile;
- synthesize biologically active substances and vitamins;
- protect the inner surface of the digestive tract by producing mucus;
- regulate the motility of the stomach and intestines;
- prevent the penetration of obviously dangerous bacteria, viruses, fungi;
- cleanse the intestines of toxins.
Large-scale studies are being conducted confirming the amazing role of intestinal bacteria in protecting the body from diabetes, atherosclerosis, and autoimmune diseases. Healthy microflora prevents the development of allergies and cancer pathologies.
Examination of stool for intestinal infections
The test for determining pathogenic flora is carried out using serological, bacteriological and microbiological methods. Initially, microscopy of the material is performed. That is, the pathogen in the native preparation is assessed under a microscope. However, this is only possible after several days of infection.
In accordance with the results of microscopy, it is determined which nutrient medium the material will be sown on. To do this, use special cups with a medium containing substances for microbial growth. Conditions are created for their development, then the morphological properties are determined.
This will allow the doctor to accurately prescribe therapy.
How to prepare for the analysis?
Before the study you should not use the following drugs:
- iron-containing;
- bismuth tripotassium dicitrate;
- various enterosorbents, for example, activated carbon;
- laxatives;
- broad-spectrum antibiotics.
It is advisable to stop taking it a week before the test.
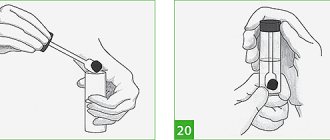
Your doctor will tell you in detail how to get tested for intestinal infections. But you should know the following features of collecting stool for analysis and what it includes:
- Only sterile containers should be used for research;
- there are special containers with a small spoon for easy collection;
- if you were unable to purchase such a container at the pharmacy, you can take an ordinary jar, after boiling it;
- It is better to collect feces in the morning;
- It is advisable to deliver the material to the laboratory immediately after collection;
- before collection, wash the external genitalia, this will reduce the risk of erroneous results;
- It is not correct to collect material from the toilet; you need to prepare the container in advance;
- In no case should you use an enema before collecting stool, as this will provide false negative results.
A stool test for intestinal infections is prepared within 5 days. This period is determined by the growth of the microorganism and its identification.
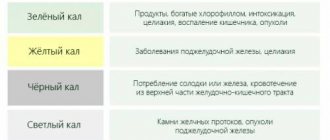
The results of the study may be as follows:
- The microflora is represented by bifidobacteria and lactobacilli. These microbes are normal inhabitants of the human body and do not pose a danger.
- E. coli is also a natural representative of the flora. But its content is insignificant. But do not forget that with a decrease in the local immunity of the mucous membranes, it can cause dysbiosis.
- Representatives of pathogenic flora may also be encountered in the analysis. These include:
- salmonella;
- shigella;
- Klebsiella;
- Proteus.
The intestines are 90% populated only by bifidobacteria. The presence of pathogenic microbes will cause gastroenteritis.
In the results form, a plus is placed opposite the column for a certain type of microbe if it is present, a minus if it was not detected. When determining resistance, a group of antibiotics and the level of sensitivity to it are written next to each type. The more advantages, the less resistant the microbe is to the antibiotic.
Stool culture for pathogenic intestinal flora is the main condition for effective treatment of intestinal infections
Symptoms of acute intestinal infections caused by pathogenic microorganisms manifest themselves in the form of nausea, fever, diarrhea, and abdominal pain. In severe cases, dehydration occurs and dangerous complications develop. The presence of pathogens can be detected, as well as their sensitivity to antibacterial drugs can be determined by stool culture for the presence of pathogenic intestinal flora.
In the laboratory, microorganisms are grown on nutrient media.
Purpose of analysis
The main goal pursued by a doctor when prescribing a bacteriological examination of stool is to establish the true cause of pathological processes in the intestines. The choice of treatment tactics that guarantees the patient’s complete recovery depends on the result of the analysis. By inoculating stool for pathogenic flora, the presence of pathogenic microorganisms is detected, which excludes the development of the disease for other reasons.
Established deviations from the norm, which confirm the infectious nature of the pathology, eliminate the need for additional diagnostic measures. The doctor has the opportunity to formulate antimicrobial therapy on an individual basis, taking into account the results of the study. Bacterial seeding is prescribed for:
- diagnosis of acute intestinal infections;
- pathogen identification;
- determining an effective drug for therapy;
- evaluation of treatment results.
Actually, stool culture for flora is a microbiological study of human biological material, performed in vitro (outside the patient’s body) in laboratory conditions. The raw materials presented for analysis are placed in a special nutrient medium. Biological materials are kept in special conditions at a certain temperature for a certain time necessary for the growth of microorganisms.
The identified pathogenic flora serves as material for the next stage of diagnosis - an antibiogram. Thanks to the antibiogram, the degree of sensitivity of dangerous microorganisms to the effects of bacteriophages and antibacterial drugs is established.
Object of study
For a healthy person, colonization of the intestines with yeast-like fungi, bifidobacteria, bacteroids, E. coli, cocci, and lactobacilli is the norm. Together they form a unique microflora that contributes to:
- strengthening the wall of the large intestine;
- protecting the colon from harmful influences;
- decomposition of fiber from food;
- synthesis of biologically active substances;
- production of substances that ensure normal functioning of the immune system.
The selection of colon contents required for culture of pathogenic intestinal flora has sound reasons. The small and large intestines are divided into a certain number of subsections with characteristic microflora. The composition of the microbiota of the small intestine adjusts bile and gastric juice. Bile and stomach acids, as well as enzymes, allow only a small number of microorganisms to exist in the small intestine. In the large intestine, a completely different picture is observed, allowing the microbiota to be defined as:
- aerobic and anaerobic (needing and not needing the presence of air);
- specializing in a certain type of broken down substance (for example, preolytics are responsible for protein conversion);
- beneficial, opportunistic and pathogenic.
The normal composition of the microbiota involves the proximity of every hundred bifidobacteria cells with one lactobacilli cell, a dozen E. coli cells, and one cell of another microorganism (for example, enterococcus). The degree of activity of each type directly depends on the state of the body.
Standards are approximate only and may vary depending on age and lifestyle
Deviations from the norm cause:
- allergic reactions;
- acute respiratory diseases;
- oncological and infectious diseases;
- age;
- working conditions;
- nutritional features.
Culture results
The performed bacterial culture reveals the presence of truly harmful bacteria belonging to the dysentery and typhoparatyphoid group, or bacteria belonging to the opportunistic pathogenic flora (UPF). Interpretation of the results confirms or refutes the presence of pathogenic microorganisms. The growth of intestinal pathogenic bacteria involves determining sensitivity to the effects of antibacterial drugs.
If the transcript does not show the growth of microorganisms that are part of the normal intestinal flora, the result of the analysis cannot be interpreted as negative. The data obtained indicate a low titer of dangerous bacteria affecting the growth of normal microbiota. A repeat study will be required to clarify. Also, the transcript of the analysis may be accompanied by a comment indicating an increase in the number of microorganisms of opportunistic intestinal flora.
The analysis is deciphered by a laboratory assistant
Additional Research
If the culture result for pathogenic flora is negative, a stool test for UPF is required if there are complaints about:
- unstable chair,
- flatulence,
- feeling of discomfort in the abdominal area,
- pain,
- allergic reactions to certain products.
The analysis is also carried out when there are symptoms of an intestinal infection or treatment has been carried out using hormonal and anti-inflammatory drugs. Newborns at risk and children who often suffer from acute respiratory infections also need such a study.
The name UPF (conditionally pathogenic flora) covers bacteria that are present in the gastrointestinal tract and have a positive effect on the vital activity of the entire human body until conditions are formed that promote a pathological increase in the number of microorganisms. Enterobacteriaceae, staphylococci, and some types of Escherichia coli are called conditionally pathogenic. A smaller amount of UPF is detected in the child’s stool. In older people, quantitative indicators increase significantly.
A colony of staphylococcus bacteria under normal conditions is not dangerous to humans
If the norm is not exceeded, conditionally pathogenic microorganisms perform a number of functions important for the body. Thus, enterococcus, which enters the child’s body with mother’s milk, helps reduce the number of conditionally pathogenic bacteria in the microbiota. In addition, enterococcus in the intestinal microflora is:
- synthesis of vitamins;
- normal absorption of sugar;
- breakdown and processing of carbohydrates;
- strengthening the immune system.
Long-term illnesses, surgical interventions, use of antibacterial drugs for a long time, an increase in quantitative indicators exceeding the permissible threshold (for enterococcus this is 100 million in 1 gram of test feces on the UPF) are conditions that contribute to the degeneration of a beneficial microorganism into a pathogenic one.
Enterococcus can cause the development of chronic gastritis, enteritis, bacteremia, various pathologies of the genitourinary system, and meningitis.
Timely diagnosis, in the presence of characteristic symptoms, helps prevent complications. Thanks to seeding for conditionally pathogenic and pathogenic intestinal flora, the doctor is able to identify disturbances in the microbiota with maximum accuracy, identify the pathogen and select the appropriate drug for therapy.
Rules for collecting biomaterial for analysis
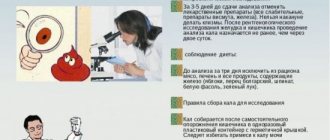
The results of stool flora testing directly depend on compliance with the rules of preparation for the test. The reliability of the results will be maximum if:
- Stop taking any medications at least three days before collecting biomaterial.
- At least twelve hours passed from the moment of stopping taking antibiotics to the moment of collecting stool for analysis.
- Do not collect stool after an enema or after taking a laxative.
- When defecating, make sure that urine does not get into the feces.
- Take the material for research with a clean spoon and place it in a clean, dry container.
- Collect stool immediately before delivery to the laboratory. The interval between the time of collection and delivery cannot exceed three hours.
Timely contact with a specialist and laboratory testing in the early stages of the disease will allow you to obtain the most accurate results, determine the correct diagnosis and prescribe appropriate therapy.
probakterii.ru
How to get tested?
To obtain reliable results, the patient should first be prepared:
- It is recommended not to eat meat dishes for 4–5 days, not to drink alcohol, to eat only dairy products, cereals, potatoes, white bread;
- three days before collecting stool, stop taking antibiotics, laxatives, iron supplements (one can assume in advance a negative result in patients who independently began treatment with antibiotics), and administering rectal suppositories.
Collection rules include:
- prevention of foreign impurities (urine, blood during menstruation in women) entering the test material; the child should be given the opportunity to urinate first; women should use a clean vaginal tampon if the analysis cannot be rescheduled;
- containers for the material being tested cannot be treated with disinfectants (bleach); the jar must be washed thoroughly with soap and poured with boiling water;
- the baby's potty is treated in the same way;
- No more than two hours are allowed for delivery to the laboratory; storage in the refrigerator allows for a 4-hour delay; the longer the delay in transportation, the less effective the data obtained will be, since some of the pathogens die.
The analysis is taken:
- at home - in a sterile container, the volume should be approximately a full teaspoon;
- in the infectious diseases room or in the hospital, a rectal smear is taken with a swab, with the patient in the lateral position, the laboratory assistant inserts a sterile swab on a stick into the rectum to a shallow depth and turns it, then immediately places it in a test tube with a special medium;
- For a small child, you can take the material directly from the diaper.
A prescription filled out by a doctor is attached to the container.
Decoding indicators
To evaluate the results of the analysis, it is important not only the presence of certain microorganisms in the feces, but also their quantity, therefore the research form always indicates the content of identified bacteria and the acceptable values for this indicator. The doctor who sent you for a stool test should understand these numbers. It is he who should ask all questions based on the results, and not engage in self-diagnosis and self-medication.
Bifidobacteria
Normal content of bifidobacteria in the stool of people of different ages
Reasons for the decline:
- Treatment with antibiotics.
- Diseases of the digestive organs.
- Poor nutrition.
- Chronic stress.
- Immunodeficiency states.
Lactobacilli
Norms by age
A decrease in the number of these microorganisms in feces can be caused by recent antibiotic therapy, disruption of the functioning of the digestive tract, as well as colonization of the intestines by pathogenic bacteria.
E. coli
Normal E. coli content in a stool sample
E. coli are very sensitive to the effects of antibiotics and high acidity; under the influence of these factors, the number of microorganisms in the feces can be significantly reduced.
Bacteroides
Normal indicators
A decrease in the amount of bacteroids in feces can be associated with serious errors in nutrition and the use of antibacterial drugs.
Enterococci
Normal content in feces
A decrease in the number of enterococci occurs due to long-term treatment with antibiotics, disorders of the pancreas and chronic stress.
A disruption of the normal balance between microorganisms in the digestive tract is most often accompanied by unformed stools, grumbling, pain and bloating, and nausea. Mucus and undigested pieces of food appear in the feces, and the smell of stool changes.
Opportunistic and pathogenic microorganisms
An increase in the number of opportunistic bacteria to 10 4 is considered acceptable. This indicator is the same for all age groups. There should be no pathogenic microbes in the stool at all. If they appear and there are some clinical signs (repeated diarrhea, fever, nausea and vomiting), the doctor diagnoses an infectious disease - salmonellosis, etc.
Composition and functions of intestinal microflora
Intestinal flora is a collection of beneficial and opportunistic microorganisms. Their purpose is to digest food, produce vitamins, stimulate the immune system, suppress the growth of pathogenic bacteria, and strengthen the colon wall.
- Normal microflora includes enterococci, Escherichia coli, bacteroides, lacto- and bifidobacteria.
- Opportunistic flora are represented by Klebsiella, Proteus, some staphylococci, Pseudomonas aeruginosa, yeasts, and Citrobacter. They are found in the large intestine in small quantities and are activated when the immune system is weakened and the number of beneficial microorganisms decreases.
- Pathogenic intestinal bacteria detected using this test include Salmonella (the causative agent of salmonellosis) and Shigella (the causative agent of dysentery).
The correctness of collecting stool and submitting it for analysis to a medical institution
To carry out the analysis correctly and obtain reliable results, it is necessary to collect stool under certain conditions, namely:
- A few days before collecting stool, it is necessary to stop taking any medications, especially antibiotics, as they can affect the test results;
- It is also forbidden to take laxatives, because stool collection is carried out after natural bowel movements;
- It is forbidden to collect feces after an enema, as it washes away the real concentration of microorganisms;
- During the collection of feces, it is necessary to prevent urine from entering along with feces, which may give incorrect readings in the transcript itself;
- Feces must be collected in a pre-prepared, sterile container using a special spatula, which is included in the kit. Such medical containers can be purchased at any pharmacy or you can disinfect your own jars. In this case, the container must be filled with feces, only one third;
- After collecting stool, it is necessary to deliver the finished container within 3 hours to the laboratory itself. If this is not possible, then you should put the container with feces in the refrigerator, but for no more than 9 hours.
It is better to carry out analysis at the earliest stages of the disease, when the concentration of microbes is much higher, which will facilitate a qualitative analysis. A referral for such an analysis is issued by a general practitioner. Such an extract must be attached to the container itself with feces. This analysis will be carried out over 5 days, due to the fact that the existing bacteria will be sent to a nutrient medium, where they will be inoculated. After the growth of colonies of microorganisms, an analysis will be carried out to determine what type of bacteria these bacteria belong to.
Rules for collecting biomaterial for analysis
The main nuance of collecting feces for this analysis is the ideal cleanliness of the dishes, namely their sterility. Because only in this case can one count on maximum reliability of the results.
So, for collecting biomaterial, a sterile container for collecting feces, which can be bought at any pharmacy, is best suited. This container is an ordinary plastic jar, which is hermetically screwed on with a lid with a built-in spatula for collecting feces. This container is sterile, so there is no need to open it unless necessary.
If for some reason it was not possible to buy a container, a glass jar with a tight-fitting lid (for baby food or mayonnaise) will also do. It must be thoroughly washed and boiled. To do this, place a waffle towel on the bottom of a small pan, place a jar on it and fill it with water so as to completely cover it. Thus, the jar needs to be boiled for 5 minutes. After this, it is taken out, placed on a clean towel and set aside until completely dry.
It is better to collect feces in the morning. First, you should empty your bladder and wash your external genitalia with water (without soap). Defecation should not occur in the toilet, but in a clean container prepared in advance. From there, take 1-2 tsp. feces into a container.
The biomaterial should be delivered to the laboratory within 8 hours after collection. It should be stored in the refrigerator at a temperature of 6-8 degrees. The collected biomaterial cannot be frozen! An enema cannot be used to obtain stool. Feces should be obtained only naturally. You will also have to postpone the stool test for the intestinal group for 2 days in the case of an X-ray examination of the gastrointestinal tract or the use of a cleansing enema.
Before collecting biomaterial, it is strictly forbidden to take:
- iron-containing preparations;
- Activated carbon;
- any laxative medications;
- preparations containing bismuth;
- suppositories with a fatty base.
Do not allow urine or water to get into the stool sample being analyzed. Women will also have to wait to get tested during their menstruation.
Interpretation of the obtained analysis results
The results obtained are entered into a special form, where the required number of bacteria is indicated in the columns. The transcript itself describes the presence of both beneficial and pathogenic bacteria, the presence and quantity of which describes the condition of the entire gastrointestinal tract. Only a qualified doctor can describe the decoding, who can accurately determine whether the presence of a particular bacterium in the human body is harmful. Microflora may consist of the following bacteria:
- Bifidobacteria, which make up about 95% of all intestinal microflora. At the same time, normal functioning of the intestines is not possible without the presence of this type of bacteria;
- Lactobacilli are also representatives of normal intestinal microflora, but their number does not exceed 5%;
- E. coli with normal concentration and correct enzymatic activity is present in every person from birth. The main condition for good functioning of the intestines is that the amount of such E. coli must be within the normal range, otherwise there is a danger of dysbacteriosis;
- The presence of coccal bacteria, which include all types of staphylococcal, streptococcal and enterococcal microbes;
- Staphylococcus aureus is one of the representatives of pathogenic bacteria; if its concentration increases, a person may experience allergic reactions or decreased immunity;
- Hemolyzing E. coli is very dangerous to human health, so even the smallest amount of it is unacceptable in the intestinal microflora;
- Pathogenic bacteria, there are a very large variety of such bacteria, so only with the help of analysis can one determine the specific causative agent of the infection.
The analysis of stool for intestinal microflora is very similar to the analysis for dysbiosis, because during its implementation, the presence of both harmful and beneficial bacteria in the human body is checked in the same way.
The state of the child’s intestinal microflora is determined. Why might a doctor prescribe such a test and what should parents know about it?
Stool analysis for dysbacteriosis: explanation | How to get tested for dysbacteriosis
Dysbiosis is a change in the composition of bacteria that are found in the intestines or on the skin. Symptoms of the disease are diarrhea, abdominal pain. In order to make sure that a person has intestinal dysbiosis, a stool test is performed.
Five days before donating stool, you must go on a special diet prescribed by your doctor. Otherwise, the analysis results may be distorted. The use of medications and laxatives, including enemas, is completely excluded. When treating with antibiotics or bacteriophages, the period before analysis should be at least 3 weeks.
For the sample, a glass container or a special container is taken for analysis; the feces must be fresh, in an amount of up to 10 grams. The material for research is collected in a container (if it is a glass container, it must be boiled for 10 minutes for sterilization) and the sample is delivered to the laboratory within 3 hours.
From the laboratory that analyzed stool for dysbacteriosis, a transcript is issued after 5-7 days in the form of a form, where all of the above indicators are indicated.
A qualitative analysis for dysbacteriosis is done within 3 hours using certain equipment and under sterile conditions - not every laboratory can afford expensive equipment, and therefore, when receiving a referral from a doctor, it is worth asking him which laboratory performs such an analysis.
How to test your child for dysbacteriosis?
The question about children's testing for dysbacteriosis is legitimate due to the characteristics of the child's body and the microflora of his intestines. In a child, the microflora is more unstable and can change under the influence of a large number of factors, which does not always make it possible to accurately determine the occurrence of dysbacteriosis. For this reason, the doctor may offer other diagnostic methods: bacteriological examination of intestinal scrapings, biochemical analysis of stool, or another type of study. Only after receiving correct and complete information that confirms the diagnosis, appropriate treatment is prescribed.
Treatment is based on eliminating the cause that caused dysbiosis. Doctors who may be involved in the procedure for prescribing treatment
- pediatrician,
- allergist,
- gastroenterologist
- and infectious disease specialist.
Why is it important to get tested for dysbacteriosis in a timely manner?
Opportunistic microflora causes disruption of the normal functioning of the intestines under certain conditions and competes with normal microflora, displacing them and populating the intestinal walls - this causes disruptions in the functioning of the entire digestive tract.
A timely analysis for dysbiosis allows you to determine the cause of the disease and provide adequate treatment. Various allergies, gastrointestinal disorders, and metabolic disorders can be caused by dysbacteriosis.
Interpretation of the results of stool tests for dysbacteriosis
The intestinal microflora in the intestine is divided into
- pathogenic microorganisms
- and opportunistic.
Stool tests may reveal:
1.
pathogenic microorganisms,
2.
total amount of E. coli,
3.
Escherichia coli with mild enzymatic activity,
4.
Escherichia in stool analysis for dysbacteriosis (Escherichia coli with normal enzymatic activity).
5.
And also lactose-negative enterobacteria, coccal forms of microbes in total, hemolyzing Escherichia coli, lactobacilli, bifidobacteria, bacteroides (not always), dental bacteria, enterococci, clostridia, peptostreptococci, Staphylococcus aureus, saprophytic and epidermal staphylococci.
6.
Other conditionally pathogenic microorganisms: Klebsiella, Enterobacter, Graphnia, Serration, Proteus, Morganella, Providence, Citrobacter.
7.
non-fermenting bacteria: pseudomonas, acinobacter.
The remaining microorganisms are representatives of the normal composition of the human intestinal microflora, the number of which must be within certain limits. A change in their quantitative or percentage ratio means that there is a disruption in the process of microorganisms and their interaction. The change may also indicate the presence of dysbiosis as a disease, or act as a symptom of the presence of non-bacterial parasites (if the analysis indicates Escherichia less than 107-108 - this is a clear sign of worms or protozoa that absorb oxygen).
Pathogenic indicators of stool tests for dysbacteriosis
Pathogenic microorganisms cause various changes in the balanced system of interaction of microorganisms, which disrupts the correct and stable functioning of the intestines and the entire body as a whole. Improper functioning of the intestines causes various diseases of the digestive tract, skin, blood, and metabolism is also disrupted.
Pathogenic microbes in stool analysis include:
- enterobacteria,
- bifidobacteria,
- lactobacilli (lactic acid microbes, lactobacilli, lactic streptococci),
- Escherichia (Escherichia coli with normal enzymatic activity),
- Escherichia coli with reduced enzymatic activity, bacteroids.
The presence of pathogenic enterobacteria (in the stool test for dysbacteriosis, salmonella, shigella or other pathogens of acute intestinal infection) indicates a serious intestinal disease caused by a certain type of bacteria.
Pathogenic microorganisms cause an acute intestinal infection, which indicates a serious infectious intestinal disease and the need for appropriate treatment. They should not be present in tests in a healthy body.
Opportunistic indicators of stool tests for dysbacteriosis
Opportunistic indicators in stool analysis for dysbacteriosis include:
- lactose-negative enterobacteria (Klebsiella, Proteus, Citrobacter, Hafnia, Enterobacter, Serration),
- various cocci,
- hemolyzing Escherichia coli,
- clostridia.
Conditionally pathogenic indicators of intestinal microflora become pathogenic when certain conditions occur: an increase in their indicator in quantity or as a percentage of normal microflora, a decrease in the effectiveness of the body’s defense or immunity.
With dysbacteriosis caused by an increase in the content of opportunistic microorganisms, allergic skin reactions may occur. And also there is a violation of the stool, vomiting, bloating, abdominal pain, but the body temperature is normal.
Stool test standards
1.
Bifidobacteria are responsible for normal intestinal function and a decrease in the indicator, the norm of which is 107-109, indicates severe dysbiosis.
2.
Lactobacilli produce lactic acid, which is important for normal intestinal function. The normal value should be no lower than 106-107.
3.
Escherichia in stool analysis is responsible for the barrier protection of the intestinal microflora from colonization by foreign microbes, and a downward deviation of the 107-108 norm often indicates the presence of non-bacterial parasites in the intestine.
4.
The presence of E. coli with reduced enzymatic activity in the analysis indicates the beginning stage of intestinal dysbiosis.
5.
The role of bacteroids has not yet been clarified and their presence is not critical.
www.astromeridian.ru
What tests are performed for dysbacteriosis?
In modern medicine, three methods are used to study the stool microlandscape (analysis for dysbiosis) - two main and one auxiliary. This is a bacteriological study (stool culture tank), biochemical analysis of stool for dysbacteriosis (express analysis) and scatology.
Scatological analysis
Scatological studies of feces are basic, primary. This is an additional method that provides general diagnostic data about the condition and functioning of the intestine. Scatological analysis is carried out in two ways. This:
- Macroscopic - they evaluate the remains of undigested food, the color of feces, its smell, shape, consistency, and see if mucus, fat (soap), and other components are present in the feces.
- Microbiological (microscopy) - evaluate digested food, muscle fiber cells, digestible and indigestible plant fiber, and the remains of various tissues.
Bacteriological analysis of stool
If scatology in an adult’s stool shows a deviation from the required values, a specialist may prescribe a stool test for dysbacteriosis. Stool analysis is performed in a bacteriological or wide-range medical laboratory, where stool is cultured for dysbacteriosis.
How long does it take to test for dysbacteriosis? This is a fairly long-term study. The analysis can take at least six days or even more to prepare.
First, the material under study is “seeded” in a bacteria-rich environment. The microorganisms grow for at least four days, then the laboratory assistant counts them.
When submitting stool for bacteriological examination, the data is calculated in colony-forming units per gram of material - CFU/g. All obtained values are recorded in a special form.
Analysis of stool for dysbacteriosis using a biochemical method
Biochemical or gas-liquid chromatographic analysis of feces for dysbiosis is a fairly new technique that became widespread at the beginning of the two thousandth. It is considered more advanced and informative than taking stool for a culture tank. In addition, the results of this study will be ready within a few hours.
In biochemistry, intestinal dysbiosis is determined by the spectrum of fatty acids, which are products of the vital activity of bacteria. If you examine the stool for a microscape using this method, this will not only reveal quantitative changes in the microbiota, but also determine in which parts of the intestine the balance is disturbed.
In addition, it is much easier to get tested for intestinal dysbiosis using a biochemical method. The collected feces do not have to be immediately brought and examined, as with bacteriological diagnostics. It can be frozen and stored in the freezer for a day.
Stool culture for analysis
Bacteriological examination of stool is an important procedure, especially for those patients who suffer from stomach diseases, including children. With the help of bacteriological analysis of stool, including that of a child, it is possible to identify information that will tell about the state of health of the child or adult, the characteristics of their digestive system and other points. It is known that fecal matter is undigested food debris that contains many elements and various microorganisms. Also, stool with stomach disease may contain other components, for example, blood, mucus or parasites. Bacteria in a child’s stool will help determine the condition of his body and begin treatment in time if necessary.
How to take the test correctly?
Preparation
Preparation for the study is as follows:
- In stopping antibacterial treatment. After completing the course of antibiotic therapy (and it must be completed), at least 5-7 days should pass.
- Following a diet that will help relieve if you have a tendency to constipation. You cannot do enemas, insert rectal glycerin suppositories into the anus, or take laxatives to obtain material for analysis.
- In purchasing a sterile container for feces and, if the container is not equipped with a special spatula, a sterile spatula. All this can be found in pharmacies.
Collection of material
Features of collecting material for research:
- Stool collection must be carried out on the day of delivery to the laboratory (not in the evening).
- Before going to the toilet, you should carry out hygiene procedures.
- Defecation should be natural - into the toilet (if its design allows for the collection of material), into a bedpan or into a clean plastic bag.
- Feces must be collected into the container with a spatula or spatula from different places (if there is mucus or blood, be sure to grab these areas).
- For research, 5-10 g of material (the volume of a teaspoon) is sufficient.
Features of analysis in children
There may be a problem with collecting material for research in children in the first months of life, since their feces are most often liquid and are completely absorbed into the diaper. In such situations, you can bring a diaper to the laboratory - the laboratory assistants themselves will extract feces from it. However, to avoid any problems, it is better to find out in advance from the medical institution the rules for collecting material from a small child. Otherwise (in preparation, delivery times, storage conditions) there are no special features.
Analysis of stool for coprogram
Stool analysis for coprogram is also called stool analysis for scatology or general stool analysis.
A general stool test is prescribed if the patient has complaints about:
- diarrhea;
- constipation;
- flatulence;
- pain in the abdominal area;
- in case of disruption of the digestive system.
An analysis for coprogram is not carried out for preventive purposes; it is done if there are suspicions of disturbances in the functioning of the gastrointestinal tract.
What does a general stool analysis show?
According to the study, it is determined:
1. The presence of bile pigments (stercobilin) in the stool.
2. The work of the digestive glands. The result of the study consists of the number of crosses placed around:
- neutral fat;
- muscle fibers;
- digestible fiber;
- fatty acids;
- starch.
The number of “pluses” indicated as a result of the analysis informs about the process of food digestion. A large number of them in the analysis indicates a disturbance in the digestive process.
3. Inflammatory intestinal process, which is detected when present in the stool:
- pus;
- mucus;
- blood.
These pathologies are also marked with crosses.
4. Increased number of leukocytes. Normally they are found in small quantities.
5. Red blood cells. Normally, they should not be present in feces.
6. Intestinal epithelium. It should also not be present in the material being studied.
7. Helminths. Neither the parasites themselves nor their eggs should normally be detected in a general stool analysis.
A medical report can be obtained the next day after submitting stool for coprogram. If at the time of the test the patient is taking medication, the doctor must be informed about this. Since certain medications affect the test result, for example, antibiotics, enzymes, laxatives, etc.
Types of analyzes
If dysbiosis is suspected, the gastroenterologist prescribes a general or biochemical stool test. Both methods will give a detailed view of the state of the intestinal microflora. The collected material is examined in an equipped laboratory.
After the required period, laboratory assistants count the colonies of bacteria that have developed in a beneficial environment. Stool testing makes it possible to assess the sensitivity of microorganisms to bacteriophages and antibiotics. Verification is carried out in two ways.
If dysbiosis is suspected, the gastroenterologist prescribes a general or biochemical stool test
Bacteriological analysis
Testing stool for microflora in a standard way involves observing excrement over several days. During the testing process, laboratory technicians determine the ratio of microorganisms.
The standard method allows you to get results 7-10 days after the analysis is submitted to the laboratory. This time is necessary for the bacteria to grow and their numbers can be seen under a microscope.
Inoculation of fecal material on a nutrient medium
Information from bacteriological test analysis is not always accurate due to the influence of the following factors:
- When collected, stool comes into contact with air, which leads to the death of anaerobic microorganisms. As a result, the amount of harmful and beneficial flora is calculated incorrectly.
- The general microflora should include mucosal bacteria that live on the intestinal mucosa. This element is not included in the bacteriological analysis of stool.
- Diagnostic accuracy reduces the time spent transporting stool to the laboratory. Part of the microbial flora dies during transportation.
Attention! It is not allowed to collect material for analysis if the bowel movement occurred as a result of taking laxatives.
Video - Examination of stool for dysbacteriosis
Biochemical analysis
This research method is more accurate and provides complete information about the state of the intestinal flora. Thanks to the speed of verification, the patient is quickly prescribed appropriate treatment, without wasting time and aggravating the situation. Information can be obtained within a couple of hours after the material is transferred to laboratory technicians. Feces intended for biochemical testing can be frozen and donated at any time.
The principle of biochemical analysis is as follows: all bacteria produce fatty acids during their life. Many of them can be formed by only one type of microorganism. Having determined the type of acids, we can draw a conclusion about the presence of microorganisms in the gastrointestinal tract, as well as which section is populated by pathogenic flora.
Biochemical analysis of stool for dysbacteriosis
An additional advantage of the method, in addition to the speed of obtaining results, is the complete identification of all types of microorganisms, including those located near the walls of the organ.
Decoding the received data
A healthy child does not have pathogenic microorganisms in his stool, i.e. the analysis must be negative for disgroup and salmonellosis, as well as for dysenteric amoeba and typhoparatyphoid group. Normally, such simple microorganisms as intestinal trichomonas and balantidium are absent.
A UPF test will tell you how many of these bacteria are in 1 gram of feces. Low values of enterococci, clostridia, candida and bacteroides are considered a negative result, because For the development of infection, a certain amount of the pathogen is necessary, and not just its presence. If opportunistic microflora prevails over the concentration of lactobacilli in the feces, this is dysbacteriosis.
If an intestinal group is detected, the analysis is supplemented with a test for the sensitivity of bacteria to antibiotics.
Antibiotic sensitivity is indicated by the following letter designations
- S - sensitive (h);
- R - stable, resistant (y);
- I - moderately stable (yy).
Sowing methods
To isolate pure cultures of pathogens, the first stage is to inoculate them on appropriate media, which is carried out under special (sterile!) conditions. Basically, the transfer of material to the medium is carried out using devices used back in the 19th century by the great Louis Pasteur:
- Bacterial loop;
- Pasteur pipette;
- Glass rod.
Of course, many instruments have undergone changes over 2 centuries, replaced by sterile and disposable plastic ones, however, the old ones have not remained in the past, continuing to serve microbiological science to this day.
The first stage of obtaining colonies requires compliance with certain rules:
- Sowing is carried out over an alcohol lamp in a box pre-treated with disinfectants and quartz treatment, or in a laminar flow hood, ensuring sterility in the work area;
- The health worker's clothing, gloves and environment must also be sterile, since the opposite interferes with the isolation of isolated strains;
- You need to work quickly but carefully in the box; you cannot talk or be distracted; at the same time, you must remember about personal safety, because the material can be infectious.