Typhoid fever is part of the group of acute intestinal infections, has a cyclical course and affects the lymphoid tissue of the small intestine. The name of the disease includes the word typhus (translated as fog or smoke), which in ancient times meant diseases that occurred with clouding of reason, hallucinations and delirium. In Russia, diseases accompanied by brain damage were called fever.
In the 19th and early 20th centuries, typhoid fever was one of the most common and severe infections throughout the world, especially in cities (crowded population, lack of sanitary and hygienic standards). Epidemics of typhoid fever occurred during periods of war, natural disasters, and famine. To date, a high incidence of typhoid fever has been registered in developing countries (30 – 70 cases of the disease per 100 thousand population).
Source of infection
The source of typhoid fever is a person (anthroponotic infection), you can get infected from a patient or a bacteria-excreting person. An infected person releases the bacteria into the environment through urine and feces, and less commonly through saliva or milk.
- Until the seventh day of illness, the infectious agent is released in small quantities.
- Massive release of bacteria begins at the end of the first week,
- and reaches its maximum at the height of clinical manifestations.
- Bacterial excretion lasts no more than three months, but in 3–5% it becomes chronic either with feces (more often) or with urine (the most dangerous in epidemiological terms).
How is it transmitted?
The transmission mechanism of the abdominal type is fecal-oral. A person can become infected (transmission routes) through:
- consumption of infected food, water
- or by contact and household means.
Outbreaks and epidemics of typhoid fever are caused by the use of water from a polluted reservoir.
Typhoid fever is a fairly contagious infection; it affects people aged 15 to 40 years, but infants also have a risk of becoming infected from their mother through breast milk.
Seasonality
Typhoid fever is a seasonal infection; the maximum number of cases is registered in the summer-autumn period, which is associated with:
- activation of transmission routes (water, food);
- optimal conditions in the environment where the pathogen is perfectly preserved and reproduces;
- seasonal changes in the human body (decreased reactivity under the influence of ultraviolet radiation, decreased acidity of gastric contents, high consumption of plant fiber, which leads to alkalization of the gastrointestinal mucosa and its irritation).
After an illness, stable and often lifelong immunity is formed. But due to the widespread use of antibiotics to treat patients with typhoid fever, which suppress the immune system, acquired immunity has become less intense and longer lasting. Therefore, the frequency of re-infection with this infection has increased.
Typhoid fever: symptoms, tests, pathogen, treatment and prevention
What it is?
Typhoid fever is a long-term infectious disease with a multi-stage, cyclical course, the distinctive features of which are inflammation of the lymphatic tissue and mucous membrane of the small intestine with the formation of specific ulcers, dangerous for the development of intestinal bleeding and perforation.
A characteristic sign that appears at the height of the disease is the involvement of the central nervous system and the development of specific retardation (stupor), as well as fogging of the patient’s consciousness with a violation of spatiotemporal orientation. The last symptom is characteristic of a severe course.
The population's susceptibility to typhoid fever is high - the risk of getting sick is especially pronounced in people aged 15 - 40 years. The minimum risk is observed in children under 2 years of age.
The causative agent of typhoid fever, routes of infection
salmonella - the causative agent of typhoid fever, photo
Typhoid fever is an infectious disease caused by Salmonella typhi, which belongs to the family of intestinal bacteria. This is an anthroponotic infection, i.e. a person is necessarily involved in its transmission, and infection occurs from a healthy person.
Typhoid fever is associated with sanitary and hygienic standards - if they are not observed, the risk of being infected increases tenfold. This occurs due to the release of bacteria from the body of the sick person in feces and urine.
There are three main routes of infection:
- Water – the danger is posed by the use of water from reservoirs, industrial water from enterprises. This path is the most common. Its risk increases in the summer (when swimming in open water bodies characterized by poor sanitary conditions);
- Food - it should be taken into account that the bacterium is well preserved and multiplies in milk and meat. Therefore, these products require heat treatment;
- Contact, realized through household items contaminated (contaminated) with pathogenic microorganisms.
Typhoid fever can cause an epidemic. Most often, it is caused by the use of a certain group of people from the same source of water, for example water from a well. Rapid elimination is possible only when a source of infection is detected and disinfected.
Most infections with typhoid fever occur in the summer and autumn. Salmonella entering the body will not necessarily lead to the development of disease.
This is explained by the fact that on the way the bacteria encounter protective barriers in the form of hydrochloric acid produced in the stomach and intestinal lymph nodes.
In these organs, the microorganism can be successfully eliminated, so the pathological process will not develop.
But if these barriers are not strong enough or the infection is very massive, then the bacteria become fixed in the lymphoid tissue of the small intestine, where they actively multiply. This stage of the disease (incubation) does not manifest itself clinically and lasts from 3 to 21 days. But there may be various fluctuations in the duration of this period.
A shorter incubation period is associated with the transmission of the pathogen through food, in which they are already actively reproducing. A longer incubation period is observed when infected by water or contact.
After this period, Salmonella from the intestinal lymphatic system enters the blood, causing bacteremia. This moment marks the initial stage of the disease - the person begins to experience symptoms of typhoid fever. They force him to see a doctor.
How does infection occur?
The causative agent of typhoid fever is the bacterium Salmonella typhi, which is part of the intestinal Salmonella family. The bacterium does not stain for Gram (Gram-negative), but is motile due to many flagella. The typhoid bacillus grows well on nutrient media containing bile. When bacteria die and destroy, endotoxin is released, the action of which causes the symptoms of the disease.
The typhoid bacillus is highly resistant when released into the external environment. The infectious agent remains viable in soil for 1 to 9 months, in water for up to a month, and in human feces for up to a year. In dairy products, typhoid bacteria not only persist, but also multiply (from 1 to 3 months), on fruits/vegetables for up to 10 days, and in meat, butter and cheese up to 120 days. The typhoid bacillus easily tolerates freezing, but when boiled and treated with chemical disinfectants (chloramine, sublimate, phenol, Lysol) they die within a few minutes.
Infection with this disease occurs when microorganisms enter the oral cavity and then into the digestive tract. The pathogen, bypassing the first physiological barriers (hydrochloric acid in the stomach, intact intestinal mucosa), goes through several stages of circulation throughout the body, which constitute the mechanism for the development of the disease:
- Implementation phase
Beginning of the incubation period. Some of the bacteria that enter the intestine are released out with feces, and the rest begins to penetrate the lymphatic formations of the small intestine, from where it travels through the lymph vessels to the regional (mesenteric) lymph nodes, and then to the retroperitoneal ones.
- Phase of lymphangitis and lymphadenitis
Lasts 7–21 days and corresponds to the end of the incubation period. Having penetrated the lymphatic system and lymph nodes, bacteria begin to actively multiply, and their accumulation in the lymphoid tissue of the small intestine causes the development of an inflammatory process (lymphadenitis and lymphangitis).
- Bacteremic phase
Corresponds to the first seven days of the disease and coincides with the end of the incubation period. After inflammation develops in the intestinal lymph nodes, the multiplied bacteria enter the common lymphatic thoracic duct, and from it into the bloodstream.
- Intoxication phase
Some of the microbes that have entered the bloodstream die, which leads to the release of endotoxin, which has a toxic effect on the body: a disorder of thermoregulation, disorders of the central and autonomic nervous system (depression of consciousness, stupor, delirium), the functioning of the heart and other vital organs.
- Phase of parenchymal dissemination of bacteria
The causative agents of typhoid fever are carried through the bloodstream to various organs and tissues, but most of the microbes settle in the lymph nodes, bone marrow, spleen and liver, where typhoid granulomas are formed. The appearance of exanthema (skin rashes) is caused by the introduction of bacteria into the vessels of the skin and the development of inflammatory reactions in them.
- Phase of release of typhoid bacillus into the external environment
The bile-hepatic system plays the main role in the isolation of microbes. From the bile ducts, the pathogen enters the intestines with the flow of bile, and then with feces into the environment.
- Allergic reaction phase
Not all microorganisms that enter the intestines again are excreted with bile. The remaining part is reintroduced into the intestinal lymphoid tissue, which has already been sensitized during the initial invasion. Due to the existing sensitization, the inflammatory reaction becomes hyperergic in nature and proceeds with the development of necrosis and ulceration.
- Immunity formation phase
At the same time, immunobiological protection is activated, aimed at removing microbes from the body and forming immunity. In the clinical course of the disease, this phase corresponds to recovery.
Typhoid fever: causes, symptoms
Typhoid fever is an infectious disease with a fecal-oral transmission mechanism, which is characterized by a cyclic course with fever and intoxication, damage to the lymphoid apparatus of the small intestine, and enlargement of the liver and spleen.
The disease is registered everywhere. It is characterized by a peak incidence in the summer-autumn period. The population's susceptibility to typhoid fever is quite high. It is most common in countries with high population density and low levels of sanitary culture. Military conflicts and natural disasters contribute to an increase in the incidence rate.
In the past, typhoid fever was widespread, severe and had a high mortality rate. Currently, thanks to the capabilities of modern medicine, the incidence rate has decreased tenfold, its course has become less severe and less often leads to the development of complications.
Causes
The causative agent of the disease is the bacterium Salmonella typhi. Infection occurs through food, water or household routes.
The causative agent of the disease is Salmonella typhi. This is a small, mobile, gram-negative rod that does not differ in morphological structure from other Salmonella. Its features are:
- complex antigenic composition;
- presence of endotoxin;
- biochemical activity;
- ability to form L-forms.
It is stable in the environment.
- Under favorable conditions, this microorganism can survive in soil and water for up to several months.
- Tolerates freezing well.
- Remains viable for a long time (up to 10 days) on vegetables, fruits, and household items.
- In some food products, such as milk, minced meat, jelly, salmonella can multiply, causing foodborne infections.
However, the microorganism quickly dies when heated and exposed to conventional disinfectants.
Routes of infection
The source of infection is a sick person or a bacteria carrier who releases salmonella into the environment through feces and urine. Of particular danger are asymptomatic carriers who lead an active lifestyle and remain undetected for a long time.
In patients, the maximum bacterial excretion is observed at the 3rd week of illness, but can continue during the period of convalescence for several weeks or months. In some cases, recovered individuals become chronic carriers of the infection for many years or even for life.
A healthy person can become infected with typhoid fever in the following ways:
- water (contamination of water supplies with wastewater, malfunction of the water supply system, violation of the water purification regime);
- food (when consuming food products contaminated with salmonella);
- household (through household items and dirty hands).
Mechanisms of disease development
In order to cause a disease, the pathogen must enter the human body in high concentration (over 10 million microbial cells). Once in the stomach, some of the bacteria die under the action of gastric juice, and some penetrate into the intestines. The latter is facilitated by:
- decreased acidity of gastric juice;
- disturbance of intestinal microflora;
- weakening of the immune system.
From the intestinal lumen, infectious agents penetrate into the lymphatic follicles and with the lymph flow into the mesenteric (mesenteric) lymph nodes, where inflammation develops and active proliferation of the pathogen is observed. All this occurs during the incubation period without causing symptoms.
At the next stage, salmonella overcome the lymphatic barrier and enter the blood. In this case, some of the bacteria die (due to phagocytosis and immune defense factors) and release the endotoxin contained within them. Its action is associated with:
- intoxication;
- damage to the cardiovascular system;
- neurological disorders.
The more massive the bacteremia, the more severe the disease.
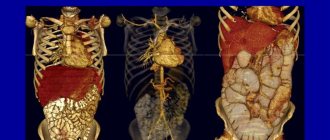
As the pathological process progresses, the pathogen spreads throughout the body and inoculates internal organs (liver, kidneys, bone marrow, spleen), which is accompanied by corresponding clinical syndromes. When the blood vessels of the skin are damaged, a rash appears on it.
The repeated introduction of Salmonella into the intestinal lymphoid tissue from the biliary tract causes a sharp increase in the inflammatory process with the formation of ulcerative defects in its wall.
At 4-5 weeks of illness, bactericidal antibodies appear in the blood and the process of phagocytosis intensifies, which reduces the intensity of bacteremia. This leads to restoration of physiological balance and recovery.
However, complete elimination of the pathogen is not always observed.
With insufficient function of the immune system and incomplete phagocytosis, salmonella remain in the cells of the phagocytic system and can provoke relapses of the disease and bacterial carriage.
Complications
If the course of the disease is unfavorable and there is no treatment, the following undesirable consequences may develop:
Typhoid fever is one of the serious diseases that poses a threat to the patient's life. Only timely diagnosis of this pathology and adequate treatment help improve the prognosis, speed up recovery and reduce the risk of complications and relapses.
Which doctor should I contact?
Typhoid fever is treated in an infectious diseases hospital. Depending on the affected organs and complications, consultation with a cardiologist, neurologist, gastroenterologist, pulmonologist or surgeon may be required.
About typhoid fever in the program “Live Healthy!” with Elena Malysheva:
Loading…
Source: https://myfamilydoctor.ru/bryushnoj-tif-prichiny-vozniknoveniya-simptomy/
Classification
The abdominal type is classified according to the following criteria:
Character of the current:
- typical;
- atypical (can occur in erased, abortive (shortened) or outpatient forms);
- rare variants (pneumotyphoid - lung damage, meningotyphoid - brain damage, nephrotyphoid - kidneys, colotyphoid - large intestine and typhoid gastroenteritis).
Duration of flow:
- spicy;
- with exacerbations (recurrent).
Severity:
- light;
- medium-heavy;
- heavy.
Presence/absence of complications:
- uncomplicated option;
- complicated: specific (intestinal bleeding or perforation, infectious-toxic shock);
- nonspecific (inflammation of the lungs, salivary glands, gallbladder and others).
What complications does typhoid fever cause?
Complications are divided into:
- on specific ones, depending on the effect of the pathogen and typhoid toxin;
- nonspecific, caused by accompanying microflora.
The first include:
- intestinal bleeding;
- perforation of the intestinal wall;
- infectious-toxic shock.
By the eighth day, a roseola rash appears on the abdomen and chest in the form of small pink spots that disappear with pressure, the number of elements is small. The
second type includes various inflammatory diseases against the background of severe suppression of the immune system (pneumonia, pyelonephritis, meningitis, mumps, stomatitis). Specific complications deserve the most attention. They can occur from the second week of illness and later.
Intestinal bleeding - caused by vascular damage during ulceration and rejection of necrotic masses. The patient turns pale, the frequency increases, blood pressure decreases, and tarry, loose stools appear on the second day.
Perforation of the wall occurs after the formation of ulcers. This pathology was found in 30% of those who died from typhus. The “signal” is abdominal pain during the peak period. With typhus there are no “dagger” pains, so even weak ones should attract attention.
Signs of typhoid fever do not exclude tension in the abdominal muscles. Local sensitivity should be determined, muscle protection should be strengthened, bowel sounds should be listened to, and the participation of the abdominal wall in breathing should be monitored. Emergency care for bleeding and perforation of the intestinal wall consists of urgent surgery for life-saving reasons.
The state of shock is caused by the release of endotoxin into the blood in weakened patients. The signs are no different from any shock.
Signs of the disease
The incubation period for this infection lasts on average 10–14 days, but can be shortened to 7 days and extended to 23. How long the incubation period will last depends on the severity of immunity and the number of microbes entering the body. Clinical manifestations of typhoid fever appear cyclically depending on the period of the disease. There are 4 periods of typhoid fever:
- Initial period
After the end of the incubation period, which may be accompanied by prodromal symptoms (malaise, feeling weak, headache, sleep disturbance, loss of appetite, mild low-grade fever), an initial period follows, lasting about a week. This stage of the disease is characterized by signs of intoxication, which can gradually increase or appear abruptly within 1 to 2 days. The temperature rises significantly, up to 30 degrees, weakness and weakness intensify, and appetite disappears. Possible constant headaches, sleep disturbances (insomnia at night, drowsiness during the day), stool retention. In some cases, patients report diarrhea of the “pea stool” type, which indicates damage to the small intestine.
General examination: the patient is lethargic and adynamic, the skin is pale, the face is pasty, blood pressure is reduced, hard breathing with intermittent dry wheezing is heard in the lungs. The tongue is thickened, covered with a gray-white coating, along the edges and at the tip the tongue is crimson with tooth marks (typhoid tongue). There is moderate hyperemia and thickening of the tonsils. The abdomen is soft, swollen (flatulence). Towards the end of the period of initial manifestations, an enlarged liver and sometimes the spleen are palpated (hepatosplenomegaly).
- High period
Lasts 7 – 14 days. At this stage, the phenomena of intoxication increase, the temperature rises to 40 - 41 degrees, and is constant. Encephalopathy is pronounced (due to the action of endotoxin): the patient is lethargic, consciousness is impaired (stunning or stupor), and begins to become delirious against a background of high fever. Headaches and insomnia are excruciating. The tongue is covered with a brown coating and is dry (fullinginous tongue). The face is very pale and pasty, the lips are dry, with cracks, the eyes are sleepy, there is almost a complete absence of facial expressions, the patient himself is indifferent. Daily diuresis also decreases and constipation appears (a characteristic sign of typhoid fever), which is associated with toxic intestinal paresis.
Approximately on the 10th day, most patients develop exanthema. The rash is localized in the lower chest and upper abdomen. Roseolas with a diameter of 2–3 mm, 5–6 pieces each, are formed. The rashes are clearly visible on pale skin and last no more than 3-4 days, after disappearing they leave light pigmentation. After the resolution of the first roseolas, new ones may appear - the “spilling” phenomenon. A number of patients experience carotene hyperchromia of the skin of the palms and feet - icteric staining.
- Resolution period
Lasts about a week. At this stage, symptoms of typhoid fever disappear, such as headaches and sleep disorders, anorexia and decreased diuresis. The temperature normalizes, but at first it becomes amphibious in nature, that is, the difference between the indicators at different times of the day is 2 - 3 degrees. Treatment with antibiotics is currently reflected in a decrease in temperature - its lysis occurs quickly and bypasses the amphibolic stage. Signs of intoxication persist for a long time (weakness, irritability, mental instability). Late complications of the disease may develop at this stage: thrombophlebitis or cholecystitis.
- Recovery period
The disease ends with recovery, the period of which previously, before the era of antibiotics, lasted 4–6 weeks. In 7–9% of cases, a relapse of the disease is possible, which occurs against the background of normal temperature and disappearance of symptoms of intoxication. Relapse is preceded by low-grade fever, persistent hepatosplenomegaly, absence of eosinophils in the blood and low levels of antibodies in it. Clinically, relapse of the disease is characterized by a milder course, a rapid increase in temperature, early appearance of exanthema, and less pronounced intoxication symptoms. The relapse lasts one day to several weeks, and can occur repeatedly.
Symptoms (signs)
The incubation period lasts from 3 to 25 days (on average two weeks). Body temperature gradually rises, reaching maximum values by the seventh day of illness. Along with the fever, symptoms of intoxication increase (weakness, weakness, headache, loss of appetite). In addition, the following symptoms appear:
- nausea and vomiting;
- diarrhea;
- flatulence;
- pale red rash on the skin of the shoulders, chest and back;
- nosebleeds;
- convulsions;
- constant cramping pain in the abdomen;
- numbness of the limbs;
- white coating on the tongue;
- disorders of the cardiovascular system;
- cough;
- increase in the size of the liver and spleen.
Due to the negative impact on the nervous system, the patient may experience lethargy, delirium, and hallucinations. The general condition improves after the temperature normalizes.
Diagnostics
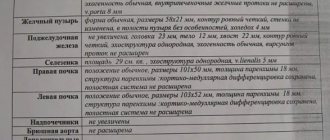
Diagnosis of typhoid fever is based on the collection of epidemiological data, the study of complaints, anamnesis and physical examination data, including laboratory tests:
- Epidemiological history
It is revealed the presence of contacts with feverish people, consumption of questionable purity of water and unwashed vegetables/fruits, milk and dairy products that have not undergone pasteurization (purchased from hand), a tense epidemiological situation regarding intestinal infections in the patient’s location, eating food in public catering establishments.
- Clinical data
High temperature, roseola rashes, lethargy of the patient, “typhoid tongue”, lack of appetite, confusion, sleep disorders and severe headaches, hepatosplenomegaly, stool retention and increased gas formation.
- General blood and urine tests
In the blood there is leukocytosis with a shift to the left, accelerated ESR. On the 4th – 5th day of the disease, a decrease in leukocytes to leukopenia, aneosinophilia, a decrease in platelets, relative lymphocytosis. Protein, casts and red blood cells are found in the urine. Later typhoid bacteria.
- Isolation of blood culture of typhoid bacillus
The decisive method in diagnosing the disease is an analysis for typhoid fever - blood culture in bile broth or Rappoport's medium. Venous blood is collected (15 ml), which is inoculated onto a nutrient medium. From the 8th day of illness, it is possible to isolate the pathogen from the elements of the rash, feces, urine and duodenal contents (isolation of rose culture, copro-, urine- and others).
- Serological methods
Serological blood tests for typhoid fever help confirm the diagnosis. The most common are the agglutination reaction (Widal reaction) and the indirect agglutination reaction (IRGA). In an infected person, specific agglutinins (antibodies) to the typhoid bacillus appear in the blood. RNGA is carried out using H-, O- and Vi-antigens on the day of admission and a week later. The diagnosis of typhoid fever is confirmed by an increase in the titer of O-antibodies by 4 times or a titer of 1:200. In the case of a positive reaction with the H-antigen, it indicates a previous history of typhoid fever or vaccination, and with the Vi-antigen, it indicates chronic carriage of the pathogen.
Comparative diagnosis of typhoid fever is carried out with influenza, malaria, brucellosis, typhus, adenovirus infection, tuberculosis, leptospirosis, sepsis and other infectious diseases.
Pathogenesis
The causative agent of typhoid fever is Salmonella typhi, a mobile gram-negative and extremely viable bacillus that produces endotoxin, which is dangerous only to humans. For example, the pathogen dies only at high temperatures, for example, by boiling. When heated to 60°C, the stick can last 30 minutes; it survives freezing perfectly. The bacterium can die within a few minutes when exposed to phenol, chlorine or Lesol. That is why wastewater and drinking water treatment plays a leading role in disease prevention.
Salmonella typhi enters the human body with food, water or milk. The only reservoir of the causative agent of typhoid fever is humans. Salmonella typhi is excreted in the patient's feces, after which flies and other insects can become carriers of the bacilli on food. In the acute stage of the disease, they are excreted with sputum, vomit and other biological fluids. Due to the fact that the bacillus survives well in the cold, survives drying out and thrives in sewage, typhus can quickly take on the character of an epidemic. Outbreaks of the disease occur mainly in unsanitary conditions due to insufficient chlorination of water, retention of sewage, or during floods and other natural disasters.
Treatment
Treatment of typhoid fever must be carried out in a hospital. All febrile patients suspected of having this infection are subject to hospitalization. Treatment is carried out comprehensively and combines etiotropic and pathogenetic therapy:
- Regime and care
The patient is prescribed strict bed rest to prevent tension in the abdominal muscles, which can cause intestinal perforation or intestinal bleeding. It is allowed to sit down on the 7th – 8th day, provided the temperature normalizes, and to walk from the 10th – 11th day. It is important to maintain good oral hygiene and ensure regular bowel movements. The administration of cleansing enemas is prohibited.
- Diet
A gentle diet is prescribed, first table 4A, the diet is expanded when the temperature normalizes and signs of intoxication weaken (tables 4, then 2, later 13). Food should be boiled or pureed, meals should be taken in fractions and small portions, drinking regime should be free - consume large amounts of liquid.
- Antibiotic therapy
The drugs of choice for typhoid fever are fluoroquinolones due to the spread of bacterial strains that are resistant to ampicillin and chloramphenicol. Antibiotic treatment is prescribed for the entire febrile period and the first 10 days after the temperature normalizes (ciprofloxacin, cefloxacin, ofloxacin).
- Immunotherapy
It is carried out according to indications (prolonged isolation of the pathogen, exacerbations and relapses of the disease). Immunomodulators (pentoxyl, thymogen) and typhoid vaccine are prescribed.
- Detoxification therapy
Saline solutions, hemodez, rheopolyglucin, and glucose are administered intravenously.
- Vitamin therapy, antioxidants
Vitamins C and E, cytochrome C, unithiol and aevit.
If intestinal bleeding occurs, the patient is prescribed absolute rest (lying on his back), hunger and cold on the stomach, and limited fluid intake (no more than half a liter and a teaspoon) for a period of 12 to 24 hours. For the purpose of hemostasis, aminocaproic acid, blood substitutes, and hemostatic agents (dicinone) are administered. If the intestinal wall is perforated, emergency surgery is indicated.
Prevention
Measures to prevent typhoid fever are divided into 2 categories:
- Specific
Specific prevention is carried out according to epidemiological indications (high incidence: 25 patients per 100 thousand population, visiting a country where there is a high incidence rate, prolonged contact with a bacterial pathogen). For this purpose, vaccination of all persons from 15 to 55 years is carried out. The first vaccination against typhoid fever is administered subcutaneously (0.5 ml), the second is performed a month later (1 ml), revaccination is carried out after 24 months (1 ml). Children from 3 years of age are vaccinated with typhoid Vi-polysaccharide vaccine (Vianvac) once (0.5 ml). Revaccination is performed after 3 years.
- Nonspecific
These include: establishing proper water supply and sewerage, control over the work of public catering establishments (compliance with the rules of food preparation, shelf life and sale of products), sanitary education work among the population, promotion and observance of personal hygiene. Also, nonspecific prevention includes: disinfection of wastewater, sanitary and technical support of water supply and sewerage structures, employment at food facilities with permission (absence of antibody titre with O- and Vi-diagnosticums, negative result of bacterial stool examination).
Typhoid fever - symptoms, treatment, causes of the disease, first signs
- Universal compliance with sanitary and hygienic rules (from personal hygiene to water supply).
- Wash your hands often with warm water and soap.
- Get the appropriate vaccination.
- In areas with poor sanitation, doctors recommend consuming only bottled water.
- Consult a doctor immediately if the first signs of the disease are detected.
Prevention of the disease also includes: supplying the population with high-quality water, timely removal of garbage and sewage from populated areas, and control of insects.
Repeated illness is an extremely rare occurrence; typhoid fever usually leaves lasting immunity.
Folk remedies
Folk remedies can only be effective in preventing this disease, but not in the treatment process. If this disease manifests itself, consult a doctor and follow his recommendations. Folk remedies in combination with medications can only speed up the recovery process from typhoid fever.
Here are fairly simple ways to avoid this disease or increase the effectiveness of traditional treatment:
- To protect yourself from typhoid fever, traditional medicine recommends chewing raw calamus root, which has a bactericidal effect.
- In conjunction with drug treatment, it is useful to take burnet root. To prepare a decoction, crushed burnet root is poured with water, then boiled and filtered through cheesecloth. The decoction should be cooled before use.
- To improve heart function in the event of viral diseases, take currant juice.
- St. John's wort has beneficial properties. It promotes faster tissue healing and also has an astringent, antibacterial and immune-strengthening effect. This herb should be consumed as an infusion.
A collection of centaury, medicinal chamomile and sage, which is poured with boiling water and infused, is also popular. It is believed that this remedy has no side effects, however (as with any recipe from traditional medicine), it is imperative to consult a specialist before using it.
Plantain helps with disorders of the gastrointestinal mucosa and bloody diarrhea. A decoction is prepared from it. In this case, the seeds are boiled and consumed shortly before meals; sometimes plantain leaves are also used.
The information is for reference only and is not a guide to action. Do not self-medicate. At the first symptoms of the disease, consult a doctor.
Source: https://yellmed.ru/bolezni/bryushnoy-tif
Question answer
When is discharge from the hospital after treatment for typhoid fever?
The timing of discharge depends on the severity of the disease, temperature readings and negative results. examination of feces and urine (carried out twice) and duodenal contents (once). A patient who has recovered from the disease is discharged no earlier than 21–23 days. A patient with a mild course of the disease spends an average of 25 days in the hospital, with a moderate course up to 30 days, and with a severe course up to 45 days.
Can you die from typhoid fever?
In the pre-antibiotic era, the death rate from typhoid fever ranged from 3 to 20%. In recent years, the mortality rate has decreased and is in the range of 0.2 – 0.3%. The possibility of an unfavorable prognosis still exists even with a mild course of the disease due to the possible occurrence of severe complications (intestinal bleeding or intestinal perforation).
What is the treatment for bacteria excretion?
Treatment for bacterial excretion has not been developed to date. It is important to treat concomitant diseases. In some cases, it is possible to stop the release of typhoid bacteria by taking ampicillin, immunostimulants and introducing a specific monovaccine.
Ласковые лучшие феи проститутки Нальчика, сладкие и ухоженные, они такие заботливые и привлекательные, что интимный досуг тебе обеспечен. Не отказывай себе в удовольствии. Встречаются не в салоне, лучшие феи проститутки Нальчика, это не развод, убедись взглянув на oopsnalchik.ru. Жрицы любви не понаслышке знают, как доставить мужчине ни с чем не сравнимое наслаждение.